Abstract
Background
The term “adrenal fatigue” (“AF”) has been used by some doctors, healthcare providers, and the general media to describe an alleged condition caused by chronic exposure to stressful situations. Despite this, “AF” has not been recognized by any Endocrinology society, who claim there is no hard evidence for the existence. The aim of this systematic review is to verify whether there is substantiation for “AF”.
Methods
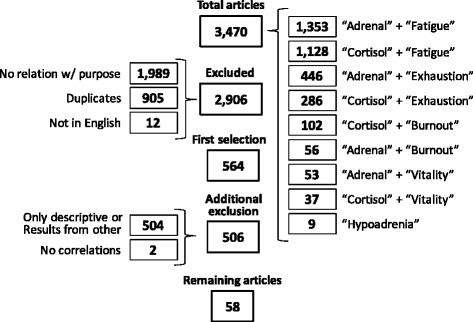
A systematic search was performed at PUBMED, MEDLINE (Ebsco) and Cochrane databases, from the beginning of the data until April 22nd, 2016. Searched key words were: “adrenal” + “fatigue”, “adrenal” + “burnout”, “adrenal” + “exhaustion”, “hypoadrenia”, “burnout” + “cortisol”, “fatigue” + “cortisol”, “clinical” + “burnout”, “cortisol” + “vitalility”, “adrenal” + “vitality”, and “cortisol” + “exhaustion”. Eligibility criteria were: (1) articles written in English, (2) cortisol profile and fatigue or energy status as the primary outcome, (3) performed tests for evaluating the adrenal axis, (4) absence of influence of corticosteroid therapy, and (5) absence of confounding diseases. Type of questionnaire to distinct fatigued subjects, population studied, tests performed of selected studies were analyzed.
Results
From 3,470 articles found, 58 studies fulfilled the criteria: 33 were carried in healthy individuals, and 25 in symptomatic patients. The most assessed exams were “Direct Awakening Cortisol” (n = 29), “Cortisol Awakening Response” (n = 27) and “Salivary Cortisol Rhythm” (n = 26).
Discussion
We found an almost systematic finding of conflicting results derived from most of the studies methods utilized, regardless of the validation and the quality of performed tests. Some limitations of the review include: (1) heterogeneity of the study design; (2) the descriptive nature of most studies; (3) the poor quality assessment of fatigue; (4) the use of an unsubstantiated methodology in terms of cortisol assessment (not endorsed by endocrinologists); (5) false premises leading to an incorrect sequence of research direction; and, (6) inappropriate/invalid conclusions regarding causality and association between different information.
Conclusion
This systematic review proves that there is no substantiation that “adrenal fatigue” is an actual medical condition. Therefore, adrenal fatigue is still a myth.
Keywords: Adrenal depletion, Adrenal fatigue, Cortisol, Adrenal insufficiency, Burnout, Fatigue
Background
The term “adrenal fatigue” (“AF”) has been used by some doctors, healthcare providers, and the general media to describe an alleged condition caused by chronic exposure to stressful situations. According to this theory, chronic stress could potentially lead to “overuse” of the adrenal glands, eventually resulting in their functional failure. In a recent search on Google (April 22, 2016), “adrenal fatigue” provided 640,000 results, and the association of the two words exhibited 1,540,000 findings. Despite this, “adrenal fatigue” has not been recognized by any endocrinology societies to date, who claim there is no evidence for the existence of this syndrome [1].
Conversely, some medical societies, although unrecognized by American Board of Medical Specialties and Association of American Medical Colleges [2, 3], claim that adrenal fatigue is a real and underdiagnosed disease [4, 5]. According to these societies, to screen for “AF” in patients, a questionnaire developed by Dr. Wilson, who is reportedly the first person to describe this supposed syndrome, is recommended to be used [6]. In addition, patients suspected of “AF” are now being tested for serum basal cortisol levels and salivary cortisol rhythm. Those who present impaired results from these tests are then treated with corticosteroids, regardless of the etiology. As a result, corticosteroids (mainly hydrocortisone) are probably being prescribed to a large number of patients, as at least 24,000 health providers [7] are instructed by one medical society (The American Academy of Anti-Aging Medicine – A4M) to prescribe corticosteroids in these cases.
Arguments for corticosteroid use as a treatment for “claimed AF” include: [1] the immediate and significant improvement seen in patients who are prescribed corticosteroid, and [2] the long and extensive clinical symptomatology of this alleged disease, which shows a slow depletion before clinical and severe hypocortisolism ensues [4–6]. Moreover, others claim that endocrinologists use much too strict diagnostic criteria before prescribing corticosteroids, and thus, many sufferers would not be receiving adequate treatment [4, 6]. However, there are logical counterarguments to routine corticosteroid use in these patients. First, corticosteroids promote a sense of wellbeing (usually temporary), regardless of the patient’s condition. Second, even at low and physiological doses, corticosteroids increase the risk for several disorders, such as psychiatric disorders [8–11], osteoporosis [12], myopathy [13], glaucoma [14], metabolic disorders [14, 15], sleep disturbances [16] and cardiovascular diseases [17, 18].
Therefore, is “adrenal fatigue” an actual disorder? Is fatigue related to depleted adrenal function? Does fatigued healthy subjects present relative adrenal failure? Is adrenal involved in the pathophysiology of fatigue in diseases? Which tests were performed in order to establish markers or triggers? The aim of this systematic review was to determine the correlation between adrenal status and fatigue states, including the recently described “burnout” or “burnout syndrome”, and other fatigue-related diseases. The primary objective was to evaluate the methodology for fatigue status assessment, including cortisol tests, and to examine the results of studies involving cortisol and fatigue correlation.
Methods
Search strategies
The PRISMA protocol for systematic reviews was utilized for this study design. A systematic search was conducted through the electronic PUBMED, MEDLINE (Ebsco), and COCHRANE databases, from the beginning of the data until April 22, 2016. The search strategy included the following keywords: (1) “adrenal + fatigue”; (2) “adrenal + burnout”; (3) “adrenal + exhaustion”; (4) “adrenal” + “fatigue”; (5) “hypoadrenia”; (6) “cortisol” + “fatigue”; (7) “cortisol” + “burnout”; (8) “clinical” + “burnout”; (9) “cortisol” + “vitality”; (10) “adrenal” + “vitality”; and (11) “cortisol” + “exhaustion”, where “a + b” means “a” and “b” together in the exact expression, and “a” +”b” means that both words needed to be contained in the article, but not necessarily together. Although the terms “adrenal + fatigue” and “adrenal” + “fatigue” were searched, as articles found using the first criteria were also found using the second criteria, further analysis were performed for the exact expression that matched with the disease. We also analyzed articles mentioned within identified studies whenever the alleged disorder, or a similar situation, were described (such as cortisol profile and exhaustion or fatigued patients).
Data extraction
All studies were evaluated by the two reviewers (F.A.C. and C.E.K.) after removal of duplicate articles, according to: (1) authorship, (2) journal, (3) publication date, (4) studied population, (5) definition of “fatigue”, “exhaustion”, and “burnout”, (6) study design and methods, (7) analysis methods to assess adrenal axis, (8) results, (9) conclusions, and (10) study variables and bias.
Inclusion and exclusion criteria
Inclusion criteria were: (1) whole article written in English, (2) cortisol profile and fatigue or energy status as the primary outcome, (3) specific tests performed for evaluating the adrenal axis, (4) absence of corticosteroid therapy, (5) absence of confounding diseases that would lead to an impaired cortisol status caused by the disorder itself (such as depression, alcoholism, and morbid obesity). Studies with a merely description about adrenal axis impairment with no tests performed were excluded.
Quality assessment
The abstract of each of identified study was analyzed by one of the authors (F.A.C.), and was excluded if it did not meet the eligibility criteria. The studies that fulfilled the inclusion criteria were entirely evaluated regarding the rationale, method design, primary outcome, assessment of fatigue, statistical analysis, results, discussion, and conclusions, in order to improve data quality. Those studies that presented any bias in the methodology, results, or interpretation of the exposed data, which could be reflected in the analysis of the study as a whole, were also excluded.
Statistical analysis
Each of the studied populations, each of the questionnaires and each of the tests performed were quantified, whereas tests results were analyzed in terms of percentage of type of responses for each of the tests performed. Results were analyzed in general and according to the underlying disease.
Results
Study selection
In total, 3,470 articles were identified. A summary of the study selection is shown in Fig. 1. The search for “adrenal” + “burnout” yielded 56 studies; “adrenal” + “exhaustion” yielded 446 articles; “adrenal” + “fatigue” yielded 1,353 articles; “fatigue” + “cortisol” yielded 1,128 articles; “cortisol” + “burnout” yielded 102 articles; “cortisol” + “vitality” yielded 37 articles; “adrenal” + “vitality” yielded 53 articles; “hypoadrenia” yielded 9 articles articles (“hypoadrenocorticism” yielded 1,302 articles but is used to refer to hypocortisolism in animals, and therefore, was not included here); and “cortisol” + “exhaustion” yielded 286 articles. Twelve studies were excluded because they were written in languages other than English, 1,989 were excluded because there was no relation with the purpose of the systematic review, whereas 905 articles of interest were duplicates. Of the 564 remaining studies, 504 had only descriptive characteristics or contained results already presented in another study (in which tests were performed), and therefore were excluded. Two studies were excluded because despite of the correlation between cortisol profile and burnout or multiple sclerosis, they did not perform correlation between fatigue and cortisol, but other aspects, as depression and pain [19, 20]. For the systematic review, we analyzed all the included and not excluded studies, which represent a total of 58 articles (1.67 % of the original search) (Table 1).
Fig. 1.
Study selection
Table 1.
