Abstract
Sudden infant death syndrome (SIDS) and other sleep-related infant deaths, such as accidental suffocation and strangulation in bed and ill-defined deaths, account for >4000 deaths annually in the USA. Evidence-based recommendations for reducing the risk of sleep-related deaths have been published, but some caregivers resist adoption of these recommendations. Multiple interventions to change infant sleep-related practices of parents and professionals have been implemented. In this review, we will discuss illustrative examples of safe infant sleep interventions and evidence of their effectiveness. Facilitators of and barriers to change, as well as the limitations of the data currently available for these interventions, will be considered.
Keywords: Infant mortality, intervention, sleep safety, sudden infant death syndrome
INTRODUCTION
Sudden infant death syndrome (SIDS) and other sleep-related infant deaths, such as accidental suffocation and strangulation in bed and ill-defined deaths, are collectively known as sudden and unexpected infant death (SUID) and account for >4000 deaths annually in the USA [1]. While the “Back to Sleep” public awareness campaign, which began in 1994 and has been superseded by the “Safe to Sleep” campaign, is credited with decreasing rates of prone infant sleeping leading to reductions in mortality rates from SIDS/SUID, these decreases have plateaued in the past decade [2]. Some caregivers, including parents, relatives, child care providers, and health care professionals, continue to resist adoption of safe infant sleep recommendations, such as placing infants supine, avoidance of smoke exposure, avoidance of parent-infant bedsharing, and avoidance of soft bedding (including blankets, pillows, and bumper pads) [3-5]. In an effort to change infant sleep-related practices of parents and professionals, multiple interventions have been implemented. These efforts to effect change have been directed at multiple levels, from infant caregivers to state legislation, and can be viewed in the context of health behavior change models and theories.
One frequently used model, by Grol and colleagues, outlines barriers and incentives that should be considered when attempting to change behavior [6]. Grol emphasizes that a number of factors, such as the innovation itself and how it can be presented in a manner that makes it attractive or accessible, should be considered when developing interventions. If the innovation is that all newborns sleep in the supine position, it is important to consider what will make this innovation attractive or accessible to parents and healthcare providers. Further, to be successful, it is important to consider all levels of influence, including the infant caregiver, the healthcare provider, and the social, organizational, economic and political contexts. Interventions to effect behavior change that improves infant sleep safety can be seen in the context of Grol’s conceptual framework [6] (Table 1). In general, there are 5 categories of safe sleep interventions: 1) Health messaging (the Innovation), 2) Education of professionals (Individual professionals), 3) Breaking down barriers (Infant caregiver), 4) Culture and tradition (Social context), and 5) Legislation and regulation (Organizational, economic and political context).
Table 1. Barriers to and incentives for behavior change (adapted from Grol[6]), as they pertain to safe infant sleep practices.
| Level | Barriers/Incentives | Examples of barriers specific to infant sleep practices |
|---|---|---|
| Innovation | Advantages in practice, feasibility, credibility, accessibility, attractiveness, personal relevance | • Parents do not understand rationale for back sleep position • Parents feel that infant is “immune” to SIDS • Parents believe that recommended sleep practices will place baby at risk (e.g., choking) |
| Individual professional (Healthcare provider) | Awareness, knowledge, attitude, motivation to change, behavioral routines | • Healthcare provider does not believe that babies should sleep supine • No standard of care for infant sleep practices in hospital or daycare center |
| Breaking down barriers (Infant caregiver) | Knowledge, skills, attitude, compliance | • No money to buy crib • Concern that infant will be uncomfortable without blankets • Maternal smoking during and after pregnancy |
| Culture and tradition (Social context) | Opinion of colleagues, cultural norms, collaboration, leadership | • Bedsharing is family or cultural norm • Elder family members are trusted sources of information and may encourage prone positioning • Parents often receive unsafe bedding as gifts for baby |
| Legislation and regulation (Organizational, economic, and political context) | Organization of care processes, staff, capacities, resources, structures; financial arrangements, regulations, policies | • No safe sleep regulations in child care • No safe sleep education given at birth hospitals |
The purpose of this review is to discuss illustrative examples of interventions to influence caregivers’ behaviors to create a safe infant sleep environment and evidence of their effectiveness. We will first discuss challenges in determining effectiveness of an intervention and then consider examples of interventions in each of the 5 categories.
CHALLENGES IN DETERMINING EFFECTIVENESS OF AN INTERVENTION
Effectiveness of an intervention is often difficult to determine. The “gold standard” is the randomized controlled trial (RCT), in which a cohort of participants is randomly assigned to an intervention or a control/comparison group. The RCT is considered to be the strongest and most reliable evidence for effectiveness [7], as the random selection of participants minimizes bias, and the study design is most likely to ascertain whether the intervention caused the desired effect or not. However, there are limitations to the use of RCTs, particularly with regards to SIDS/SUID interventions. First, RCTs are expensive and often time-consuming to conduct. Without substantial funding, it is difficult to conduct an RCT, and few RCTs in the topic area of SIDS/SUID have been conducted. Secondly, some RCTs cannot be conducted because of ethical reasons. For example, one cannot randomize infants to either sleep prone or sleep supine and then measure outcomes. Thirdly, the generalizability of RCT results may be limited. For instance, an RCT that demonstrates effectiveness in Australia may not be effective in the U.S. Finally, if the ultimate outcome measure is an event that occurs infrequently in the population (such as SUID, with rates in developed countries ranging from 0.2-1.0/1000 live births) [8], an RCT would require an impractically large sample size. Thus, RCTs pertaining to SIDS/SUID have used alternative outcome measures, such as changes in practice (e.g., smoking cessation, observed positioning of infants for sleep).
Due to these challenges, the majority of SIDS/SUID interventions are not RCTs, but observational studies, in which an intervention is implemented, and outcomes after the intervention are measured and often compared with outcomes before the intervention. These types of evaluation, although they provide evidence for effectiveness of an intervention, are considered to be of weaker design than the RCT, as there may be confounding factors or events (e.g., media attention to a prominent member of the community whose infant died from SIDS) occurring simultaneously with the intervention that can impact the outcome measures. In addition, as participants are not randomized to the intervention or comparison group, it is difficult to attribute causality. For example, if pacifiers are provided to a cohort of families and there is a subsequent increase in pacifier use, it is difficult to ascertain whether the increased pacifier use is because of the intervention or because that particular cohort of families would have given their infant a pacifier anyway.
