Abstract
Background
We aimed at evaluating frequency and factors associated with late presentation and advanced HIV disease and excess risk of death due to these conditions from 1985 to 2013 among naïve HIV infected patients enrolled in the Italian MASTER Cohort.
Methods
All antiretroviral naive adults with available CD4+ T cell count after diagnosis of HIV infection were included. Multivariable logistic regression analysis investigated factors associated either with late presentation or advanced HIV disease. Probabilities of survival were estimated both at year-1 and at year-5 according to the Kaplan-Meier method. Flexible parametric models were used to evaluate changes in risk of death overtime according to late presentation and advanced HIV disease. The analyses were stratified for calendar periods.
Results
19,391 patients were included (54 % were late presenters and 37.6 % were advanced presenters). At multivariable analysis, the following factors were positively associated with late presentation: male gender (OR = 1.29), older age (≥55 years vs. <25 years; OR = 7.45), migration (OR = 1.54), and heterosexual risk factor for HIV acquisition (OR = 1.52) or IDU (OR = 1.27) compared to homosexual risk. Survival rates at year-5 increased steadily and reached 92.1 % for late presenters vs. 97.4 % for non-late presenters enrolled in the period 2004–2009. Using flexible parametric models we found a sustained reduction of hazard ratios over time for any cause deaths between late and non-late presenters over time. Similar results were found for advanced HIV disease.
Conclusion
Screening polices need to be urgently implemented, particularly in most-at-risk categories for late presentation, such as migrants, older patients and those with heterosexual intercourse or IDU as risk factors for HIV acquisition. Although in recent years the impact of late presentation on survival decreased, about 10 % of patients diagnosed in more recent years remains at increased risk of death over a long-term follow-up.
Electronic supplementary material
The online version of this article (doi:10.1186/s12889-016-3477-z) contains supplementary material, which is available to authorized users.
Keywords: HIV infection, AIDS, Late diagnosis, Late presentation, Advanced HIV disease
Background
In 2011 consensus definitions of late presentation and advanced HIV disease were formulated [1]. Late presenters were defined as patients diagnosed with a CD4+ T cell count <350/mm3 or with an AIDS defining event. About 50 % of HIV infected patients in Europe were late presenters [1, 2]. Different HIV transmission patterns were reported in late vs. non-late presenters, although late presentation remains a major problem in any HIV exposure groups [1, 3]. Indeed, rates of late presentation in 2010–2013 were higher in Central Europe (49.8 %), followed by Northern (48.8 %), Southern (45.8 %) and Eastern Regions (38.3 %), especially among intravenous drug users (IDUs) [3, 4].
Late presentation is associated with a greater risk of polypharmacy, drug non adherence and suboptimal virological and immunological effectiveness of antiretroviral therapy [5–7]. From a pharmaco-economical point of view, late presentation increases costs for health care [5]. Patients presenting late show higher rates of AIDS and death when compared with subjects presenting earlier [6, 8, 9], especially during the first year after HIV diagnosis [1]. Moreover, from a public health perspective, people presenting late were spending longer time being unaware of their status, did not start any combination antiretroviral therapy (cART), which is effective in reducing HIV RNA (thereby reducing the risk of transmission by >95 % [10]), so late presentation contributes to enhance rates of HIV transmission [11]. Indeed, some studies reported that community HIV RNA concentrations were correlated with incedence of new HIV diagnoses in specific contexts (e.g., among IDUs or men who have sex with men, MSM) [12, 13]. For these reasons, the World Health Organization (WHO), promotes initiatives to increase HIV testing and retention into care, aimed at reducing rates of late diagnosis and consequently HIV transmission [14], but in reality such campaigns are poorly implemented in some contexts.
In Italy, people presenting late were older (age >50 years), migrants, and more frequently were diagnosed in the Southern-Central Regions [15, 16]. Italian late presenters acquired HIV infection most frequently by heterosexual contacts [15, 16], and secondly by IDU, whereas in other European Countries higher rates of late presenters were reported among IDUs [17].
Until now, national studies evaluated late presentation in a limited period [15, 18, 19]. Moreover, regional analyses were performed along a extended time of observation, but sample was not representative of the national scenario of late presentation and size of the population did not allow to perform a stratified analysis by calendar periods [20, 21]. So, we believe that the available results are not powerful enough to drive preventative strategies and monitor the effects of late presentation on patient survival.
The aim of this study was to study late presentation in a large national Italian cohort from the beginning of the epidemic in Italy to present days. In particular, we evaluated frequency of late presentation over calendar years and associated factors. We further examined whether late presentation was associated with patient survival, and if differences in the mortality rates between late presenters and non late presenters improved overtime to have indications on possible gaps in HIV disease management that may be still present in these patients.
Methods
HIV positive patients enrolled in the Italian MASTER (Standardized Management of Antiviral Therapy) Cohort [22] from January 1985 to December 2013 were selected. Epidemiological, virological, immunological, demographical and clinical data from all patients in the Cohort are stored and annually updated into a common database (Health & Notes 3.5®, Healthware S.p.A., Naples, Italy).
All antiretroviral treatment-naïve patients with available CD4+ T cell count at enrolment were included in the study. CD4+ T cell count at enrolment was defined as CD4+ T cell count closest to and within 6 months since enrolment. Viral load was available since 1996 and defined as HIV RNA closest to or within 30 days since enrolment, including only treatment-naïve subjects at enrolment.
Late presentation refers to people diagnosed with HIV with a CD4+ T cell count below 350/mm3 or with an AIDS defining event regardless of the CD4+ T cell count in the 6 months following HIV diagnosis. Advanced HIV disease refers to people diagnosed with HIV with a CD4+ T cell count below 200/mm3 or with an AIDS defining event, regardless of CD4+ T cell count in the 6 months following HIV diagnosis. HCV co-infection was defined on the basis of positive HCV antibodies.
Vital status and date of death were ascertained through clinical charts, and through a record-linkage with Local Health Authority mortality registers in about one third of patients.
Statistical analysis
Follow-up was determined from enrolment to 31 December 2013 or last follow-up visit, or death, whichever occurred first.
