Abstract
Outcome after surgery in patients with asthma remains unknown. The purpose of this study is to investigate postoperative major complications and mortality in surgical patients with asthma.
Using reimbursement claims from the Taiwan National Health Insurance Research Database, the authors identified 24,109 surgical patients with preoperative asthma and 24,109 nonasthma patients undergoing major surgeries using matching procedure with propensity score by sociodemographics, coexisting medical conditions, and surgical characteristics. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for 30-day postoperative complications and mortality associated with asthma were analyzed in the multivariate logistic regressions.
Asthma increased postoperative pneumonia (OR 1.48; 95% CI 1.34–1.64), septicemia (OR 1.11; 95% CI 1.02–1.21), and urinary tract infection (OR 1.17; 95% CI 1.09–1.26). Preoperative emergency care for asthma was significantly associated with postoperative 30-day in-hospital mortality, with an OR of 1.84 (95% CI 1.11–3.04). Preoperative emergency service, hospitalizations, admission to intensive care unit, and systemic use of corticosteroids for asthma were also associated with higher postoperative complication rates for asthmatic patients.
Postoperative complications and mortality were significantly increased in asthmatic patients. We suggest urgent efforts to revise protocols for asthma patients’ perioperative care.
INTRODUCTION
Asthma is a common clinical condition characterized by variable airway obstruction and hyper-responsiveness sustained by chronic inflammation.1,2 It is a worldwide problem, with an estimated 300 million affected individuals, and it is believed to contribute to one of every 250 deaths.3,4 The annual economic cost of asthma was $56 billion in the United States between 2002 and 2007.5 Days lost from work have also been reported as a substantial economic and social consequence of asthma in the United States, the United Kingdom, and Asian regions.6–8
Patients with asthma are noted to face higher risk of pulmonary complications during the perioperative period and increased risks of various complications after surgeries.9–11 Asthma increased risk of respiratory complications after adeno-tonsillectomy in children with obstructive breathing during sleep.9 Although the incidence of perioperative bronchospasm and laryngospasm was low, complications increased in elderly patients and in those with active asthma.10 These studies, however, were limited to asthma patients without adequate control, or focused on a single type of surgery or single outcome after surgery.9–11
The association between preoperative asthma and postoperative adverse events was not completely understood. We conducted this nationwide retrospective matched-cohort study using Taiwan's National Health Insurance Research Database to investigate comprehensive postoperative major complications and mortality for patients with asthma when receiving major surgeries. The impacts of various severity-related clinical characteristics of asthma on patients’ postoperative adverse events were also evaluated.
METHODS
Data Sources
Retrospective data were collected from reimbursement claims of Taiwan's National Health Insurance Program, which was implemented in March 1995 and covers more than 99% of the 22.6 million Taiwan residents. The National Health Research Institutes of Taiwan established a National Health Insurance Research Database that records all beneficiaries’ medical services, including inpatient and outpatient demographics, primary and secondary diagnoses, procedures, prescriptions and medical expenditures for public research interest. The validity of this database has been favorably evaluated, and research articles based on it have been accepted in prominent scientific journals worldwide.12–14
Ethical Approval
Insurance reimbursement claims from the National Health Insurance Research Database are available for public access. To protect personal privacy, the electronic database with patient identifications was decoded and scrambled for further research access. Although informed consent was not required because of this privacy protection, this study was approved both by the Taiwan's National Health Research Institutes (NHIRD-103-121) and Taipei Medical University's Institutional Review Board (TMU-JIRB-201505055; TMU-JIRB-201404070).12–14
Study Population
We examined medical claims and identified 24,109 patients ≥20 years of age with preoperative asthma from 1,834,149 surgical patients who underwent major inpatient surgeries between 2008 and 2010 in Taiwan. These surgeries required general, epidural, or spinal anesthesia and hospitalization for more than 1 day. To identify patients with asthma more strictly and to avoid those with minor or borderline asthma, the current study required at least 2 visits for medical care with primary diagnosis of asthma from physicians specialized in pulmonary medicine within the 24-month preoperative period of index surgery. Using matching procedure by propensity score with age, sex, low income, types of surgery, risk of surgery, types of anesthesia, operation in teaching hospital, and coexisting medical conditions, we selected 24,109 surgical patients from surgical patient populations who were free from diagnosis of asthma, preoperatively.
