Abstract
Background
Known factors affecting the management of vesicoureteral reflux (VUR) include reflux grade, infection frequency, age and gender. We hypothesized that provider preference is highly associated with management.
Methods
Utilizing the national billing database, Faculty Practice Solutions Center (FPSC), a multivariable logistic regression model was applied to analyze the association of pediatric urologist treatment patterns, patient age, gender, uni- or bilateral disease, insurance type, presence of nephropathy and race with the type of VUR treatment a patient would receive.
Results
We identified 59 pediatric urologists who managed 7,882 new reflux patients from 2009 to 2011. There was wide variation in surgical utilization between surgeons (mean 50%) but minimal change for each surgeon (5%) over the 3-year period. For every 100 new reflux patients, surgeon median utilization of reimplant and Deflux was 26% and 20%, respectively. Age ranked highest in predicting surgical vs. non-surgical management. A surgeon’s historic Deflux utilization rate ranked highest in predicting surgery type. Older age, female gender and white race also increased the odds of Deflux utilization over reimplant.
Conclusions
A surgeon’s historic Deflux utilization was the most important predictor of VUR surgery type. Although data on reflux grade was not available, analysis of patient and surgeon characteristics suggests that surgeon preference is the first or second most critical factor in determining a patient’s treatment.
Keywords: vesicoureteral reflux, Deflux, ureteral reimplantation
Introduction
Standard management of primary vesicoureteral reflux (VUR) in the pediatric population includes observation, prophylactic antibiotics, subureteric injection of Deflux (dextranomer/hyaluronic acid polymer) or ureteral reimplantation. Commonly known factors affecting the management choice include the grade of reflux, frequency and severity of urinary tract infection, age and gender. There are no current guidelines on the use of each treatment modality and therefore there is high variability in the treatment of vesicoureteral reflux.1 Provider characteristics have been shown to be highly predictive of treatment choices for adult patients with urologic disorders such as prostate cancer, incontinence, renal masses, and those needing urinary diversion.2–5 Based upon the wide variation of Deflux utilization, we hypothesized that provider preference might be the most critical factor in the ultimate management of patients with reflux.
Materials
The Faculty Practice Solutions Center (FPSC) was initiated by an alliance between the University Health System Consortium (UHC) and the Association of American Medical Colleges (AAMC) in 2001 in an effort to collect benchmarking data on academic clinical practices throughout the country. Its goal is to improve performance and outcomes. The FPSC involves over 90 participating institutions nationwide with over 60,000 physicians. Coding data include hospital, de-identified provider and specialty, patient identification, date of birth, gender, race, Current Procedural Terminology (CPT) codes, International Classification of Diseases book 9 (ICD-9) diagnosis billing codes, service date, site of service, payer category and more. FPSC is unique not only for its large scale of data capture, but also for its role in tracking billing information, which offers a more reliable reflection of practice patterns with both CPT and ICD-9 codes.
Methods
The FPSC database designates specialty, urology, but not subspecialty. Pediatric urologists were identified by those urologists who performed at least 3 orchiopexies (CPT 54640) or 3 hypospadias repairs (CPT 54324) in 2009. The orchiopexy code we used (54640) is specific to those done for undescended testes. In order to exclude the possibility of capturing orchiopexies performed by adult urologists, we did not include orchiopexies done for emergent torsion (54600, 54620). New patients seen by these physicians in 2009 were identified using the new consult or new patient CPT codes: 99201–05, 99241–45. VUR patients with and without nephropathy were identified by ICD-9 codes 593.7 and 593.71–73, respectively. Reflux grade and UTI history were not available in this database.
Based on 2009 data, five variables were calculated to characterize the practice pattern of each physician. The number of patients treated with reimplantation or Deflux in 2009 divided by the number of new consults seen in 2009, are designated R/P or D/P, respectively (Figure 1). The percentage of surgical patients treated with reimplantation or Deflux was designated R/S or D/S, respectively.
Figure 1.
