Abstract
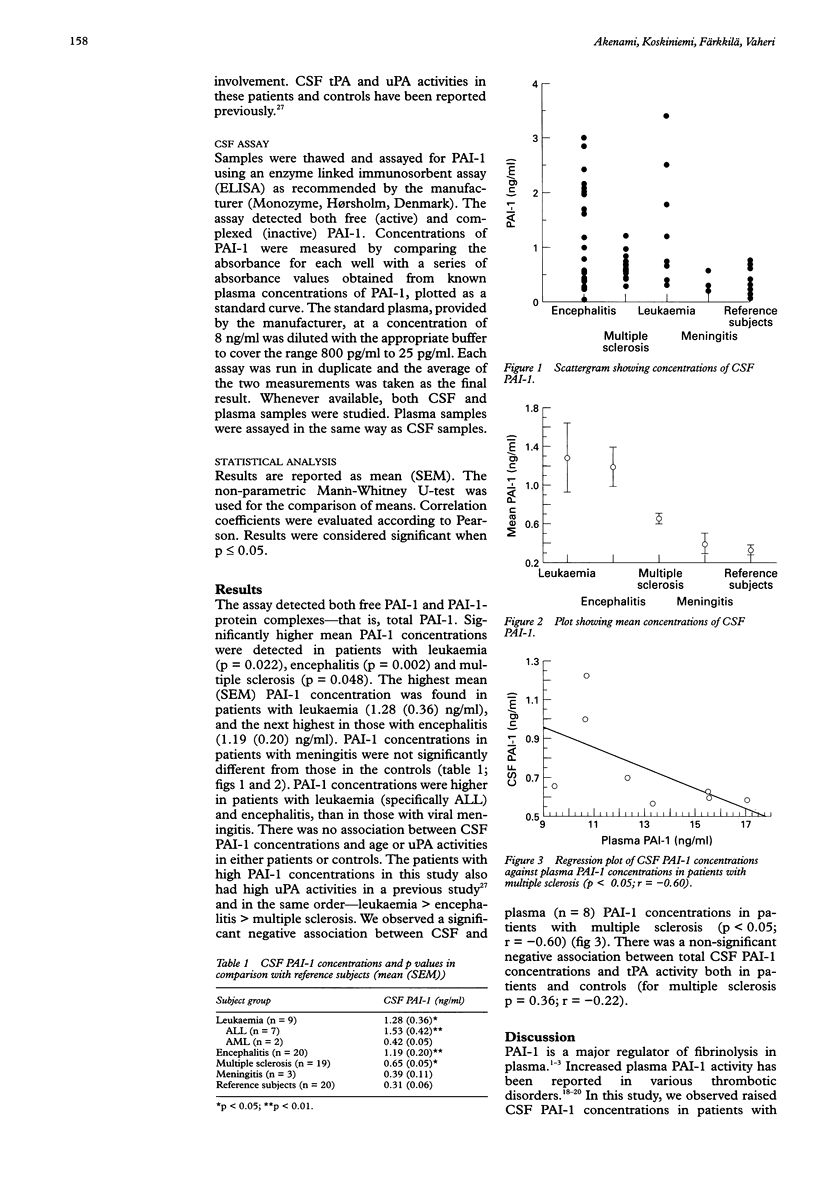
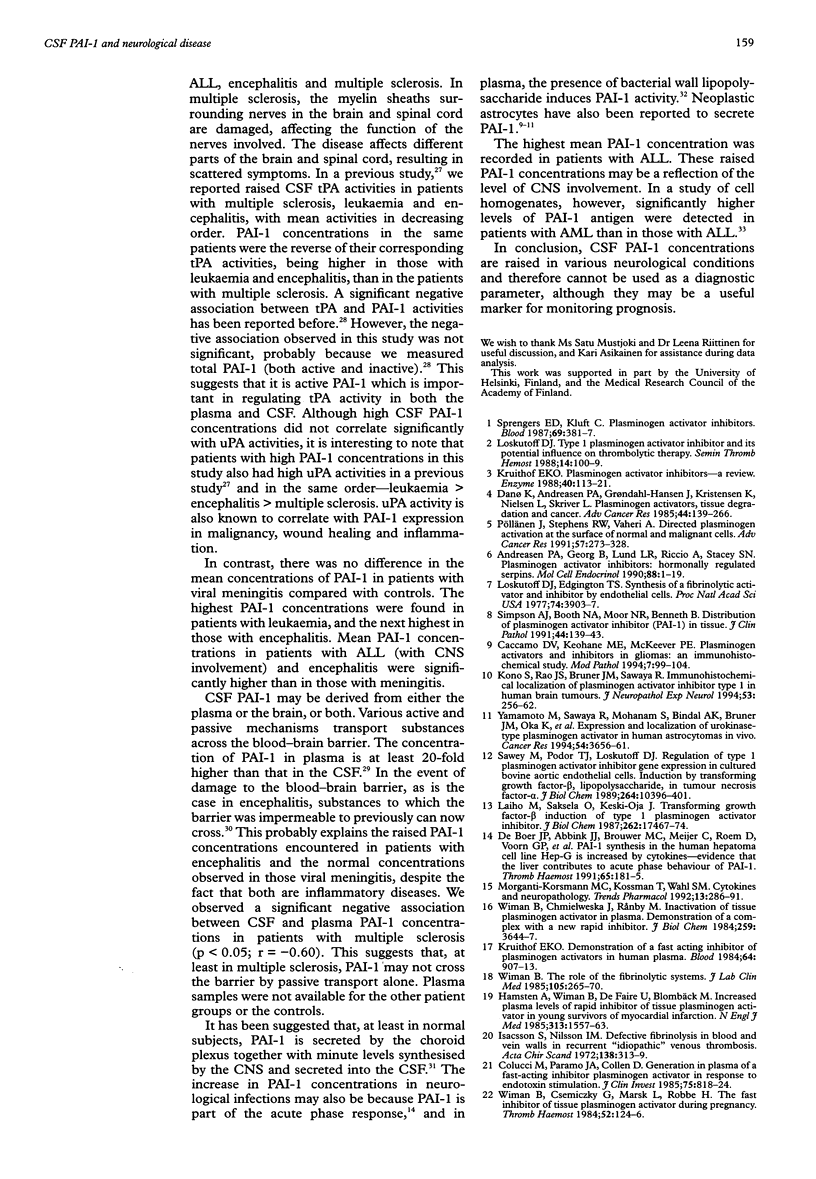
AIM: To study cerebrospinal fluid (CSF) concentrations of plasminogen activator inhibitor type-1 (PAI-1) in patients with neurological disease. METHODS: CSF PAI-1 concentrations were measured in 51 patients with neurological disease and 20 reference subjects using an ELISA. The patient group comprised three patients with viral meningitis, 20 with encephalitis, nine with acute lymphoblastic (n = 7) and myeloid (n = 2) leukaemia (with central nervous system involvement), and 19 with multiple sclerosis. RESULTS: Raised PAI-1 concentrations were observed in patients with leukaemia, encephalitis and multiple sclerosis. There was no difference in the mean concentrations of PAI-1 in patients with meningitis when compared with the reference subjects. The highest mean (SEM) PAI-1 concentration was found in patients with leukaemia (1.28 (0.36) ng/ml), and the next highest in those with encephalitis (1.19 (0.20) ng/ml). these values were much higher than those in patients with viral meningitis. In a previous report, raised CSF tissue-type plasminogen activator (tPA) activities were detected in patients with multiple sclerosis, leukaemia and encephalitis, with mean activities in decreasing order. PAI-1 concentrations in the same patients were the reverse of their corresponding tPA activities, being higher in those with leukaemia and encephalitis, than in patients with multiple sclerosis. There was no association between CSF PAI-1 concentrations and age in either patients or controls. Similarly, there was no association between CSF PAI-1 concentrations and urokinase-type plasminogen activator (uPA). CONCLUSIONS: Raised CSF PAI-1 concentrations may be used as a non-specific marker of neurological disease. Moreover, PAI-1 may play an important role in regulating the functions tPA, and probably uPA, in CSF.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akenami F. O., Sirén V., Koskiniemi M., Siimes M. A., Teräväinen H., Vaheri A. Cerebrospinal fluid activity of tissue plasminogen activator in patients with neurological diseases. J Clin Pathol. 1996 Jul;49(7):577–580. doi: 10.1136/jcp.49.7.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen P. A., Georg B., Lund L. R., Riccio A., Stacey S. N. Plasminogen activator inhibitors: hormonally regulated serpins. Mol Cell Endocrinol. 1990 Jan 2;68(1):1–19. doi: 10.1016/0303-7207(90)90164-4. [DOI] [PubMed] [Google Scholar]