Differences in demographic and clinical features of patients were tested using common statistical methods for comparisons of means and proportions. Associations of demographical and clinical features with late presentation and advanced HIV disease were investigated using a logistic regression model, providing estimates of the odds ratios (ORs) as measures of association and their 95 % confidence intervals (95 % CIs). We adjusted the models for the following a priori confounders: gender, age at enrolment, country of origin, HIV exposure category and period of enrolment as covariates. Separate analyses have been performed in patients presenting at different time periods. The probabilities of survival were estimated at year-1 and at year-5 according to the Kaplan-Meier methods according to late presentation, advanced HIV disease and time periods. The survival curves were compared using the log-rank test. As sensitivity analysis, we calculated probabilities of survival at year-1 and at year-5 applying an inverse probability weighted method to the Kaplan-Meier curves in order to adjust for selection bias due to lost to follow-up (365 days and over since their last visit or exams). Cubic splines were modeled using flexible parametric models [23–25] to evaluate changes of risk of death overtime between late presenters and non late presenters and between subjects with and without advanced HIV disease. The models were adjusted for a priori confounders, including age, gender, country of origin and HIV exposure category. The results were expressed in terms of hazard ratios (HRs) over time and their 95%CIs.
All statistical tests were two-sided, assuming a level of significance of 0.05 and were performed using Stata software version 12.0 (Stata Corp, College Station, TX, USA).
Results
Overall population
19,391 patients were included in the study contributing 143,097 person-years (median 5.2 years of follow-up). Among these patients, 10,486 (54.1 %) were late presenters and 7,291 (37.6 %) had advanced HIV disease at presentation. Table 1 reports the main demographic, epidemiological and clinical characteristics.
Table 1.
Characteristics of subjects at enrolment according to late presentation
| Subjects’ characteristics | No | Yes | Total | P value |
|---|---|---|---|---|
| n (%)* | n (%)a | n (%)b | ||
| Total | 8905 | 10486 | 19391 | |
| Gender | ||||
| Male | 6477 (44.7) | 8022 (55.3) | 14499 (74.8) | <0.001 |
| Female | 2428 (49.6) | 2464 (50.4) | 4892 (25.2) | |
| Age at enrolment (years) | ||||
| < 25 | 1869 (71.9) | 729 (28.1) | 2598 (13.4) | <0.001 |
| 25–34 | 4362 (49.3) | 4478 (50.7) | 8840 (45.6) | |
| 35–44 | 1863 (36.2) | 3290 (63.9) | 5153 (26.6) | |
| 45–54 | 602 (30.8) | 1355 (69.2) | 1957 (10.1) | |
| ≥ 55 | 209 (24.8) | 634 (75.2) | 843 (4.3) | |
| Mean age, years (SD) | 32.1 (8.9) | 37.0 (9.9) | 34.8 (9.8) | <0.001 |
| Mean CD4 T+ cell count//mm3 (SD) | 644.4 (275) | 171.1 (137.4) | 403.1 (320.4) | <0.001 |
| Period of enrolment | ||||
| 1985–1991 | 2612 (60.8) | 1681 (39.2) | 4293 (22.1) | <0.001 |
| 1992–1997 | 2010 (41.3) | 2855 (58.7) | 4865 (25.1) | |
| 1998–2003 | 1727 (40.6) | 2528 (59.4) | 4255 (21.9) | |
| 2004–2009 | 1642 (42.5) | 2217 (57.5) | 3859 (19.9) | |
| 2010–2013 | 914 (43.1) | 1205 (56.9) | 2119 (10.9) | |
| Country of origin | ||||
| Availableb | 8738 (98.1) | 10210 (97.4) | 18948 (97.7) | <0.001 |
| Italy | 7996 (47.1) | 8991 (52.9) | 16987 (89.4) | |
| Others | 742 (37.8) | 1219 (62.2) | 1961 (10.3) | |
| HIV exposure category | ||||
| Availableb | 8156 (91.6) | 9528 (90.9) | 17684 (91.2) | <0.001 |
| MSM | 1333 (47.8) | 1455 (52.2) | 2788 (15.8) | |
| IDUs | 3879 (51.5) | 3654 (48.5) | 7533 (42.6) | |
| Heterosexuals | 2337 (39.2) | 3620 (60.8) | 5957 (33.7) | |
| MSM-IDUs | 60 (57.1) | 45 (42.9) | 105 (0.6) | |
| Heterosexuals-IDUs | 256 (41.0) | 368 (59.0) | 624 (3.5) | |
| Haemophilia/Perinatal transmission | 26 (53.1) | 23 (46.9) | 49 (0.3) | |
| Unknown | 32 (48.5) | 34 (51.5) | 66 (0.4) | |
| Others | 233 (41.5) | 329 (58.5) | 562 (3.2) | |
| Viral load at enrolmentc | ||||
| Availableb | 3678 (41.3) | 5348 (51.0) | 9026 (46.5) | <0.001 |
| Mean HIV RNA, log10 copies/ml (SD) | 4.2 (1.0) | 4.9 (0.9) | 4.6 (1.0) | |
| Hepatitis C co-infection | ||||
| Availableb | 6913 (77.6) | 6923 (66.0) | 13836 (71.4) | <0.001 |
| No | 3250 (45.2) | 3942 (54.8) | 7192 (52.0) | |
| Yes | 3663 (55.1) | 2981 (44.9) | 6644 (48.0) | |
| Hepatitis B co-infection | ||||
| Availableb | 7832 (88.0) | 7836 (74.7) | 15668 (80.8) | <0.001 |
| No | 6889 (50.8) | 6669 (49.2) | 13558 (86.5) | |
| Yes | 943(44.7) | 1167 (55.3) | 2110 (13.5) | |
aRow percentages bcolumn percentages. cViral load is available since 1996 and defined as viral load closest to and within 30 days since enrolment, including only treatment-naïve subjects at enrolment. CD4+ T cell count at enrolment is defined as CD4+ T cell count closest to and within 6 months since enrolment. IDUs Intravenous drug users, MSM Men who have sex with men
Percentages of late presenters increased from 1985–1991 (39.2 %) to 1992–1997 (58.7 %) and then remained stable over time (56.9 % in 2010–2013). Likewise, the prevalence of advanced HIV disease at presentation increased from 1985–1991 (26.9 %) to 1992–1997 (42.1 %), and then showed a modest reduction up to 2010–2013 (38.7 %). The cumulative probability of loss to follow-up at year-3 was 21.4 % (95 % CI 20.8-22.0 %).
