Supplemental Digital Content is available in the text
Abstract
We aimed to examine whether early life bereavement, as indicator of severe stress, was associated with an increased risk of schizophrenia later in life.
Based on population registers, we established a cohort of all children born in Denmark (N = 1 686 416) and Sweden (N = 2 563 659) from 1973 to 1997. Children were categorized as exposed if they lost a first-degree relative during the first 18 years of life. Outcome is the first diagnosis of schizophrenia as either inpatient or outpatient. Log-linear Poisson regression models were used to estimate incidence rate ratios (IRRs).
A total of 188,850 children (4.6%) experienced death of a first-degree relative from birth to 18 years of age. Compared with unexposed children, those exposed had overall a 39% higher risk of schizophrenia (= 1.39, 95% CI [confidence interval]: 1.32–1.47). The IRR was particularly high if the family member committed suicide (aIRR = 2.11, 95% CI: 1.90–2.34) or died due to an injury or accident (aIRR = 1.44, 95% CI: 1.27–1.63). The IRR of schizophrenia decreased with increasing child's age at bereavement (P < 0.0001). Children who experienced >1 death during the first 18 years of life (aIRR = 1.79, 95% CI: 1.46–2.19) had a higher risk than those with a single death (aIRR = 1.37, 95% CI: 1.30–1.45).
The study suggested that exposure to death of a first-degree relative before 18 years was associated with an increased risk of schizophrenia in later life. The complex mechanisms behind these associations remain to be elucidated.
INTRODUCTION
Schizophrenia is a severe mental disorder characterized by fundamental and characteristic distortions of thinking, perception, and emotions. It has a lifetime risk of 1%1 and an annual incidence rate of 10 to 20/100,000 person-years.2,3 It has been increasingly recognized that genetic predisposition and early environmental exposures interact to shape brain development and function, which may possibly lead to psychiatric disorders including schizophrenia.4–6 A recent review7 based on 61 studies using Swedish national registry data summarizes that schizophrenia has a multifactorial etiological bases with factors surrounding pregnancy, parental age, low socioeconomic status, substance misuse, and poor cognitive performance besides population genetics to be associated with an increased risk of later schizophrenia.
Early childhood adversities, including abuse, neglect, and bullying have been associated with increased risks of a number of psychiatric disorders,8 such as adult depression,9 personality disorder,10,11 and substance use disorder.12 A recent meta-analysis indicates that childhood adversity is strongly associated with an increased risk for psychosis. However, the issues regarding the effect of age of exposure to psychosis outcome is not addressed, and the psychosis literature has tended to focus exclusively on hallucinatory and delusional symptoms and not on other symptoms.13
The death of a close family relative is considered one of the most severe life events14 and has been associated with different adverse aspects of health and social well-being.15 Childhood parental loss has been studied in relation to some psychiatric diseases,16–21 especially major depression.16–18 The studies on schizophrenia have yielded equivocal findings22–26 and a number of methodological limitations make it difficult to draw firm conclusions. Furthermore, it has not been clarified the extent to which the severity of the stressful life event would play a role (for example, the closeness of the relationship and multiple losses), or if age at exposure modifies the risk of schizophrenia.
Using nationwide Danish and Swedish data, we estimated the association between exposure to death of a first-degree relative from birth to 18 years of age and the risk of subsequent schizophrenia. In particular, we examined whether the risks differ by nature of the bereavement (child's relationship with the deceased, unexpectedness of the death) and child age at bereavement.23,27,28
MATERIALS AND METHODS
Ethics Statement
The study was approved by the Research Ethics Committee at the Karolinska Institute in Sweden, and the Research Ethics Committee of the Central Region and the Data Protection Agency in Denmark.
Study Population
We conducted the nationwide cohort study by combining several national registers from Sweden and Denmark.29 All legal residents in Nordic countries are assigned a unique personal identification number (CPR number), which allows record linkage of individual information between national registers.30
We used data from the Swedish Multi-generation Register29 and the Danish Civil Registry System31 to identify all children born between January 1, 1973, and December 31, 1997, (in Sweden, N = 2,563,659; in Denmark, N = 1,686,416). We followed the children from 10 years of age until emigration, death, the first diagnosis of schizophrenia, or end of follow-up (December 31, 2007), whichever came first. We excluded children who were unable to be linked to their parents (N = 7516, 0.18%), who emigrated (N = 106,807, 2.51%), who died (N = 36,055, 0.85%), and who were diagnosed with schizophrenia before 10 years of age (N = 364, 0.01%). At the beginning of follow-up, there were 188,850 and 3,910,483 children in the exposed and unexposed groups, respectively.
Exposure
We categorized children as exposed to bereavement when they experienced death of a first-degree relative (father, mother, or sibling) from birth to 18 years. The exposure was treated as a time-varying variable. The children who lost a first-degree relative from birth to 10 years of age were allocated to the exposed cohort at the beginning of the follow-up (at 10 years of age). Other children were allocated to the unexposed cohort at the beginning of the follow-up and were moved to the exposed cohort if they lost a first-degree relative from 10 to 18 years of age. Family relatives were identified using the Danish Civil Registry System31 and the Swedish Multi-generation Register.29
Information on causes of death and diagnoses was retrieved using 3 versions of the International Classification of Diseases (ICD-8, ICD-9, and ICD-10). In Denmark, ICD-8 was used from 1978 to 1993 and ICD-10 from 1994 to 2007; in Sweden ICD-8 was used from 1973 to 1986, ICD-9 from 1987 to 1996, and ICD-10 from 1997 to 2008.