Example of Physician Characteristics - 2009
To determine if the physicians’ practice patterns in 2009 were predictive of treatment choices in the future, we evaluated patients with VUR who saw these physicians for an initial consultation in 2010 to determine if these patients had a Deflux or reimplantation procedure in 2010 or 2011. Deflux procedures were identified using the CPT code 52327 and reimplantation procedures were identified using CPT codes: 50780 and 50782. We excluded laparoscopic ureteral reimplantation (50947, 50948) since it is not considered standard practice and was only performed 10 times over 3 years. Exclusion criteria included patients over the age of 10 years, those bearing diagnosis codes associated with posterior urethral valves, neurogenic bladder, spina bifida, ureterocele, ureteropelvic junction obstruction, hypospadias, spinal cord injury, sacral agenesis, VATER syndrome, urethral fistula, bladder fistula, bladder exstrophy, traumatic ureteral, bladder or urethral injury, prune belly syndrome, renal agenesis or solitary kidney. In addition, those patients with concomitant procedure codes associated with bladder augmentation, valve ablation, ureterocele excision or incision, and other ureteral surgery were excluded.
Statistical Analyses
In order to examine the magnitude of variability between surgeons, mixed effects models were fitted to practice pattern metrics (D/P, R/P, D/S, R/S, and D/P + R/P) from 2009 through 2011. Each model included a fixed effect for year (in order to adjust for any overall time trends) and a random effect for surgeon. The joint effects of the 2009 D/P, R/P, D/S, R/S and D/P + R/P of the treating physician, patient age, gender, uni- or bilateral disease, insurance type, region, presence of nephropathy, and race upon the treatment received between 2010 and 2011 were analyzed using multivariable logistic regression models incorporating random effects for physician and hospital.
The probability of a patient having reimplantation or Deflux was analyzed using two separate mixed effects logistic regression models. First, a model was fitted to all patients whether or not the patient received either surgical treatment as a binary outcome. Then, a model was fitted to data from patients who received treatment using reimplantation vs. Deflux as the binary outcome.
The D/P, R/P, D/S, R/S and D/P + R/P are highly correlated with one another. Therefore, rather than including all five of these numbers in each analysis, the Akaike Information Criterion (AIC) was used to select among models including one or more of the D/P, R/P, D/S, R/S and D/P + R/P. The AIC is based on the likelihood ratio statistic, which measures how closely a statistical model fits the observed data. Results reported are for the “best” model for each analysis; i.e. the model with the smallest AIC.6
Variable importance rank was calculated such that for a given ordering of the variables in a model, variables were added sequentially and the reduction in deviance for the addition of each variable was calculated.7,8 The reduction in deviance was then averaged over 1,000 randomly sampled permutations of the order in which variables could enter the model, and variables were ranked in order of average reduction in deviance. It should be noted that variable importance is a distinct concept from statistical significance and would not necessarily be expected to yield the same ranking of variables as one might get from a p-value ordering.9
Data extraction was conducted using SAS for Windows, Version 9.3. Statistical analyses were conducted using R, version 2.15.2, with mixed effects logistic regression modeling conducted using the R package lme4, version 0.999999-0.
Results
We identified 59 pediatric urologists who saw 7,882 new VUR patients from January 1, 2009 through December 31, 2011. We found that each physician who met our criteria as a pediatric urologist performed a minimum of 20 elective orchiopexies per year and saw a minimum of 22 unique reflux patients per year. Table 1 illustrates representative demographics for one year – 2010.
Table 1.