Most patients were Italians (89.4 %) and males (74.8 %). Frequency of males ranged from 77.7 to 71.8 % among observational periods. Mean age was 34.8 years (standard deviation, SD 9.8). Major risk factors for HIV acquisition were IDU (42.6 %) and sexual transmission (15.8 % MSM, 33.7 % heterosexuals). In particular, for males the major risk factors were in the order: IDU (46.7 %), heterosexual transmission (24.8 %) and MSM (21 %). For females the major risk factors were: heterosexual transmission (59.7 %) and IDU (30.5 %). Fourty-eight percent patients had HCV co-infection; while 13.5 % patients were co-infected by HBV. Prevalence of HCV co-infection decreased steadily, from 79.2 % in 1985–1991 to 20.3 % in 2010–2012, whereas prevalence of HBV remained stable between 10 % and 19.1 % throughout the entire study period.
Considering cART, no prescription, two nucleoside reverse-transcriptase inhibitors plus one non-nucleoside reverse-transcriptase inhibitors (2NRTIs + NNRTI) and 2NRTIs plus one protease inhibitor either boosted or unboosted by ritonavir (2NRTIs + PI ± r) in the periods under study were, respectively: a) 1985–1991: 51, 0 and 0 %, b) 1992–1997: 45.6, 3.2 and 15.5 %; c) 1998–2003: 5.2, 29.9 and 41.6 %; d) 2004–2009: 1.6, 31.2 and 45.7 %; e) 2010–2013: 0.4, 16.5 and 37.7 %.
Table 1 describes demographic and clinical features according to late presentation. Subjects with foreign origins had more frequently late presentation than Italians (62.2 vs. 52.9 %, p<0.001). Patients presenting late were older than non-late presenters [mean age of late presenters was 37 years (SD 9.9) vs. 32 years (SD 8.9) for non late presenters]. Mean CD4+ T cell count was 171/mm3 (SD 137.4) and 644.4/mm3 (SD 275) in late and non-late presenters, respectively. Subjects with heterosexual risk factor had a late presentation more frequently than MSM and IDUs (60.8 vs. 52.2 % and 48.5 %, p < 0.001). Prevalence of late presenters among MSM decreased from 58.7 % in 1985–1991 to 44.9 % in 2010–2013, whereas, among subjects with heterosexual intercourse as risk factor for HIV acquisition, it increased from 37.2 % in 1985–1991 to 58.2 % in 1992–1997 and to 65.7 % in 2010–2013. HCV co-infected patients were less frequently late presenters than non-HCV co-infected (44.9 vs. 54.8 %, p<0.001), whereas HBV co-infected had an higher prevalence of late presentation than individuals not co-infected by HBV (55.3 vs. 49.2 %, p<0.001).
Factors associated with late presentation
As shown in Table 2, when compared with MSM, the following categories were more likely to present late: people of male gender (OR = 1.29), with older age (≥55 years vs. <25 years; OR = 7.45), migrants (OR = 1.54), heterosexuals (OR = 1.52), and IDUs (OR = 1.27).
Table 2.
Multivariable logistic regression model: association of demographical and clinical features with late presentation according to observation period
| Total period (n = 17333) | 1985–1991 (n = 4254) | 1992–1997 (n = 4614) | 1998–2003 (n = 3892) | 2004–2009 (n = 3142) | 2010–2013 (n = 1431) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Category | ORs (95 % CI) | P value | ORs (95 % CI) | P value | ORs (95 % CI) | P value | ORs (95 % CI) | P value | ORs (95 % CI) | P value | ORs (95 % CI) | P value |
| Gender | Male vs Female | 1.29 (1.19–1.40) | <0.001 | 1.18 (1.00–1.40) | 0.054 | 1.45 (1.25–1.69) | <0.001 | 1.31 (1.12–1.54) | 0.001 | 1.17 (0.97–1.42) | 0.099 | 1.10 (0.82–1.46) | 0.525 |
| Age at enrollment | <25 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||
| 25–34 | 2.44 (2.21–2.70) | <0.001 | 2.55 (2.20–2.97) | <0.001 | 2.99 (2.42–3.69) | <0.001 | 2.52 (1.88–3.39) | <0.001 | 1.48 (1.10–2.00) | 0.009 | 1.58 (1.04–2.40) | 0.032 | |
| 35–44 | 4.11 (3.65–4.61) | <0.001 | 5.33 (4.04–7.02) | <0.001 | 4.84 (3.82–6.14) | <0.001 | 4.44 (3.29–6.01) | <0.001 | 2.49 (1.84–3.35) | <0.001 | 2.65 (1.74–4.03) | <0.001 | |
| 45–54 | 5.79 (4.98–6.74) | <0.001 | 5.04 (2.90–8.73) | <0.001 | 5.20 (3.68–7.35) | <0.001 | 7.70 (5.35–11.08) | <0.001 | 3.57 (2.56–4.99) | <0.001 | 3.75 (2.39–5.90) | <0.001 | |
| ≥55 | 7.45 (6.06–9.16) | <0.001 | 21.65 (6.07–77.22) | <0.001 | 8.06 (5.19–12.53) | <0.001 | 10.08 (6.27–16.19) | <0.001 | 4.19 (2.76–6.36) | <0.001 | 3.98 (2.29–6.94) | <0.001 | |
| Country of Origin | Others vs Italy | 1.54 (1.38–1.73) | <0.001 | 1.91 (1.04–3.49) | 0.036 | 0.94 (0.67–1.33) | 0.742 | 1.53 (1.25–1.88) | <0.001 | 1.48 (1.21–1.81) | <0.001 | 1.52 (1.15–2.03) | 0.004 |
| HIV exposure category | MSM | Ref. | Ref. | Ref. | Ref | Ref. | Ref. | ||||||
| IDUs | 1.27 (1.15–1.40) | <0.001 | 0.59 (0.43–0.80) | 0.001 | 1.44 (1.18–1.76) | <0.001 | 1.27 (1.04–1.56) | 0.017 | 1.18 (0.93–1.50) | 0.172 | 2.12 (1.30–3.47) | 0.003 | |