Measures and Definitions
We identified income status by defining low-income patients as those qualifying for waived medical copayment, because this status is verified by the Taiwan Bureau of National Health Insurance. Also recorded were whether the surgery was performed in a teaching hospital and the types of surgery and anesthesia. We used the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) to define preoperative medical diseases and postoperative complications. Preoperative asthma (ICD-9-CM 493) was defined as the major exposure. Coexisting medical conditions were determined from medical claims for the 24-month preoperative period, including hypertension (ICD-9-CM 401–405), mental disorders (ICD-9-CM 290–319), diabetes (ICD-9-CM 250), hyperlipidemia (ICD-9-CM 272.0, 272.1, 272.2), congestive heart failure (ICD-9-CM 428), liver cirrhosis (ICD-9-CM 571.2 and 571.5), and renal dialysis (administration code D8, D9). Thirty-day in-hospital mortality after the index surgery and postoperative complications were considered as the study's outcomes. These complications included pneumonia (ICD-9-CM 480–486), septicemia (ICD-9-CM 038 and 998.5), and urinary tract infection (ICD-9-CM 599.0).
This study also considered patients receiving asthma-related systemic corticosteroids, such as methylprednisolone, prednisolone, dexamethasone or hydrocortisone orally or intravenously. We also identified patients receiving emergency care, hospitalization or intensive care unit (ICU) admissions for asthma within the 24 months, preoperatively.
Statistical Analysis
We used propensity score-matched pair method to analyze asthma patients and nonasthma controls. We developed a nonparsimonious multivariable logistic regression model to estimate a propensity score for preoperative asthma, irrespective of outcome. Clinical significance guided the initial choice of covariates in this model: age, sex, low income, hypertension, mental disorders, diabetes, hyperlipidemia, congestive heart failure, liver cirrhosis, renal dialysis, operation in teaching hospital, types of surgery, risk of surgery, and types of anesthesia. The χ2 tests were used to measure covariate balance and a P-value <0.05 was suggested to represent meaningful covariate imbalance. We matched patients with asthma to nonasthma patients using a greedy-matching algorithm with a calliper width of 0.2 standard deviations of the log odds of the estimated propensity score. This method could remove 98% of the bias from measured covariates.12,15
Adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for 30-day postoperative pneumonia, septicemia, urinary tract infection and mortality between patients with and without asthma were analyzed with multivariate logistic regression by controlling sex, age, types of surgery and anesthesia, risk of surgery, operation in teaching hospital and preoperative coexisting medical conditions. The adjusted ORs and 95% CIs of 30-day postoperative pneumonia, septicemia, urinary tract infection, and mortality associated with preoperative asthma-related emergency care, hospitalizations, ICU admissions and use of systemic corticosteroids were calculated in the multivariate logistic regressions. SAS version 9.1 (SAS Institute Inc, Cary, NC) statistical software was used for data analyses; 2-sided P value <0.05 indicated significant differences between groups.