Summary of selected studies
| First Author & Reference | Year of Publication | Number of Patients | Population | Questionnaire | Tests | Results | Comments |
|---|---|---|---|---|---|---|---|
| McLennan [21] | 2016 | 257 | H/B | Maslach | HCC | Nl | |
| Schmidt [69] (part 1) | 2016 | 265 | Breast Cancer | FAQ | DAC, CAR, SCR, NSC | ↑NSC, ↑AUC, Nl CAR, Nl DAC, ↓SCR | Pts. mostly on chemotherapy (ChTx); schemes not specified. No controls, only correlation between fatigue levels and tests. ChTx related to worse fatigue. Initial tests performed during, w/ or w/o ChTx. |
| Schmidt [69] (part 2) | 2016 | 265 | Breast Cancer | FAQ | DAC, CAR, SCR, NSC | ↑AUC, ↑CAR, ↑NSC, ↑SCR, Nl DAC | Second test of the study, performed after 14 weeks of procedures. |
| Sjors [25] | 2015 | 220 | H/B | SMBQ | DAC, CAR | ↓CAR, ↑DAC | Results normalized after adjustment of anti-depressive use; SCR results not provided |
| Oosterholt [28] | 2015 | 91 | H/B | Maslach | DAC, CAR, SCR, AUC, CAR 60 min | Nl SCR, ↓CAR, Nl AUC, Nl CAR 60 min, ↓DAC | Control of variations did not change results |
| De Vente [22] | 2015 | 95 | H/B | Acute Psychosocial Stressor diagnosis | MSC, MST | Nl MSC, Nl MST | MST: Nl (women), reduced (men); MSC: Nl (men), reduced (women). Mental arithmetic and public speech stressors also performed |
| Lennartsson [24] | 2015 | 56 | H/B | DCSRD; exclusion w/ SEQ | DHEA-S; ACTH; ACTH and DHEA-S post-TSST (TSST stress test performed) | ↓DHEA-S, ↓post-TSST DHEA-S, Nl ACTH, Nl post-TSST ACTH | |
| Tao [23] | 2015 | 171 | H/B | Maslach | MSC, ACTH | ↑ACTH, ↑MSC | |
| Jonsson [29] | 2015 | 51 | H/B | SMBQ | MSC, MST | Nl MSC, ↓MST | |
| Lennartsson [27] | 2015 | 56 | H/B | DCSRD and SMBQ | MSC, MST, ACTH, ACTH post-TSST (TSST stress test performed) | Nl MSC, Nl MST, Nl ACTH, Nl post-TSST ACTH | Severe BO: lower ACTH, cortisol response to TSST vs controls, whereas low BO: higher ACTH, cortisol responses vs controls |
| Schmaling [26] | 2015 | 62 | Healthy | ADAS | AUC, SCR | ↓AUC, ↓SCR | 31 couples studied, one of which had chronic fatigue (but not CFS) |
| Sveinsdottir [68] | 2015 | 1150 | Chronic Lombalgia | CFQ | DAC, CAR, SCR, NSC | Nl DAC, Nl CAR, Nl NSC, Nl SCR | **Colocar como SAUDÁVEL – porque é só lombalgia (increased CAR in Low back pain) |
| Powell [67] | 2015 | 76 | Multiple Sclerosis | CFQ | DAC, CAR, SCR | ↓DAC, ↑CAR, Nl SCR | Sleep disorders excluded; adjusted for depressive symptoms; NSC not published. Multiple sclerosis had increased awakening cortisol and decreased CAR |
| Cruz [70] | 2015 | 43 | Breast cancer | BFI and CFQ | MSC, DHEA-S | Nl MSC, Nl DHEA-S | Pts undergoing ChTx included anthracyclines |
| Marchand [31] | 2014 | 1043 | H/B | Maslach | DAC, CAR, SCR, NSC | ↑DAC, ↓CAR, ↑SCR, ↓NSC | Only BO; Groups of severe distress or depression not included |
| Aggarwal [30] | 2014 | 227 | Healthy | CFQ | MSC, NSC, 0.25 mg DST, DHEA-S | Nl MSC, Nl NSC, Nl 0.25 mg DST, ↓DHEA-S | Evaluation of chronic, widespread pain, chronic orofacial pain, chronic fatigue (but not CFS), irritable bowel syndrome |
| Tell D [71] | 2014 | 130 | Breast cancer | MFI | DAC, CAR, SCR, NSC | ↓CAR, ↓SCR, ↑DAC, ↑NSC | Post-surgery breast cancer, regardless of ChTx. Not adjusted to sleeping patterns |
| Wolfram [32] | 2013 | 53 | H/B | Maslach | MSC, 1 mcg CST, DST/CRH test (1.5 mg DST + 100 mcg CRH) | Nl MSC, ↓post-1 mcg ACTH, Nl ACTH and cortisol DST-CRH | High over-commitment present blunted serum and salivary cortisol and ACTH responses to DST-CRH test |
| Klaassen [33] | 2013 | 27 | Healthy | MP (Beck & Luine, 2010) and Stress Tasks (Wang, 2006) | MSC, post-stress | Nl MSC, Nl post-stress | A complex test sequence was performed but not reproduced |
| Eek [34] | 2012 | 581 | Healthy | SOFI-20 | DAC, CAR, NSC, SCR, MSC | Nl DAC, Nl CAR, Nl NSC, Nl SCR, Nl MSC | Women: reduced awakening, increased CAR, increased SCR; Men: increased awakening and reduced CAR – when fatigued |
| Sjors [35] | 2012 | 247 | H/B | DCSRD and SMBQ | DAC, 15 min CAR | Nl DAC, Nl 15 min CAR | |
| Rahman [54] | 2011 | 30 | CFS | Previous Dx – No questionnaire | MSC, SCR, NSC | Nl MSC, Nl SCR, Nl NSC | |
| Moya-Albiol [37] | 2010 | 64 | H/B | Maslach | DAC, CAR | Nl DAC, Nl CAR | |
| Kumari [38] | 2009 | 4,299 | Healthy | SF-36 | DAC, CAR, NSC, SCR | ↓DAC, ↓CAR, ↑NSC, ↓SCR | Adjusted for WC, BMI, sleep duration, CVD medication, depressive symptoms, smoking, alcohol intake provides Nl awakening but lower SCR |
| Osterberg [39] | 2009 | 304 | H/B | Maslach | DAC, CAR, NSC, SCR | Nl DAC, Nl CAR, ↓NSC, ↑SCR | 0.5 mg DST was not compared to controls |
| Wingenfeld [41] | 2009 | 279 | H/B | Maslach and Maastricht | AUC, SCR | Nl AUC, Nl SCR | DAC and CAR not done; conclusions different from results. For AUC, Low BO: Nl, moderate: increased, severe: decreased |
| Rydstedt [40] | 2009 | 76 | Healthy | NRWS | DAC, NSC | Nl DAC, Nl NSC | |
| Papadopoulos [55] | 2009 | 38 | CFS | CFQ and SF-36 | MSC, AUC, morning AUC, 0,5 mg DST | ↑MSC, ↑AUC, ↑MAUC, Nl 0.5 mg DST | Data on absolute cortisol levels at each point not published. DST reduction evaluated by percent reduction. |
| Bay [72] | 2009 | 75 | Post traumatic brain injury | POMS | AUC | Nl AUC | Correlation between brain injury-related fatigue level and cortisol AUC. Basal and NSC results not reported; SCR not evaluated. |
| Sudhaus [73] | 2009 | 43 | Chronic Lombalgia | MFI | DAC, CAR, MAUC | ↓CAR, Nl DAC, Nl MAUC (correlation between fatigue levels among low back pain subjects) | |
| Lindeberg [36] | 2008 | 78 | Healthy | SF-36 | DAC, CAR, NSC, SCR | Nl DAC, ↓CAR, Nl NSC, ↓SCR | |
| Sertoz [42] | 2008 | 72 | H/B | Maslach | Basal and post 1.0 mcg DST cortisol | Nl basal cortisol and 1.0 mg DST | |
| Bellingrath [43] | 2008 | 101 | H/B | Maslach and Maastricht | DAC, CAR, NSC, SCR, 0.25 mg DST | Nl DAC, Nl CAR, Nl NSC, Nl SCR, ↓0.25 mg DST | |
| Nater [57] | 2008 | 185 | CFS | SF-36 and MFI | DAC, CAR, MAUC | Nl DAC, Nl CAR, ↓MAUC | |
| Torres-Harding [56] | 2008 | 108 | CFS | FSE | AUC, SCR | Nl AUC, Nl SCR | Multiple psychological tests performed. Data on NSC, basal and CAR not published. |
| Sonnenschein [45] | 2007 | 42 | H/B | Maslach | CAR, 0.5 mg DST, DHEA-S | Nl CAR, Nl 0.5 mg DST, Nl DHEA-S | Adjusted for depression, sleep quality. Awakening levels and each level graphics not available |
| Harris [44] | 2007 | 44 | Healthy | SF-36 | DAC, CAR, NSC, SCR | Nl DAC, Nl CAR, Nl NSC, Nl SCR | Other aspects also correlated: complains, job stress and demand, QOL and coping. Adjusted for coffee and tobacco. |
| Langelaan [46] | 2006 | 55 | H/B | Maslach | DAC, CAR, 0.5 mg DST, DHEA-S | Nl DAC, Nl CAR, Nl 0.5 mg DST, Nl DHEA-S | Engaged work also compared and had stronger suppression in DST |
| Mommersteeg [47] | 2006 | 109 | Healthy | NC-WHO | DAC, CAR, 0.5 mg DST, SCR, AUC, NSC | Nl DAC, Nl CAR, Nl NSC, Nl SCR, Nl 0.5 mg DST, Nl AUC | |
| Barroso [74] | 2006 | 40 | HIV | HRFS | MSC, NSC | ↓MSC, ↑NSC | |
| Jerjes [58] | 2006 | 80 | CFS | CFQ | UFC, TCM | ↓UFC, Nl TCM | |
| Grossi [48] | 2005 | 64 | H/B | SMBQ | DAC, CAR | ↓DAC, ↑CAR | Groups were high x moderate x low BO score; correlation was significant |
| Segal [59] | 2005 | 40 | CFS | No questionnaire | MSC, 1 mcg CST | ↓ MSC, ↓1 mcg CST | DHEA-S collected only in CFS. No questionnaires used. |
| Jerjes [60] | 2005 | 35 | CFS | CFQ | MSC, SCR, NSC, AUC | ↓MSC, ↓SCR, ↓AUC ↓, Nl NSC | |
| Bower [75] | 2005 | 29 | Breast cancer | SF-36 | DAC, AUC, SCR, NSC | ↑AUC, ↓SCR, Nl DAC, ↑NSC | Post-ChTx (regardless of time) complete cancer remission and exclusion of other disorders |
| McLean [76] | 2005 | 55 | Fybro-mialgia | SF-36 | DAC, 60 min CAR, SCR, AUC, NSC | Nl DAC, Nl 60 min CAR, Nl SCR, Nl AUC, Nl NSC (correlation between fatigue levels among FMG subjects) | FMG subjects presented Nl DAC and CAR, as controls. |
| Roberts [62] | 2004 | 92 | CFS | CFQ and SF-36 | DAC, CAR, MAUC | Nl DAC, ↓CAR, ↓MAUC | |
| Crofford [61] | 2004 | 72 | CFS/FMG | POMS | ACTH, MSC, SCR, NSC, AUC | Nl ACTH, Nl SCR, Nl NSC, ↓AUC, Nl MSC | Tests performed in: CFS, FMG and CFS + FMG; FMG w/o fatigue had Nl AUC and increased BMC levels |
| Moch [50] | 2003 | 16 | H/B | Maslach | UFC, DHEA-S, ACTH, MSC | ↓UFC, Nl DHEA-S, Nl ACTH, ↓MSC | Only women; longitudinal evaluation – Nl initial cortisol. |
| De Vente [49] | 2003 | 45 | H/B | Maslach | DAC, MSC, post-TSST | ↑DAC, ↑MSC, Nl post-TSST | |
| Gaab [63] | 2002 | 42 | CFS | MFI | DAC, CAR, SCR, 0.5 mg DST | ↓0.5 mg DST, Nl AUC, Nl CAR, Nl DAC, Nl SCR, Nl NSC | CAR also performed at 15, 45 and 60 min. |
| Dekkers [77] | 2000 | 53 | Rheumatoid Arthritis | MFI | DAC, CAR, SCR, AUC | Nl AUC, Nl SCR Nl, ↓DAC, ↑CAR | 5/25 subjects with RA taking prednisone (5–10 mg/d); RS subjects had smaller SCR, increased AM cortisol and decreased CAR. 15 and 45 min CAR also performed. |
| Melamed [51] | 1999 | 111 | H/B | SMBQ and Maastricht | MSC and 4 PM cortisol | ↑MSC, Nl 4 PM cortisol | |
| Pruessner [52] | 1999 | 66 | Healthy | Maslach | DAC, CAR, 0.5 mg DST | ↓DAC, ↓CAR, ↓0.5 mg DST | 15 min and 60 min CAR also performed |
| Strickland [65] | 1998 | 74 | CFS | Not specified/detailed | MSC, NSC | ↓NSC, Nl MSC | Adjusted for depression |
| Young [66] | 1998 | 45 | CFS | NC-WHO | UFC, SCR, MSC, AUC | Nl UFC, Nl SCR, Nl MSC, Nl AUC | |
| Scott [64] | 1998 | 28 | CFS | Not specified (not detailed) | MSC, ACTH, 100 mcg CRH cortisol stimulation | Nl MSC, Nl ACTH, CRH stim test: ↓cortisol, ↓ACTH | |
| Raikkonen [53] | 1996 | 22 | Healthy | Not assessed | 1 mcg CST, DST (non specified), OGTT, MSC, ACTH, cortisol/ACTH ratio | ↑Cortisol/ACTH ratio; ↑CST, Nl DST, Nl OGTT, Nl MSC, Nl ACTH | Full article not assessed – not in PUBMED or other database |
Questionnaires: SMBQ shirom-melamed burnout questionnaire, BFI brief fatigue inventory, CFQ chalder fatigue questionnaire, Maslach maslach burnout inventory, SF-36 short form health survey 36, NC - WHO neurasthenia criteria, DCSRD diagnosis criteria of stress-related exhaustion disorder, SEQ stress-energy questionnaire, ADAS, abbreviated dyadic adjustment scale, MFI multidimensional fatigue inventory, FAQ fatigue assessment questionnaire, MP memory performance, POMS profile of mood states, Stress Tasks, FSE fatigue severity scale, SOFI Swedish occupational fatigue inventory, Maastricht Maastricht vital exhaustion questionnaire, NRWS need for recovery from work scale, HRFS HIV-related fatigue scale, WC waist circumference
Other abbreviations: CFS chronic fatigue syndrome, H / B healthy/burnout, 24 h-UFC 24-h urinary free cortisol, FMG fibromyalgia; ↑: Increased or elevated; ↓: Decreased or reduced; →: Unchanged; Nl: Normal
Study characteristics
Among the 58 studies included, 33 (56.9 % of the selected studies) were performed in healthy subjects [21–53], since we considered “burnout” not an actual disorder but instead a stressful condition presented by some groups of health workers. Despite the several studies describing cortisol impairment in Chronic Fatigue Syndrome (CFS), only 13 (22.4 %) studies performed an actual assessment of the hypothalamic–pituitary–adrenal (HPA) axis [54–66]. Twelve studies (20.7 %) were found in which tests for cortisol profiling were performed for other diseases [67–77]. However, for analysis purposes, one study [69] was divided into two studies as it performed two distinct protocols at different moments. Among these, five were done performed in patients with a diagnosis of breast cancer who had undergone or were undergoing chemotherapy. One study tested patients with fibromyalgia, two studies compared patients with chronic lower pain, one with rheumatoid arthritis, one with post brain injury, two with multiple sclerosis, and one involved patients with human immunodeficiency virus (HIV) and CFS. One study evaluated both patients with fibromyalgia and patients with CFS in different groups.