Information on causes of death was obtained from the Cause of Death Register in Denmark and Sweden,29 and categorized into 4 groups: death from suicide (ICD-8 codes E950-E959, E980-E989; ICD-9 codes E950-E959, E980-E989; and ICD-10 codes X60-X84, Y10-Y34, Y870, Y872), death from accident/injury (ICD-8 codes E800-E949, E960-E979, E990-E999; ICD-9 codes E800-E949, E960-E979, E990-E999; and ICD-10 codes V01-X59, X85-Y09, Y35-Y98 except Y870, Y872), death from psychiatric disorders (ICD-8 codes 290–315; ICD-9 codes 290–315; and ICD-10 F00-F99), death from other diseases and medical conditions (ICD-8 codes 000–799 except 290–315, ICD-9 codes 000–799 except 290–315, and ICD-10 codes A00-R99 except F00-F99).
In the bereaved cohort, 4.0% of bereaved children experienced >1 loss of relatives from birth to 18 years of age. When multiple losses happened, the first bereavement was used to classify the exposure status of the children in the main analyses. When evaluating the effect of multiple losses, children were categorized into those who experienced >1 loss (n = 7558, 0.2%), a single loss (n = 181,292, 4.4%), and the unexposed (n = 3,910,483, 95.4%).
Outcome
Information on schizophrenia in children was retrieved from the Danish National Hospital Register,32 which includes diagnoses from all admittance to inpatient care since 1969 and includes outpatients since 1995, and the Danish Psychiatric Central Register,33 which includes diagnoses from all inpatient and outpatient psychiatric hospital-based units in Denmark. In Sweden, information on schizophrenia was retrieved from the Swedish Hospital Discharge Register,29 which includes diagnoses on all discharges from psychiatric hospitals since 1973. Schizophrenia cases were diagnosed following the visit to outpatient care or the first admittance to a psychiatric hospital due to schizophrenia (ICD-8 codes 295, 297, 298.2, 298.3, 298.9; ICD-9 codes 295, 297, 298C-298Y; ICD-10 codes F20-F29). If the diagnosis of schizophrenia preceded the bereavement, the children were categorized as unexposed.
Covariates
Information on country, sex, perinatal characteristics (calendar year of child birth, gestational age, parity, birth weight, and Apgar score at 5 minutes), maternal age, and maternal origin were obtained from the Swedish Medical Birth Register established in 197334 and Danish Medical Birth Register established in 1968,35 respectively. We used the Swedish Education Register and the Danish Integrated Database for Longitudinal Labour Market Research29 to retrieve the information on maternal education and social status. At last, we used the psychiatric registers as described above for cases33 to obtain the information on family history of psychiatric disorder (ICD-8: 290–315, ICD-9: 290–319, ICD-10: F00-F99).
Statistical Analysis
We estimated incidence rate ratios (IRRs) by applying log-linear Poisson regression model on aggregated person-year data. We adjusted for the following factors, which may be associated with both postnatal stress and schizophrenia: country (Denmark, Sweden), calendar year of childbirth (1983–1990,1991–1992, and 1-year categories from 1993 to 2007), child age at each calendar year (10–12, 1-year categories from 13 to 31, and 32–34 years), child sex (male, female), maternal characteristics (age at childbirth [<27, 27–30, ≥31 years], parity [1, 2, ≥3], social status [top level status, skilled workers/white collars, unskilled workers, not in labor market], education [≤9, 10–14, ≥15 years], and maternal origin [Nordic, non-Nordic]), paternal age at childbirth (<27, 27–30, ≥31 years), and family history of psychiatric disorder (Yes, No). Family history of psychiatric disorder, child age, and calendar year of childbirth were generated as time-dependent variables.
Analyses were repeated by type of deceased relatives of children (father, mother, and sibling), cause of death, and age at bereavement (0–3, 4–9, 10–12, and 13–18 years). Furthermore, the analyses were performed by sex of the deceased parent and sex of the child to evaluate effect of modification by sex of the deceased and child.
We carried out stratified analyses by specific baseline characteristics of study population, including sex, country, birth outcomes (birth weight [<2500, 2500–3249, 3250–3999, ≥4000 g], Apgar score at 5 minutes [0–6, 7–10], and gestational age [<37, ≥37 weeks]), maternal characteristics (maternal age, education at birth, and social status), paternal age, and family history of psychiatric disease to assess whether these factors modified the effects of early life bereavement on schizophrenia.
We also evaluated the effect of single and multiple losses of death of first-degree relatives on risk of schizophrenia, and observed whether there was a dose-response relation.
We used SAS 9.2 statistical software packages (SAS Institute, Inc, Cary, NC) for data management and statistical analyses. In all the analyses, we did not make use of the information of subjects with missing values due to a very low proportion of them in exposure and confounder variables in the study.
RESULTS
A total of 188,850 children (4.6%) experienced death of a first-degree relative from birth until 18 years of age, among whom 42,111 (1.03%) children lost a mother, 95,873 (2.34%) lost a father, and 50,866 (1.24%) lost a sibling. During follow-up (from 1 year to 25 years [median: 11 years]), 17,953 children were diagnosed with schizophrenia during 49.3 million person-years (36.4/100,000 person-years).
Characteristics of Study Population and Schizophrenia
Table 1 presented the baseline characteristics of exposed and unexposed children. Exposed children tended to be born to older parents, have a lower birth weight, and have a family history of psychiatric disorders. In addition, mothers of exposed children tended to have a shorter term education and higher parity, compared to unexposed children.
TABLE 1.