Furthermore, in determining how to measure effectiveness, one also needs to consider the ultimate goals of the intervention. Most would consider a decrease in SIDS/SUID deaths as an ultimate goal. And indeed, many studies report effectiveness based on decreased numbers of deaths. However, in addition to the aforementioned caveat about the sample size required to determine the impact on a low-frequency event, such as SIDS/SUID, using the number of deaths as an outcome measure is not sufficient; the size of the denominator, i.e., the size of the population in which the deaths can occur, is important as well. Infant mortality statistics are described in rates, usually the number of infant deaths per 1000 live births. The number of live births provides the denominator, without which one cannot ascertain whether a decrease in the absolute number of deaths is significant or not.
Another ultimate goal of these interventions may be an increased proportion of the population adhering to safe sleep recommendations. There are difficulties in this strategy as well. The preferred approach would be to conduct unannounced direct observations of behavior. This approach is most feasible when the persons being observed are in a circumscribed setting, such as a hospital. However, unannounced observations in other settings, such as child care sites and homes, are more challenging to accomplish. Therefore, most researchers have used proxy measures, such as surveys in which respondents report their knowledge, attitudes, intentions, and behaviors. Many interventions have used a pre- and post-intervention design, comparing knowledge, attitudes, and intentions before and after an intervention. One limitation of this approach is that the survey is often conducted soon after the intervention, and it is difficult to know if these results are sustained. In addition, participants may be reluctant to be forthcoming about their true attitudes and intentions in any survey, if these are inconsistent with what is perceived to be desired behavior. Finally, attitudes and intentions may not be predictive of actual behavior because of unanticipated barriers. A parent, after participating in a safe sleep discussion, may know that she should place the infant on the back and may intend to do that, but opposition from her partner or mother may prevent her from changing her behavior. Thus, measurements of attitudes and intentions may not correlate well with actual behavior – and, at worst, may only be a reflection of the participants’s knowledge of the outcome desired by those implementing the intervention.
With these challenges in mind, we will now discuss the five broad categories of interventions outlined above, along with specific examples.
INTERVENTIONS FOCUSED ON HEALTH MESSAGING
“Sound bites,” which try to convey an entire message in a few seconds, are frequently used for health messaging and branding, but are often inadequate as the entire health message. For instance, “Back to Sleep” conveys the message that infants should be placed on their back to sleep, and that everyone can then go back to sleep. However, many families have questions [3, 9-11]: Won’t my baby choke if she’s on her back? Won’t he sleep longer if he’s on his stomach? Why is back sleeping so important? How does it work? People are more likely to follow a health recommendation if they understand the rationale [12]. Thus, the first concept behind health messaging interventions is to answer questions that pose a barrier to adherence. Additionally, some parents consider their infants as being “immune” to SIDS or a sleep-related death, because this tragedy only happens to others [12]. The Health Belief Model states that one’s assessment of personal risk of a disease directly impacts on the likelihood of adherence to a behavioral change [13]. Thus, the second concept behind health messaging interventions is to provide messages that promote the realization that every infant is potentially at risk. The goal is to sell the innovation by making it credible, feasible, and a priority.
Most interventions use the traditional format of an educational session to answer frequently asked questions about safe sleep practices. A Washington, DC intervention with low-income mothers used 15-minute sessions focusing on parental concerns, such as aspiration/choking if the infant is supine, infant comfort (i.e., the infant will not sleep as long if supine), and parental belief that bedsharing is the best way to maintain vigilance over the infant while sleeping. A randomized controlled trial demonstrated that, when compared with a control group of parents 6 months after the intervention, parents attending the educational session were more likely to place their infants on the back (75% vs 45%, p<0.0001), less likely to bedshare (16% vs 44.2%%, p<0.0001), less likely to cite infant comfort as a reason for sleep position (14.5% vs 29.2%, p<0.0001), and more likely to be aware of recommendations to place infants supine (72.4% vs 38.9%%, p<0.0001) [14]. Such interventions can have a sustained impact. One randomized controlled trial in Porto Alegro Brazil found that mothers who received individual education about safe sleep were 2.2 times more likely to be placing their infants supine at 3 months of age [15].
B’more for Healthy Babies is a public health campaign in Baltimore, Maryland. The city Department of Health, in an analysis of sudden unexpected infant deaths (SUIDs), found that 85% of infants died while outside of the crib or bassinet, and that 78% died while bedsharing. The city thus began a public service campaign with a compelling video entitled, “SLEEP SAFE: Alone, Back, Crib. No Exceptions,” which features testimonials from 3 Baltimore parents who have lost babies while bedsharing, interspersed with additional information from parents and health professionals. By featuring local families, the video reinforces the idea that infants are not “immune” to SIDS/SUID and that safe sleep practices are relevant for all families. The video is shown to all mothers who give birth in one of the 7 birth hospitals in Baltimore, and B’more for Healthy Babies has expanded its reach by showing the video in places such as WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) sites, city detention centers, Department of Social Services offices, and jury duty locations. The campaign has created additional videos specifically targeting fathers, grandparents, and Spanish speakers. Preliminary results show that, since the SLEEP SAFE campaign began in 2010, the rate of infant sleep-related deaths has decreased by 46% (Stephanie Regenold, personal communication, 2014). Other jurisdictions have also begun to utilize videos to educate families. Westchester Medical Center in New York state surveyed new mothers after they viewed an educational video on safe infant sleep practices. They found that mothers who viewed the video were less likely to intend to place their infants on the side for sleep than those who did not view the video (7.1% vs. 23.9%, p<0.05) [16].
“Scary” health messages are a frequently used intervention. These campaigns attempt to increase perception of individual risk with the implied message that horrible things will happen if recommendations are not followed. Scary health messages, with images of diseased lungs, or a dead person in a morgue, have frequently been used in efforts to curb cigarette smoking [17]. The Milwaukee Wisconsin Department of Health took this approach with safe infant sleep messaging. The city’s rates of infant deaths associated with bedsharing were extremely high and increasing, and the Department of Health developed a campaign that showed photographs of an adult bed with a tombstone as the headboard (“For too many babies last year, this was their final resting place.” January 2010) and an infant lying in an adult bed alongside a butcher knife (“Your baby sleeping with you can be just as dangerous.” November 2011). This campaign received a great deal of publicity and generated much controversy. No formal evaluation of effectiveness has been conducted; however, the Department of Health reported that requests for free cribs increased from 671 in 2009, a year before the first advertisements, to 1604 in 2010 and 2043 in 2011 after the campaign began. The number of cribs distributed dropped after the second, most controversial advertisement but was still higher than baseline. The assessment of city health officials was that the number of cribs distributed was not associated with the level of controversy of the advertisements, but with the increase in awareness of the unsafe sleep environment (Erica S. LeCounte, MPH, City of Milwaukee Health Department, personal communication, 2015).