| Heterosexuals | 1.52 (1.37–1.69) | <0.001 | 0.54 (0.37–0.77) | 0.001 | 1.44 (1.15–1.81) | 0.002 | 1.69 (1.39–2.06) | <0.001 | 1.73 (1.43–2.10) | <0.001 | 1.89 (1.42–2.50) | <0.001 | |
| MSM-IDUs | 0.89 (0.59–1.34) | 0.584 | 0.44 (0.21–0.93) | 0.032 | 0.69 (0.34–1.38) | 0.294 | 0.86 (0.32–2.30) | 0.77 | 2.47 (0.61–9.97) | 0.204 | 2.89 (0.25–32.84) | 0.393 | |
| Heterosexuals-IDUs | 1.88 (1.56–2.26) | <0.001 | 1.47 (0.95–2.27) | 0.085 | 2.39 (1.73–3.29) | <0.001 | 1.42 (0.93–2.17) | 0.106 | 0.67 (0.40–1.11) | 0.121 | 1.07 (0.4–2.88) | 0.896 | |
| Haemophilia /Perinatal transmission | 0.84 (0.36–1.09) | 0.574 | 0.26 (0.09–0.76) | 0.014 | 0.55 (0.17–1.72) | 0.302 | 1.73 (0.32–9.40) | 0.528 | 1.43 (0.08–24.65) | 0.808 | 2.01 (0.43–9.38) | 0.373 | |
| Unknown | 1.05 (0.42–1.10) | 0.856 | 0.95 (0.14–6.53) | 0.958 | 1.21 (0.43–3.36) | 0.718 | 1.89 (0.16–22.73) | 0.617 | 1.50 (0.52–4.36) | 0.456 | 0.79 (0.35–1.81) | 0.582 | |
| Others | 1.43 (0.83–1.20) | 0.001 | 0.97 (0.49–1.90) | 0.92 | 1.09 (0.71–1.66) | 0.702 | 1.21 (0.79–1.85) | 0.372 | 2.37 (1.53–3.67) | <0.001 | 1.58 (0.99–2.53) | 0.055 | |
| Period of enrollment | 1985–1991 | Ref. | |||||||||||
| 1992–1997 | 1.56 (1.43–1.71) | <0.001 | |||||||||||
| 1998–2003 | 1.29 (1.16–1.43) | <0.001 | |||||||||||
| 2004–2009 | 1.14 (1.02–1.28) | 0.026 | |||||||||||
| 2010–2013 | 1.17 (1.01–1.35) | 0.032 | |||||||||||
The associations of demographical and clinical features with late presentation were investigated using a logistic regression model, providing estimates of the odds ratios (ORs) as measures of association. Separate analyses have been performed in different time periods. 95 % CI 95 % confidence interval, OR odds ratio. Ref reference category
In the time-stratified analysis, statistically significant associations between late presentation and male gender were found in all periods, but not in the more recent years (2004–2009 and 2010–2013). Age >25 years and migration were associated with late presentation in any time periods. Heterosexual transmission and IDU compared to MSM were associated with higher risk of late presentation in almost all time periods.
We also found associations when we evaluated factors related with advanced HIV disease (see Additional file 1: Table S1). In the overall population, advanced HIV disease was positively associated with male gender [OR = 1.47, 95%CI 1.35–1.60], older age at enrolment (≥55 years vs. <25 years; OR = 9.59, 95%CI 7.83–11.75), migration (OR = 1.39, 95%CI 1.24–1.56) and heterosexual intercourse (OR = 1.44, 95%CI 1.30–1.60) or IDU (OR = 1.17, 95%CI 1.05–1.29) as risk factor for HIV acquisition compared to MSM.
Survival analysis stratified along calendar years
Survival estimates for people presenting late compared to non-late presenters were 73.9 vs. 99.6 % at year-1 and 35.8 vs. 93.3 % at 5-year in 1985–1991 (log-rank test p<0.001 for both comparisons). Survival rates increased steadily in 1992–1997 and in 1998–2003 either for late presenters or for non late presenters. Survival rates at year-1 and at year-5 reached 95.9 and 92.1 % for late presenters vs.99.2 and 97.4 % for non-late presenters in 2004 to 2009 but differences between late and non late presenters remained significant for both comparisons (p <0.001). (Fig. 1a). Similarly, a better survival was observed in subjects presenting without advanced HIV disease than in subjects with advanced HIV disease (log-rank test p< 0.001 for the whole period) (Fig. 1b). Survival rates at year-1 and at year-5 increased in subjects without advanced HIV disease at presentation from 99.5 and 90.8 % in 1985–1991 to 99 and 96.6 % in 2004–2009. For subjects with advanced HIV disease at presentation, survival rates at year-1 and at year-5 increased from 62.8 and 17.2 % in 1985–1991 to 94.6 and 90.8 % in 2004–2009. When we calculated the survival estimates at year-1 and at year-5 using a model weighted for losses to follow-up, the survival estimates for late-presenters and subjects with advanced HIV disease were lower in 1985–1991 and in 1992–1997 than non-weighted survival estimates (see Additional file 1: Table S2). Late presentation and advanced HIV disease were also evaluated in multivariate flexible parametric models with restricted cubic-splines for the HRs of these variables, which showed a sustained reduction of HRs over time in all periods (Fig. 2). Moreover, when mortality at year-1 was studied in the same models, HRs for late presenters vs. non late presenters were 70.4 (95%CI 46–108) in 1985–1991, 22.1 (95%CI 13.8–35.4) in 1992–1997, 5.4 (95%CI 3.5–8.3) in 1998–2003 and 2.5 (95%CI 1.5–4.3) in 2004–2009.