Baseline Characteristics of the Study Population
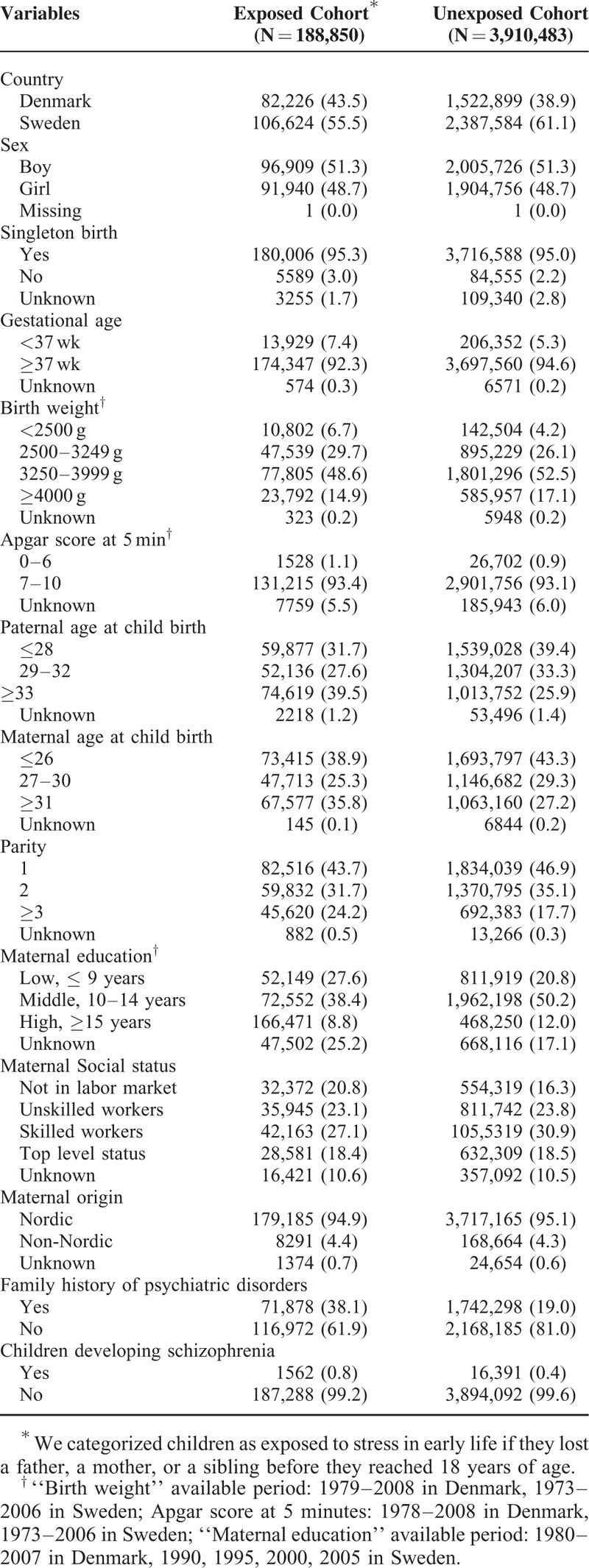
There were significant variations in incidence rate of schizophrenia according to baseline characteristics (Supplemental Table 1 Distribution of cases of schizophrenia in the study population). The risk of schizophrenia in Denmark was 2.5 times that in Sweden, and boys had a 31% higher risk compared to girls. Other risk factors for schizophrenia included low birth weight (<2500 g), low Apgar score (0–6 at 5 minutes), high paternal age at birth (≥33 years), not in labor market of maternal social status, non-Nordic country of maternal birth, and family history of psychiatric disorders.
Early Life Exposure to Death of a First-Degree Relative and Risk of Schizophrenia
Table 2 presents the association between early life bereavement before 18 years and risk of schizophrenia. Compared with the unexposed, children exposed to bereavement had a 39% higher risk of schizophrenia (aIRR = 1.39, 95% CI [confidence interval]: 1.32–1.47) after adjusting for the potential confounders. When the analyses were performed by the type of deceased relative, the association between mother's death (aIRR = 1.48, 95% CI: 1.34–1.64) and schizophrenia was slightly but not significantly larger than deaths of other relatives (aIRR = 1.36, 95% CI: 1.27–1.46 for father's death, aIRR = 1.37, 95% CI: 1.24–1.52 for death of sibling).
TABLE 2.