RESULTS
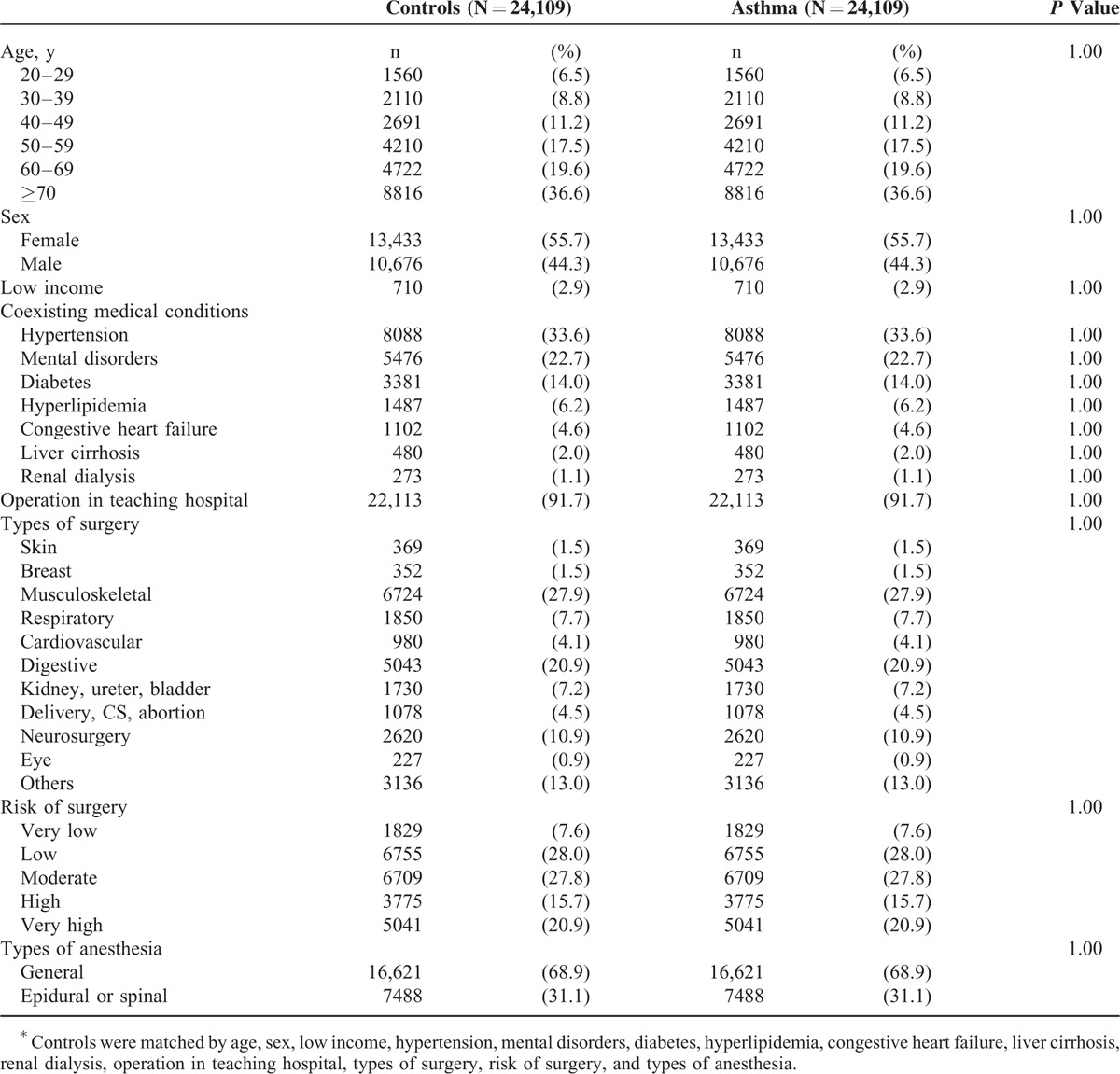
After being matched by propensity score procedure, there were no significant differences between surgical patients with and without asthma relating to age, sex, low income, types of surgery, risk of surgery, types of anesthesia, operation in teaching hospital, hypertension, mental disorders, diabetes, hyperlipidemia, congestive heart failure, liver cirrhosis, and renal dialysis (Table 1).
TABLE 1.