Fig. 1.
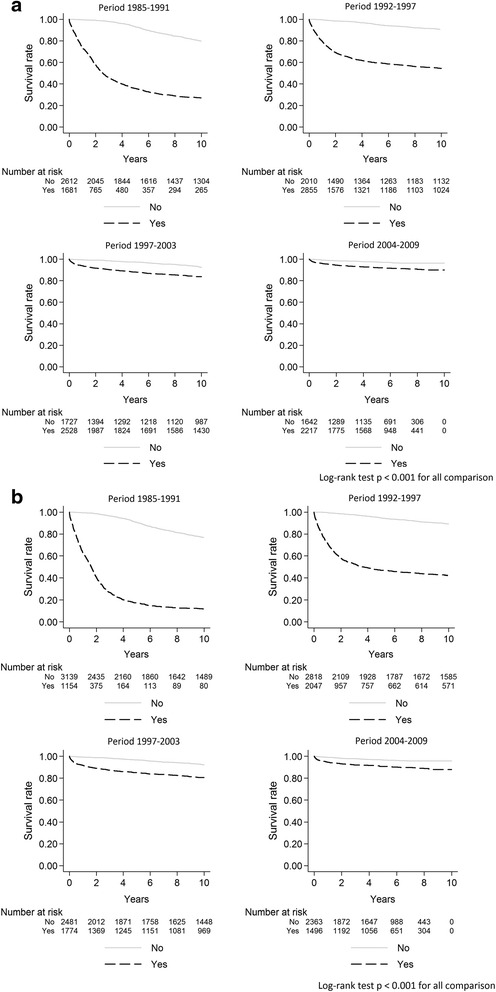
Survival rates from 1985 to 2009 according to late presentation (a) and advanced HIV disease (b)
Fig. 2.
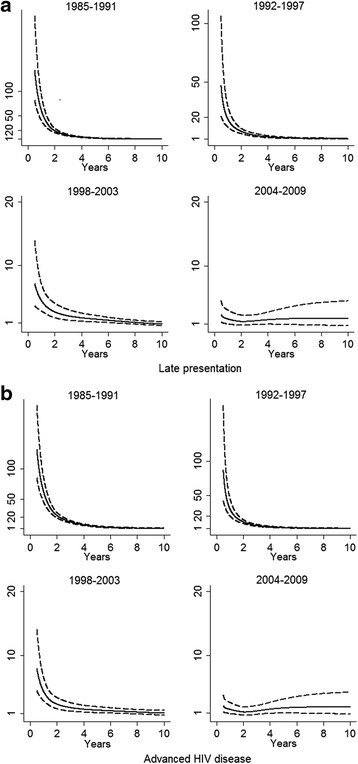
Hazard ratios over time for late presentation (a) and advanced HIV disease (b) using flexible parameter models
Discussion
In the present study we evaluated factors associated with late presentation and compared risk of death for late presenters with risk of death for non late presenters from 1985 to 2013 in a large cohort of drug naïve HIV infected subjects enrolled in Italy. These analyses were also stratified for calendar periods.
Overall, proportion of late presentation and advanced HIV disease were 54 and 38 %, respectively. Late diagnoses were more frequent in the period from 1992 to 2009. Proportion of late presenters in our cohort is in line with previous studies reported by Collaboration of Observational HIV Epidemiological Research Europe Study (COHERE) for Southern Europe in the same time frame [1, 3] and by other recent European and Italian studies [15–21, 26–29]. This was not unexpected because the Italian MASTER Cohort is one of the main contributors to COHERE. Also, profile of people presenting late was similar to previous European and Italian estimates [1, 3, 15]. Indeed, patients presenting late were mostly males, migrants and older than individuals who presented earlier. Only in specific contexts female patients accounted for the majority of late presentations, especially because of the female component of the migrant population coming from Sub Saharian Africa [30–32].
We assessed evolution of factors associated with late presentation along calendar periods. In parallel with a decrease of late presentation among MSM over calendar periods, there was a increase in prevalence of late presentation among heterosexuals, and heterosexual transmission was one of the main risk factors for late presentation from 1992 to 2013. So, we could hypothesize that information and screening polices were quite successful among MSM communities, although a increase of HIV diagnoses in young MSM has been recently reported [33]. The most likely explanation is that older MSM had personal experiences of HIV complications occurring in friends, partners or members of the same community, while younger MSM may only be informed through preventative campaigns in the field. Although the youngest MSM may have not been involved or not respondent to these campaigns as demonstrated by an increase of new HIV diagnoses in the same population in the latest years [33], the level of information in MSM may be higher than in other populations. Moreover, information campaigns in MSM were proven to be successful [34], while heterosexuals did not regularly practice safe sex even if they were well informed about prevention of HIV or other sexually transmitted diseases [35]. It is difficult to explain this possible discrepancy but general differences in the cultural level or background of experiences may play a role.
Compared to MSM, IDUs had a greater risk of late presentation, consistently in all calendar periods. This result has to be referred to syringe exchange (especially in Italy where programs to provide syringes to IDUs are lacking). However, even in IDU populations the risk of HIV acquisition appeared to be more linked with heterosexual intercourses than with IDU by itself [36]. Also, use of recreational drugs (even not intravenous) may be responsible for a increased risk of transmission through sexual intercourses independently from gender and types of sexual relationships. Therefore, further behavioral studies should be conducted to understand the actual ways of HIV transmission and behaviors that may enhance this risk.
Overall, the risk of late presentation was frequently associated with heterosexual transmission in more recent years. Lack of knowledge and underestimation of HIV transmission through this route probably contributed to a late diagnosis, especially among heterosexuals. Indeed, the main reason for late HIV testing reported by heterosexual late presenters was unawareness of risk or unawareness of symptoms of HIV [32]. People presenting late often declare that they were not ill, although the majority of them were symptomatic during the year preceding HIV diagnosis and consulted a physician for these symptoms [32]. In other cases (as among foreign patients, women and IDUs), socioeconomic status and poor access to health care may have contributed to late presentation [37, 38]. At the same time, it is possible that some other factors may contribute to decreased use of condoms, either among heterosexuals or MSM, as alcohol abuse and/or illicit drug use. So, informative campaigns for prevention and early diagnoses should be targeted to persons with any risk behaviors (including heterosexual individuals) rather than to the classical risk categories, such as IDUs or MSM.
