Abstract
Patients with chronic obstructive pulmonary disease (COPD) have a high risk of osteoporosis and fractures. The incidence rate of hip fracture has steadily increased over time and is a major common event in patients with osteoporosis and COPD. Total hip replacement (THR) is commonly performed in patients with hip fracture. Our aim was to compare the complications of THR between patients with and without COPD.
Longitudinally linked data from the National Health Insurance Research Database, which consists of registration, claims, and reimbursement records, for a cohort of 1,000,000 randomly selected enrollees traced retrospectively from 1996 to 2000 in Taiwan. Patients who had undergone THR surgery between January 1, 2004, and December 31, 2008, were identified and divided into COPD and non-COPD cohorts. Outcomes and complications, including 90-day mortality, 1-year mortality, 1-year wound infection, 30-day readmission for hospitalization, 30-day pneumonia, 30-day acute respiratory failure, 30-day cerebrovascular accident, and length of stay during hospitalization, were measured after THR.
The COPD group had a significantly higher ratio of complications, including 30-day readmission (14.0% vs 8.4%), 30-day pneumonia (10.4% vs 4.4%), 30-day acute respiratory failure (1.5% vs 0.5%), 1-year mortality (6.9% vs 2.7%), and length of stay in the hospital (10.6% vs 0.8%) than the non-COPD group.
In addition to airway diseases, patients in the COPD group had higher mortality than those in non-COPD group after THR. Surgeons should give more attention to airway evaluation and selection of patients with COPD for THR.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a chronic systemic inflammatory disease and is one of the leading causes of death in the United States. Osteoporosis has been found to be the most common and serious comorbidity in patients with COPD,1 and fractures were found to account for the majority of adverse events after osteoporosis. Many factors contribute to fractures in patients with COPD, including old age, smoking habit, use of oral or inhaled corticoids, and sedentary lifestyle.1–6
Fractures and their complications are the clinical sequelae of osteoporosis. Hip fracture is one of the most serious potential consequences of osteoporosis because of the associated morbidities, which include pain, disabilities, and limitations in physical activity. These morbidities lead to diminished quality of life, the need for long-term care services, and premature mortality. Hip fracture is a major health problem, and the annual number of hip fractures is expected to increase worldwide from 1.66 million in 1990 to 6.26 million by 2050.7 Total hip replacement (THR) is commonly performed in patients with hip fractures, with excellent outcomes, and patient satisfaction.8 Patients with COPD have an increased risk of postoperative pulmonary complications that varies depending on the region of the body upon which the surgery is performed.9–11 The purpose of this study was to determine the relationship between COPD and THR outcomes by investigating the effect of COPD on complication rates and to compare the incidence of various types of complications in patients with and without COPD after receiving THR.
METHODS
Ethics Statement
This retrospective study was approved by the Institutional Review Board (IRB) of the Chi Mei Medical Center, Taiwan (IRB no. 10405-E04). Consent was specifically waived by the approving IRB because all personal identifying information was removed from the dataset and strict anonymity was maintained before further analysis.
Data Sources
Since March 1995, the Taiwan Department of Health has run the National Health Insurance (NHI) program, which is a compulsory single-payer health care plan with universal coverage. The NHI is operated by the Taiwanese government as a sole insurer that covers ∼99% of the total 23-million population and contracts with 97% of the healthcare providers of Taiwan.12 The NHI Research Database (NHIRD) is a medical claims database that was developed for research purposes and is managed by the National Health Research Institutes. To date, the NHIRD is one of the largest administrative health care databases in the world. It provides all inpatient and outpatient claims data from the NHI program, including patients’ demographic characteristics, disease diagnostic codes (based on the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM)), prescription records, and medical expenditures. In this study, we analyzed the longitudinally linked NHIRD data, which consists of registration, claims, and reimbursement records for a cohort of 1,000,000 randomly selected enrollees traced retrospectively from 1996 to 2000. The identities of these selected subjects were made anonymous by encrypting their original identification information. There were no statistically significant differences in age, sex, and health care cost distributions among the subjects.
Patients
Our study cohort consisted of patients who underwent THR surgery between January 1, 2004, and December 31, 2008, and were identified by ICD-9-CM codes 81.51 (THR), 81.52 (partial hip replacement), and 81.53 (revision of hip replacement) that were listed as the major operation in the NHIRD database. During the study period, only the data from the first-time THR registries were analyzed to ensure the independence of observations. The exclusion criteria included age <40 years and diagnosis with cancers before THR surgery (found ICD-9-CM 140–239 codes 3 years before the surgery date). In total, 2426 qualified patients who had THR surgery were preliminarily retrieved after the exclusion filtering (Figure 1). To investigate the complications of THR patients with a COPD history, the study cohort was divided into COPD and non-COPD groups in which the COPD patients were identified by the diagnostic codes (ICD-9-CM 490–492, 496) within 2 years before the THR surgery from their inpatient and outpatient records.
FIGURE 1.