- Caccamo D. V., Keohane M. E., McKeever P. E. Plasminogen activators and inhibitors in gliomas: an immunohistochemical study. Mod Pathol. 1994 Jan;7(1):99–104. [PubMed] [Google Scholar]
- Colucci M., Paramo J. A., Collen D. Generation in plasma of a fast-acting inhibitor of plasminogen activator in response to endotoxin stimulation. J Clin Invest. 1985 Mar;75(3):818–824. doi: 10.1172/JCI111777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danø K., Andreasen P. A., Grøndahl-Hansen J., Kristensen P., Nielsen L. S., Skriver L. Plasminogen activators, tissue degradation, and cancer. Adv Cancer Res. 1985;44:139–266. doi: 10.1016/s0065-230x(08)60028-7. [DOI] [PubMed] [Google Scholar]
- De Vries T. J., Mooy C. M., Van Balken M. R., Luyten G. P., Quax P. H., Verspaget H. W., Weidle U. H., Ruiter D. J., Van Muijen G. N. Components of the plasminogen activation system in uveal melanoma--a clinico-pathological study. J Pathol. 1995 Jan;175(1):59–67. doi: 10.1002/path.1711750110. [DOI] [PubMed] [Google Scholar]
- Emeis J. J., Kooistra T. Interleukin 1 and lipopolysaccharide induce an inhibitor of tissue-type plasminogen activator in vivo and in cultured endothelial cells. J Exp Med. 1986 May 1;163(5):1260–1266. doi: 10.1084/jem.163.5.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gijtenbeek J. M., Emeis J. J., van der Sande J. J., Lulf R. E. Different types of plasminogen activator activity in human brain tumours: relation with peritumoral oedema? Clin Neurol Neurosurg. 1994 Nov;96(4):305–309. doi: 10.1016/0303-8467(94)90119-8. [DOI] [PubMed] [Google Scholar]
- Hamsten A., Wiman B., de Faire U., Blombäck M. Increased plasma levels of a rapid inhibitor of tissue plasminogen activator in young survivors of myocardial infarction. N Engl J Med. 1985 Dec 19;313(25):1557–1563. doi: 10.1056/NEJM198512193132501. [DOI] [PubMed] [Google Scholar]
- Isacson S., Nilsson I. M. Defective fibrinolysis in blood and vein walls in recurrent "idiopathic" venous thrombosis. Acta Chir Scand. 1972;138(4):313–319. [PubMed] [Google Scholar]
- Kono S., Rao J. S., Bruner J. M., Sawaya R. Immunohistochemical localization of plasminogen activator inhibitor type 1 in human brain tumors. J Neuropathol Exp Neurol. 1994 May;53(3):256–262. doi: 10.1097/00005072-199405000-00006. [DOI] [PubMed] [Google Scholar]
- Koskiniemi M., Vaheri A., Taskinen E. Cerebrospinal fluid alterations in herpes simplex virus encephalitis. Rev Infect Dis. 1984 Sep-Oct;6(5):608–618. doi: 10.1093/clinids/6.5.608. [DOI] [PubMed] [Google Scholar]