The median number of tested subjects in the 58 studies was 72 (range: 16–4,299). The median numbers of participants in articles involving healthy individuals, patients with CFS, or patients with other diseases were 76 (16–4,299), 45 (28–185), and 65 (29–1150), respectively. The largest number of healthy subjects included groups of workers whose cortisol results were compared to exhaustion and fatigue status, in an attempt to discriminate correlations between cortisol and energy levels. One study involving 4,299 individuals was responsible for more subjects than the sum of all the other studies.
Methods used to evaluate fatigue in the general study population
Some authors utilized more than one method to compare the different patients and were included in multiple groups. A summary of all the methods used to assess fatigue, and their results, is shown in Table 2. Among the 58 studies, 27 (46.6 %) utilized the Cortisol Awakening Response (CAR) to assess the HPA axis. This method is based on previous studies [77–81] that indicate cortisol levels rise by 50 % on average within 30 min of waking as a physiological response to stay alert, with a blunted CAR resulting in fatigue symptoms. For the CAR, salivary cortisol is collected immediately on waking (t = 0) and again 30 min later (t = 30), and the difference (delta cortisol) between the two measurements are analyzed. Among the 27 studies that employed CAR, fourteen (51.9 %) showed a normal response, nine (23.3 %) had a diminished delta cortisol, and four (14.8 %) demonstrated an increased delta cortisol.
Table 2.
Assessed methods and results of all selected studies (N = 58)
| Procedure (*) | Number of studies (% of total) | Not different (%) | Decreased (%) | Increased (%) |
|---|---|---|---|---|
| DAC | 29 (50.0 %) | 19 (65.5 %) | 6 (20.7 %) | 4 (13.8 %) |
| CAR | 27 (46.6 %) | 14 (51.9 %) | 9 (33.3 %) | 4 (14.8 %) |
| SCR | 26 (44.8 %) | 16 (61.5 %) | 7 (26.9 %) | 3 (11.5 %) |
| MSC | 22 (37.9 %) | 14 (63.6 %) | 4 (18.2 %) | 4 (18.2 %) |
| NSC | 22 (37.9 %) | 13 (59.1 %) | 3 (13.6 %) | 6 (27.3 %) |
| AUC | 13 (22.4 %) | 8 (61.5 %) | 3 (23.1 %) | 2 (15.4 %) |
| DST | 9 (15.5 %) | 6 (66.7 %) | 3 (33.3 %) | - |
| DHEA-S | 6 (10.3 %) | 4 (66.7 %) | 2 (33.3 %) | - |
| ACTH | 6 (10.3 %) | 5 (83.3 %) | - | 1 (16.7 %) |
| MST | 5 (8.6 %) | 4 (80.0 %) | 1 (20.0 %) | - |
| UFC | 3 (5.2 %) | 1 (33.3 %) | 2 (66.7 %) | - |
| CST | 3 (5.2 %) | - | 2 (66.7 %) | 1 (33.3 %) |
| MAUC | 3 (5.2 %) | - | 2 (66.7 %) | 1 (33.3 %) |
| CAR 60 min | 2 (3.4 %) | 2 (100 %) | - | - |
| ACTH MST | 2 (3.4 %) | 2 (100 %) | - | - |
| 4 PM cortisol | 1 | 1 | - | - |
| DST + CRH cortisol | 1 | 1 | - | - |
| DST + CRH ACTH | 1 | 1 | - | - |
| CAR 15 min | 1 | 1 | - | - |
| TCM | 1 | 1 | - | - |
| DHEA-S MST | 1 | - | 1 | - |
| CRST cortisol | 1 | - | 1 | - |
| CRST ACTH | 1 | - | 1 | - |
| OGTT cortisol | 1 | - | - | 1 |
| Cortisol/ACTH ratio | 1 | - | - | 1 |
Legends: (*): DAC direct awakening cortisol, CAR cortisol awakening response, SCR salivary cortisol rhythm, MSC morning serum (& salivary) cortisol, NSC night salivary cortisol, AUC area under-the-curve (Estimated Cortisol Release), DST dexamethasone suppression test, DHEA - S dehydroepiandrosterone sulfate, ACTH adrenocorticotropic hormone, MST mental stress test, UFC 24 h-urinary free cortisol, CST cosyntropin stimulation test, MAUC morning area under-the-curve (morning estimated cortisol release), CRH corticotropin releasing hormone, TCM total urinary cortisol metabolites, CRST corticotropin releasing stimulation test (?), OGTT oral glucose tolerance test
Another method that became widely used to evaluate exhaustion/burnout/fatigue states is the salivary cortisol rhythm (SCR), which evaluates the change in cortisol levels between morning, afternoon, and late night. A total of 26 studies evaluated SCR (44.8 %). Some heterogeneity in the method was found between studies, but in general, salivary cortisol was collected at 8 AM, 4 PM, and 10–11 PM. While the SCR is considered as another fatigue marker [82, 83], like the CAR, there is no justification for considering this as an etiology for “adrenal fatigue”. Sixteen (61.5 %) studies showed no difference between fatigued and control patients, whereas seven (26.9 %) demonstrated an impaired decrease in the circadian SCR. The remaining three (11.6 %) studies disclosed a more pronounced decrease in cortisol level.
The direct awakening cortisol (DAC) level, collected at the exact moment of waking, was used in 29 studies (50.0 %). Unlike CAR, DAC reflects sleep quality rather than being a possible identifying factor of fatigue [84–86], even though a poor quality sleep plays an important role in the fatigue process [87–89]. In studies that employed DAC, inconsistent results were observed: normal results were found in nineteen (65.5 %) studies, elevated levels were shown in four (13.8 %), and reduced levels in six (20.7 %).
The DAC, CAR and SCR methods were by far the most commonly elected ones for examining the correlation between cortisol profile and fatigue status. However, a few other studies analyzed other aspects of cortisol release.
The dexamethasone (Dex) suppression test (DST) was also used in nine (15.3 %) studies. The DST identifies autonomous hypercortisolism, as cortisol production is normally suppressed by Dex. DSTs have also been used to investigate hypocortisolism, based on the supposed assumption that it promotes “oversuppression” of cortisol in low cortisol states, indicating that lower levels of cortisol would disclose a more prolonged suppression than controls [55, 90–93], although many studies do not show correlation between DST and fatigue [47, 55, 94, 95]. In six studies, a lower Dex dose (0.5 mg) was used in an attempt to improve the test sensitivity. Among these, four studies (66.7 %) showed the same results for both groups, whereas in two others (33.3 %), the test resulted in lower and prolonged suppression of cortisol levels in fatigued subjects. Moreover, an even lower Dex dose (0.25 mg) was performed in two studies and resulted in reduced cortisol in one study and normal levels in the group with exhaustion. In one study, Dex dose was not specified, but levels were not different among exhausted and control groups. As a whole, the DST was used in nine studies, and no significant differences were observed between fatigued and non-fatigued groups in six of these studies (66.7 %), whereas reduced levels were observed in three studies (33.3 %).
Adrenocorticotropic hormone (ACTH) is a pituitary peptide hormone that stimulates cortisol production by the adrenocortical zona fasciculata. Elevated ACTH occurs early in primary adrenal insufficiency, whereas inappropriate (normal) ACTH levels in the presence of low serum cortisol are found in secondary adrenal failure. Although, normal ACTH levels with normal cortisol levels does not exclude the possibility of relative adrenocortical failure. Six (10.3 %) studies employed the morning ACTH levels to compare fatigued and non-fatigued patients; no significant differences for ACTH, as well as for cortisol, were found in five studies (83.3 %), meanwhile one showed elevated ACTH levels in burnout patients (16.7 %).
On the other hand, three studies (5.2 %) used the low-dose cosyntropin (a synthetic 1-24ACTH) stimulation test (CST), in which 1 μg of cosyntropin is used instead of the classic 250 μg dose, based on the premise that the CST is more accurate and sensitive for verifying the adrenocortical cortisol reserve [96], even though most findings indicate that both doses have similar accuracy [97, 98]. Surprisingly, one of three (33.3 %) studies disclosed a paradoxically higher cortisol increase compared to controls, while in two (66.7 %) lower levels were observed. Conversely, impaired cortisol and ACTH responses was observed in the fatigued group in a single study in which corticotropin-releasing hormone (CRH) was used to stimulate the HPA axis.
Three (5.2 %) studies measured 24 h-urinary free cortisol (UFC) in an attempt to correlate cortisol excretion rates with intensity of fatigue. Although the 24 h-UFC reflects the total cortisol produced per day, it was initially conceived to investigate cortisol excess syndromes, although diminished levels could hypothetically imply subnormal adrenal function, despite of lack of any evidence. One of these studies (33.3 %) found no correlation between 24 h-UFC and energy status, whereas two studies (66.7 %) showed reduced values in fatigued patients.
Thirteen studies (22.4 %) estimated total cortisol release (AUC) by calculating the areas under the curves for the whole day salivary cortisol collection by using three or more daily salivary cortisol levels over four or more days. Assessment of the total 24 h cortisol release by this method would complement the SCR, since the lack of the expected decrease throughout the day observed in some studies can be due either to a non-elevated morning serum cortisol (MSC) level or to a full day elevated cortisol, although three daily levels of cortisol is probably too few for a minimally precise AUC; herein, findings are conflicting. AUC was elevated in two (15.4 %) studies, normal in eight (61.5 %), and reduced in another three (23.1 %).
Twenty-two studies (37.9 %) compared baseline MSC between controls and fatigued patients; traditionally [98], this is the initial cortisol assessment to investigate possible hypocortisolism. Basal MSC was not different between individuals in fourteen (63.6 %) of these studies, was significantly reduced in fatigued patients in three (23.1 %), and was elevated in two (15.4 %).
Twenty-two articles (37.9 %) correlated late night salivary cortisol (11 PM NSC) and fatigue status. The NSC was initially validated to assess cortisol excess, as physiologically, one expects lower cortisol levels at the end of the day; although, NSC has been extended to investigate hypocortisolism in these studies, despite of lack of validation. Three studies (13.6 %) showed a lower cortisol level in fatigued subjects compared to controls, thirteen (59.1 %) found no differences, and six (27.3 %) showed increased levels in fatigued subjects.
Six studies (10.3 %) investigated the correlation between dehydroepiandrosterone sulfate (DHEA-S) levels and fatigue status. Reduced DHEA-S levels are usually found in hypocortisolism and are a potential marker of fatigue, although there is still not enough evidence to corroborate this affirmation. Four studies (66.7 %) found no correlation with DHEA-S, whereas two (33.3 %) found lower levels in chronic exhausted patients.