INTERVENTIONS FOCUSED ON EDUCATION OF PROFESSIONALS
Interventions focused on professionals train them to provide both safe sleep messages and appropriate role modeling for families, as there continues to be much resistance to safe sleep guidelines amongst professionals [18-21]. Healthcare professionals and child care providers have concerns similar to those expressed by parents, including concerns about the risk of aspiration or diminished sleep quality while supine [18-21] and may lack confidence when speaking to parents about these issues [22]. Professional educational interventions have most commonly, but not exclusively, targeted healthcare professionals; however, others have targeted child care providers and first responders. These interventions are aimed at facilitating behavior change at both the individual provider and the organizational context levels. They increase knowledge and awareness among providers, while also creating a culture of infant sleep safety, with a consistent standard of care expected of all staff members.
Nursing staff at birth hospitals are responsible for much of the initial education that new parents receive about safe sleep. In addition, staff practice is closely observed by parents. If healthcare professionals are observed placing an infant in a non-supine position, parents may assume that supine positioning is not important and are more likely to use a non-supine position for their infant at home even when advised otherwise [23]. Indeed, one study found that parents who reported seeing hospital personnel placing infants on the side were most likely to place their infant in the prone position [23]. Investigators at Yale-New Haven Hospital noted that only 20% of newborn infants were placed in the supine position. Therefore, all nursing personnel in the well-newborn nursery were required to attend a 30-minute educational session about SIDS and safe sleep recommendations, which explicitly addressed concerns about choking and aspiration in the newborn period. The importance of modeling recommended behavior was emphasized. The intervention was effective in altering healthcare professional behavior, such that 99% of infants were in the supine position in unannounced audits 3 months after the intervention. Parents were also 12 times more likely to report after the intervention that they observed nursery staff exclusively using the supine position [24].
Infants who require intensive care after birth are at higher risk for SIDS, particularly if they are born prematurely or have low birth weight [25, 26]. Further, infants who require intensive care are often placed prone to improve respiratory mechanics while being mechanically ventilated [27, 28], and are more likely to be placed prone after hospital discharge [29]. However, the risk of SIDS with prone positioning may be higher for infants born prematurely [30]. The AAP has recommended that preterm infants be placed routinely in the supine position by the time that they are 32 weeks postmenstrual age [31], so that they can become accustomed to supine sleeping before discharge. To emphasize this practice, researchers at Children’s Mercy Hospital (Kansas City, Missouri) implemented a safe sleep educational model in their neonatal intensive care unit (NICU), consisting of a NICU Safe Sleep policy, educational updates, safe sleep packet with video for families, and wearable blankets instead of receiving blankets. In addition, data from unannounced observations, using a safe sleep observation checklist, were collected and shared with staff. Use of a safe sleep environment increased from 21% to 88% after the intervention [32].
Quality improvement (QI) programs are used by most hospitals to systematically and continuously implement small, incremental changes in policy and practice, such that changes lead to measurable improvements in healthcare delivery and outcomes [33]. The goal is to standardize and improve care so that it is more efficient and effective. The cornerstone of many QI programs is the Model for Improvement (Fig. 1) [34], which uses the Plan-Do-Study-Act (PDSA) cycle: Once a practice needing improvement is identified, staff create a PLAN for a small, incremental change. Staff then make the change in their practice (DO) and STUDY the results of this change by assessing through observational audits whether there is an improved outcome. Finally, the staff ACT by discussing what worked and didn’t work, and develop a new PLAN. The cycle thus repeats itself on a continuous basis. PDSA cycles are generally rapid cycles, with observational audits occurring on a weekly or biweekly basis. Recently, hospitals have been using QI methodology to improve safe infant sleep practices [35]. For example, staff may report that 60% of infants have thick blankets in their bassinets. The PLAN may be to coach nurses on strategies to talk to parents about the dangers of thick blankets. The nurses then use these strategies for 1 week (DO), followed by observational audits to determine if there is a change (STUDY). Finally, the team discusses what worked and what didn’t (ACT), modifies the plan to achieve a better result, and the cycle starts again. One study reported that using QI methodology in a NICU resulted in increases in supine positioning (from 39% to 83%, p<0.001) and firm sleep surfaces (from 5% to 96%, p<0.001), and decreases in soft objects in the infant sleep area (from 45% to 75%, p=0.001). Parental adherence with safe sleep practices after NICU discharge also improved from 23% to 82% (p<0.001) [36].
Fig. (1).
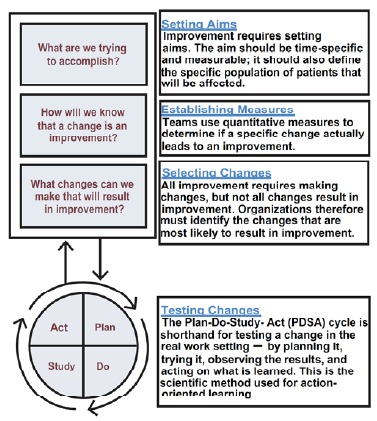
Model for Improvement, adapted from Institute for Health Care Improvement and the Health Resources and Services Administration [34].
Another strategy that uses QI methodology is the tracking of sentinel events in hospitals. A sentinel event is “an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof” [37]. Each sentinel event triggers a focused review and a Root Cause Analysis: What went wrong here? How can we prevent this from occurring again? MedStar Franklin Square Medical Center (Baltimore, Maryland) considers any sleep-related infant death to be a sentinel event for the birth hospital. It is unusual for a U.S. birth hospital to have access to any future outcomes data on infants that were born at that specific hospital. This is particularly true in cities, where pediatric emergency departments are likely to be in children’s hospitals, which do not have delivery facilities or newborn nurseries. Thus, if an infant dies, the newborn nursery staff will likely never be notified. In Baltimore, all infant deaths occurring after nursery discharge are tracked by the Child Death Review Team, and feedback is provided to the birth hospital staff. Since 2007, MedStar Franklin Square Medical Center has conducted a Root Cause Analysis after each death, with continuous QI through PDSA cycles. Several changes in protocol have resulted from these PDSA cycles. All parents of newborns now receive sleep safety education and sign a commitment statement that their infant will be placed in a safe sleep position; all nurses, non-professional staff, and physicians are trained in safe infant sleep practices; and there are periodic, unannounced “bed checks” to assess infant sleep position and location. In addition, a safe sleep video is available 24 hours a day on the Baby Channel, which is freely available to all hospital patients. The goal of the continuous QI is that all families receive consistent safe sleep messaging. They are beginning to see an impact from their efforts; between October 2011 and June, 2013, there were no sleep-related deaths reported among their discharged newborns. (Scott Krugman, MD, personal communication, 2015).