Patient and Surgery Characteristics By Treatment (2010)
| Treatment | Reimplant | Deflux | No Surgery |
|---|---|---|---|
| Median Age (yrs) at | 3.6 (0.1–9.9) | 4.0 (0.0–9.9) | 1.6 (0.0–9.9) |
| Initial Consult (range) | |||
| Race | |||
| White | 67 (29%) | 55 (45%) | 645 (32%) |
| Asian | 2 (1%) | 0 | 9 (<1%) |
| Black | 3 (1%) | 0 | 28 (1%) |
| Hispanic | 15 (7%) | 5 (4%) | 110 (5%) |
| Native American | 1 (<1%) | 0 | 1 (<1%) |
| Other | 13 (6%) | 5 (4%) | 75 (4%) |
| Unknown | 128 (56%) | 58 (47%) | 1140 (57%) |
| Gender | |||
| Female | 162 (71%) | 105 (85%) | 1491 (74%) |
| Male | 67 (29%) | 15 (12%) | 490 (24%) |
| Unknown | 0 | 3 (2%) | 27 (1%) |
| Insurance Type | |||
| Commercial | 137 (60%) | 74 (60%) | 1222 (61%) |
| Medicaid | 76 (33%) | 39 (32%) | 617 (31%) |
| Self Pay | 4 (2%) | 3 (2%) | 66 (3%) |
| Other | 12 (5%) | 7 (6%) | 103 5%) |
| Bilateral Procedure | |||
| No | 139 (61%) | 70 (57%) | - |
| Yes | 90 (39%) | 53 (43%) | - |
Surgeon Practice Patterns
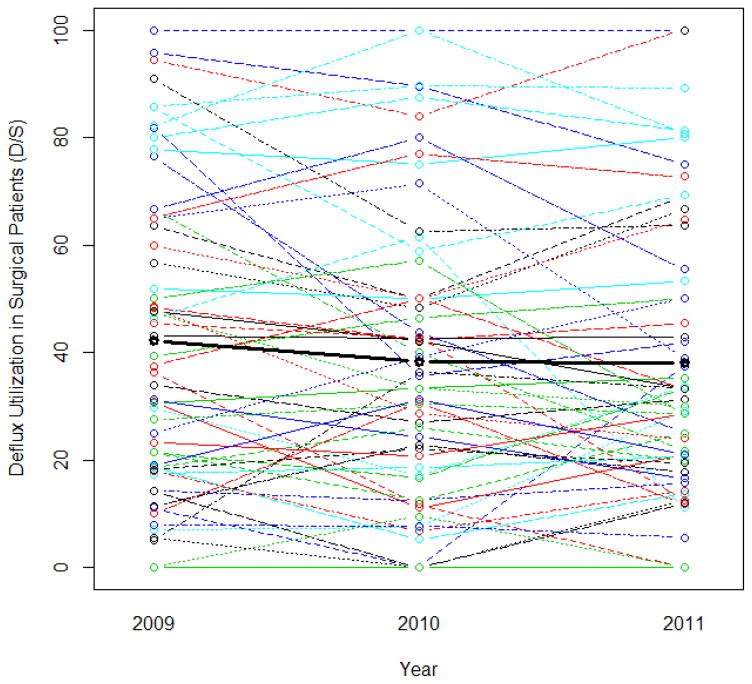
There was wide variation in surgical utilization between surgeons but minimal change for each individual surgeon over the 3-year period. Figures 2 and 3 show the percentage of new patients treated with Deflux (D/P) and percentage of surgical patients treated with Deflux (D/S) for each urologist from 2009 through 2011.
Figure 2.
Deflux utilization in new VUR patients over time for each urologist. Each line corresponds to a single urologist. The bold line depicts the mean for each year.
Figure 3.
Deflux utilization in surgical patients over time for each urologist. Each line corresponds to a single urologist. The bold line depicts the mean for each year.
For all of the metrics analyzed, variability between surgeons was a significant source of variation in the data. The between-surgeon standard deviations were significantly different from 0 (likelihood ratio test P < 0.001, Table 2), and larger than the residual (within-surgeon) standard deviations in all cases.
Table 2.