IRRs of Schizophrenia in Children Who Lost a First-Degree Relative During Early Life
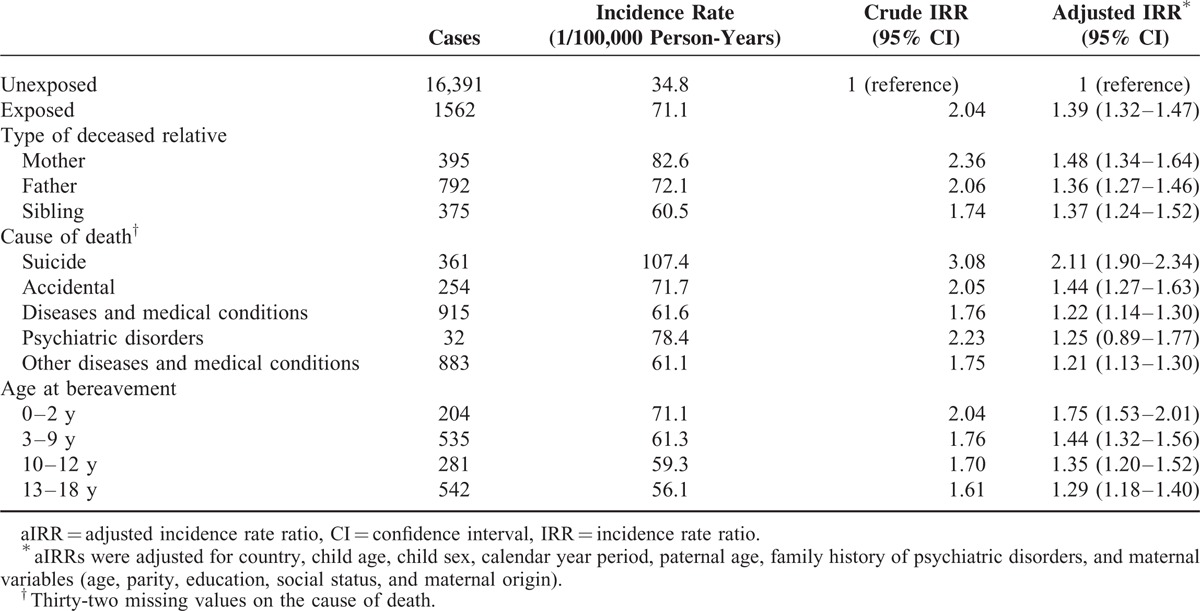
The risk of schizophrenia differed by the causes of death (Table 2). Compared with the unexposed, suicide death was associated with the highest risk of schizophrenia (aIRR = 2.11, 95% CI: 1.90–2.34). The risk for death from accidental causes (aIRR = 1.44, 95% CI: 1.27–1.63) was higher than for death from disease and medical conditions (aIRR = 1.22, 95% CI: 1.14–1.30). We separated the death due to psychiatric disorders from those due to diseases and medical conditions and found that the risk for death from psychiatric disorders (aIRR = 1.25, 95% CI: 0.89–1.77) was similar as those from other diseases and medical conditions (aIRR = 1.21, 95% CI: 1.13–1.30). The risk for death from psychiatric disorders was not statistically significant, which may be due to a small sample size.
Compared with the unexposed, children exposed to bereavement at 0 to 2, 3 to 9, 10 to 12, and 13 to 18 years had a 75%, 44%, 35%, and 29% higher risk of schizophrenia, respectively (Table 2). There was a decreasing trend of the risk with increasing children age at bereavement (trend χ2 = 148.71, P < 0.0001).
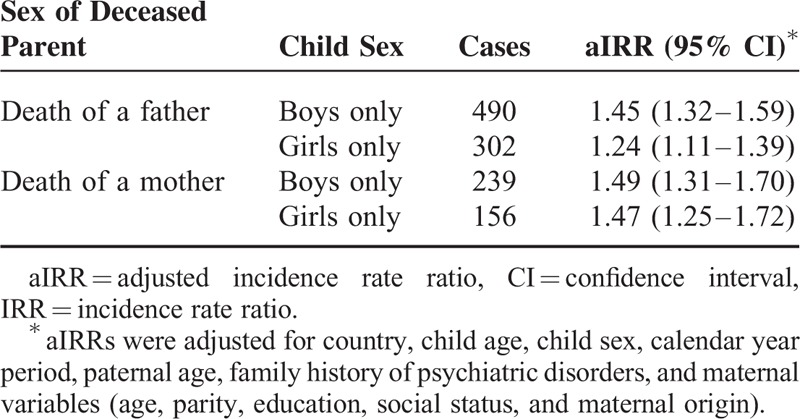
Further analyses performed by the deceased parent's sex and child's sex showed that boys who experienced a death of a father had a slightly but not significantly higher risk than girls. However, boys had a similar risk of schizophrenia as girls if both of them experienced a death of a mother (Table 3).
TABLE 3.
IRRs of Schizophrenia in Children Who lost a First-Degree Relative During Early Life, According to Sex of Parent and Sex of Child
The association between bereavement during the first 18 years of life and schizophrenia remained relatively stable across most of the subcategories of children's baseline characteristics. However, among children with birth weight <2500 g, low Apgar score at 5 minutes, children with maternal education at birth ≥15 years, or maternal social status being unskilled worker, the associations were not statistically significant (Figure 1).
FIGURE 1.