Another approach for achieving a culture of infant sleep safety within hospitals is to provide rewards for hospitals that do so. Cribs for Kids® and Halo Innovations are collaborating on the National Safe Sleep Hospital Initiative. This Initiative provides materials for educating staff and families, and hospitals can document compliance with the program online. Hospitals are Safe Sleep Certified when they meet specific requirements, such as developing safe sleep policy statements, training staff on safe sleep, and participating in continuous quality improvement in safe sleep. Hospitals can qualify for Safe Sleep Certification at 3 levels: Certified Safe Sleep Hospital, Certified Safe Sleep Leader, and Certified Safe Sleep Champion. This program is beginning in Ohio, and there are plans for expansion to all 50 states in the U.S. (Michael Goodstein, personal communication, 2015).
Several professional educational interventions have also focused on child care providers. One randomized controlled trial of licensed child care centers and family child care homes has been published.[18] In this trial, child care providers underwent direct observations of sleep practices within their child care sites and then were randomized to receive the American Academy of Pediatrics safe sleep curriculum, either before (intervention group) or after (control group) a second direct observation. A total of 264 programs, with 1212 providers, completed the study. Knowledge about the supine recommendation increased from 60.0% at baseline to 70.4% in the control group and 80.5% in the intervention group. The percentage of programs reporting exclusive use of the supine position increased from 65.0% to 70.4% in the control group (p=0.01) and 87.8% in the intervention group (p<0.001). Observed supine placement increased from 51.0% to 57.1% for the control group (not significant) and to 62.1% for the intervention group (p<0.01). The curriculum is available online in English and Spanish [38].
The DOSE:Direct On-Scene Education™ program in Florida was launched in April 2012 as a collaboration between Healthy Mothers, Healthy Babies Coalition of Broward County and Fort Lauderdale Fire Rescue to address the issue of sleep-related infant deaths. First responders for 911 emergency calls are trained in safe infant sleep and provide safe sleep education to families. A first responder assesses every home that is entered after any 911 call: is there an infant? What is the sleep environment? If there is a 911 call for a 65-year-old woman with chest pain, the team, while responding to the call, will also assess the home for the presence of an infant and the sleep environment and provide a “Safe to Sleep Survival Kit.” Thus far, >1500 first responders have been trained, and >1200 Safe to Sleep Survival Kits distributed by first responders. In Broward County in 2013, 15 families with no crib in the home were identified, and 14 accepted a portable crib from the local Cribs for Kids® program. Furthermore, the number of sleep-related infant deaths in this EMS (Emergency Medical Service) area has gone from the highest to the lowest in all of Broward County, Florida. The DOSE: Direct On Scene Education™ program is currently being expanded to additional states (Jennifer Combs, personal communication, 2015).
INTERVENTIONS FOCUSED ON BREAKING DOWN BARRIERS
There may be multiple potential barriers to adherence to safe sleep recommendations. For instance, financial inability to purchase a crib may lead to bedsharing. Smoking, alcohol use, and drug use, which increase the risk for SIDS, especially in combination with bedsharing, may be important coping mechanisms for parents. Cultural norms and family traditions, such as bedsharing or use of thick blankets, which are in conflict with safe sleep recommendations, may also pose barriers. Several interventions aim to understand and eliminate these barriers, thereby both increasing accessibility to the innovation and changing attitudes of the infant caregivers.
Cribs for Kids® provides free or reduced-cost cribs to families. There are >500 Cribs for Kids® partners throughout the US that provide a portable crib to low-income families who do not have a crib. Families receive the crib and a fitted crib sheet embossed with the safe sleep message, wearable blanket, pacifier, and safe sleep education, including brochures, a safe sleep refrigerator magnet, Safe Sleep for Your Baby DVD [39] (produced by NICHD), and a copy of the baby board book Sleep Baby Safe and Snug (see below). Since its inception in 1998, >300,000 safe sleep environments have been distributed. A survey of crib recipients found that 38% of infants would have slept in the adult bed with the parents if a crib had not been given to them [40]. Although Cribs for Kids® does not have national data, they report that in Alleghany County (Pittsburgh), Pennsylvania, >23,000 cribs have been distributed to low-income families since 1998. During that period of time, there has only been one sleep-related infant death among crib recipients. This infant was at the grandmother’s house without the portable crib and died while sleeping on the grandmother’s bed. Furthermore, the number of SUIDs in Alleghany County has decreased from 20 in 1998 to 6-9 annually (Judith Bannon, personal communication, 2015).
Bedtime Basics for Babies was a free crib and safe sleep educational intervention funded in Washington State, Indiana, and Washington, DC by First Candle and the Gates Foundation. A portable crib, crib sheet, wearable blanket, pacifier, and safe sleep education were provided to low-income families whose infants were at high risk for SIDS. Parents also viewed an informational video about safe infant sleep before being given the crib. Data were collected in 2010 and 2011. Parental knowledge about recommended infant sleep position improved from 76% to 94% (p<0.001), intended use of supine positioning increased from 80-84% to 87% (p<0.001), and bedsharing the night before decreased from 38% to 16% (p<0.001) [41].
The Halo® In-Hospital SleepSack Program provides free swaddle wearable blankets to hospital NICUs and well baby nurseries to replace traditional blankets. Thus far, >1300 hospitals in the U.S. and Canada, comprising approximately 1.8 million births annually, are participating in this program. Eighty percent of these hospitals offer the In-Hospital Modeling Program, using HALO® SleepSack® Swaddles instead of receiving blankets (Bill Schmid, personal communication, 2014).
In Scotland, >20% of pregnant women smoke, and fewer than 1 in 20 will quit [42]. As more than 50% of women eventually become pregnant [43], pregnancy provides an ideal opportunity to help women quit smoking. Smoking cessation has many positive benefits; it protects from SIDS, miscarriage, stillbirth, preterm births, and low-birth-weight infants [44]. It is estimated that one-third of SIDS deaths could be prevented if all maternal smoking during pregnancy were eliminated [45, 46]. In the Cessation in Pregnancy Incentives Trial (CPIT), a randomized controlled trial, pregnant smokers were randomized to receive usual care only or usual care in addition to up to 400 British pounds, divided into 4 payments for achieving specific goals: setting a quit date, and abstinence as demonstrated by expired air carbon monoxide level <10 parts/million at 4, 12, and 34-38 weeks gestation. 23% of participants in the intervention group quit smoking, compared to 9% in the control group [47].