Between- and Within-Surgeon Standard Deviations (SD) of Practice Pattern Metrics
| Metric | Between-Surgeon SD | Within-Surgeon SD | Likelihood Ratio Test P-Value for Surgeon Effect |
|---|---|---|---|
| D/P | 0.17 | 0.10 | <0.001 |
| R/P | 0.24 | 0.20 | <0.001 |
| D/P + R/P | 0.26 | 0.26 | <0.001 |
| D/S | 0.26 | 0.11 | <0.001 |
| R/S | 0.26 | 0.11 | <0.001 |
The between-surgeon standard deviations were significantly different from 0 (likelihood ratio test P < 0.001), and larger than the residual (within-surgeon) standard deviations in all cases.
Utilization of Any Surgery
For new patients seen in 2010, age was ranked highest in predicting surgical vs. non-surgical treatment from 2010 to 2011. Mixed effects logistic regression analysis found each additional year of age associated with a 26% increase in the odds of treatment vs. observation (P<0.001) (Table 3). Second and fourth in importance ranking was physician practice patterns. For every 10% increase in a physician’s percentage of surgical patients treated with reimplantation (R/S), there was a 22% increase in the odds of surgical treatment vs. observation (P = 0.003). In addition, for every 10% increase in a physician’s percentage of new patients treated with Deflux (D/P), there was a 34% increase in odds of surgical treatment (P = 0.006). Regional differences, which ranked third in importance ranking, did not effect the odds of a patient receiving surgery or observation. Nephropathy was identified in 19% of reflux patients. A diagnosis of nephropathy was associated with a significantly higher (80% increase) odds of surgical treatment (p = 0.038) compared to the diagnosis of reflux without nephropathy.
Table 3.
Logistic Regression Analysis of Probability of Any Surgical Treatment (Deflux or Reimplantation) vs. No Surgical Treatment
| Variable | OR | P- Value | 95% Confidence Interval for OR | Variable Importance Rank* |
|---|---|---|---|---|
| Age (years) | 1.26 | <0.001 | (1.18, 1.34) | 1 |
| R/S | 1.02 | 0.003 | (1.01, 1.04) | 2 |
| Region: Midwest (Referent) | 1.00 | - | - | 3 |
| Northeast | 0.48 | 0.128 | (0.19, 1.23) | |
| South | 0.74 | 0.368 | (0.39, 1.42) | |
| West | 0.67 | 0.398 | (0.26, 1.70) | |
| D/P | 1.03 | 0.006 | (1.01, 1.05) | 4 |
| Nephropathy: No (Referent) | 1.00 | - | - | 5 |
| Yes | 1.80 | 0.038 | (1.03, 3.14) | |
| Insurance Type: Commercial (Referent) | 1.00 | - | - | 6 |
| Medicaid or Self Pay | 1.15 | 0.506 | (0.77, 1.70) | |
| All Other | 0.85 | 0.680 | (0.38, 1.89) | |
| Gender: Female (Referent) | 1.00 | - | - | 7 |
| Male | 1.17 | 0.475 | (0.76, 1.81) | |
| Race: White (Referent) | 1.00 | - | - | 8 |
| Non-White | 0.95 | 0.824 | (0.61, 1.49) |
Based on average reduction in deviance when covariates added to model sequentially, averaged over 1000 randomly sampled permutations of variable ordering.
Surgery Type
For every 100 new reflux patients in 2009, surgeon median utilization of reimplant (R/P) and Deflux (D/P) was 26% and 20%, respectively (Table 4). The median reimplant percent of surgery patients (R/S) and Deflux percent of surgery patients (D/S) was 63% and 38%, respectively (Table 4). Among those who undergo surgery, variable importance rank found a surgeon’s rate of new patients treated with Deflux (D/P) to be the highest predictor of surgery type.
Table 4.
Physician Characteristics (Urologists Included In Multivariable Analysis, Based on 2009 Data)
| Median (Range) | |
|---|---|
| Number of New VUR Patients in 2009 | 54 (22–112) |
| Number of VUR Patients with Reimplantation | 13 (0–63) |
| Number of VUR Patients with Deflux | 9 (0–37) |
| R/P Percentage | 26% (0%–111%) |
| D/P Percentage | 20% (0%–79%) |
| D/P + R/P Percentage | 45% (7%–135%) |
| R/S Percentage | 63% (0%–100%) |
| D/S Percentage | 38% (0%–100%) |
Median practice patterns of pediatric urologists caring for patients with VUR.