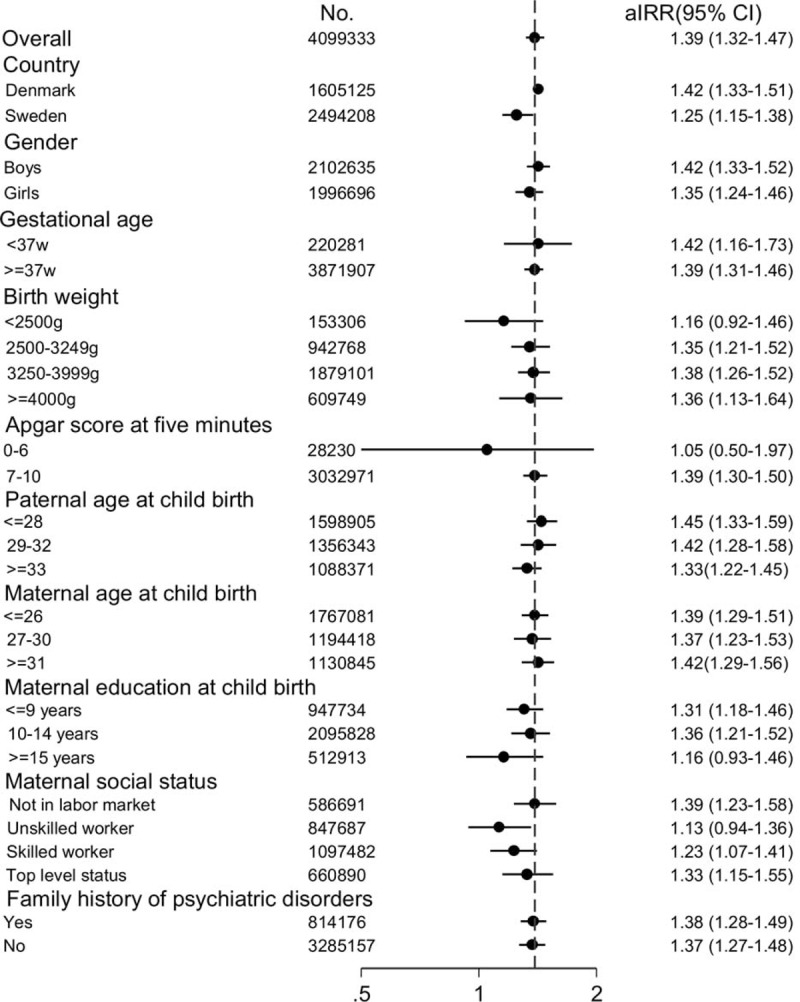
The association between exposure to loss of a first-degree relative in early life and schizophrenia: stratification analyses by the baseline characteristics. ∗aIRRs were adjusted for country, child age, child sex, calendar year period, paternal age, family history of psychiatric disorders, and maternal variables (age, parity, education, social status, and maternal origin). aIRR = adjusted incidence rate ratio, CI = confidence interval.
Exposure to Multiple Deaths of a First-Degree Relative and Risk of Schizophrenia
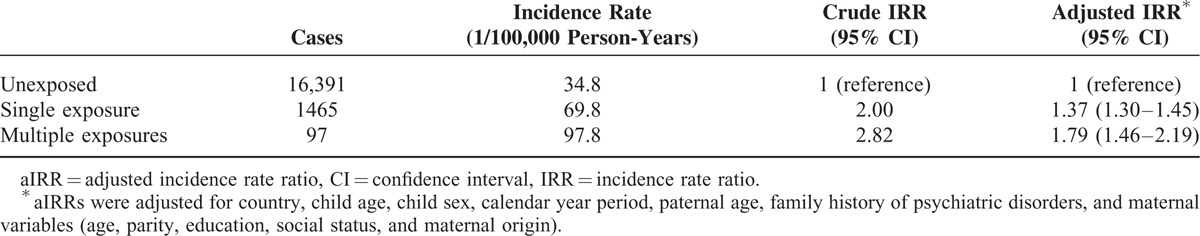
Table 4 presented the risk of schizophrenia among single and multiple exposed children. Compared with the unexposed, single exposed children had a 37% higher risk of schizophrenia (aIRR = 1.37; 95% CI: 1.30–1.45), and multiple exposed had a 79% higher risk (aIRR = 1.79; 95% CI: 1.46–2.19).
TABLE 4.
IRRs of Schizophrenia in Children Who Experienced a Loss or Multiple Loss of a First-Degree Relative
DISCUSSION
In this large population-based cohort study, exposure to death of a first-degree relative from birth to 18 years of age was associated with an increased risk of schizophrenia in later life. The risk was most pronounced for suicidal death, followed by injury/accidental death. Risk of schizophrenia decreased with increasing child's age at bereavement. Similar results were observed when analyses were performed by type of deceased first-degree relative (mother, father, siblings). The risk of schizophrenia increased with the number of deceased relatives.
Our results are in line with 2 cohort studies on childhood bereavement and psychotic disorders.23,27 Our study had similar design and results as one of them in which Abel et al23 used only Swedish data (children born between 1973 and 1985) to examine the effect of bereavement during childhood period on the risk of psychosis. They defined exposure time as from birth to 13 years, which was different with ours from birth to 18 years. Moreover, Abel et al23 performed logistic regression to estimate odd ratios and person–year information was not considered, while our study used log-linear Poisson regression of aggregated person-year data to estimate IRR and defined exposure as time-dependent variable. In addition, our study could obtain more precise estimation due to increased sample size (children born between 1973 and 1997 in both Denmark and Sweden). Another Swedish study, where exposure was defined as the bereavement of first- and second-degree relatives during the first 2 years of childhood, showed a nonsignificant association.22 The different results may be due to the diversity of exposure definition in these 2 studies. Early case-control studies on parental loss and schizophrenia produced mixed results.24,26,36,37 The methodological diversity and limitation may explain the varied findings and make it difficult to draw firm conclusion.
If stress plays a role in the etiology of schizophrenia, it is expected that more severe stress exposure is associated with a higher risk. However, most studies on bereavement and schizophrenia have not examined effects of types of the deceased relatives and causes of death as indicator of stress severity, and no study has investigated whether multiple exposures to bereavement are associated with a higher risk than a single exposure. We found that death of first-degree relatives by different family members (father, mother, or sibling) had similar effects on subsequent schizophrenia. There was a trend of increased risk of schizophrenia as the increasing exposure frequencies, which also indicated a dose-response effect.
It is possible that observed associations between early life bereavement and schizophrenia may be partly confounded by genetic disposition. In the study, suicide of a family member was associated with the highest risk of schizophrenia, followed by death from accident or injury. Suicide and accidental decedents received more inpatient psychiatric care27 and psychiatric disorders are also related to accidental death,38 which made it to be possible that the parents who died due to suicide or accident were more likely to have mental problem. Therefore, the observed effect on suicide or accident may reflect a heritability of mental health in part. However, the risk of schizophrenia was elevated among children exposed to death due to diseases and medical conditions, as well as among those without family history of psychiatric disorders. Thus, confounding by genetic disposition is unlikely to be the sole explanation for the observed associations.