Baseline Characteristics of Surgical Patients With Asthma and Controls∗
Compared with surgical patients without asthma (Table 2), asthmatic patients had higher risks of postoperative pneumonia (OR = 1.48; 95% CI 1.34–1.64), septicemia (OR = 1.11; 95% CI 1.02–1.21), and urinary tract infection (OR = 1.17; 95% CI 1.09–1.26). Use of emergency medical services because of asthma within the 3 preoperative months was associated with higher rates for pneumonia (OR = 2.03; 95% CI 1.57–2.63), septicemia (OR = 1.44; 95% CI 1.13–1.85), and postoperative mortality (OR = 1.84; 95% CI 1.11–3.04). Increased risks of postoperative pneumonia (OR = 2.68; 95% CI 1.86–3.85) and urinary tract infection (OR = 1.75; 95% CI 1.27–2.41) were also noted in asthmatic patients who were hospitalized for asthma in the 3 months before the index surgery. The adjusted ORs for postoperative pneumonia, septicemia, and urinary tract infection associated with preoperative inpatient care ≥11 cumulative days for asthma in the 24 months before the surgery were 1.69 (95% CI 1.29–2.21), 1.69 (95% CI 1.35–2.12), and 1.71 (95% CI 1.39–2.11), respectively. Among patients with asthma, those with preoperative admission to ICU because of asthma had significantly higher risk of postoperative pneumonia (OR = 1.64; 95% CI 1.37–1.97), septicemia (OR = 1.75; 95% CI 1.50–2.05), urinary tract infection (OR = 1.85; 95% CI 1.60–2.15), and mortality (OR = 1.88; 95% CI 1.35–2.62).
TABLE 2.
Risk of Complications Associated With Asthma in the Multiple Logistic Regression Models
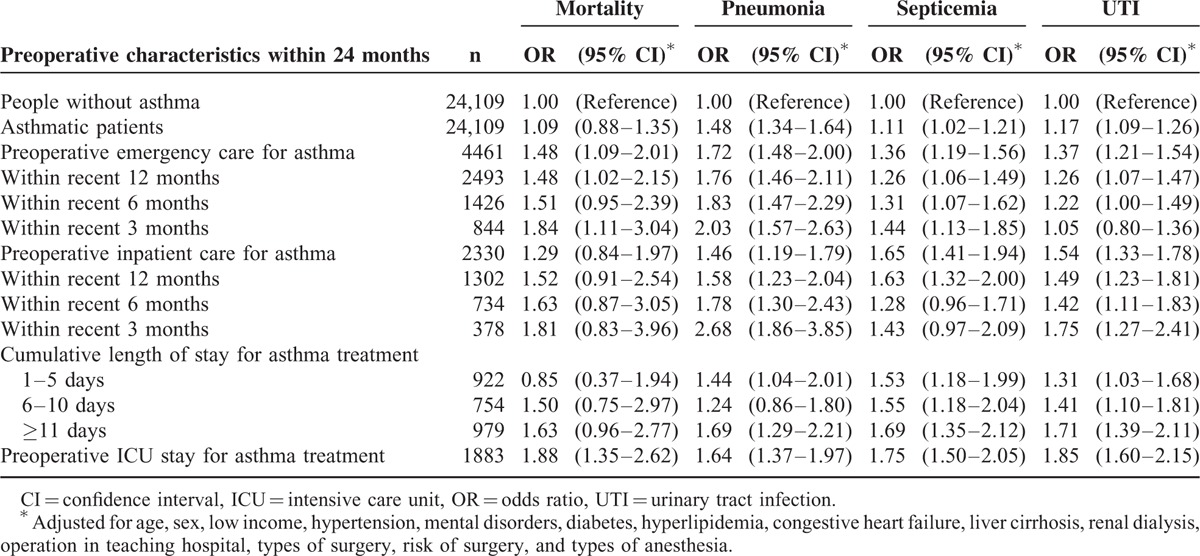
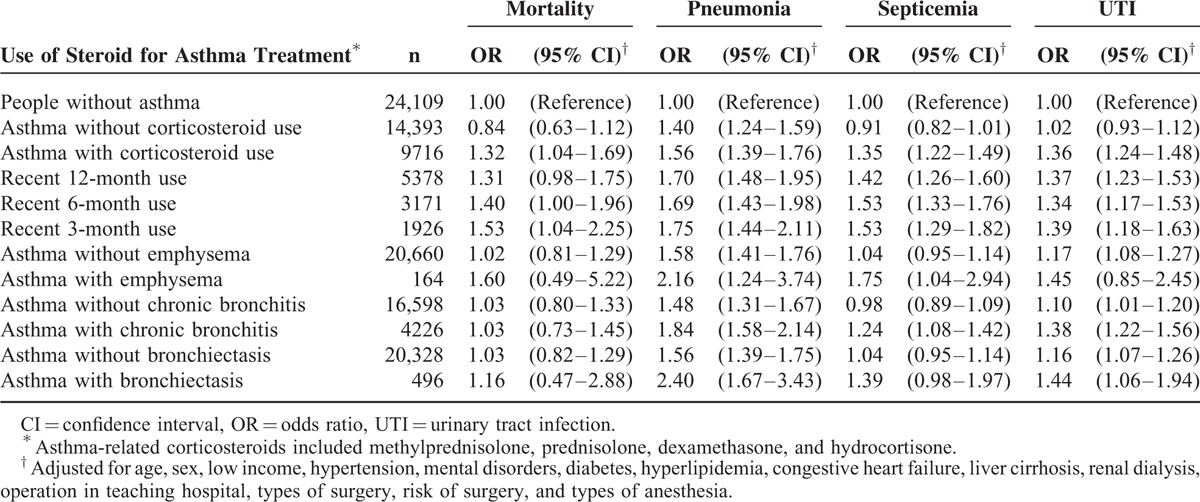
Table 3 shows that the medication of systemic corticosteroids for surgical patients with primary diagnosis of asthma within 3 months preoperatively was an independent risk factor for postoperative pneumonia (OR = 1.75; 95% CI 1.44–2.11), septicemia (OR = 1.53; 95% CI 1.29–1.82), urinary tract infection (OR = 1.39; 95% CI 1.18–1.63), and mortality (OR = 1.53; 95% CI 1.04–2.25). Asthmatic patients’ emphysema (OR = 2.16; 95% CI 1.24–3.74), chronic bronchitis (OR = 1.84; 95% CI 1.58–2.14), and bronchiectasis (OR = 2.40; 95% CI 1.67–3.43) have impacts on postoperative pneumonia.
TABLE 3.
Association between Preoperative Systemic Steroid Use and Postoperative Adverse Events in Patients With Asthma
DISCUSSION