In our study we found that survival rates at year-1 and at year-5 increased steadily either for late presenters or for non late presenters. However, survival was always poorer in late presenters compared to non late presenters in all time periods. Using flexible parametric models we found that the excess mortality rate in late presenters was highest immediately after diagnosis and then declined, mostly in farthest years (from 1985 to 1998). Similar results were found for people with advanced HIV disease. In more recent years, improved standards of care and more effective antiretroviral therapies were introduced [39], so this improved clinical outcomes even in patients who presented late. This consideration is important because if the definition of late presentation is applied to classify patients by clinical risk, the existing definition may be anachronistic and should be somehow revised. Alternatively, the improved clinical outcome in late presenters may be due to different composition of the patient cohort across calendar periods. If this is true, the definition should be made more specific in different categories of patients. Notwithstanding these considerations, late presentation should be avoided anyway because it has a strong negative impact on test-and-treat strategies promoting HIV transmission. Also, anticipation of therapy at higher CD4 T cell counts improves patient survival as demonstrated by the START study [40], so more recent guidelines recommend to start cART irrespectively of CD4 T cell count at diagnosis [41]. Moreover, earlier cART reduces morbidities [40], which was not an outcome of our study.
Several limitations of our work should be considered. First, we likely underestimated late presenters in farthest periods, because people diagnosed at that time may have died after the access to the hospital and not survived long enough to be enrolled in the cohort. Second, transient low CD4 T+ cell count in patients with recent infections may lead to overestimation of late presenters, classified according to the consensus definition [42]. However, percentage of patients with recent infection in our cohort was very small and did not influence the results. Indeed, people with a diagnosis of acute or recent infection were very few in the cohort (<1 % in any calendar periods under study). Furthermore, our cohort was affected by a high cumulative probability of loss to follow-up at year-3. This high rate of loss to follow-up is common in retrospective cohort studies, however. Selection bias due to loss to follow up represents a threat to the internal validity of the survival estimates and unadjusted model could overestimated the survival estimates. In our paper we tried to mitigate this selection bias presenting also inverse probability-of-censoring weighted survival estimates.
Conclusions
In conclusion, late presentation affected over 50 % of HIV diagnoses in our cohort. Combination antiretroviral therapy and improved health care contributed to reduce short and long term mortality among late presenters in more recent years. Interestingly, we found that the excess risk of death due to late presentation on overall mortality (at year-1 and at year-5) decreased over calendar years. However, statistically significant differences in survival rates between late and non late presenters were found in all time periods. IDUs, people with heterosexual intercourses, migrants and older patients were more at risk of presenting late in our cohort. Similar associations were found for advanced HIV disease. However, results obtained in the overall populations have to be carefully interpreted, because factors associated with late presentation may change over time, as showed by our analysis stratified by calendar years. Further strategies to encourage and facilitate earlier diagnosis are needed: widespread testing, reaching vulnerable populations, identify and fight against stigma. Increasing HIV testing, information campaigns about HIV risk factors and improvement of the test-and-treat strategy recommended by in the Italian Guidelines only recently [41] will hopefully reduce rates of HIV transmission and late presentations. So our results should be interpreted as a baseline analysis for further monitoring of patient characteristics at diagnosis and clincal outcomes over the long term.
Acknowledgements
MASTER Cohort study group is a large national project involving the major centers providing care to HIV/AIDS patients and includes the following doctors: Francesco Castelli, Eugenia Quiros-Roldan, Paola Nasta, Malattie Infettive, Università degli Studi di Brescia; Alfredo Scalzini, Filippo Castelnuovo, Malattie Infettive Spedali Civili di Brescia; Elena Raffetti, Francesco Donato, Unità di Igiene, Epidemiologia e Sanità Pubblica, Università degli Studi di Brescia; Franco Maggiolo, Malattie Infettive Ospedale Papa Giovanni XXIII, Bergamo; Gioacchino Angarano, Nicoletta Ladisa, Clinica di Malattie Infettive Policlinico di Bari; Francesco Mazzotta, Massimo Di Pietro Malattie Infettive S.M. Annunziata, Firenze; Andrea Gori, Giuseppe Lapadula, Silvia Costarelli, Malattie Infettive Ospedale San Gerardo di Monza; Laura Sighinolfi, Malattie Infettive Nuovo Polo Ospedaliero di Cona, Ferrara; Angelo Pan, Silvia Lorenzotti, Malattie Infettive Istituti Ospitalieri Cremona; Roberto Cauda, Simona Di Giambenedetto Malattie Infettive Policlinico A. Gemelli - Università Cattolica di Roma; Carlo Torti, Università Magna Grecia di Catanzaro; Mattia Prosperi, University of Florida; Nicola Mazzini, MISI Foundation; Emanuele Focà.
Funding
The MASTER Cohort was funded by MISI Foundation (Fondazione Malattie Infettive e Salute Internazionale, http://www.fondazionemisi.it).
Availability of data and materials
For ethical and legal restriction we can not upload a minimal dataset. The data are available upon request, the interested researchers could contact directly the statistician, Dr. Elena Raffetti (elena.raffetti@gmail.com) or the scientific secretariat of the MASTER Cohort (francesca.brognoli@bsnet.it).
Authors’ contributions
ER, and CT conceived the study and participated in its design and coordination; ER performed the statistical analysis and draft the manuscript; MCP and CT interpreted the data and participated in drafting the manuscript; FrC, CS, FC, FM, EDF, ADA, AG, NL, MDP, LS and FZ made substantial contributions to the acquisition of data; FrC contributed to manuscript for intellectual content. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and the principles of Good Clinical Practice. All patients provided written informed consent to include their clinical and biological data in the MASTER database for scientific purposes. Data submitted by the participating clinics to the data center were anonymized. The study was approved by the Ethical Committees of the Spedali Civili Hospital of Brescia (Coordinating Centre) and of the following Institutions: University Hospital of Ferrara; “Papa Giovanni XXIII” Hospital, Bergamo; University of Bari; “San Gerardo” Hospital, Monza; Hospital of Cremona; “S. M. Annunziata” Hospital, Firenze; University of Sacred Heart, Rome.