INTERVENTIONS FOCUSED ON UTILIZING CULTURE AND TRADITION
One of the tenets of culturally-competent practice is to utilize traditions and norms that are protective for health. There are a growing number of Interventions that take incorporate cultural norms and family traditions (i.e., the social context) to encourage safe sleep practices.
Charlie’s Kids takes advantage of the age-old tradition of reading books with your children. Reading with your children beginning in infancy is associated with improved language skills and promotes parent-child bonding [48]. Charlie’s Kids has produced a board book for babies, entitled Sleep Baby Safe and Snug [49], which provides safe sleep messaging within the context of an easy-to-read story. Currently, the book is available in English and Spanish (Duerme bebe comodo y seguro); since June 2013, >400,000 books have been distributed in 33 states. Charlie’s Kids has collaborated with multiple organizations to provide Sleep Baby Safe and Snug to as many families as possible. A randomized controlled trial is being conducted, testing the effectiveness of the book vs. traditional safe sleep educational brochures in increasing knowledge and improving safe sleep practices (Samuel Hanke, personal communication, 2015).
Several communities are re-introducing traditional infant sleep areas as a strategy to increase safety when infants sleep in their parents’ beds. In New Zealand, where SUID rates are among the highest for developed countries [8], indigenous SUID rates are more than 4 times those in the European population [50], and deaths associated with bedsharing are common [50], two traditional sleep spaces have been introduced. The wahakura, which is a low-sided (6 inches tall) infant bed woven from flax, was traditionally used in the Maori (indigenous) communities (Fig. 2) and has been actively reintroduced and promoted. It is meant to be used wherever the infant sleeps, but is usually placed in the adult bed next to the parent as a separate infant sleep space within the adult bed. Preliminary results from a randomized controlled trial [51] suggest that rates of use, quantity and quality of maternal sleep, breastfeeding, and head covering events are similar for the wahakura and a standard bassinet placed next to the parents’ bed or in the parents’ room. A similar New Zealand product is the pēpi-pod (“pēpi” is the Maori word for “baby”), a portable plastic container fitted with a firm mattress and used as an infant bed that, like the wahakura, can be placed on the adult bed next to a parent (Fig. 3). The pēpi-pod was originally introduced as an emergency infant bed after the 2011 Christchurch earthquakes [52]. The wahakura and pēpi-pod are part of a national education program in New Zealand that promotes safe sleep among families at high risk for SUID. The program has been adopted by district health boards as a targeted approach for reducing sudden infant deaths and promoting infant health, especially in regions of New Zealand with more vulnerable populations. Receiving a portable sleep space comes with an expectation that recipients help spread awareness about safe sleep to others, and this has stimulated conversations about safe sleep within the local communities. There is some indication that there is a greater reduction in SUIDs in District health boards with pēpi-pod and wahakura programs, compared with those without such programs [53].
Fig. (2).
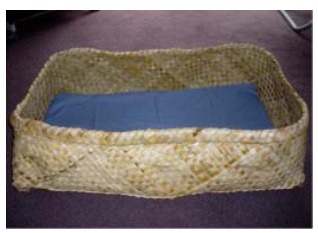
Wahakura, as used by the Maori (indigenous) communities in New Zealand.
Fig. (3).

New Zealand pēpi-pod (used with permission from Change for our Children).
Since 1938, every expectant mother in Finland has received a baby box as a gift from the government. This cardboard box contains a tightly fitting mattress and fitted sheet, clothing, and supplies for the infant’s first 6 months. In order for an expectant mother to be eligible to receive the baby box, she must begin attending prenatal visits before the fourth month of pregnancy. Many Finnish infants sleep in the box for the first few months, and it is considered by parents to be extremely practical, as it is portable. If it becomes soiled, it can be easily replaced [54]. At least one U.S. community (in Alaska) is now providing baby boxes to families who do not have cribs [55].
American Indian communities have the highest SUID rates in the country [56]. Although the reasons for this are not entirely understood, high rates of maternal smoking and bedsharing in these communities are likely strongly contributory [57, 58]. Efforts to modify these behaviors among young American Indian parents have largely been unsuccessful. The National Center for the Review and Prevention of Infant Deaths is collaborating with the International Association of Indigenous Aging to work with elders in several American Indian tribes in Michigan. The premise is that the elders in the community are trusted sources of information for parents. Elders learn about safe sleep messages, discuss how their own traditional practices align or do not align with these messages, and then develop strategies (such as talking circles and traditional craft making) to engage with young parents.
In many communities, it is traditional to celebrate the upcoming birth of an infant by having a party, called a “baby shower.” There are gifts for the expectant mother, customarily products that can be used for the infant, such as clothing, diapers, and feeding supplies. Bedding, including blankets and bumper pads, has been among the traditional gifts. A recent trend has been the themed baby shower, in which attendees provide gifts that pertain to the theme – e.g., a safety baby shower. The Kansas Infant Death and SIDS (KIDS) Network and Wichita Black Nurses Association have implemented Community Baby Showers in high-risk (largely African-American) communities. Pregnant women are invited to these baby showers by churches, clinics, physician offices, and media. The theme of the baby shower is safe sleep, and attendees receive safe sleep education and products to promote a safe sleep environment, including portable cribs and wearable blankets. Preliminary results show that attendance at a Community Baby Shower improves knowledge about safe sleep, and intention to provide a safe sleep environment [59]. The KIDS Network has expanded their Community Baby Showers to Spanish-speaking communities and, in collaboration with Kansas University School of Medicine-Wichita, to high-risk obstetrical and pediatric clinic settings (Christy Schunn, personal communication, 2015). A safe sleep baby shower gift list is also available in the book, 14 Ways to Protect Your Baby from SIDS [60].