Accumulating evidence suggests that early life adversities negatively affect future health and social well-being, by both biological and psychosocial mechanisms.39,40 Early life stress could interact with the genetic susceptibility to impact the development of psychopathology in adulthood. Early life adversities may lead to sustained dysfunction of hypothalamic-pituitary-adrenal (HPA) axis in human,41–43 possibly mediated by epigenetic modification, such as increased methylation of glucocorticoid receptor gene44,45 or FK506 binding protein 5 gene.46 Elevated glucocorticoids impair neuronal growth and survival,47 diminish neurotrophins, and modify immune function,48 all of which had been associated with psychiatric disorders.47 Severe psychosocial stressors embedded in early life may be more likely to increase the susceptibility to future psychiatric diseases by the long-lasting dysfunction of hypothalamic-pituitary-adrenal axis.41–43 In addition, social and environmental factors following the death of a close family member, such as single-parental household, unemployment of the living parent, low socioeconomic status, extensive changes of caretaking, and health risk behaviors of children could contribute to the development of future schizophrenia.
The association between bereavement and subsequent schizophrenia risk tended to decrease with child's age, and loss of a close relative during the first 3 years of life was associated with the highest risk. This may reflect the greater vulnerability of brain development during one's very early years of life when bereavement may lead to adverse or stressful family environment, although the child may not be able to perceive directly this life event. We also found that bereavement exposure during adolescence was associated with an increased risk of schizophrenia later in life, although the risk was lower than that during childhood. Recent evidence provides a molecular basis of the interaction between genetic susceptibility of mental health problem and stress exposure during adolescence, such as deoxyribonucleic acid methylation modification.45
Our study has several methodological strengths. First, we examined the association between early life bereavement and the risk of schizophrenia in offspring in the largest population cohort to date. The large sample size in our study made it possible to analyze the effects of different types, causes, and timing of bereavement as well as child sex and other variables. Second, ascertainment of exposure information and psychiatric outcomes from registers are considered to be highly accurate and complete since reporting is mandated by the laws.49 For example, validation studies on register diagnosis of schizophrenia confirmed a low number of false-positive diagnoses. There was 94% to 98% agreement between register diagnoses of schizophrenia and research diagnoses.50,51 Third, in contrast to many previous studies on this topic, we included potentially important confounders, including several sociodemographic and perinatal factors, and family history of psychiatric illnesses.
However, several limitations need to be considered. First, diagnostic criteria might be different between Denmark and Sweden since the 2 countries used different version of ICD during the study period. Outpatients were included in the identification of schizophrenia in registers of Denmark since 1995, but not in Sweden. However, it is unlikely to bias the association between bereavement during early life and schizophrenia since the difference in diagnostic criteria and cases definition in 2 countries was not associated with bereavement exposure. Second, we could not obtain longitudinal data on personal socioeconomic status. We adjusted for maternal education and social status at child birth, which are related to personal socioeconomic status. Third, we were not able to include information on lifestyle factors that are important in the etiology of schizophrenia. For example, individuals who experienced adverse childhood experiences are more likely to have health risk behaviors, such as tobacco smoking, alcoholism, and drug use.52,53 Systematic reviews suggest that daily tobacco smoking54 and cannabis use55 are potentially associated with the development of psychotic illness. In addition, cannabis use and childhood trauma could interact to increase the risk of psychosis.56,57 Thus, the post-loss lifestyle factors may have a causal role on the occurrence of schizophrenia by itself or through its interaction with childhood trauma. However, as such changes may be in the causal pathways from exposure to outcome, it may not be necessary to control such factors.58 Fourth, it should be acknowledged that schizophrenia cases not recorded in the registers should be misclassified as noncases. However, this misclassification is most likely to be nondifferential between children exposed and unexposed to bereavement, and may, if anything, bias the risk estimates toward unity.
In conclusion, exposure to death of a first-degree relative before 18 years of age was associated with an increased risk of schizophrenia in later life, regardless of relationship to the deceased, age and sex of the child. The risk was particularly associated with death due to suicide or accidental death, death during early childhood, and exposure to multiple deaths. The complex mechanisms behind these associations remain to be elucidated. These findings suggest that bereaved children could be considered as a “high-risk” group of developing schizophrenia, particularly those of parents with mental health problems, and public health program is needed to provide health and social support for the bereaved children. In clinical practice, the history of bereavement of a patient with schizophrenia should be taken into account in the treatment.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, ICD = International Classification of Diseases, IRR = incidence rate ratio.
Author Contributions: Conceived and designed the study: JL. Performed the study: HL JO WY SV MV CO MG JL. Analyzed the data: HL. Contributed reagents/materials/analysis tools: HL JO WY SV MV CO MG JL. Wrote the first draft of the manuscript: HL. Contributed to the writing of the manuscript: JO WY SV MV CO MG JL. ICMJE criteria for authorship read and met: HL JO WY SV MV CO MG JL. Agree with manuscript results and conclusions: HL JO WY SV MV CO MG JL. Obtained research funding for this study: JL.