Abbreviations
- AIDS
Acquired Immune Deficiency Syndrome
- cART
Combination Antiretroviral Therapy
- HBV
Hepatitis B Virus
- HCV
Hepatitis C Virus
- HIV
Human Immuno-Deficiency Virus
- IDU
Intravenous Drug Use
- IDUs
Intravenous Drug Users
- MASTER Cohort
Standardized Management of Antiviral Therapy Cohort
- MSM
Men Have Sex With Men
Additional file
Multivariable logistic regression model: association of demographical and clinical features with advanced HIV disease according to observation period. Table S2. Survival rate at year-1 and at year-5 from 1985 to 2009 according to late presentation and advanced HIV disease (weighted for losses to follow-up). (DOCX 23 kb)
Contributor Information
Elena Raffetti, Email: elena.raffetti@hotmail.it.
Maria Concetta Postorino, Email: cettypostorino@gmail.com.
Francesco Castelli, Email: francesco.castelli@unibs.it.
Salvatore Casari, Email: s.casari@infettivibrescia.it.
Filippo Castelnuovo, Email: filippo.castelnuovo@spedalicivili.brescia.it.
Franco Maggiolo, Email: franco31556@hotmail.com.
Elisa Di Filippo, Email: elisadifilippo@libero.it.
Alessandro D’Avino, Email: alessandro-davino@virgilio.it.
Andrea Gori, Email: andrea.gori@unimib.it.
Nicoletta Ladisa, Email: nladisa@hotmail.com.
Massimo Di Pietro, Email: massimo.dipietro@asf.toscana.it.
Laura Sighinolfi, Email: laurasighi@libero.it.
Fabio Zacchi, Email: zacchi.fabio@virgilio.it.
Carlo Torti, Email: torti@unicz.it.
References
- 1.Mocroft A, et al. Risk factors and outcomes for late presentation for HIV-positive persons in Europe: results from the Collaboration of Observational HIV Epidemiological Research Europe Study (COHERE) PLoS Med. 2013;10(9):e1001510. doi: 10.1371/journal.pmed.1001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antinori A, et al. Late presentation of HIV infection: a consensus definition. HIV Med. 2011;12(1):61–64. doi: 10.1111/j.1468-1293.2010.00857.x. [DOI] [PubMed] [Google Scholar]
- 3.Mocroft A., et al., Late presentation for HIV care across Europe: update from the Collaboration of Observational HIV Epidemiological Research Europe (COHERE) study, 2010 to 2013. Euro Surveill. 2015;20(47):7–18. [DOI] [PubMed]
- 4.Public Health England (PHE) HIV new diagnoses, treatment and care in the UK 2015 report. 2015. [Google Scholar]
- 5.Sabin CA, et al. Late presenters in the era of highly active antiretroviral therapy: uptake of and responses to antiretroviral therapy. AIDS. 2004;18(16):2145–2151. doi: 10.1097/00002030-200411050-00006. [DOI] [PubMed] [Google Scholar]
- 6.Sabin CA, et al. Deaths in the era of HAART: contribution of late presentation, treatment exposure, resistance and abnormal laboratory markers. AIDS. 2006;20(1):67–71. doi: 10.1097/01.aids.0000196178.73174.24. [DOI] [PubMed] [Google Scholar]
- 7.Sabin CA, et al. Late diagnosis in the HAART era: proposed common definitions and associations with mortality. AIDS. 2010;24(5):723–727. doi: 10.1097/QAD.0b013e328333fa0f. [DOI] [PubMed] [Google Scholar]
- 8.Celesia BM, et al. Late presentation of HIV infection: predictors of delayed diagnosis and survival in Eastern Sicily. Eur Rev Med Pharmacol Sci. 2013;17(16):2218–2224. [PubMed] [Google Scholar]
- 9.Jiang H, et al. Gender difference in advanced HIV disease and late presentation according to European consensus definitions. Sci Rep. 2015;5:14543. doi: 10.1038/srep14543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iwuji CC, et al. Evaluation of the impact of immediate versus WHO recommendations-guided antiretroviral therapy initiation on HIV incidence: the ANRS 12249 TasP (Treatment as Prevention) trial in Hlabisa sub-district, KwaZulu-Natal, South Africa: study protocol for a cluster randomised controlled trial. Trials. 2013;14:230. doi: 10.1186/1745-6215-14-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen MS, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore DM, et al. HIV Community Viral Load and Factors Associated With Elevated Viremia Among a Community-Based Sample of Men Who Have Sex With Men in Vancouver, Canada. J Acquir Immune Defic Syndr. 2016;72(1):87–95. doi: 10.1097/QAI.0000000000000934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wood E, et al. Longitudinal community plasma HIV-1 RNA concentrations and incidence of HIV-1 among injecting drug users: prospective cohort study. BMJ. 2009;338:b1649. doi: 10.1136/bmj.b1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO . Guidance on provider-initiated HIV testing and counselling in health facilities. 2007. [Google Scholar]
- 15.Camoni L, et al. Late presenters among persons with a new HIV diagnosis in Italy, 2010–2011. BMC Public Health. 2013;13:281. doi: 10.1186/1471-2458-13-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Camoni L, et al. The continued ageing of people with AIDS in Italy: recent trend from the national AIDS Registry. Ann Ist Super Sanita. 2014;50(3):291–297. doi: 10.4415/ANN_14_03_12. [DOI] [PubMed] [Google Scholar]
- 17.Hall HI, et al. Late diagnosis and entry to care after diagnosis of human immunodeficiency virus infection: a country comparison. PLoS One. 2013;8(11):e77763. doi: 10.1371/journal.pone.0077763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Girardi E, et al. Delayed presentation and late testing for HIV: demographic and behavioral risk factors in a multicenter study in Italy. J Acquir Immune Defic Syndr. 2004;36(4):951–959. doi: 10.1097/00126334-200408010-00009. [DOI] [PubMed] [Google Scholar]