The morning estimated total cortisol release (MAUC) is obtained by calculating the area under the curves for the period between the awakening moment and 1 hour later, and is based on determining three or more salivary cortisol levels during this period of the day, although this method has also not been validated by any indexed study. A total of four studies (6.9 %) among the selected studies reported the MAUC. Two of these studies (50.0 %) showed reduced MAUC levels in fatigued subjects, one demonstrated increased results (25.0 %), and one demonstrated no differences (25.0 %).
Mental stress tests (MST) have been performed in some studies in order to identify possible differences in cortisol and ACTH release between fatigued and non-fatigued individuals. The most employed test was the Trier Social Stress Test (TSST), which has been already validated as a stress trigger test [99–102], and requires complete HPA axis integrity for a proper response. Other types of MSTs have also been proposed and validated [103, 104]. MSTs were performed in five different studies in order to correlate cortisol and ACTH responses and burnout status. No difference was seen in four studies (80.0 %), whereas in one (20.0 %), cortisol and ACTH responses were impaired in exhausted individuals.
Some other tests were performed in a smaller number of the selected studies, as follows: two studies performed a 60 min CAR (both showed normal results among fatigued and non-fatigued subjects); one study performed a 15 min CAR (and showed normal results); two studies performed the ACTH MST (both used the TSST and found normal results); one study performed the DHEA-S MST (which also used the TSST and demonstrated normal results); one study performed the cortisol post Oral Glucose Tolerance Test (OGTT) (and found no differences among fatigued and non-fatigued subjects); one study calculated cortisol/ACTH ratio (and found an increased ratio among exhausted subjects); one study evaluated the 4 PM cortisol level (and found no significant differences between exhausted subjects and controls); one study used 1.5 mg-Dex followed by 0.1 mg-CRH to stimulate cortisol and ACTH (and showed normal responses); one study stimulated ACTH and cortisol with 0.1 mg of CRH (and found reduced levels of both hormones in fatigued subjects compared to controls); and finally, one study evaluated the multiple urinary cortisol metabolites and calculated the Total Cortisol Metabolites (TCM) (and found no differences between fatigued subjects and controls).
Finally, we were not able to find studies in which the gold standard test for assessing the integrity and functionality of the HPA axis—the insulin tolerance test (ITT)—were performed. The same was true for the lipopolysaccharides (LPS) stimulation test. Both tests stimulate hypothalamic CRH secretion, leading to a complete evaluation of the HPA axis.
Fatigue in burnout syndrome
Burnout syndrome or clinical burnout, or simply “burnout”, refers to a decrease in the cognitive functions, emotional exhaustion, and physical fatigue that is triggered by stressful situations associated with excessive working [105]. However, there is no pathognomonic marker for burnout [105]. For practical purposes, we considered non-CFS burnout patients as “healthy”, as burnout is yet to be considered a disease and its characterization is still heterogeneous. A summary of the performed methods and their respective results in non-CFS burnout/healthy patients [21–53] are shown in Table 3. Assessment of the HPA axis integrity in burnout patients (at the pituitary and hypothalamic levels) has not been determined.
Table 3.
Studies in Burnout syndrome and healthy subjects (N = 33): Methods of assessment and respective results
| Procedure | Number of studies (% of total) | Not different (%) | Decreased (%) | Increased (%) |
|---|---|---|---|---|
| DAC | 17 (51.5 %) | 10 (58.8 %) | 4 (23.5 %) | 3 (17.7 %) |
| CAR | 16 (48.5 %) | 9 (56.2 %) | 6 (37.5 %) | 1 (6.3 %) |
| MSC | 12 (36.4 %) | 8 (66.7 %) | 1 (8.3 %) | 3 (25.0 %) |
| SCR | 12 (36.4 %) | 7 (58.3 %) | 3 (25.0 %) | 2 (16.7 %) |
| NSC | 10 (30.3 %) | 7 (70.0 %) | 2 (20.0 %) | 1 (10.0 %) |
| DST | 7 (21.2 %) | 5 (71.4 %) | 2 (28.6 %) | - |
| MST | 5 (15.2 %) | 4 (80.0 %) | 1 (20.0 %) | - |
| DHEA-S | 5 (15.2 %) | 3 (60.0 %) | 2 (40.0 %) | - |
| ACTH | 4 (10.1 %) | 3 (75.0 %) | - | 1 (25.0 %) |
| AUC | 3 (9.1 %) | 2 (66.7 %) | 1 (33.3 %) | - |
| ACTH MST | 2 (6.1 %) | 2 (100 %) | - | - |
| CST | 2 (6.1 %) | - | 1 (50 %) | 1 (50 %) |
| 4 PM cortisol | 1 | 1 | - | - |
| DST + CRH cortisol | 1 | 1 | - | - |
| DST + CRH ACTH | 1 | 1 | - | - |
| CAR 15 min | 1 | 1 | - | - |
| CAR 60 min | 1 | 1 | - | - |
| DHEA-S MST | 1 | - | 1 | - |
| UFC | 1 | - | 1 | - |
| OGTT cortisol | 1 | - | - | 1 |
| Cortisol/ACTH ratio | 1 | - | - | 1 |
Legends: (*): DAC direct awakening cortisol, CAR cortisol awakening response, MSC morning serum (& salivary) cortisol, SCR salivary cortisol rhythm, NSC night salivary cortisol, DST dexamethasone suppression test, MST mental stress test, DHEA - S dehydroepiandrosterone sulfate, ACTH adrenocorticotropic hormone, AUC area under-the-curve (estimated cortisol release), CST cosyntropin stimulation test, CRH corticotropin releasing hormone, UFC 24 h-urinary free cortisol, OGTT oral glucose tolerance test
Fatigue in chronic fatigue syndrome
CFS is a diagnosis used for patients who present severe fatigue for more than six months, not explained by any hormonal, metabolic, inflammatory, or other disorders. Correlations between CFS and the HPA axis have been studied [54–66] and the results are shown in Table 4.
Table 4.
Studies in Chronic Fatigue Syndrome (N = 13): Methods of assessment and respective results
| Procedure | Number of studies (% of total) | Not different (%) | Decreased (%) | Increased (%) |
|---|---|---|---|---|
| MSC | 8 (61.5 %) | 5 (62.5 %) | 2 (25.0 %) | 1 (12.5 %) |
| SCR | 6 (46.2 %) | 5 (83.3 %) | 1 (16.7 %) | - |
| AUC | 6 (46.2 %) | 3 (50.0 %) | 2 (33.3 %) | 1 (16.7 %) |
| NSC | 5 (38.5 %) | 4 (80.0 %) | 1 (20.0 %) | |
| DAC | 3 (23.1 %) | 3 (100.0 %) | - | - |
| CAR | 3 (23.1 %) | 2 (66.7 %) | 1 (33.3 %) | - |
| ACTH | 2 (15.4 %) | 2 (100.0 %) | - | - |
| DST | 2 (15.4 %) | 1 (50.0 %) | 1 (50.0 %) | - |
| UFC | 2 (15.4 %) | 1 (50.0 %) | 1 (50.0 %) | - |
| CST | 1 (7.7 %) | - | 1 (100.0 %) | - |
Legends: (*): MSC morning serum (& salivary) cortisol, SCR salivary cortisol rhythm, AUC area under-the-curve (estimated cortisol release), NSC night salivary cortisol, DAC direct awakening cortisol, CAR cortisol awakening response, ACTH adrenocorticotropic hormone, DST dexamethasone suppression test, UFC 24 h-urinary free cortisol, CST cosyntropin stimulation test
Fatigue in other disorders
Complaints regarding fatigue not entirely explained by the underlying pathophysiology of the disease have been observed in patients suffering from other disorders, such as chronic low back pain [106, 107], breast cancer survivors [108–110], and HIV [111, 112]. Therefore, the role of the HPA axis in the etiology of fatigue in these subjects has been analyzed [67–77] and the findings are presented in Table 5.
Table 5.
Studies in Other Disorders (N = 12): Methods of and respective results
| Procedure | Number of studies (% of total studies) | Not different (%) | Decreased (%) | Increased (%) |
|---|---|---|---|---|
| DAC | 9 (75.0 %) | 6 (66.7 %) | 2 (22.2 %) | 1 (11.1 %) |
| SCR | 8 (66.7 %) | 4 (50.0 %) | 3 (37.5 %) | 1 (12.5 %) |
| CAR | 8 (66.7 %) | 3 (37.5 %) | 2 (25.0 %) | 3 (37.5 %) |
| NSC | 7 (58.3 %) | 2 (28.6 %) | - | 5 (71.4 %) |
| AUC | 4 (33.3 %) | 3 (75.0 %) | - | 1 (25.0 %) |
| MSC | 2 (16.7 %) | 1 (50.0 %) | 1 (50.0 %) | - |
| DHEA-S | 1 (8.3 %) | 1 (100.0 %) | - | - |
Legends: (*): DAC direct awakening cortisol, SCR salivary cortisol rhythm, CAR cortisol awakening response, NSC night salivary cortisol, AUC area under-the-curve (estimated cortisol release), MSC morning serum (& salivary) cortisol, DHEA - S Dehydroepiandrosterone sulfate
Questionnaires for fatigue assessment
Among all studies included in this review, nineteen different types of questionnaires and scores were reported. The most commonly used were: the Maslach Burnout Inventory (MBI, n = 15), SF-36 (n = 9), the Chalder Fatigue Scale (CFS, n = 8), the General Fatigue Scale of the Multidimensional Fatigue Inventory (MFI, n = 6) and the Shirom Melamed Burnout Questionnaire (n = 6). In ten studies, more than one type of survey was performed. In four studies, the methods to assess fatigue were not specified or assessed. A summary of the assessed questionnaires is shown in Table 6.
Table 6.
Assessed questionnaires employed in the selected studies (N = 58)
| Questionnaire | General | Healthy/Burnout | CFS | Other diseases |
|---|---|---|---|---|
| Maslach Burnout Inventory | 15 (25.7 %) | 15 | - | - |
| SF-36 -Short Form Health Survey 36 | 9 (15.5 %) | 4 | 3 | 2 |
| CFQ -Chalder Fatigue Questionnaire | 8 (13.8 %) | 1 | 4 | 3 |
| SMBQ - Shirom-Melamed Burnout Questionnaire | 6 (10.3 %) | 6 | - | - |
| MFI -Multidimensional Fatigue Inventory | 6 (10.3 %) | - | 2 | 4 |
| DCSRD: Diagnosis criteria of stress-related exhaustion disorder | 3 (5.2 %) | 3 | - | - |
| Maastricht Vital Exhaustion Questionnaire | 2 (3.4 %) | 2 | - | - |
| FAQ -Fatigue Assessment Questionnaire | 2 (3.4 %) | - | - | 2 |
| NC-WHO -Neurasthenia Criteria | 2 (3.4 %) | 1 | 1 | - |
| POMS -Profile of Mood States | 2 (3.4 %) | - | 1 | 1 |
| SOFI -Swedish Occupational Fatigue Inventory | 1 | 1 | - | - |
| ADAS -Abbreviated Dyadic Adjustment Scale | 1 | 1 | - | - |
| SEQ -Exclusion with Stress-Energy Questionnaire | 1 | 1 | - | - |
| MP -Memory performance | 1 | 1 | - | - |
| Stress Tasks | 1 | 1 | - | - |
| NRWS - Need for Recovery from Work Scale | 1 | 1 | - | - |
| FSE -Fatigue Severity Scale | 1 | - | 1 | - |
| HRFS -HIV-related Fatigue Scale | 1 | - | - | 1 |
| BFI: Brief Fatigue Inventory | 1 | - | - | 1 |
| More than one questionnaire | 10 (17.2 %) | 6 | 3 | 1 |
| Stress tests | 5 (8.6 %) | 5 | - | - |
| Not specified | 4 (6.9 %) | - | 4 |
Legends: Maslach maslach burnout inventory, SF-36 short form health survey 36, CFQ chalder fatigue questionnaire, SMBQ shirom-melamed burnout questionnaire, MFI multidimensional fatigue inventory, DCSRD diagnosis criteria of stress-related exhaustion disorder, Maastricht Maastricht vital exhaustion questionnaire, FAQ fatigue assessment questionnaire, NC - WHO neurasthenia criteria, POMS profile of mood states, SOFI Swedish occupational fatigue inventory, ADAS abbreviated dyadic adjustment scale, SEQ stress-energy questionnaire, MP memory performance, Stress Tasks; NRWS need for recovery from work scale, FSE fatigue severity scale, HRFS HIV-related fatigue scale, BFI brief fatigue inventory
Discussion
Theories on adrenal impairment as the genesis for fatigue are tempting, as they allow for a treatable condition. Despite the widespread use of the term “adrenal fatigue” by the general media and certain health practitioner groups, in this systematic review, only ten citations [113–122] were found with this exact expression, and they were all only descriptive and did not perform any test regarding the HPA axis and “adrenal fatigue”. Studies that tried to correlate the HPA axis and fatigue states used the term “burnout” instead of “adrenal fatigue” to denote adrenal depletion. Therefore, a distinction between the “general information” and the actual scientific literature regarding this condition is evident. First, this suggests that the terminology of a hypothetical adrenal depletion should be normalized, with a suitable name given for the purported condition, as “adrenal fatigue” has been already been stigmatized and lacks proper scientific support. Second, methodology employed to evaluate the proposed correlation between fatigue and adrenal function should be standardized among physicians and medical associations that claim for the existence of adrenal impairment in patients with fatigue before evident clinical hypocortisolism manifests, in order to strength eventual evidence, in case one finds actual and proper causal correlation.