Multivariable analysis performed in those patients treated surgically found for every 10% increase in a surgeon’s percent of new patients treated with Deflux (D/P), there was a 2.2-fold increased odds of a patient receiving Deflux injection over reimplantation (p<0.001). Similarly, for every 10% increase in a surgeon’s percent of new patients treated with reimplantation (R/P), there was a 64% increased odds of receiving a reimplant over Deflux (P= 0.001). Furthermore, for each additional year of patient age, there was an associated 42% increased odds of receiving Deflux over reimplantation (p<0.001) (Table 5). Male gender was associated with an 8-fold lower odds of receiving Deflux over reimplantation (P = 0.001). A surgeon’s percentage of new patients treated with Deflux (D/P) was ranked first, gender was ranked second and age was ranked third in variable importance affecting treatment choice. Lastly, non-white race was associated with a 3-fold lower odds of Deflux rather than reimplantation when compared to white patients (P = 0.032).
Table 5.
Logistic Regression Analysis of Probability of Deflux vs. Reimplantation in Patients Who Received Treatment
| Variable | OR | P-Value | 95% Confidence Interval for OR | Variable Importance Rank* |
|---|---|---|---|---|
| D/P | 1.08 | <0.001 | (1.05, 1.11) | 1 |
| Gender: Female (Referent) | 1.00 | - | - | 2 |
| Male | 0.12 | 0.001 | (0.03, 0.44) | |
| Age (Years) | 1.42 | <0.001 | (1.17, 1.73) | 3 |
| R/P | 0.95 | 0.001 | (0.92, 0.98) | 4 |
| Race: White (Referent) | 1.00 | - | - | 5 |
| Non-White | 0.32 | 0.032 | (0.11, 0.91) | |
| Region: Midwest (Referent) | 1.00 | - | - | 6 |
| Northeast | 0.31 | 0.283 | (0.04, 2.63) | |
| South | 0.93 | 0.911 | (0.26, 3.31) | |
| West | 2.50 | 0.321 | (0.41, 15.3) | |
| Insurance Type: Commercial (Referent) | 1.00 | - | - | 7 |
| Medicaid or Self Pay | 1.32 | 0.562 | (0.52, 3.34) | |
| All Other | 2.87 | 0.266 | (0.45, 18.3) | |
| Nephropathy: No (Referent) | 1.00 | - | - | 8 |
| Yes | 0.99 | 0.984 | (0.23, 4.15) | |
| Bilateral Procedure: No (Referent) | 1.00 | - | - | 9 |
| Yes | 1.04 | 0.928 | (0.42, 2.61) |
Based on average reduction in deviance when covariates added to model sequentially, averaged over 1000 randomly sampled permutations of variable ordering.
Discussion
To our knowledge, the current study is the first analysis attempting to identify management patterns of urologists treating children with VUR. Ferrer et al evaluated 155 surveys from pediatric urologists and found general agreement in the diagnostic workup of VUR patients and those with febrile UTIs, however, the indications for treatment were not as clear.10 While common reasons to choose surgical intervention include severity and frequency of UTI, renal scarring, and persistence of reflux, no standard algorithm has been accepted. Furthermore, the choice of endoscopic or open surgical intervention lacks a specific algorithm and leaves the recommended procedure to each surgeon. Our findings demonstrate that surgeons indeed differ greatly in their utilization of surgery for reflux. Our analysis presents true practice patterns in contrast to survey-based studies that rely upon opinion and memory.