- 19.d’Arminio Monforte A, et al. Late presenters in new HIV diagnoses from an Italian cohort of HIV-infected patients: prevalence and clinical outcome. Antivir Ther. 2011;16(7):1103–1112. doi: 10.3851/IMP1883. [DOI] [PubMed] [Google Scholar]
- 20.Borghi V, et al. Late presenters in an HIV surveillance system in Italy during the period 1992–2006. J Acquir Immune Defic Syndr. 2008;49(3):282–286. doi: 10.1097/QAI.0b013e318186eabc. [DOI] [PubMed] [Google Scholar]
- 21.Loconsole D, et al. Surveillance of new HIV infections/diagnoses in Puglia region (south Italy), years 2007–2011. Ann Ig. 2013;25(4):291–298. doi: 10.7416/ai.2013.1931. [DOI] [PubMed] [Google Scholar]
- 22.Torti C., et al. Cohort Profile: Standardized Management of Antiretroviral Therapy Cohort (MASTER Cohort). Int J Epidemiol. 2015. [Epub ahead of print] [DOI] [PubMed]
- 23.Lambert P. Further development of flexible parametric models for survival analysis. The Stata J. 2009;9(2):265–290. [Google Scholar]
- 24.Royston P, Parmar MK. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med. 2002;21(15):2175–2197. doi: 10.1002/sim.1203. [DOI] [PubMed] [Google Scholar]
- 25.Lambert PC, et al. Quantifying differences in breast cancer survival between England and Norway. Cancer Epidemiol. 2011;35(6):526–533. doi: 10.1016/j.canep.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Zoufaly A, et al. Late presentation for HIV diagnosis and care in Germany. HIV Med. 2012;13(3):172–181. doi: 10.1111/j.1468-1293.2011.00958.x. [DOI] [PubMed] [Google Scholar]
- 27.Vives N, et al. Factors associated with late presentation of HIV infection in Catalonia, Spain. Int J STD AIDS. 2012;23(7):475–480. doi: 10.1258/ijsa.2011.011280. [DOI] [PubMed] [Google Scholar]
- 28.Helleberg M, et al. Late presenters, repeated testing, and missed opportunities in a Danish nationwide HIV cohort. Scand J Infect Dis. 2012;44(4):282–288. doi: 10.3109/00365548.2011.626440. [DOI] [PubMed] [Google Scholar]
- 29.Ndiaye B, et al. Factors associated with presentation to care with advanced HIV disease in Brussels and Northern France: 1997–2007. BMC Infect Dis. 2011;11:11. doi: 10.1186/1471-2334-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sulis G, et al. Clinical and epidemiological features of HIV/AIDS infection among migrants at first access to healthcare services as compared to Italian patients in Italy: a retrospective multicentre study, 2000–2010. Infection. 2014;42(5):859–867. doi: 10.1007/s15010-014-0648-7. [DOI] [PubMed] [Google Scholar]
- 31.Yombi JC, et al. Late presentation for human immunodeficiency virus HIV diagnosis results of a Belgian single centre. Acta Clin Belg. 2014;69(1):33–39. doi: 10.1179/0001551213Z.00000000014. [DOI] [PubMed] [Google Scholar]
- 32.Hachfeld A, et al. Reasons for late presentation to HIV care in Switzerland. J Int AIDS Soc. 2015;18(1):20317. doi: 10.7448/IAS.18.1.20317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.ISS, Istituto Superiore di Sanità, Dati HIV e AIDS. Notiziario ISS, Novembre. 2015. http://www.iss.it/binary/ccoa/cont/HIV_AIDS_DIC_2015.pdf.
- 34.Grov C, et al. Men who have sex with mens’ exposure to, use of, and subjective experiences with the ’NYC Condom’. AIDS Behav. 2014;18(11):2172–2177. doi: 10.1007/s10461-014-0783-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hotton AL, et al. relationship dynamics and sexual risk reduction strategies among heterosexual young adults: a qualitative study of sexually transmitted infection clinic attendees at an urban Chicago health center. AIDS Patient Care STDs. 2015;29(12):668–674. doi: 10.1089/apc.2015.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cruciani M, et al. Increasing prevalence of HIV infection among first time clients in Italian drug treatment services - is it sexual transmission? BMC Infect Dis. 2015;15(1):201. doi: 10.1186/s12879-015-0940-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lodi S, et al. Delayed HIV diagnosis and initiation of antiretroviral therapy: inequalities by educational level, COHERE in EuroCoord. AIDS. 2014;28(15):2297–2306. doi: 10.1097/QAD.0000000000000410. [DOI] [PubMed] [Google Scholar]
- 38.Sobrino-Vegas P, et al. Educational gradient in HIV diagnosis delay, mortality, antiretroviral treatment initiation and response in a country with universal health care. Antivir Ther. 2012;17(1):1–8. doi: 10.3851/IMP1939. [DOI] [PubMed] [Google Scholar]
- 39.CASCADE Collaboration Changes in the uptake of antiretroviral therapy and survival in people with known duration of HIV infection in Europe: results from CASCADE. HIV Med. 2000;1(4):224–231. doi: 10.1046/j.1468-1293.2000.00033.x. [DOI] [PubMed] [Google Scholar]
- 40.The INSIGHT START Study Group Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N Engl J Med. 2015;373:795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ministero della Salute . Linee guida italiane sull’utilizzo dei farmaci antiretrovirali e sulla gestione diagnositico-clinica delle persone con infezione da HIV-1. 2015. [Google Scholar]
- 42.Sasse A, et al. Late presentation to HIV testing is overestimated when based on the consensus definition. HIV Med. 2015;17(3):231–234. doi: 10.1111/hiv.12292. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
For ethical and legal restriction we can not upload a minimal dataset. The data are available upon request, the interested researchers could contact directly the statistician, Dr. Elena Raffetti (elena.raffetti@gmail.com) or the scientific secretariat of the MASTER Cohort (francesca.brognoli@bsnet.it).