No confirmed methods of clinical screening for AF are available. Indeed, the popular questionnaire developed by Dr. Wilson and published in the first book exclusively dedicated to the description of this supposedly disease [6] has not been cited in any indexed databases. Another theory, the “Thompson cortisol hypothesis” [123], suggests that cortisol is responsible for yawning and fatigue; however, again, no studies that tested this theory have been published in indexed journals. Validated surveys have been used in studies that investigate fatigue states, but they were not correlated with proper cortisol assessment methods. The TSST is the only survey to have enough credibility to be officially tested and standardized as a trigger of stress [99–102].
Functional tests are the only methods to assess adrenal cortisol production endorsed by endocrinology societies [97]. Although, the ITT is considered the gold standard test to evaluate the entire HPA axis, neither the ITT (or the similar LPS stimulation test) was performed in any studies investigating the correlation between fatigue states and adrenocortical function. Moreover, we generally found conflicting data using most of the functional tests when trying to differentiate exhausted, fatigued, and burnout individuals from healthy patients. For example, using the low-dose CST, we found an unexpected increase in cortisol levels in fatigued subjects in the selected studies. This may have been perhaps the result of a relative secondary adrenal insufficiency, which leads to an amplified adrenal cortisol response due to an upregulation of ACTH receptors, but this sounds unjustifiable since the lack of continuous stimulation of the adrenal cortices would cause atrophy, rendering them non-responsive to a low- (and even high) dose of cosyntropin stimulation in the long run. Regardless of the theoretical explanation, CST has shown to be not a good marker of fatigue. Similarly, ACTH levels were also poorly studied and did not show significant correlations in most fatigued subjects. In addition, despite its lack of standardization, the DST was performed in nine studies, but conflicting results invalidated attempts to establish this as a new marker for fatigue states. Moreover, the 24 h-UFC has been shown to be so far inaccurate for investigation of adrenal impairment. Findings were also contradictory in the six studies that calculated cortisol AUC as well as in the four studies that performed MAUC. Therefore, the above methods cannot be used to differentiate fatigued from non-fatigued individuals.
In this review, we also examined whether cortisol markers can be used to assess cortisol impairment. The results of our review indicate that the three major tests (CAR, DAC and SCR) used to identify the underlying causes of the fatigue/exhaustion state failed to do so, since they were unable to demonstrate significant differences or proper causality. CAR and DAC frequently showed inconsistent results in studies that used heterogeneous groups of subjects. CAR and DAC are not necessarily indicatives of the etiology and pathogenesis of the fatigue status, since both can be consequences of other disorders, such as sleep disturbances. Indeed, a recent study [124] was the first to use CAR as a marker of improvement of burnout syndrome, which reinforces the use of this method for monitoring the consequences of fatigue states, but not for its etiology [77–81].
With regards to the SCR, the results may be misleading if they are not analyzed together with the total 24 h cortisol release. This is because a non-physiological blunted rhythm can be due either to an impairment of the lowering cortisol trend throughout the day or due to a lower morning cortisol level. Despite this, studies that evaluated total 24 h cortisol by measuring serial salivary cortisol levels also showed conflicting findings. Our systematic review corroborates another systematic review [83] that shows inconsistency regarding measuring methods among across different randomized controlled trials. Similarly, baseline MSC and NSC were poor markers of fatigue status as it failed to reveal any differences in burnout/exhaustion/fatigue patients compared to healthy subjects.
Adrenal size could be considered another marker of adrenal activity, as hypertrophic/hyperplastic adrenal glands could be the result of an ACTH over-stimulation by the pituitary, as seen in subjects exposed to chronic stress [125, 126], whereas a diminished or atrophic gland may reflect adrenal insufficiency at any level of the HPA axis [98]. However, not a single study could be identified in which the adrenal size has been checked in fatigued or exhausted patients. Similarly, although DHEA-S could also be a potential marker for adrenal atrophy or dysfunction, is still uncertain whether it plays any pathophysiological role in fatigue. Finally, none of the abovementioned methods were accurate markers of fatigue, nor could they be correlated with the HPA axis dysfunction as an etiology of fatigue.
It is also important to note that once adrenal impairment is confirmed using any of these tests, the etiology should also be elucidated. As the HPA axis can be affected by several chronic and/or metabolic disorders, other primary conditions must be excluded before intrinsic disorders of the HPA axis are deemed responsible. Typical differential diagnosis of “adrenal fatigue” and related states are: (1) sleep obstructive apnea syndrome; (2) adrenal insufficiency; (3) mental illnesses; (4) excessive working (overwork); (5) night-shift workers; (6) other hormonal deficiencies; (7) liver and kidney dysfunctions; (8) heart conditions; (9) chronic pulmonary obstructive disease; (10) autoimmune diseases.
Although conflicting data were reported, patients with CFS tend to have a normal cortisol profile, and the abnormalities found can be typically be explained by a poor quality sleeping patterns. Therefore, health providers should not be concerned about adrenal function in CFS subjects once they had been already excluded to other conditions prior to the diagnosis of CFS. Similarly, studies investigating patients with the burnout syndrome were greatly inconsistent So far, HPA axis tests should not be used as markers for burnout syndrome by health practitioners. Similar conclusions can be drawn for the use of HPA axis tests as markers for fibromyalgia and other chronic diseases, which tend to demonstrate inconsistent findings, whereas studies that were performed in breast cancer subjects tended to show depletion of cortisol levels; however, studies in breast cancer were performed while administering chemotherapy, which can introduce a confounding bias.
Therefore, based on our current knowledge, cortisol tests should not yet be used in clinical practice for examining any condition, except if adrenal impairment is suspected. Moreover, glucocorticoid therapy should be avoided in patients, as it can increase the risk of cardiovascular disease or osteoporosis, even in low doses.
Limitations
Some limitations of this review include: (1) our inability to perform a meta-analysis due to heterogeneity of the study design; (2) the descriptive nature of most studies, and the reporting of a condition that has not been scientifically proven without adding new data nor providing solid arguments; (3) the fact that most studies were published in low impact journals; (4) the inadequate and poor quality assessment of fatigue; (5) the use of an unsubstantiated methodology in terms of cortisol assessment; (6) the lack of concern regarding validated adrenal assessment (as endorsed by endocrinologists); (7) false premises leading to an incorrect sequence of thinking and research direction; and, (8) inappropriate/invalid conclusions regarding causality and association between different information, in particular, whether any abnormalities would be a marker or a potential target for treatment.
Final discussions
Our results corroborate an Endocrine Society warning statement regarding adrenal fatigue (1), as saying that “adrenal fatigue is not a real medical condition”. While a recent systematic review on burnout was published (109) that implicated some HPA dysfunctions as markers or triggers of burnout, there were important bias selection regarding the articles chosen. Therefore, we recommend that for further prospective studies aiming to correlate fatigue, exhaustion, or burnout status with impairment of the HPA axis, an ITT or a 250 μg CST should be performed to evaluate the adrenocortical ability to release cortisol, measurements of ACTH, DHEA-S, and corticosterone (an intermediate steroid product that is impaired earlier than cortisol [127]), the adoption of the most validated questionnaires, particularly Maslach Burnout Inventory, the Chalder Fatigue Scale, SF-36 or the General Fatigue Scale of the Multidimensional Fatigue Inventor, and considering different study populations, including: (a) healthy subjects; (b) burnout healthy subjects; (c) subjects with overtraining syndrome; (d) subjects post-chemotherapy; (e) subjects with CFS; and (f) subjects with fibromyalgia.
In addition, we do not recommend the use of the many methods reported in the articles evaluated in this systematic review, as they are not accurate to determine whether a patient has or has not adrenal failure.
The answer to whether “adrenal fatigue” or depletion exists or not may not be simple, but different answers can be offered according to the presence of an underlying disease. However, so far, there is no substantiation to show its existence.
Conclusion
To our knowledge, this is the first systematic review made by endocrinologists to examine a possible correlation between the HPA axis and a purported “adrenal fatigue” and other conditions associated with fatigue, exhaustion or burnout. So far, there is no proof or demonstration of the existence of “AF”. While a significant number of the reported studies showed differences between the healthy and fatigued groups, important methodological issues and confounding factors were apparent. Two concluding remarks emerge from this systematic review: (1) the results of previous studies were contradictory using all the methods for assessing fatigue and the HPA axis, and (2) the most appropriate methods to assess the HPA axis were not used to evaluate fatigue. Therefore, “AF” requires further investigation by those who claim for its existence.
Acknowledgements
We acknowledge the support of the adrenal team of Endocrinology Unit of Federal University of Sao Paulo: Flavia Barbosa, MD, PhD; Regina do Carmo, MD, PhD; Marcelo Vieira, MD; Rafaela Fontenele, MD and Denise Farinelle, MD, who helped giving some ideas regarding the most important aspects to be discussed in the systematic review. All them are aware of the inclusion of their names in this section.
Funding
No funding was obtained for the research for the design strategy, for collection, analysis and interpretation of data and for writing the manuscript.
Availability of data and materials
Searched studies that were not open access were assessed using CAPES/CNPq and Federal University of Sao Paulo bases, which were responsible for providing all the supplied data to all MEDLINE (Ebsco), PubMed and Cochrane databases.
Authors’ contributions
FAC performed the research and selection of the studies, analyzed the results, detailed each selected study in the Table 1, calculated the results and performed part of the discussions and conclusions. CEK participated in the design of the systematic review, including selection of the searched expressions and the databases, including and excluding criteria, quality assessmentand statistical analysis; CEK also performed part of the discussion, the conclusions and helped to organize the sequence of the systematic review. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests regarding financial and non-financial aspects.
Consent for publication
We declare that the consent for publication is not applicable to this study.
Ethics approval and consent to participate
This systematic review did not include direct human material or data, but indirectly used human subjects from the selected studies. All the selected studies were supposed to have an explicit statement of approval of an appropriate ethics committee in order to be included, as required from the ethics committee of the Federal University of Sao Paulo. Therefore, we declare that ethics approval and consent to participate is not applicable to this study.