Our results should be interpreted in light of limitations. Most important is the absence of radiographic reflux grade, which is a major determining factor in VUR management. However, in our experience, the distribution of reflux grades between surgeons do not show significant variability. Moreover, our analysis of individual surgeons excludes institutional bias. Second, UTI frequency and severity were unavailable. Similar to VUR grade, it is assumed that for these large academic pediatric practices, there is a common distribution of UTI frequency. Third, patients who were seen by providers who do not choose surgery type, such as nurse practitioners or pediatric nephrologists, were not captured. Fourth, it is important to note that patients included in this study were referred with the diagnosis of reflux and therefore excludes patients who may have acquired the diagnosis while under the care of the urologist. Finally, coding differences, omissions or inaccuracies may confound the data from this billing database. Databases that draw from billing (CPT) sources, such as FPSC, tend to be more accurate than administrative, non-billing, databases that use ICD-9 diagnosis and procedural codes.
Variations in treatment patterns depend on patient and surgeon factors. Figures 2 and 3, and Table 2 illustrate the marked variability between surgeons yet relative consistency of each individual surgeon from year to year. There was wide variation in surgical utilization between surgeons (mean 50%) but minimal change for each surgeon (5%) over the 3-year period. This suggests that surgeons are practicing based on their past tendencies more than a shared consensus practice pattern.
A study by Routh et al found that in 11,415 pediatric patients, those who received Deflux surgery instead of ureteral reimplantation were older, female, white, and publicly insured.11 Similarly, reflux grade was not available in their database (Pediatric Health Information System). They found hospital type, academic and metropolitan, was the most important predictor of procedure choice but they lacked data on individual providers. Similar to Routh’s study, we found that white patients, older patients, and females were more likely to receive Deflux. Unique to our study is that a surgeon’s historical practice pattern was the most important and significant predictor of whether a patient would receive Deflux. Our results, along with those by Routh et al draw the same conclusion that VUR management and type of surgical management in particular are highly variable between providers.11 Provider preference plays a major role in treatment type and may have more importance than patient factors.
Outcome studies in adult urology have found similar phenomena. Pollack et al utilized the SEER-Medicare database to characterize practice patterns among 3 U.S. cities.2 They found widely varied rates of prostatectomy utilization, racial, ethnic and socioeconomic composition of patients. Poon et al found that surgeons who practice in large population areas were more likely to place male slings for incontinence and those at academic institutions were more likely to place artificial urinary sphincters.3 Lane et al found surgeon volume, fellowship training, and proportionate use of robotic surgery were associated with higher partial nephrectomy implementation in adults.4 These studies, along with the present one, demonstrate the large role that surgeon preference plays in patient management.
In the analysis of surgical vs. non-surgical management of reflux, it is not surprising that increasing age was a significant predictor of surgery and ranked first in variable importance. This is consistent with the general management of VUR patients who do not have spontaneous resolution. Szymanski et al found higher age at presentation to be an independent predictor of ureteral reimplantation.12 They also found that patients followed for antenatal hydronephrosis, bilateral reflux and high-grade reflux were independent predictors of ureteral reimplantation. In addition to patient characteristics we found that surgeon characteristics predict surgical treatment. AVUR patient has increased odds of having surgical treatment for every incremental increase in a surgeon’s historical rate of reimplantation (R/S) and Deflux injection utilization (D/P).
In the analysis of type of anti-reflux surgery, higher odds of Deflux was associated with a surgeon’s historic Deflux utilization (D/P) and similarly, higher odds of reimplantation was associated with a surgeon’s reimplant utilization (R/P) (Table 5). This strongly suggests that a surgeon’s past practice predicts their future choices. In our analysis, a surgeon’s historic percentage of new patients treated with Deflux (D/P) bears greater importance than other independently significant predictors that we analyzed, including gender and age, in choice of treatment. The findings that female gender and white race independently predicted greater odds of Deflux over reimplantation were unexpected.