The work was supported by the European Research Council (ERC-2010-StG-260242-PROGEURO), the Swedish Council for Working Life and Social Research (Grant no. 2010–0092), the Danish Medical Research Council (09–072986), National Natural Science Foundation of China (81428011), and the Lundbeck Foundation (MEPRICA).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.McGrath J, Saha S, Chant D, et al. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 2008; 30:67–76. [DOI] [PubMed] [Google Scholar]
- 2.Kirkbride JB, Errazuriz A, Croudace TJ, et al. Incidence of schizophrenia and other psychoses in England, 1950-2009: a systematic review and meta-analyses. PLoS One 2012; 7:e31660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sutterland AL, Dieleman J, Storosum JG, et al. Annual incidence rate of schizophrenia and schizophrenia spectrum disorders in a longitudinal population-based cohort study. Soc Psychiatry Psychiatr Epidemiol 2013; 48:1357–1365. [DOI] [PubMed] [Google Scholar]
- 4.Walker E, Kestler L, Bollini A, et al. Schizophrenia: etiology and course. Annu Rev Psychol 2004; 55:401–430. [DOI] [PubMed] [Google Scholar]
- 5.Van Os J, Rutten BP, Poulton R. Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull 2008; 34:1066–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis DA, Levitt P. Schizophrenia as a disorder of neurodevelopment. Annu Rev Neurosci 2002; 25:409–432. [DOI] [PubMed] [Google Scholar]
- 7.Harper S, Towers-Evans H, MacCabe J. The aetiology of schizophrenia: what have the Swedish Medical Registers taught us? Soc Psychiatry Psychiatr Epidemiol 2015; 50:1471–1479. [DOI] [PubMed] [Google Scholar]
- 8.Carr CP, Martins CM, Stingel AM, et al. The role of early life stress in adult psychiatric disorders: a systematic review according to childhood trauma subtypes. J Nerv Ment Dis 2013; 201:1007–1020. [DOI] [PubMed] [Google Scholar]
- 9.Gibb BE, Chelminski I, Zimmerman M. Childhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatients. Depress Anxiety 2007; 24:256–263. [DOI] [PubMed] [Google Scholar]
- 10.Sar V, Akyuz G, Kugu N, et al. Axis I dissociative disorder comorbidity in borderline personality disorder and reports of childhood trauma. J Clin Psychiatry 2006; 67:1583–1590. [DOI] [PubMed] [Google Scholar]
- 11.Heins M, Simons C, Lataster T, et al. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry 2011; 168:1286–1294. [DOI] [PubMed] [Google Scholar]
- 12.McLaughlin KA, Green JG, Gruber MJ, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatry 2010; 67:124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull 2012; 38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skodol AE, Shrout PE. Use of DSM-III Axis IV in clinical practice: rating etiologically significant stressors. Am J Psychiatry 1989; 146:61–66. [DOI] [PubMed] [Google Scholar]
- 15.Stroebe MS, Hansson RO, Schut H, et al. Handbook of Bereavement Research and Practice: Advances in Theory and Intervention. Washington, DC: American Psychological Association; 2008. [Google Scholar]
- 16.Kendler KS, Neale MC, Kessler RC, et al. Childhood parental loss and adult psychopathology in women: a twin study perspective. Arch Gen Psychiatry 1992; 49:109–116. [DOI] [PubMed] [Google Scholar]
- 17.Kendler KS, Sheth K, Gardner CO, et al. Childhood parental loss and risk for first-onset of major depression and alcohol dependence: the time-decay of risk and sex differences. Psychol Med 2002; 32:1187–1194. [DOI] [PubMed] [Google Scholar]
- 18.Tyrka AR, Wier L, Price LH, et al. Childhood parental loss and adult psychopathology: effects of loss characteristics and contextual factors. Int J Psychiatry Med 2008; 38:329–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breier A, Kelsoe JR, Kirwin PD, et al. Early parental loss and development of adult psychopathology. Arch Gen Psychiatry 1988; 45:987–993. [DOI] [PubMed] [Google Scholar]
- 20.Tsuchiya KJ, Agerbo E, Mortensen PB. Parental death and bipolar disorder: a robust association was found in early maternal suicide. J Affect Disord 2005; 86:151–159. [DOI] [PubMed] [Google Scholar]
- 21.Stikkelbroek Y, Prinzie P, de Graaf R, et al. Parental death during childhood and psychopathology in adulthood. Psychiatry Res 2012; 198:516–520. [DOI] [PubMed] [Google Scholar]
- 22.Class Q, Abel K, Khashan A, et al. Offspring psychopathology following preconception, prenatal and postnatal maternal bereavement stress. Psychol Med 2014; 44:71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abel KM, Heuvelman HP, Jorgensen L, et al. Severe bereavement stress during the prenatal and childhood periods and risk of psychosis in later life: population based cohort study. BMJ 2014; 348:f7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agid O, Shapira B, Zislin J, et al. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Mol Psychiatry 1999; 4:163–172. [DOI] [PubMed] [Google Scholar]
- 25.Clarke MC, Tanskanen A, Huttunen MO, et al. Sudden death of father or sibling in early childhood increases risk for psychotic disorder. Schizophr Res 2013; 143:363–366. [DOI] [PubMed] [Google Scholar]
- 26.Furukawa T, Mizukawa R, Hirai T, et al. Childhood parental loss and schizophrenia: evidence against pathogenic but for some pathoplastic effects. Psychiatry Res 1998; 81:353–362. [DOI] [PubMed] [Google Scholar]