INTERVENTIONS FOCUSED ON LEGISLATION AND REGULATION
The underlying concept for legislation and regulation, which targets the organizational, economic and political context, is that adherence to guidelines is more likely if mandated [61]. Most safe infant sleep legislation and regulation have focused on child care professionals. Approximately 20% of SIDS deaths in the U.S. occur in child care settings [62, 63], and unaccustomed prone positioning has been associated with these deaths[62]. After studies in the 1990’s demonstrated that 75% of child care providers were placing infants prone for sleep [64, 65], many states began implementing child care regulations regarding infant sleep position, infant sleep location, use of bedding, and prohibition of smoking[66]. Other states have required SIDS risk reduction training for all child care providers [66]. Currently, 43 states regulate infant sleep position and 17 require SIDS risk reduction training for providers at licensed child care centers. However, there is much variability in the requirements. With regards to sleep position, 10 require supine sleep position, 25 allow a physician waiver, 3 allow a physician or parent waiver, and 5 allow side or back positioning [67]. To date there has been no analysis of the effectiveness of these efforts in decreasing the proportion of infants who die in child care settings. In addition, these regulations are only applicable to child care providers who are subject to regulation, i.e., those who are licensed. At least 30% of family child care homes are unlicensed [68]. Further, relatives, friends, and nannies provide informal care, and this care is also unlicensed and unregulated. It is virtually impossible for regulatory and licensing agencies to identify and locate these unlicensed providers and provide educational information and training opportunities [63].
Other efforts at using legislation have targeted hospital care. In 2010, Pennsylvania passed the Sudden Infant Death Syndrome Education and Prevention Act (Act 73 of 2010), which mandates consistent infant safe sleep education in all birth hospitals. All parents must receive infant safe sleep information prior to hospital discharge and sign that they have received and understand the information. Preliminary data show that, while Act 73 has improved provision of safe sleep education to parents, this has not translated to behavior change by hospital personnel with regards to increased supine positioning of infants (many continue to use non-supine positions because of concerns about aspiration or choking) (Michael Goodstein, personal communication, 2015). Nonetheless, other states have passed (California, Connecticut, Nebraska, Illinois, Michigan, Texas, and Florida) similar legislation [69].
FUTURE DIRECTIONS AND CONCLUSIONS
Countless interventions to improve the sleep safety of infants have been implemented. It is important to consider the different levels of barriers to and incentives for behavior change when developing interventions. Using a multi-level approach is ideal and may be more effective than targeting one specific level. Despite the multiple challenges and limitations of intervention evaluation, evaluation is still important, as it provides details of the intervention that are helpful for others considering similar interventions. Particularly as the success of an intervention may be context-dependent, it is important and helpful for those who implement interventions to conduct formal program evaluations that include both quantitative and qualitative components so that processes are transparent and that interventions are more easily translated to other communities. Further, if an intervention is found to be effective, there is more likelihood of sustainability. Therefore, formal process evaluation and testing of effectiveness are critical if interventions are to become independently sustainable. Continued funding, sustainability, and expansion for such projects are most possible if effectiveness data are available. Although the RCT is the gold standard for determining effectiveness of an intervention, it is currently not feasible in many instances. In those cases, the most rigorous evaluation design possible should be implemented. Agencies funding interventions should also include funding to evaluate the interventions to ensure that they are completed.
ACKNOWLEDGEMENTs
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.United States Department of Health and Human Services (US DHHS), Centers of Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Office of Analysis and Epidemiology (OAE), Division of Vital Statistics (DVS), Linked Birth / Infant Death Records on CDC WONDER Online Database; Available from:http://wonder.cdc.gov/lbd.html.
- 2.Moon R.Y. American Academy of Pediatrics, Task Force on Sudden Infant Death Syndrome. Technical report-SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;129(5):e1341–e1367. doi: 10.1542/peds.2011-2285. [DOI] [PubMed] [Google Scholar]
- 3.Colson E.R., Rybin D., Smith L.A., Colton T., Lister G., Corwin M.J. Trends and factors associated with infant sleeping position: the national infant sleep position study, 1993-2007. Arch. Pediatr. Adolesc. Med. 2009;163(12):1122–1128. doi: 10.1001/archpediatrics.2009.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colson E.R., Willinger M., Rybin D., et al. Trends and factors associated with infant bed sharing, 1993-2010: the National Infant Sleep Position study. JAMA Pediatr. 2013;167(11) doi: 10.1001/jamapediatrics.2013.2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shapiro-Mendoza C.K., Colson E.R., Willinger M., Rybin D.V., Camperlengo L., Corwin M.J. Trends in infant bedding use: national infant sleep position study, 1993-2010. Pediatrics. 2015;135(1):10–17. doi: 10.1542/peds.2014-1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grol R., Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med. J. Aust. 2004;180(6) Suppl.:S57–S60. doi: 10.5694/j.1326-5377.2004.tb05948.x. [DOI] [PubMed] [Google Scholar]
- 7.Owens D.K., Lohr K.N., Atkins D., et al. Agency for Healthcare Research and Quality. Methods Guide for Comparative Effectiveness Reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Grading the Strength of a Body of Evidence When Comparing Medical Interventions. [PubMed] [Google Scholar]
- 8.Hauck F.R., Tanabe K.O. International trends in sudden infant death syndrome and other sudden unexpected deaths in infancy: need for better diagnostic standardization. Curr. Pediatr. Rev. 2010;6(1):95–101. [Google Scholar]