Abbreviations
- 24 h UFC
24-h urinary free cortisol
- ACTH
Adrenocorticotropic hormone
- ADAS
Abbreviated dyadic adjustment scale
- AF
Adrenal fatigue
- AUC
Estimated cortisol release (area under the curve)
- BFI
Brief fatigue inventory
- CAR
Cortisol awakening response
- CFQ
Chalder fatigue questionnaire
- CFS
Chronic fatigue syndrome
- CST
Cosyntropin stimulation test
- DAC
Direct awakening cortisol
- DCSRD
Diagnosis criteria of stress-related exhaustion disorder
- DHEA-S
Dehydroepiandrosterone sulfate
- DST
Dexamethasone suppression test
- FAQ
Fatigue assessment questionnaire
- FMG
Fibromyalgia
- FSE
Fatigue severity scale
- H/B
Healthy/Burnout
- HRFS
HIV-related fatigue scale
- Maastricht
Maastricht vital exhaustion questionnaire
- Maslach
Maslach burnout inventory
- MFI
Multidimensional fatigue inventory
- MP
Memory performance
- MSC
morning serum cortisol (& salivary)
- MST
Mental stress tests
- NC-WHO
Neurasthenia criteria
- NRWS
Need for recovery from work scale
- NSC
Night salivary cortisol
- POMS
Profile of mood states
- SCR
Salivary cortisol rhythm
- SEQ
Exclusion with stress-energy questionnaire
- SF-36
Short form health servey 36
- SMBQ
Shirom-melamed burnout questionnaire
- SOFI
Swedish occupational fatigue inventory
- UFC
24 h Urinary free cortisol
Contributor Information
Flavio A. Cadegiani, Email: flaviounb@gmail.com
Claudio E. Kater, Email: kater@unifesp.br
References
- 1.The Endocrine Society. Hormone Health Netowrk. Hormones and Health. Myth vs Fact. Adrenal Fatigue. Available from : http://www.hormone.org/hormones-and-health/myth-vs-fact/adrenal-fatigue. Accessed 23 Aug 2016.
- 2.Association of American Medical Colleges. Careers in Medicine. List of Specialities. Avaliable from: https://www.aamc.org/cim/specialty/list/us/. Accessed 23 Aug 2016.
- 3.American Board of Medical Specialities. Avaliable fromL http://www.abms.org/. Accessed 23 Aug 2016.
- 4.The American Academy of Anti-Aging Medicine. Beyond Adrenal Fatigue: From Anedecdotal to Evidence Based Medicine. Avaliable from: http://www.a4m.com/assets/pdf/medical-news/A4M_Hypocortisolism_paper_draft_3-Final.pdf. Accessed 23 Aug 2016.
- 5.Functional Medicine Institute. Adrenal Fatigue. https://www.functionalmedicine.org/content_management/files/AFMCPSeptember2011/9_Onsite%20Course%20Materials/Thursday/Lukaczer%20Panico_Thyroid%20Dysfunction%201%20per%20page.pdf. Accessed 23 Aug 2016.
- 6.Wilson JL. Adrenal Fatigue the 21st Century Stress Syndrome. 1 2001. [Google Scholar]
- 7.The American Academy of Anti-Aging Medicine. Overview. Available from: http://www.a4m.com/about-a4m-overview.html. Accessed 23 Aug 2016.
- 8.Lotan I, Fireman L, Benninger F, Weizman A, Steiner I. Psychiatric side effects of acute high-dose corticosteroid therapy in neurological conditions. Int Clin Psychopharmacol. 2016;31(4):224–231. doi: 10.1097/YIC.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 9.Cerullo MA. Expect psychiatric side effects from corticosteroid use in the elderly. Geriatrics. 2008;63(1):15–18. [PubMed] [Google Scholar]
- 10.Kenna HA, Poon AW, Angeles CP D l, Koran LM. Psychiatric complications of treatment with corticosteroids: review with case report. Psychiatry Clin Neurosci. 2011;65(6):549–560. doi: 10.1111/j.1440-1819.2011.02260.x. [DOI] [PubMed] [Google Scholar]
- 11.Drozdowicz LB, Bostwick JM. Psychiatric adverse effects of pediatric corticosteroid use. Mayo Clin Proc. 2014;89(6):817–834. doi: 10.1016/j.mayocp.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Whittier X, Saag KG. Glucocorticoid-induced Osteoporosis. Rheum Dis Clin North Am. 2016;42(1):177–189. doi: 10.1016/j.rdc.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Gupta A, Gupta Y. Glucocorticoid-induced myopathy: Pathophysiology, diagnosis, and treatment. Indian J Endocrinol Metab. 2013;17(5):913–916. doi: 10.4103/2230-8210.117215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huscher D, Thiele K, Gromnica-Ihle E, Hein G, Demary W, Dreher R, Zink A, Buttgereit F. Dose-related patterns of glucocorticoid-induced side effects. Ann Rheum Dis. 2009;68(7):1119–1124. doi: 10.1136/ard.2008.092163. [DOI] [PubMed] [Google Scholar]
- 15.Filipsson H, Monson JP, Koltowska-Haggstrom M, Mattsson A, Johannsson G. The impact of glucocorticoid replacement regimens on metabolic outcome and comorbidity in hypopituitary patients. J Clin Endocrinol and Metab. 2006;91:3954–3961. doi: 10.1210/jc.2006-0524. [DOI] [PubMed] [Google Scholar]
- 16.McDonough AK, Curtis JR, Saag KG. The epidemiology of glucocorticoid-associated adverse events. Curr Opin Rheumatol. 2008;20(2):131–137. doi: 10.1097/BOR.0b013e3282f51031. [DOI] [PubMed] [Google Scholar]
- 17.Oray M, Abu Samra K, Ebrahimiadib N, Meese H, Foster CS. Long-term side effects of glucocorticoids. Expert Opin Drug Saf. 2016;15(4):457–465. doi: 10.1517/14740338.2016.1140743. [DOI] [PubMed] [Google Scholar]
- 18.Wei L, MacDonald TM, Walker BR. Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med. 2004;141:764–770. doi: 10.7326/0003-4819-141-10-200411160-00007. [DOI] [PubMed] [Google Scholar]
- 19.Rystedt LW, Cropley M, Devereux JJ, Michalianou G. The relationship between long-term job strain and morning and evening saliva cortisol secretion among white-collar workers. J Occup Health Psychol. 2008;13(2):105–113. doi: 10.1037/1076-8998.13.2.105. [DOI] [PubMed] [Google Scholar]
- 20.Gold SM, Kruger S, Ziegler KJ, Krieger T, Schulz KH, Otte C, Heesen C. Endocrine and immune substrates of depressive symptoms and fatigue in multiple sclerosis patients with comorbid major depression. J Neurosurg Psychiatry. 2011;82:814–818. doi: 10.1136/jnnp.2010.230029. [DOI] [PubMed] [Google Scholar]
- 21.McLennan SN, Ihle A, Steudte-Schmiedgen S, Kirschbaum C, Kliegel M. Hair cortisol and cognitive performance in working age adults. Psychoneuroendocrinology. 2016;67:100–103. doi: 10.1016/j.psyneuen.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 22.De Vente W, van Amsterdam JG, OIff M, Kamphuis JH, Emmelkamp PM. Burnout is associated with reduced parasympathetic activity and reduced HPA axis responsiveness, predominantly in males. Biomed Res Int. 2015;431725. [DOI] [PMC free article] [PubMed]
- 23.Tao N, Zhang J, Song Z, Tang J, Liu J. Relationship between job burnout and neuroendocrine indicators in soldiers in the Xinjiang arid desert: a cross-sectional study. Int J Environ Res Public Health. 2015;12(12):15154–15161. doi: 10.3390/ijerph121214977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lennartsson AK, Sjörs A, Jonsdottir IH. Indication of attenuated DHEA-S response during acute psychosocial stress in patients with clinical burnout. J Psychosom Res. 2015;79(2):107–111. doi: 10.1016/j.jpsychores.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Sjörs A, Jonsdottir IH. No alterations in diurnal cortisol profiles before and during the treatment in patients with stress-related exhaustion. Int J Occup Med Environ Health. 2015;28(1):120–129. doi: 10.13075/ijomeh.1896.00208. [DOI] [PubMed] [Google Scholar]
- 26.Schmaling KB, Romano JM, Jensen MP, Wilkinson CW, McPherson S. Salivary cortisol responses to household tasks among couples with unexplained chronic fatigue. J Fam Psychol. 2015;29(2):296–301. doi: 10.1037/fam0000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lennartsson AK, Sjörs A, Währborg P, Ljung T, Jonsdottir IH. Burnout and hypocortisolism - A matter of severity? A study on ACTH and cortisol responses to acute psychosocial stress. Front Psychiatry. 2015;2:6–8. doi: 10.3389/fpsyt.2015.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oosterholt BG, Maes JH, Van der Linden D, Verbraak MJ, Kompier MA. Burnout and cortisol: Evidence for a lower cortisol awakening response in both clinical and non-clinical burnout. J Psychosom Res. 2015;78(5):445–451. doi: 10.1016/j.jpsychores.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Jonsson P, Osterberg K, Wallergard M, et al. Exaustion-related changes in cardiovascular and cortisol reactivity to acute psychosocial stress. Physiol Behav. 2015;151:327–337. doi: 10.1016/j.physbeh.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 30.Aggarwal VR, Macfarlane GJ, Tajar A, Mulvey MR, Power A, Ray D, McBeth J. Functioning of the hypothalamic-pituitary-adrenal and growth hormone axes in frequently unexplained disorders: results of a population study. Eur J Pain. 2014;18(3):447–454. doi: 10.1002/j.1532-2149.2013.00413.x. [DOI] [PubMed] [Google Scholar]
- 31.Marchand A, Durand P, Juster RP, Lupien SJ. Workers psychological distress, depression, and burnout symptoms: associations with diurnal cortisol profiles. Scand J Work Environ Health. 2014;40(3):305–314. doi: 10.5271/sjweh.3417. [DOI] [PubMed] [Google Scholar]
- 32.Wolfram M, Bellingratin S, Feuerhahn N, Kudielka BM. Emotional exhaustion and over commitment to work are differentially associated with hypothalamus-pituitary-adrenal (HPA) axis responses to a low-dose ACTH1-24 (Synacthen) and dexamethasone-CRH test in healthy school teachers. Stress. 2013;16(1):54–64. doi: 10.3109/10253890.2012.683465. [DOI] [PubMed] [Google Scholar]
- 33.Klaassen EB, de Groot RH, Evers EA, Nicolson NA, Veltman DJ, Jolles J. Cortisol and induced cognitive fatigue: effects on memory activation in healthy males. Biol Psychol. 2013;94(1):167–174. doi: 10.1016/j.biopsycho.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 34.Eek F, Karlson B, Garde AH, Hansen AM, Orbaek P. Cortisol, sleep, and recovery – Some gender differences but no straight associations. Psychoneuroendocrinology. 2012;17(1):56–64. doi: 10.1016/j.psyneuen.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Sjörs A, Ljung T, Jonsdottir IH. Long-term follow-up of cortisol awakening response in patients treated for stress-related exhaustion. BMJ Open. 2012;2:e001091. doi: 10.1136/bmjopen-2012-001091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lindeberg SI, Eek F, Lindbladh E, Ostergren PO, Hansen AM, Karlson B. Exhaustion measured by the SF-36 vitality scale is associated with a flattened diurnal cortisol profile. Neurosci Biohav Rev. 2010;35:97–100. doi: 10.1016/j.neubiorev.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 37.Moya-Albiol L, Serrano MA, Salvador A. Job satisfaction and cortisol awakening response in teachers scoring high and low on burnout. Span J Psychol. 2010;13(2):629–636. doi: 10.1017/S1138741600002304. [DOI] [PubMed] [Google Scholar]
- 38.Kumari M. Cortisol secretion and fatigue: Associations in a community based cohort. Psychoneuroendocrinology. 2009;34(10):1423–1436. doi: 10.1016/j.psyneuen.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Osterberg K, Karlson B, Hansen AM. Cognitive performance in patients with burnout, in relation to diurnal salivary cortisol. Stress. 2009;12(1):70–81. doi: 10.1080/10253890802049699. [DOI] [PubMed] [Google Scholar]
- 40.Rydstedt LW, Cropley M, Devereux JJ, Michalianou G. The effects of gender, long-term need for recovery and trait inhibition-rumination on morning and evening saliva cortisol secretion. Stress Coping. 2009;22(4):465–474. doi: 10.1080/10615800802596378. [DOI] [PubMed] [Google Scholar]