Conclusion
As expected, age was independently associated with surgical treatment of reflux. Surprisingly, female gender and white race were independently associated with endoscopic treatment and a surgeon’s historic Deflux utilization was the most important predictor of surgery type. Although data on reflux grade was not available, these results combined with the finding that the majority of surgeons had minimal change in their Deflux utilization suggest that surgeon preference is the first or second most critical factor in determining a patient’s treatment.
Acknowledgments
Funding source: The project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, #UL1 TR000002.
UHC-AAMC Faculty Practice Solutions Center and David Troland, Manager -Physician Services Analytics, as well as Ayan Patel, UC Davis Clinical and Translational Science Center, provided assistance with data acquisition and management.
Abbreviations
- VUR
vesicoureteral reflux
- D/S
Percentage of surgical patients treated with Deflux
- R/S
percentage of surgical patients treated with reimplantation
- D/P
percentage of new patients treated with Deflux
- R/P
Percentage of new patients treated with reimplantation
- D/P + R/P
percentage of new patients treated with any surgery
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Lendvay TS, Sorensen M, Cowan CA, Joyner BD, Mitchell MM, Grady RW. The evolution of vesicoureteral reflux management in the era of dextranomer/hyaluronic acid copolymer: a pediatric health information system database study. The Journal of urology. 2006 Oct;176(4 Pt 2):1864–1867. doi: 10.1016/j.juro.2006.04.088. [DOI] [PubMed] [Google Scholar]
- 2.Pollack CEWG, Bekelman J, Liao KJ, Armstrong K. Physician Social Networks and Variation in Prostate Cancer Treatment in Three Cities. Health Serv Res. 2012;47(1 Pt 2):380–403. doi: 10.1111/j.1475-6773.2011.01331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poon SA, Silberstein JL, Savage C, Maschino AC, Lowrance WT, Sandhu JS. Surgical practice patterns for male urinary incontinence: analysis of case logs from certifying American urologists. The Journal of urology. 2012 Jul;188(1):205–210. doi: 10.1016/j.juro.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lane BRGS, Eggener S, Tobert CM, Kahnoski RJ, Kutikov A, Smaldone M, Whelan CM, Shalhav A, Uzzo RG. Differential Use of Partial Nephrectomy for Intermediate and High Complexity Tumors May Explain Variability in Reported Utilization Rates. The Journal of urology. 2013 doi: 10.1016/j.juro.2013.01.007. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Silberstein JL, Poon SA, Maschino AC, et al. Urinary Diversion Practice Patterns Among Certifying American Urologists. The Journal of urology. 2012 Sep 23; doi: 10.1016/j.juro.2012.08.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. [Google Scholar]
- 7.Kruskal W. Relative importance by averaging over orderings. The American Statistician. 1987;41:6–10. [Google Scholar]
- 8.McCullagh PNJ. Generalized Linear Models. 2. 1989. [Google Scholar]
- 9.Kruskal W. Concepts of relative importance in recent scientific literature. The American Statistician. 1989;43:2–6. [Google Scholar]
- 10.Ferrer FA, McKenna PH, Hochman HI, Herndon A. Results of a vesicoureteral reflux practice pattern survey among American Academy of Pediatrics, Section on Pediatric Urology members. The Journal of urology. 1998 Sep;160(3 Pt 2):1031–1037. doi: 10.1097/00005392-199809020-00019. [DOI] [PubMed] [Google Scholar]
- 11.Routh JC, Nelson CP, Graham DA, Lieu TA. Variation in surgical management of vesicoureteral reflux: influence of hospital and patient factors. Pediatrics. 2010 Mar;125(3):e446–451. doi: 10.1542/peds.2009-1237. [DOI] [PubMed] [Google Scholar]
- 12.Szymanski KM, Oliveira LM, Silva A, Retik AB, Nguyen HT. Analysis of indications for ureteral reimplantation in 3738 children with vesicoureteral reflux: a single institutional cohort. Journal of pediatric urology. 2011 Dec;7(6):601–610. doi: 10.1016/j.jpurol.2011.06.002. [DOI] [PubMed] [Google Scholar]