- 9.Colson E.R., Levenson S., Rybin D., et al. Barriers to following the supine sleep recommendation among mothers at four centers for the Women, Infants, and Children Program. Pediatrics. 2006;118(2):e243–e250. doi: 10.1542/peds.2005-2517. [DOI] [PubMed] [Google Scholar]
- 10.Colson E.R., McCabe L.K., Fox K., et al. Barriers to Following the Back-to-Sleep Recommendations: Insights From Focus Groups With Inner-City Caregivers. Ambul. Pediatr. 2005;5(6):349–354. doi: 10.1367/A04-220R1.1. [DOI] [PubMed] [Google Scholar]
- 11.Oden R., Joyner B.L., Ajao T.I., Moon R. Factors influencing African-American mothers' decisions about sleep position: a qualitative study. J. Natl. Med. Assoc. 2010;102(10):870–880. doi: 10.1016/s0027-9684(15)30705-7. [DOI] [PubMed] [Google Scholar]
- 12.Moon RY, Oden RP, Joyner BL, Ajao TI. Qualitative analysis of beliefs and perceptions about sudden infant death syndrome (SIDS) among African-American mothers: Implications for safe sleep recommendations. J Pediatr. 2010;157(1):92–97. doi: 10.1016/j.jpeds.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 13.Becker M.H. The health belief model and personal health behavior. Health Educ. Monogr. 1974;2(4) [Google Scholar]
- 14.Moon R.Y., Oden R.P., Grady K.C. Back to Sleep: educational intervention with Women, Infants, and Children program clients. Pediatrics. 2004;113(3):542–547. doi: 10.1542/peds.113.3.542. [DOI] [PubMed] [Google Scholar]
- 15.Issler R.M., Marostica P.J., Giugliani E.R. Infant sleep position: a randomized clinical trial of an educational intervention in the maternity ward in Porto Alegre, Brazil. Birth. 2009;36(2):115–121. doi: 10.1111/j.1523-536X.2009.00308.x. [DOI] [PubMed] [Google Scholar]
- 16.Canter J., Rao V., Patrick P.A., Alpan G., Altman R.L. The impact of a hospital-based educational video on maternal perceptions and planned practices of infant safe sleep. J. Spec. Pediatr. Nurs. 2015 doi: 10.1111/jspn.12114. [DOI] [PubMed] [Google Scholar]
- 17.Montazeri A., McEwen J. Effective communication: perception of two anti-smoking advertisements. Patient Educ. Couns. 1997;30(1):29–35. doi: 10.1016/s0738-3991(96)00958-5. [DOI] [PubMed] [Google Scholar]
- 18.Moon R.Y., Calabrese T., Aird L. Reducing the risk of sudden infant death syndrome in child care and changing provider practices: lessons learned from a demonstration project. Pediatrics. 2008;122(4):788–798. doi: 10.1542/peds.2007-3010. [DOI] [PubMed] [Google Scholar]
- 19.Moon R.Y., Oden R.P. Back to sleep: can we influence child care providers? Pediatrics. 2003;112(4):878–882. doi: 10.1542/peds.112.4.878. [DOI] [PubMed] [Google Scholar]
- 20.Lerner H., McClain M., Vance J.C. SIDS education in nursing and medical schools in the United States. J. Nurs. Educ. 2002;41(8):353–356. doi: 10.3928/0148-4834-20020801-08. [DOI] [PubMed] [Google Scholar]
- 21.Price SK, Gardner P, Hillman L, Schenk K, Warren C. Changing Hospital Newborn Nursery Practice: Results from a Statewide Back to Sleep" Nurses Training Program. Matern Child Health J. 2007 doi: 10.1007/s10995-007-0243-y. [DOI] [PubMed] [Google Scholar]
- 22.Cowan S., Pease A., Bennett S. Usage and impact of an online education tool for preventing sudden unexpected death in infancy. J. Paediatr. Child Health. 2013;49(3):228–232. doi: 10.1111/jpc.12128. [DOI] [PubMed] [Google Scholar]
- 23.Brenner R., Simons-Morton B.G., Bhaskar B., et al. Prevalence and predictors of the prone sleep position among inner-city infants. JAMA. 1998;280:341–346. doi: 10.1001/jama.280.4.341. [DOI] [PubMed] [Google Scholar]
- 24.Colson E.R., Joslin S.C. Changing nursery practice gets inner-city infants in the supine position for sleep. Arch. Pediatr. Adolesc. Med. 2002;156(7):717–720. doi: 10.1001/archpedi.156.7.717. [DOI] [PubMed] [Google Scholar]
- 25.Malloy M.H., Hoffman H.J. Prematurity, sudden infant death syndrome, and age of death. Pediatrics. 1995;96(3 Pt 1):464–471. [PubMed] [Google Scholar]
- 26.Sowter B., Doyle L.W., Morley C.J., Altmann A., Halliday J. Is sudden infant death syndrome still more common in very low birthweight infants in the 1990s? Med. J. Aust. 1999;171(8):411–413. doi: 10.5694/j.1326-5377.1999.tb123719.x. [DOI] [PubMed] [Google Scholar]
- 27.Baird T.M., Paton J.B., Fisher D.E. Improved oxygenation with prone positioning in neonates: stability of increased transcutaneous pO2. J. Perinatol. 1991;11(4):315–317. [PubMed] [Google Scholar]
- 28.Martin R.J., DiFiore J.M., Korenke C.B., Randal H., Miller M.J., Brooks L.J. Vulnerability of respiratory control in healthy preterm infants placed supine. J. Pediatr. 1995;127:609–614. doi: 10.1016/s0022-3476(95)70125-7. [DOI] [PubMed] [Google Scholar]
- 29.Vernacchio L., Corwin M.J., Lesko S.M., et al. Sleep position of low birth weight infants. Pediatrics. 2003;111(3):633–640. doi: 10.1542/peds.111.3.633. [DOI] [PubMed] [Google Scholar]
- 30.Oyen N., Markestad T., Skjaerven R., et al. Combined effects of sleeping position and prenatal risk factors in sudden infant death syndrome: the Nordic epidemiological SIDS study. Pediatrics. 1997;100(4):613–621. doi: 10.1542/peds.100.4.613. [DOI] [PubMed] [Google Scholar]
- 31.American Academy of Pediatric Committee on Fetus and Newborn Hospital discharge of the high-risk neonate. Pediatrics. 2008;122(5):1119–1126. doi: 10.1542/peds.2008-2174. [DOI] [PubMed] [Google Scholar]
- 32.Voos K.C., Terreros A., Larimore P., Leick-Rude M.K., Park N. Implementing safe sleep practices in a neonatal intensive care unit. J. Matern. Fetal Neonatal Med. 2014:1–4. doi: 10.3109/14767058.2014.964679. [DOI] [PubMed] [Google Scholar]
- 33.Institute of Medicine (IOM) Advancing quality improvement research: challenges and opportunities. Workshop summary. Washington, DC: The National Academies Press; 2007. [Google Scholar]
- 34.Model for Improvement.[cited 2014 October 27]. Available from:www.hrsa.gov/quality/toolbox/methodology/index.html.
- 35.Mason B., Ahlers-Schmidt C.R., Schunn C. Improving safe sleep environments for well newborns in the hospital setting. Clin. Pediatr. (Phila.) 2013;52(10):969–975. doi: 10.1177/0009922813495954. [DOI] [PubMed] [Google Scholar]
- 36.Gelfer P., Cameron R., Masters K., Kennedy K.A. Integrating “Back to Sleep”. RecommendationsInto Neonatal ICU Practice. Pediatrics; 2013. [DOI] [PubMed] [Google Scholar]
- 37.The Joint Commission Sentinel Event. Available from:http://www.jointcommission.org/sentinel_ event.aspx.
- 38.Healthy Child Care America website: http://www.healthychildcare. org/section_SIDS.cfm . 2004.
- 39.National Institute for Child Health and Human Development, Safe Sleep for Your Baby. Available from:https://www.youtube. com/watch?v=29sLucYtvpA.