- 27.Wilcox HC, Kuramoto SJ, Lichtenstein P, et al. Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death. J Am Acad Child Adolesc Psychiatry 2010; 49:514–523. [DOI] [PubMed] [Google Scholar]
- 28.Li J, Vestergaard M, Cnattingius S, et al. Mortality after parental death in childhood: a nationwide cohort study from three Nordic countries. PLoS medicine 2014; 11:e1001679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Vestergaard M, Obel C, et al. Cohort profile: the Nordic Perinatal Bereavement Cohort. Int J Epidemiol 2011; 40:1161–1167. [DOI] [PubMed] [Google Scholar]
- 30.Frank L. Epidemiology. When an entire country is a cohort. Science 2000; 287:2398–2399. [DOI] [PubMed] [Google Scholar]
- 31.Pedersen CB, Gotzsche H, Moller JO, et al. The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull 2006; 53:441–449. [PubMed] [Google Scholar]
- 32.Andersen TF, Madsen M, Jorgensen J, et al. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999; 46:263–268. [PubMed] [Google Scholar]
- 33.Munk-Jorgensen P, Mortensen PB. The Danish Psychiatric Central Register. Dan Med Bull 1997; 44:82–84. [PubMed] [Google Scholar]
- 34.Axelsson O. The Swedish medical birth register. Acta Obstet Gynecol Scand 2003; 82:491–492. [DOI] [PubMed] [Google Scholar]
- 35.Knudsen LB, Olsen J. The Danish Medical Birth Registry. Dan Med Bull 1998; 45:320–323. [PubMed] [Google Scholar]
- 36.Ragan PV, McGlashan TH. Childhood parental death and adult psychopathology. Am J Psychiatry 1986. [DOI] [PubMed] [Google Scholar]
- 37.Watt NF, Nicholi A., Jr Early death of a parent as an etiological factor in schizophrenia. Am J Orthopsychiatry 1979; 49:465. [DOI] [PubMed] [Google Scholar]
- 38.Crump C, Sundquist K, Winkleby MA, et al. Mental disorders and risk of accidental death. Br J Psychiatry 2013; 203:297–302. [DOI] [PubMed] [Google Scholar]
- 39.Bateson P, Barker D, Clutton-Brock T, et al. Developmental plasticity and human health. Nature 2004; 430:419–421. [DOI] [PubMed] [Google Scholar]
- 40.Gluckman PD, Hanson MA, Cooper C, et al. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 2008; 359:61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tyrka AR, Wier L, Price LH, et al. Childhood parental loss and adult hypothalamic-pituitary-adrenal function. Biol Psychiatry 2008; 63:1147–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pfeffer CR, Altemus M, Heo M, et al. Salivary Cortisol and Psychopathology in Children Bereaved by the September 11, 2001 Terror Attacks. Biol Psychiatry 2007; 61:957–965. [DOI] [PubMed] [Google Scholar]
- 43.Nicolson NA. Childhood parental loss and cortisol levels in adult men. Psychoneuroendocrinology 2004; 29:1012–1018. [DOI] [PubMed] [Google Scholar]
- 44.Perroud N, Dayer A, Piguet C, et al. Childhood maltreatment and methylation of the glucocorticoid receptor gene NR3C1 in bipolar disorder. Br J Psychiatry 2014; 204:30–35. [DOI] [PubMed] [Google Scholar]
- 45.van der Knaap LJ, Riese H, Hudziak JJ, et al. Glucocorticoid receptor gene (NR3C1) methylation following stressful events between birth and adolescence. The TRAILS study. Transl Psychiatry 2014; 4:e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klengel T, Mehta D, Anacker C, et al. Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions. Nat Neurosci 2013; 16:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Duman RS. Neuronal damage and protection in the pathophysiology and treatment of psychiatric illness: stress and depression. Dialogues Clin Neurosci 2009; 11:239–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Epel ES. Psychological and metabolic stress: a recipe for accelerated cellular aging? Hormones (Athens, Greece) 2009; 8:7–22. [DOI] [PubMed] [Google Scholar]
- 49.Danish Act on the Civil Registration System. Act no. 426 of 31 May 2000. Denmark: The Danish Civil Registration Office. Available: http://www.cpr.dk/index.asp?d=140&o=7&n=0&h=7&s=5 2000. [Google Scholar]
- 50.Uggerby P, Ostergaard SD, Roge R, et al. The validity of the schizophrenia diagnosis in the Danish Psychiatric Central Research Register is good. Dan Med J 2013; 60:A4578. [PubMed] [Google Scholar]
- 51.Ekholm B, Ekholm A, Adolfsson R, et al. Evaluation of diagnostic procedures in Swedish patients with schizophrenia and related psychoses. Nord J Psychiatry 2005; 59:457–464. [DOI] [PubMed] [Google Scholar]
- 52.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998; 14:245–258. [DOI] [PubMed] [Google Scholar]
- 53.Dube SR, Felitti VJ, Dong M, et al. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med 2003; 37:268–277. [DOI] [PubMed] [Google Scholar]
- 54.Gurillo P, Jauhar S, Murray RM, et al. Does tobacco use cause psychosis? Systematic review and meta-analysis. Lancet Psychiatry 2015; 2:718–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Large M, Sharma S, Compton MT, et al. Cannabis use and earlier onset of psychosis: a systematic meta-analysis. Arch Gen Psychiatry 2011; 68:555–561. [DOI] [PubMed] [Google Scholar]
- 56.Houston JE, Murphy J, Shevlin M, et al. Cannabis use and psychosis: re-visiting the role of childhood trauma. Psychol Med 2011; 41:2339–2348. [DOI] [PubMed] [Google Scholar]
- 57.Harley M, Kelleher I, Clarke M, et al. Cannabis use and childhood trauma interact additively to increase the risk of psychotic symptoms in adolescence. Psychol Med 2010; 40:1627–1634. [DOI] [PubMed] [Google Scholar]
- 58.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