This is the first nationwide population-based cohort study using propensity score-matched procedure and multivariate adjustment to evaluate postoperative major adverse outcomes in surgical patients with various clinical scenarios of asthma. Our findings showed patients with asthma had higher risks of postoperative pneumonia, septicemia, and urinary tract infection when compared with nonasthmatic patients. Among surgical patients with asthma, preoperative emergency visits, hospitalizations, or ICU stay because of asthma significantly increased postoperative adverse events. Preoperative use of systemic corticosteroids was also identified as an independent risk factor for postoperative complications and mortality.
Cardiovascular diseases, mental disorders, diabetes, and hyperlipidemia were identified as common coexisting medical conditions for patients with asthma and contributed to increased health care use, poor quality of life, and inadequate control for asthma.16–19 These comorbidities may change the asthma phenotype and act as confounding factors in assessment of asthma control and outcomes.17 Coexisting medical conditions, including diabetes, schizophrenia and liver cirrhosis, have been associated with postoperative adverse outcomes.12–14 To reduce confounding bias, these potential confounding factors were properly adjusted under matching procedure with propensity score and multivariate regression models in this study.
Hospitalization for asthma and use of systemic corticosteroids during the preceding 6 months might increase risk of future hospital admissions for asthma.20 This study showed history of asthma exacerbation in the prior 12 months is one of the strongest predictors of future exacerbations.21 We also found that the history of asthma-specific emergency visits, hospitalizations, ICU stay, and use of systemic corticosteroids were independent contributing factors for postoperative major adverse outcomes in asthmatic patients. Surgical patients with emergency care for asthma in the preoperative 3 months had nearly doubled risk of postoperative mortality compared with controls. Patients who were hospitalized for asthma in the 3 months preceding surgery had almost 3 times the risk of developing postoperative pneumonia compared with controls. Cumulative asthma-specific hospital stay and ICU admissions because of asthma in the prior 24 months were significantly associated with increased risk of postoperative complications and mortality.