- Kruithof E. K., Nicolosa G., Bachmann F. Plasminogen activator inhibitor 1: development of a radioimmunoassay and observations on its plasma concentration during venous occlusion and after platelet aggregation. Blood. 1987 Nov;70(5):1645–1653. [PubMed] [Google Scholar]
- Kruithof E. K. Plasminogen activator inhibitors--a review. Enzyme. 1988;40(2-3):113–121. doi: 10.1159/000469153. [DOI] [PubMed] [Google Scholar]
- Kruithof E. K., Tran-Thang C., Ransijn A., Bachmann F. Demonstration of a fast-acting inhibitor of plasminogen activators in human plasma. Blood. 1984 Oct;64(4):907–913. [PubMed] [Google Scholar]
- Laiho M., Saksela O., Keski-Oja J. Transforming growth factor-beta induction of type-1 plasminogen activator inhibitor. Pericellular deposition and sensitivity to exogenous urokinase. J Biol Chem. 1987 Dec 25;262(36):17467–17474. [PubMed] [Google Scholar]
- Loskutoff D. J., Edgington T. E. Synthesis of a fibrinolytic activator and inhibitor by endothelial cells. Proc Natl Acad Sci U S A. 1977 Sep;74(9):3903–3907. doi: 10.1073/pnas.74.9.3903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loskutoff D. J. Type 1 plasminogen activator inhibitor and its potential influence on thrombolytic therapy. Semin Thromb Hemost. 1988 Jan;14(1):100–109. doi: 10.1055/s-2007-1002762. [DOI] [PubMed] [Google Scholar]
- Morganti-Kossmann M. C., Kossmann T., Wahl S. M. Cytokines and neuropathology. Trends Pharmacol Sci. 1992 Jul;13(7):286–291. doi: 10.1016/0165-6147(92)90087-m. [DOI] [PubMed] [Google Scholar]
- Pöllänen J., Stephens R. W., Vaheri A. Directed plasminogen activation at the surface of normal and malignant cells. Adv Cancer Res. 1991;57:273–328. doi: 10.1016/s0065-230x(08)61002-7. [DOI] [PubMed] [Google Scholar]
- Rao J. S., Chen M., Festoff B. W. Plasminogen activator inhibitor 1, the primary regulator of fibrinolysis, in normal human cerebrospinal fluid. J Neurosci Res. 1993 Feb 15;34(3):340–345. doi: 10.1002/jnr.490340311. [DOI] [PubMed] [Google Scholar]
- Rånby M., Sundell I. B., Nilsson T. K. Blood collection in strong acidic citrate anticoagulant used in a study of dietary influence on basal tPA activity. Thromb Haemost. 1989 Nov 24;62(3):917–922. [PubMed] [Google Scholar]
- Sawaya R., Rayford A., Kono S., Ang K. K., Feng Y., Stephens L. C., Rao J. S. Plasminogen activator inhibitor-1 in the pathogenesis of delayed radiation damage in rat spinal cord in vivo. J Neurosurg. 1994 Sep;81(3):381–387. doi: 10.3171/jns.1994.81.3.0381. [DOI] [PubMed] [Google Scholar]