- 41.Wingenfeld K, Schulz M, Damkroeger A, Rose M, Driessen M. Elevated diurnal salivary cortisol in nurses is associated with burnout but not with vital exhaustion. Psychoneuroendocrinology. 2009;34(8):1144–1151. doi: 10.1016/j.psyneuen.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 42.Sertoz O, Tolga Binbay I, Koylu E, Noyan A, Yildirim E, Elbi MH. The role of BDNF and HPA axis in the neurobiology of burnout syndrome. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(6):1459–1465. doi: 10.1016/j.pnpbp.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 43.Bellingrath S, Weigl T, Kudielka BM. Cortisol dysregulation in school teachers in relation to burnout, vital exhaustion, and effort-reward-imbalance. Biol Psychol. 2008;78(1):104–113. doi: 10.1016/j.biopsycho.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 44.Harris A, Ursin H, Murison R, Eriksen HR. Coffee, stress and cortisol in nursing staff. Psychoneuroendocrinology. 2007;32(4):322–330. doi: 10.1016/j.psyneuen.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 45.Sonnenschein M, Mommersteeg PM, Houtveen JH, Sorbi MJ, Schaufeli WB, van Doornen LJ. Exhaustion and endocrine functioning in clinical burnout: an in-depth study using the experience sampling method. Biol Psychol. 2007;75(2):176–184. doi: 10.1016/j.biopsycho.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 46.Langelaan S, Bakker AB, Schaufeli WB, van Rhenen W, van Doornen LJ. Do burned-out and work-engaged employees differ in the functioning of the hypothalamic-pituitary-adrenal axis? Scand J Work Environ Health. 2006;32(5):339–348. doi: 10.5271/sjweh.1029. [DOI] [PubMed] [Google Scholar]
- 47.Mommersteeg PM, Heijnen CJ, Verbraak MJ, van Doornen LJ. Clinical burnout is not reflected in the cortisol awakening response, the day-curve or the response to a low-dose dexamethasone suppression test. Psychoneuroendocrinology. 2006;31(2):216–225. doi: 10.1016/j.psyneuen.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 48.Grossi G, Perski A, Ekstedt M, Johansson T, Lindström M, Holm K. The morning salivary cortisol response in burnout. J Psychosom Res. 2005;59(2):103–111. doi: 10.1016/j.jpsychores.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 49.De Vente W, Olff M, Van Amsterdam JG, Kamphuis JH, Emmelkamp PM. Physiological differences between burnout patients and healthy controls: blood pressure, heart rate, and cortisol responses. Occup Environ Med. 2003;60(Suppl 1):i54–i61. doi: 10.1136/oem.60.suppl_1.i54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moch SL, Panz VR, Joffe BI, Havlik I, Moch JD. Longitudinal changes in pituitary-adrenal hormones in South African women with burnout. Endocrine. 2003;21(3):267–272. doi: 10.1385/ENDO:21:3:267. [DOI] [PubMed] [Google Scholar]
- 51.Melamed S, Ugarten U, Shirom A, Kahana L, Lerman Y, Froom PJ. Chronic burnout, somatic arousal and elevated salivary cortisol levels. J Psychosom Res. 1999;46(6):591–598. doi: 10.1016/S0022-3999(99)00007-0. [DOI] [PubMed] [Google Scholar]
- 52.Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 1999;61(2):197–204. doi: 10.1097/00006842-199903000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Räikkönen K, Hautanen A, Keltikangas-Järvinen L. Feelings of exhaustion, emotional distress, and pituitary and adrenocortical hormones in borderline hypertension. J Hypertens. 1996;14(6):713–718. doi: 10.1097/00004872-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 54.Rahman K, Burton A, Galbraith S, Lloyd A, Vollmer-Conna U. Sleep-wake behavior in chronic fatigue syndrome. Sleep. 2011;34(5):671–678. doi: 10.1093/sleep/34.5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Papadopoulos A, Ebrecht M, Roberts AD, Poon L, Rohleder N, Cleare AJ. Glucocorticoid receptor mediated negative feedback in chronic fatigue syndrome using the low dose (0.5 mg) dexamethasone suppression test. J Affect Disord. 2009;112(1–3):289–294. doi: 10.1016/j.jad.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 56.Torres-Harding S, Sorenson M, Jason L, Maher K, Fletcher MA, Reynolds N, Brown M. The associations between basal salivary cortisol and illness symptomatology in chronic fatigue syndrome. J Appl Biobehav Res. 2008;13:157–180. doi: 10.1111/j.1751-9861.2008.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nater UM, Maloney E, Boneva RS, Gurbaxani BM, Lin JM, Jones JF, Reeves WC, Heim C. Attenuated morning salivary cortisol concentrations in a population-based study of persons with chronic fatigue syndrome and well controls. J Clin Endocrinol Metab. 2008;93(3):703–709. doi: 10.1210/jc.2007-1747. [DOI] [PubMed] [Google Scholar]
- 58.Jerjes WK, Taylor NF, Peters TJ, Wessely S, Cleare AJ. Urinary cortisol and cortisol metabolite excretion in chronic fatigue syndrome. Psychosom Med. 2006;68(4):578–582. doi: 10.1097/01.psy.0000222358.01096.54. [DOI] [PubMed] [Google Scholar]
- 59.Segal TY, Hindmarsh PC, Viner RM. Disturbed adrenal function in adolescents with chronic fatigue syndrome. J Pediatr Endocrinol Metab. 2005;18(3):295–301. doi: 10.1515/JPEM.2005.18.3.295. [DOI] [PubMed] [Google Scholar]
- 60.Jerjes WK, Cleare AJ, Wessely S, Wood PJ, Taylor NF. Diurnal patterns of salivary cortisol and cortisone output in chronic fatigue syndrome. J Affect Disord. 2005;87(2–3):299–304. doi: 10.1016/j.jad.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 61.Crofford LJ, Young EA, Engleberg NC, Korszun A, Brucksch CB, McClure LA, Brown MB, Demitrack MA. Basal circadian and pulsatile ACTH and cortisol secretion in patients with fibromyalgia and/or chronic fatigue syndrome. Brain Behav Immun. 2004;18(4):314–325. doi: 10.1016/j.bbi.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 62.Roberts AD, Wessely S, Chalder T, Papadopoulos A, Cleare AJ. Salivary cortisol response to awakening in chronic fatigue syndrome. Br J Psychiatry. 2004;184:136–141. doi: 10.1192/bjp.184.2.136. [DOI] [PubMed] [Google Scholar]
- 63.Gaab J, Huster D, Peisen R, Engert V, Schad T, Schurmeyer TH, Schurmeyer TH, Ehlert U. Low-dose dexamethasone suppression test in chronic fatigue syndrome and health. Psychosom Med. 2002;64:311–318. doi: 10.1097/00006842-200203000-00015. [DOI] [PubMed] [Google Scholar]
- 64.Scott LV, Medbak S, Dinan TG. Blunted adrenocorticotropin and cortisol responses to corticotropin-releasing hormone stimulation in chronic fatigue syndrome. Acta Psychiatr Scand. 1998;97(6):450–457. doi: 10.1111/j.1600-0447.1998.tb10030.x. [DOI] [PubMed] [Google Scholar]
- 65.Strickland P, Morriss R, Wearden A, Deakin B. A comparison of salivary cortisol in chronic fatigue syndrome, community depression and healthy controls. J Affect Disord. 1998;47(1–3):191–194. doi: 10.1016/S0165-0327(97)00134-1. [DOI] [PubMed] [Google Scholar]
- 66.Young AH, Sharpe M, Clements A, Dowling B, Hawton KE, Cowen PJ. Basal activity of the hypothalamic-pituitary-adrenal axis in patients with the chronic fatigue syndrome (neurasthenia) Biol Psychiatry. 1998;43(3):236–237. doi: 10.1016/S0006-3223(97)00404-6. [DOI] [PubMed] [Google Scholar]
- 67.Powell DJ, Moss-Morris R, Liossi C, Schlotz W. Circadian cortisol and fatigue severity in relapsing-remitting multiple sclerosis. Psychoneuroendocrinology. 2015;56:120–131. doi: 10.1016/j.psyneuen.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 68.Sveinsdottir V, Eriksen HR, Ursin H, Hansen ÅM, Harris A. Cortisol, Health, and Coping in Patients with Nonspecific Low Back Pain. Appl Psychophysiol Biofeedback. 2016;41(1):9–16. doi: 10.1007/s10484-015-9300-2. [DOI] [PubMed] [Google Scholar]
- 69.Schmidt ME, Semik J, Habermann N, Wiskemann J, Ulrich CM, Steindof K. Cancer-related shows a stable association with diurnal cortisol dysregulation in breast cancer patients. Brain Behav Immun. 2016;52:98–105. doi: 10.1016/j.bbi.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 70.Cruz FM, Munhoz BA, Alves BC, Gehrke FS, Fonseca F, Kuniyoshi RK, Cubero D, Peppone LJ, Del Giglio A. Biomarkers of fatigue related to adjuvant chemotherapy for breast cancer: evaluation of plasma and lymphocyte expression. Clin Transl Med. 2015;4:4. doi: 10.1186/s40169-015-0051-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tell D, Mathews HL, Janusek LW. Day-to-day dynamics of associations between sleep, napping, fatigue, and the cortisol diurnal rhythm in women diagnosed as having breast cancer. Psychosom Med. 2014;76(7):519–528. doi: 10.1097/PSY.0000000000000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bay E, Xie Y. Psychological and biological correlates of fatigue after mild-to-moderate traumatic brain injury. West J Nurs Res. 2009;31:731–747. doi: 10.1177/0193945909334856. [DOI] [PubMed] [Google Scholar]
- 73.Sudhaus S, Fricke B, Stachon A, Schneider S, Klein H, During M, Hasenbring M. Salivary cortisol and psychological mechanisms in patients with acute versus chronic low back pain. Psychoneuroendocrinology. 2009;34(4):513–522. doi: 10.1016/j.psyneuen.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 74.Barroso J, Burrage J, Carlson J, Carlson BW. Salivary cortisol values in HIV-positive people. J Assoc Nurses AIDS Care. 2006;17:29–36. doi: 10.1016/j.jana.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 75.Bower JE, Ganz PA, Dickerson SS, Petersen L, Aziz N, Fahey JL. Diurnal cortisol rhythm and fatigue in breast cancer survivors. Psychoneuroendocrinology. 2005;30:92–100. doi: 10.1016/j.psyneuen.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 76.McLean SA, Williams DA, Harris RE, Kop WJ, Groner KH, Ambrose K, Lyden AK, et al. Momentary relation- ship between cortisol secretion and symptoms in patients with fibromyalgia. Arthritis Rheum. 2005;52:3660–3669. doi: 10.1002/art.21372. [DOI] [PubMed] [Google Scholar]
- 77.Dekkers JC, Geenen R, Godaert GLR, van Doornen LJP, Bijlsma JWJ. Diurnal courses of cortisol, pain, fatigue, negative mood, and stiffness in patients with recently diagnosed rheumatoid arthritis. Int J Behav Med. 2000;7:353–371. doi: 10.1207/S15327558IJBM0704_06. [DOI] [Google Scholar]