Use of systemic corticosteroids is highly associated with the potential infectious complications because these inhibit the immune system and reduce inflammatory response, which may predispose patients to infection.22 A retrospective cohort study reported that asthmatic patients treated preoperatively with systemic corticosteroids received surgical procedures with a relatively low incidence of complications, including postoperative bronchospasm and wound infection.23 Another investigation showed corticosteroid-dependent asthmatic patients can tolerate surgical procedures well without serious pulmonary or wound complications.24 These studies, however, are limited by small sample sizes and are prone to referral bias, or lack the power to identify independent predictors of morbidity and mortality in surgical patients with asthma. Our study showed that use of systemic corticosteroids within 3 months before surgery significantly increased postoperative morbidity and mortality in asthmatic patients. The use of systemic corticosteroids implied that patients might have been treated with steroids because of active asthma, exacerbation of chronic asthma, or in a state of possible immune-suppression, all of which might contribute to increased postoperative morbidity and mortality. As history of asthma exacerbation can be easily and reliably obtained in preoperative evaluation, this should be routinely checked during preoperative assessment of surgical risks for asthmatic patients, especially their use of systemic corticosteroids, emergency visits, hospitalization, or ICU admission for asthma.25
Although the reason asthmatic patients had more postoperative adverse events than the general population is still unclear, several explanations can be considered. First, patients with asthma have increased risks of airway-related infections.26–28 Impaired innate and adaptive immune functions among asthmatic patients have been suggested as potential underlying mechanisms.29,30 Second, psychologic stress has been suspected as an asthma trigger in recent decades.31,32 Rather than directly causing the asthma symptoms, stress modulates the immune system and increases the magnitude of airway inflammatory response to allergens and irritants.33 Third, a number of perioperative medications, including anesthetics, can induce allergic reactions through histamine release. Neuromuscular blocking drugs are the most common medications to cause allergic reactions in the operating theatre, and some, such as mivacurium and atracurium, have histamine-releasing effects.34 Intraoperative IgE-mediated anaphylaxis can be triggered by rocuronium, succinylcholine, and vecuronium.35 There is a concern that nonsynthetic opioids such as morphine can induce bronchospasm through histamine release; however, few subject data support this.36 In addition, bronchospasm can be provoked by cold inspired gases, tracheal intubation, tracheal extubation, and airway suctioning. Increased airway tone because of vagal stimulation can be caused by endoscopy or peritoneal or visceral stretching during surgery.37 Finally, asthmatic patients were more likely to have psychiatric illness, which is a contributing factor for postoperative adverse events.13,38
This study has some limitations. First, Taiwan's National Health Insurance Research Database lacks data on asthmatic patients’ current symptoms and lung function, as well as laboratory data that would facilitate analysis of the association between severity of asthma and postoperative adverse outcomes. Second, detailed information on sociodemographics, dietary habits, and lifestyle factors was not available in the insurance claims data for this study to validate the association of these factors with postoperative adverse outcomes. Third, although the surgical patients without asthma were those who had no medical visits for asthma within 24 months before the index surgery, some mild or borderline asthma may have existed in this group such that the influence of asthma on postoperative outcomes may be underestimated. Finally, although we used matching procedure and multivariate adjustment to control several confounders, residual confounding is possible.
In conclusion, we showed that asthma significantly increased postoperative pneumonia, sepsis, urinary tract infection and subsequent mortality, particularly for asthmatic patients with preoperative asthma-related emergency care, hospitalizations, ICU admissions, and use of systemic corticosteroids. These risk factors need to be routinely considered during preoperative assessment of surgical patients with asthma to provide better perioperative care for this population.