- 40.Carlins E.M., Collins K.S. Cribs for Kids: risk and reduction of sudden infant death syndrome and accidental suffocation. Health Soc. Work. 2007;32(3):225–229. doi: 10.1093/hsw/32.3.225. [DOI] [PubMed] [Google Scholar]
- 41.Hauck F.R., Tanabe K.O., McMurry T., Moon R.Y. Evaluation of Bedtime Basics for Babies: A National Crib Distribution Program to Reduce the Risk of Sleep-Related Sudden Infant Deaths. J. Community Health. 2014 doi: 10.1007/s10900-014-9957-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.NHS Information Services Division Scotland, Maternity & Births: Publications. 2014 [cited 2014 October 27]; Available from:www.isdscotland.org/Health-Topics/Maternity-and-Births/Publications/ data-tables.asp. 2014.
- 43.Dye JL. Fertility of American Women: June 2008, Current Population Reports, in Current Population Reports2010; U.S. Census Bureau: Washington DC. 2008 [Google Scholar]
- 44.Best D. American Academy of Pediatrics Committee on Environmental Health, Committee on Native American Child Health, Committee on Adolescence. Technical Report--Second hand and Prenatal Tobacco Smoke Exposure. Pediatrics. 2009 [Google Scholar]
- 45.Mitchell E.A., Milerad J. Smoking and the sudden infant death syndrome. Rev. Environ. Health. 2006;21(2):81–103. doi: 10.1515/reveh.2006.21.2.81. [DOI] [PubMed] [Google Scholar]
- 46.Dietz P.M., England L.J., Shapiro-Mendoza C.K., Tong V.T., Farr S.L., Callaghan W.M. Infant morbidity and mortality attributable to prenatal smoking in the U.S. Am J. Prev. Med. 2010;39(1):45–52. doi: 10.1016/j.amepre.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Tappin D., Bauld L., Purves D., et al. Financial incentives for smoking cessation in pregnancy: randomised controlled trial. BMJ. 2015;350:h134. doi: 10.1136/bmj.h134. [DOI] [PubMed] [Google Scholar]
- 48.High P.C., Klass P. Literacy promotion: an essential component of primary care pediatric practice. Pediatrics. 2014;134(2):404–409. doi: 10.1542/peds.2014-1384. [DOI] [PubMed] [Google Scholar]
- 49.Hutton J. Sleep baby, safe and snug. Cincinnati: Blue Manatee Press; 2013. [Google Scholar]
- 50.Tipene-Leach D., Hutchison L., Tangiora L., et al. SIDS-related knowledge and infant care practices among Maori mothers. N. Z. Med. J. 2010;123(1326):88–96. [PubMed] [Google Scholar]
- 51.Tipene-Leach D., Baddock S., Williams S., et al. Methodology and recruitment for a randomised controlled trial to evaluate the safety of wahakura for infant bedsharing. BMC Pediatr. 2014;14(1):240. doi: 10.1186/1471-2431-14-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cowan S., Bennett S., Clarke J., Pease A. An evaluation of portable sleeping spaces for babies following the Christchurch earthquake of February 2011. J. Paediatr. Child Health. 2013;49(5):364–368. doi: 10.1111/jpc.12196. [DOI] [PubMed] [Google Scholar]
- 53.Statistics New Zealand.[cited 2014 October 31]; Available from:www.stats.govt.nz/infoshare/.
- 54.Lee H. Why Finnish babies sleep in cardboard boxes, in BBC News. 2013 [Google Scholar]
- 55.Demer L. 2015. [Google Scholar]
- 56.Wong C.A., Gachupin F.C., Holman R.C., et al. American Indian and Alaska Native Infant and Pediatric Mortality, United States, 1999-2009. Am. J. Public Health. 2014 doi: 10.2105/AJPH.2013.301598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Indian Health Service . Department of Health and Human Services, Regional differences in Indian health. Rockville, MD: Indian Health Service; 2003. [Google Scholar]
- 58.Lahr M.B., Rosenberg K.D., Lapidus J.A. Maternal-Infant Bedsharing: Risk Factors for Bedsharing in a Population-Based Survey of New Mothers and Implications for SIDS Risk Reduction. Matern. Child Health J. 2007;11(3):277–286. doi: 10.1007/s10995-006-0166-z. [DOI] [PubMed] [Google Scholar]
- 59.Ahlers-Schmidt C.R., Schunn C., Dempsey M., Blackmon S. Evaluation of community baby showers to promote safe sleep. Kansas J Med. 2014;7(1):1–5. [Google Scholar]
- 60.Moon RY, Hauck FR. Seattle: Parenting Press; Hauck. 14 Ways to Protect Your Baby from SIDS2011; [Google Scholar]
- 61.Gielen A.C., McDonald E.M., Gary T.L., Bone L.R. Using the PRECEDE/PROCEED model to apply health behavior theories. In: Glanz K., Rimer B.K., Viswanath K., editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. pp. 407–433. [Google Scholar]
- 62.Moon R.Y., Patel K.M., Shaefer S.J. Sudden infant death syndrome in child care settings. Pediatrics. 2000;106(2 Pt 1):295–300. doi: 10.1542/peds.106.2.295. [DOI] [PubMed] [Google Scholar]
- 63.Moon R.Y., Sprague B.M., Patel K.M. Stable prevalence but changing risk factors for sudden infant death syndrome in child care settings in 2001. Pediatrics. 2005;116(4):972–977. doi: 10.1542/peds.2005-0924. [DOI] [PubMed] [Google Scholar]
- 64.Gershon N.B., Moon R.Y. Infant sleep position in licensed child care centers. Pediatrics. 1997;100(1):75–78. doi: 10.1542/peds.100.1.75. [DOI] [PubMed] [Google Scholar]
- 65.Moon R.Y., Biliter W.M. Infant sleep position policies in licensed child care centers after back to sleep campaign. Pediatrics. 2000;106(3):576–580. doi: 10.1542/peds.106.3.576. [DOI] [PubMed] [Google Scholar]
- 66.Moon R.Y., Kotch L., Aird L. State child care regulations regarding infant sleep environment since the Healthy Child Care America-Back to Sleep campaign. Pediatrics. 2006;118(1):73–83. doi: 10.1542/peds.2005-3055. [DOI] [PubMed] [Google Scholar]
- 67.National Resource Center for Health and Safety in Child Care and Early Education. [cited 2014 October 14]. nrckids.org.
- 68.Galinsky E., Howes C., Kontos S., Shinn M. The study of children in family child care and relative care: highlights of findings. New York: Families and Work Institute; 1994. [Google Scholar]
- 69.Altimari D. Hartford CT.: 2015. would require 'safe sleep' instruction for new parents, in Hartford Couran. [Google Scholar]