- 78.Elder GJ, Wetherell MA, Barclay NL, Ellis JG. The cortisol awakening response--applications and implications for sleep medicine. Sleep Med Rev. 2014;18(3):215–224. doi: 10.1016/j.smrv.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 79.Smyth N, Thorn L, Hucklebridge F, Evans P, Clow A. Detailed time course of the cortisol awakening response in healthy participants. Psychoneuroendocrinology. 2015;62:200–203. doi: 10.1016/j.psyneuen.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 80.Clow A, Hucklebridge F, Stalder T, Evans P, Thorn L. The cortisol awakening response: more than a measure of HPA axis function. Neurosci Biobehav Rev. 2010;35(1):97–103. doi: 10.1016/j.neubiorev.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 81.Stalder T, Kirschbaum C, Kudielka BM, Adam EK, Pruessner JC, Wust S, et al. Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology. 2016;63:414–432. doi: 10.1016/j.psyneuen.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 82.Powell DJ, Liossi C, Moss-Morris R, Schlotz W. Unstimulated cortisol secretory activity in everyday life and its relationship with fatigue and chronic fatigue syndrome: a systematic review and subset meta-analysis. Psychoneuroendocrinology. 2013;38(11):2405–2422. doi: 10.1016/j.psyneuen.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 83.Ryan R, Booth S, Spathis A, Mollart S, Clow A. Use of Salivary Diurnal Cortisol as an Outcome Measure in Randomised Controlled Trials: a Systematic Review. Ann Behav Med. 2016;50(2):210–236. doi: 10.1007/s12160-015-9753-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang J, Ma RC, Kong AP, So WY, Li AM, Lam SP, et al. Relationship of sleep quantity and quality with 24-h urinary catecholamines and salivary awakening cortisol in healthy middle-aged adults. Sleep. 2011;34(2):225–233. doi: 10.1093/sleep/34.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Backhaus J, Junghanns K, Hohagen F. Sleep disturbances are correlated with decreased morning awakening salivary cortisol. Psychoneuroendocrinology. 2004;29(9):1184–1191. doi: 10.1016/j.psyneuen.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 86.Wilhelm I, Born J, Kudielka BM, Schlotz W, Wust S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007;32:358–366. doi: 10.1016/j.psyneuen.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 87.Darwent D, Dawson D, Paterson JL, Roach GD, Ferguson SA. Managing fatigue: It really is about sleep. Accid Anal Prev. 2015;82:20–26. doi: 10.1016/j.aap.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 88.Wright J, O’Connor KM. Fatigue. Med Clin North Am. 2014;98(3):597–608. doi: 10.1016/j.mcna.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 89.Rosenthal TC, Majeroni BA, Pretorius R, Malik K. Fatigue: an overview. Am Fam Physician. 2008;78(10):1173–1179. [PubMed] [Google Scholar]
- 90.Verhaeghe J, Van Den Eede F, Van Den Ameele H, Sabbe BG. Neuro-endocrine correlates of burnout. Tijdschr Psychiatr. 2012;54(6):517–526. [PubMed] [Google Scholar]
- 91.Kudielka BM, Bellingrath S, Hellhammer DH. Cortisol in burnout and vital exhaustion: an overview. G Ital Med Lav Ergon. 2006;28(1):34–42. [PubMed] [Google Scholar]
- 92.Galli U, Gaab J, Ettlin DA, Ruggia F, Ehlert U, Palla S. Enhanced negative feedback sensitivity of the hypothalamus-pituitary-adrenal axis in chronic myogenous facial pain. Eur J Pain. 2009;13(6):600–605. doi: 10.1016/j.ejpain.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 93.Gaab J, Hüster D, Peisen R, Engert V, Schad T, Schürmeyer TH, Ehlert U. Low-dose dexamethasone suppression test in chronic fatigue syndrome and health. Psychosom Med. 2002;64(2):311–318. doi: 10.1097/00006842-200203000-00015. [DOI] [PubMed] [Google Scholar]
- 94.Hyyppä MT, Lindholm T, Lehtinen V, Puukka P. Self-perceived fatigue and cortisol secretion in a community sample. J Psychosom Res. 1993;37(6):589–594. doi: 10.1016/0022-3999(93)90053-I. [DOI] [PubMed] [Google Scholar]
- 95.Danhof-Pont MB, van Veen T, Zitman FG. Biomarkers in burnout: a systematic review. J Psychosom Res. 2011;70(6):505–524. doi: 10.1016/j.jpsychores.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 96.Tordjman K, Jaffe A, Trostanetsky Y, Greenman Y, Limor R, Stern N. Low-dose (1 microgram) adrenocorticotrophin (ACTH) stimulation as a screening test for impaired hypothalamo-pituitary-adrenal axis function: sensitivity, specificity and accuracy in comparison with the high-dose (250 microgram) test. Clin Endocrinol (Oxf) 2000;52(5):633–640. doi: 10.1046/j.1365-2265.2000.00984.x. [DOI] [PubMed] [Google Scholar]
- 97.Ospina NS, Al Nofal A, Bancos I, Javed A, Benkhadra K, Kapoor E, et al. ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2016;101(2):427–434. doi: 10.1210/jc.2015-1700. [DOI] [PubMed] [Google Scholar]
- 98.Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(2):364–389. doi: 10.1210/jc.2015-1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Birkett MA. The Trier Social Stress Test protocol for inducing psychological stress. J Vis Exp. 2011;56. [DOI] [PMC free article] [PubMed]
- 100.Skoluda N, Strahler J, Schlotz W, Niederberger L, Marques S, Fischer S, et al. Intra-individual psychological and physiological responses to acute laboratory stressors of different intensity. Psychoneuroendocrinology. 2015;51:227–236. doi: 10.1016/j.psyneuen.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 101.Campbell J, Ehlert U. Acute psychosocial stress: does the emotional stress response correspond with physiological responses? Psychoneuroendocrinology. 2012;37(8):1111–1134. doi: 10.1016/j.psyneuen.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 102.Hellhammer J, Schubert M. The physiological response to Trier Social Stress Test relates to subjective measures of stress during but not before or after the test. Psychoneuroendocrinology. 2012;37(1):119–124. doi: 10.1016/j.psyneuen.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 103.Schmieder R, Rüddel H, Schãchinger H, Neus H. How to perform mental stress tests. J Hum Hypertens. 1987;1(3):223–228. [PubMed] [Google Scholar]
- 104.McKinney ME, Miner MH, Ruddel H, Mcllvain HE, Witte H, Buell JC, et al. The standardized mental stress test protocol: test-retest reliability and comparison with ambulatory blood pressure monitoring. Psychophysiology. 1985;22(4):453–463. doi: 10.1111/j.1469-8986.1985.tb01632.x. [DOI] [PubMed] [Google Scholar]
- 105.Kakiashvili T, Leszek J, Rutkowski K. The medical perspective on burnout. Int J Occup Med Environ Health. 2013;26(3):401–412. doi: 10.2478/s13382-013-0093-3. [DOI] [PubMed] [Google Scholar]
- 106.Salvetti Mde G, Pimenta CA, Braga PE, McGillion M. Prevalence of fatigue and associated factors in chronic low back pain patients. Rev Lat Am Enfermagem. 2013;21:12–19. doi: 10.1590/S0104-11692013000700003. [DOI] [PubMed] [Google Scholar]
- 107.Snekkevik H, Eriksen HR, Tangen T, Chalder T, Reme SE. Fatigue and depression in sick-listed chronic low back pain patients. Pain Med. 2014;15(7):1163–1170. doi: 10.1111/pme.12435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Crosswell AD, Lockwood KG, Ganz PA, Bower JE. Low heart rate variability and cancer-related fatigue in breast cancer survivors. Psychoneuroendocrinology. 2014;45:58–66. doi: 10.1016/j.psyneuen.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fagundes CP, Murray DM, Hwang BS, Gouin JP, Thayer JF, Sollers JJ, 3rd, et al. Sympathetic and parasympathetic activity in cancer-related fatigue: more evidence for a physiological substrate in cancer survivors. Psychoneuroendocrinology. 2011;36(8):1137–1147. doi: 10.1016/j.psyneuen.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Schmidt ME, Chang-Claude J, Seibold P, Vrieling A, Heinz J, Flesh-Janys D, et al. Determinants of long-term fatigue in breast cancer survivors: results of a prospective patient cohort study. Psychooncology. 2015;24(1):40–46. doi: 10.1002/pon.3581. [DOI] [PubMed] [Google Scholar]
- 111.Claborn KR, Miller MB, Meier E. Initial Validation of the HIV Treatment Regimen Fatigue Scale for Adults Prescribed Antiretroviral Therapy. J Assoc Nurses AIDS Care. 2015;26(4):308–315. doi: 10.1016/j.jana.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Claborn KR, Meier E, Miller MB, Leffingwell TR. A systematic review of treatment fatigue among HIV-infected patients prescribed antiretroviral therapy. Psychol Health Med. 2015;20(3):255–265. doi: 10.1080/13548506.2014.945601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Alghadir AH, Gabr SA. Physical activity and enviromental influences on adrenal fatigue os Saudi adults: biochemical analysis and questionnaire survey. J Phys Ther Sci. 2015;27(7):2045–2051. doi: 10.1589/jpts.27.2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.De Kock A, Malan L, Hamer M, Cockeran M, Malan NT. Defensive coping and renovascular disease risk - Adrenal fatigue in a cohort of Africans and Caucasians: The SABPA study. Physiol Behav. 2015;147:213–219. doi: 10.1016/j.physbeh.2015.04.033. [DOI] [PubMed] [Google Scholar]
- 115.Wilcox CS, Schutz MM, Rostagno MR, Lay DC, Jr, Eicher SD. Repeated mixing and isolation: measuring chronic, intermittent stress in Holstein calves. J Dairy Sci. 2013;96(11):7223–7233. doi: 10.3168/jds.2013-6944. [DOI] [PubMed] [Google Scholar]
- 116.Allen LV., Jr Adrenal fatigue. Int J Pharm Compd. 2013;17(1):39–44. [PubMed] [Google Scholar]
- 117.Pranjić N, Nuhbegović S, Brekalo-Lazarević S, Kurtić A. Is adrenal exhaustion synonym of syndrome burnout at workplace? Coll Antropol. 2012;36(3):911–919. [PubMed] [Google Scholar]
- 118.Shah R, Greenberger PA. Chapter 29: unproved and controversial methods and theories in allergy-immunology. Allergy Asthma Proc. 2012;33(Suppl 1):S100–S102. doi: 10.2500/aap.2012.33.3562. [DOI] [PubMed] [Google Scholar]
- 119.Munsterhjelm K, Nordell KM, Brunes B, Andersson KE, Saupe G. Physicians defend Scandlab: Salivary cortisol test can determine adrenal fatigue. Lakartidningen. 2011;108(21):1196–1197. [PubMed] [Google Scholar]
- 120.Nippoldt T. Mayo Clinic office visit. Adrenal fatigue. An interview with Todd Nippoldt, M.D. Mayo Clin Womens Healthsource. 2010;14(3):6. [PubMed] [Google Scholar]
- 121.Head KA, Kelly GS. Nutrients and botanicals for treatment of stress: adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Altern Med Rev. 2009;14(2):114–140. [PubMed] [Google Scholar]
- 122.Tome ME, McNabb FM, Gwazdauskas FC. Adrenal responses to chronic and acute water stress in Japanese quail Coturnix japonica. Comp Biochem Physiol A Comp Physiol. 1985;81(1):171–179. doi: 10.1016/0300-9629(85)90284-1. [DOI] [PubMed] [Google Scholar]
- 123.Thompson SBN. Yawning, fatigue, and cortisol: Expanding the Thompson Cortisol Hypothesis. Medical Hypothesis. 2014;86(4):494–496. doi: 10.1016/j.mehy.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 124.Oosterholt BG, Maes JH, Van der Linden D, Verbraak MJ, Kompier MA. Getting better, but not well: A 1.5 year follow-up of cognitive performance and cortisol levels in clinical and non-clinical burnout. Biol Psychol. 2016;27:89–99. doi: 10.1016/j.biopsycho.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 125.Ulrich-Lai YM, Figueiredo HF, Ostrander MM, Choi DC, Engeland WC, Herman JP. Chronic stress induces adrenal hyperplasia and hypertrophy in a subregion-specific manner. Am J Physiol Endocrinol Metab. 2006;291(5):E965–E973. doi: 10.1152/ajpendo.00070.2006. [DOI] [PubMed] [Google Scholar]
- 126.Harvey PW, Sutcliffe C. Adrenocortical hypertrophy: establishing cause and toxicological significance. J Appl Toxicol. 2010;30(7):617–626. doi: 10.1002/jat.1569. [DOI] [PubMed] [Google Scholar]
- 127.Biglieri EG, Kater CE, Brust N, Chang B, Hirai J. The mineralocorticoid hormone pathways in hypertension with hyperaldosteronism. Clin Exp Hypertens A. 1982;4(9–10):1677–1683. doi: 10.3109/10641968209061633. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Searched studies that were not open access were assessed using CAPES/CNPq and Federal University of Sao Paulo bases, which were responsible for providing all the supplied data to all MEDLINE (Ebsco), PubMed and Cochrane databases.