Footnotes
Abbreviations: CI = confidence interval, ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification, OR = odds ratio.
This study is based in part on data obtained from the National Health Insurance Research Database, which is provided by Taiwan's Bureau of National Health Insurance of the Ministry of Health and Welfare, and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, the Ministry of Health and Welfare, or the National Health Research Institutes.
T-LC has equal contribution with the corresponding author.
This research was supported in part by Shuang Ho Hospital, Taipei Medical University (104TMU-SHH-23), Taiwan's Ministry of Science and Technology (MOST104-2314-B-038-027-MY2; MOST104-2221-E-038-015; and NSC102-2314-B-038-021-MY3), and Taiwan's Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med 2006; 355:2226–2235. [DOI] [PubMed] [Google Scholar]
- 2.National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma: summary Report 2007. J Allergy Clin Immunol 2007; 120:S94–S138. [DOI] [PubMed] [Google Scholar]
- 3.Fanta CH. Asthma. N Engl J Med 2009; 360:1002–1014. [DOI] [PubMed] [Google Scholar]
- 4.Masoli M, Fabian D, Holt S, et al. Global initiative for asthma program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004; 59:469–478. [DOI] [PubMed] [Google Scholar]
- 5.Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol 2011; 127:145–152. [DOI] [PubMed] [Google Scholar]
- 6.Lai CK, De Guia TS, Kim YY, et al. Asthma control in the asia-pacific region: the asthma insights and reality in asia-pacific study. J Allergy Clin Immunol 2003; 111:263–268. [DOI] [PubMed] [Google Scholar]
- 7.Birnbaum HG, Berger WE, Greenberg PE, et al. Direct and indirect costs of asthma to an employer. J Allergy Clin Immunol 2002; 109:264–270. [DOI] [PubMed] [Google Scholar]
- 8.Bahadori K, Doyle-Waters MM, Marra C, et al. Economic burden of asthma: a systematic review. BMC Pulm Med 2009; 19:9–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalra M, Buncher R, Amin RS. Asthma as a risk factor for respiratory complications after adenotonsillectomy in children with obstructive breathing during sleep. Ann Allergy Asthma Immunol 2005; 94:549–552. [DOI] [PubMed] [Google Scholar]
- 10.Warner DO, Warner MA, Barnes RD, et al. Perioperative respiratory complications in patients with asthma. Anesthesiology 1996; 85:460–467. [DOI] [PubMed] [Google Scholar]
- 11.Su FW, Beckman DB, Yarnold PA, et al. Low incidence of complications in asthmatic patients treated with preoperative corticosteroids. Allergy Asthma Proc 2004; 25:327–333. [PubMed] [Google Scholar]
- 12.Yeh CC, Liao CC, Chang YC, et al. Adverse outcomes after noncardiac surgery in patients with diabetes: a nationwide population-based retrospective cohort study. Diabetes Care 2013; 36:3216–3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liao CC, Shen WW, Chang CC, et al. Surgical adverse outcomes in patients with schizophrenia: a population-based study. Ann Surg 2013; 257:433–438. [DOI] [PubMed] [Google Scholar]
- 14.Lin CS, Lin SY, Chang CC, et al. Postoperative adverse outcomes after non-hepatic surgery in patients with liver cirrhosis. Br J Surg 2013; 100:1784–1790. [DOI] [PubMed] [Google Scholar]
- 15.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 1985; 39:33–38. [Google Scholar]
- 16.Cazzola M, Calzetta L, Bettoncelli G, et al. Asthma and comorbid medical illness. Eur Respir J 2011; 38:42–49. [DOI] [PubMed] [Google Scholar]
- 17.Boulet LP. Influence of comorbid conditions on asthma. Eur Respir J 2009; 33:897–906. [DOI] [PubMed] [Google Scholar]