- Sawdey M., Podor T. J., Loskutoff D. J. Regulation of type 1 plasminogen activator inhibitor gene expression in cultured bovine aortic endothelial cells. Induction by transforming growth factor-beta, lipopolysaccharide, and tumor necrosis factor-alpha. J Biol Chem. 1989 Jun 25;264(18):10396–10401. [PubMed] [Google Scholar]
- Simpson A. J., Booth N. A., Moore N. R., Bennett B. Distribution of plasminogen activator inhibitor (PAI-1) in tissues. J Clin Pathol. 1991 Feb;44(2):139–143. doi: 10.1136/jcp.44.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprengers E. D., Kluft C. Plasminogen activator inhibitors. Blood. 1987 Feb;69(2):381–387. [PubMed] [Google Scholar]
- Sutton R., Keohane M. E., VanderBerg S. R., Gonias S. L. Plasminogen activator inhibitor-1 in the cerebrospinal fluid as an index of neurological disease. Blood Coagul Fibrinolysis. 1994 Apr;5(2):167–171. doi: 10.1097/00001721-199404000-00002. [DOI] [PubMed] [Google Scholar]
- Wada H., Kumeda Y., Ogasawara Z., Ohiwa M., Kaneko T., Tamaki S., Ohno T., Kageyama S., Kobayashi T., Deguchi K. Plasminogen activators and their inhibitors in leukemic cell homogenates. Am J Hematol. 1993 Feb;42(2):166–170. doi: 10.1002/ajh.2830420205. [DOI] [PubMed] [Google Scholar]
- Wiman B., Chmielewska J., Rånby M. Inactivation of tissue plasminogen activator in plasma. Demonstration of a complex with a new rapid inhibitor. J Biol Chem. 1984 Mar 25;259(6):3644–3647. [PubMed] [Google Scholar]
- Wiman B., Csemiczky G., Marsk L., Robbe H. The fast inhibitor of tissue plasminogen activator in plasma during pregnancy. Thromb Haemost. 1984 Oct 31;52(2):124–126. [PubMed] [Google Scholar]
- Wiman B., Ljungberg B., Chmielewska J., Urdén G., Blombäck M., Johnsson H. The role of the fibrinolytic system in deep vein thrombosis. J Lab Clin Med. 1985 Feb;105(2):265–270. [PubMed] [Google Scholar]
- Yamamoto M., Sawaya R., Mohanam S., Bindal A. K., Bruner J. M., Oka K., Rao V. H., Tomonaga M., Nicolson G. L., Rao J. S. Expression and localization of urokinase-type plasminogen activator in human astrocytomas in vivo. Cancer Res. 1994 Jul 15;54(14):3656–3661. [PubMed] [Google Scholar]
- de Boer J. P., Abbink J. J., Brouwer M. C., Meijer C., Roem D., Voorn G. P., Lambers J. W., van Mourik J. A., Hack C. E. PAI-1 synthesis in the human hepatoma cell line HepG2 is increased by cytokines--evidence that the liver contributes to acute phase behaviour of PAI-1. Thromb Haemost. 1991 Feb 12;65(2):181–185. [PubMed] [Google Scholar]