- 18.Kuehn BM. Asthma linked to psychiatric disorders. J Am Med Assoc 2008; 299:158–160. [DOI] [PubMed] [Google Scholar]
- 19.Gershon AS, Wang C, Guan J, et al. Burden of comorbidity in individuals with asthma. Thorax 2010; 65:612–618. [DOI] [PubMed] [Google Scholar]
- 20.Lieu TA, Quesenberry CP, Sorel ME, et al. Computer-based models to identify high-risk children with asthma. Am J Respir Crit Care Med 1998; 157:1173–1180. [DOI] [PubMed] [Google Scholar]
- 21.Bloomberg GR, Trinkaus KM, Fisher EB, Jr, et al. Hospital readmissions for childhood asthma: a 10-year metropolitan study. Am J Respir Crit Care Med 2003; 167:1068–1076. [DOI] [PubMed] [Google Scholar]
- 22.Aberra FN, Lewis JD, Hass D, et al. Corticosteroids and immunomodulators: postoperative infectious complication risk in inflammatory bowel disease patients. Gastroenterology 2003; 125:320–327. [DOI] [PubMed] [Google Scholar]
- 23.Kabalin CS, Yarnold PR, Grammer LC. Low complication rate of corticosteroid-treated asthmatics undergoing surgical procedures. Arch Intern Med 1995; 155:1379–1384. [PubMed] [Google Scholar]
- 24.Oh SH, Patterson R. Surgery in corticosteroid-dependent asthmatics. J Allergy Clin Immunol 1974; 53:345–351. [DOI] [PubMed] [Google Scholar]
- 25.Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol 2012; 129:S34–S48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Juhn YJ, Kita H, Yawn BP, et al. Increased risk of serious pneumococcal disease in patients with asthma. J Allergy Clin Immunol 2008; 122:719–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klemets P, Lyytikäinen O, Ruutu P, et al. Risk of invasive pneumococcal infections among working age adults with asthma. Thorax 2010; 65:698–702. [DOI] [PubMed] [Google Scholar]
- 28.Talbot TR, Hartert TV, Mitchel E, et al. Asthma as a risk factor for invasive pneumococcal disease. N Engl J Med 2005; 352:2082–2090. [DOI] [PubMed] [Google Scholar]
- 29.Contoli M, Message SD, Laza-Stanca V, et al. Role of deficient type III interferon-lambda production in asthma exacerbations. Nat Med 2006; 12:1023–1026. [DOI] [PubMed] [Google Scholar]
- 30.Wark PA, Johnston SL, Bucchieri F, et al. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med 2005; 201:937–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Busse WW, Kiecolt-Glaser JK, Coe C, et al. NHLBI Workshop summary. Stress and asthma. Am J Respir Crit Care Med 1995; 151:249–252. [DOI] [PubMed] [Google Scholar]
- 32.Wright RJ, Rodriguez M, Cohen S. Review of psychosocial stress and asthma: an integrated biopsychosocial approach. Thorax 1998; 53:1066–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun 2007; 21:993–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hepner DL, Castells MC. Anaphylaxis during the perioperative period. Anesth Analg 2003; 97:1381–1395. [DOI] [PubMed] [Google Scholar]
- 35.Sadleir PH, Clarke RC, Bunning DL, et al. Anaphylaxis to neuromuscular blocking drugs: incidence and cross-reactivity in Western Australia from 2002 to 2011. Br J Anaesth 2013; 110:981–987. [DOI] [PubMed] [Google Scholar]
- 36.Rosow CE, Moss J, Philbin DM, et al. Histamine release during morphine and fentanyl anesthesia. Anesthesiology 1982; 56:93–96. [DOI] [PubMed] [Google Scholar]
- 37.Woods BD, Sladen RN. Perioperative considerations for the patient with asthma and bronchospasm. Br J Anaesth 2009; 103:i57–i65. [DOI] [PubMed] [Google Scholar]
- 38.Miles JF, Garden GM, Tunnicliffe WS, et al. Psychological morbidity and coping skills in patients with brittle and non-brittle asthma: a case-control study. Clin Exp Allergy 1997; 27:1151–1159. [DOI] [PubMed] [Google Scholar]