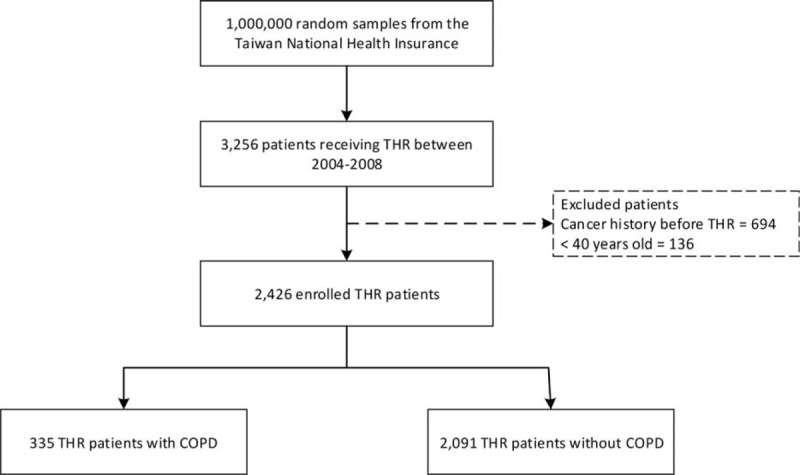
Flowchart of the patients included in the study.
Outcome Measures
The index date was the date of occurrence of administrative claims of THR surgery as operation codes. Eight study outcomes and complications were measured after the index date, including 90-day mortality, 1-year mortality, 1-year wound infection (ICD-9-CM codes 996.60,66,67,69; 998.3,5,59; 711.05,06,08; 730.25,26,28), 30-day readmission for hospitalization, 30-day pneumonia (ICD-9-CM codes 480–488), 30-day acute respiratory failure (ARF; ICD-9-CM codes 518.5,81,82,84), 30-day cerebrovascular accident (CVA; ICD-9-CM codes 430–437), and length of stay (LOS) during the hospitalization.
Other Variables
The covariate variables included the patients’ characteristics (age and sex) and comorbidities. The examined comorbidities were traced back from 2 years to the index date, which included cardiovascular disease (CVD; ICD-9-CM codes: 401–405), CVA (ICD-9-CM codes 430–438), chronic kidney disease (CKD; ICD-9-CM codes 582, 583, 585, 586, 588), and diabetes (ICD-9-CM code: 250).
Statistical Analysis
Continuous variables are presented as means (standard deviations), and discrete variables are expressed as frequencies and percentages. The chi-square test was performed to compare categorical variables, and Student's t test was used to compare continuous variables. A 2-sided P value of < 0.05 was considered to indicate statistical significance. To investigate associations of COPD with complications and mortality for patients who received THR, univariate analysis was performed using the Kaplan–Meier survival estimate, with significance determined by the log-rank test. Multiple regression analysis was performed by using a Cox proportional hazards model with the significant characteristics identified in the univariate tests and estimating the hazard ratios (HRs) and 95% confidence intervals (CIs). All statistical analyses were performed by using SPSS (version 15, SPSS Inc, Chicago, IL).
RESULTS
Patient Characteristics
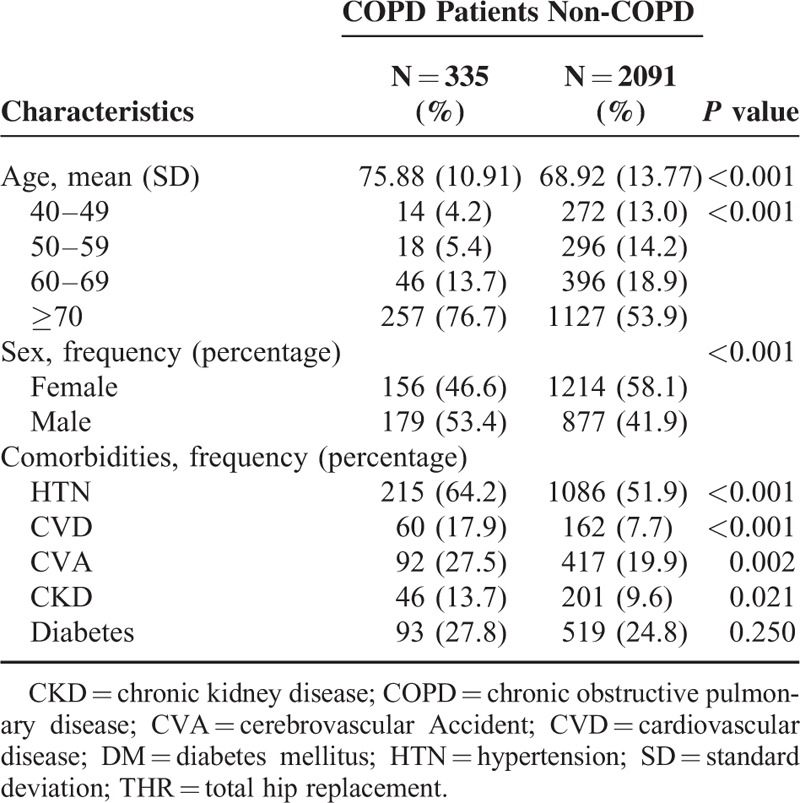
The comparisons of baseline characteristics between the COPD (335 patients) and non-COPD (control) (2091 patients) groups for patients who received THR are shown in Table 1. The COPD group had a significantly higher mean age (75.88 vs 68.92 years) with a higher percentage of patients age >70 years (76.7% vs 53.9%), a large proportion of men (53.4% vs 41.9%), and higher prevalence of comorbidities (HTN [64.2% vs 51.9%], CVD [17.9% vs 7.7%], CVA [27.5% vs 19.9%], and CKD [13.7% vs 9.6%]) than the non-COPD group did.
TABLE 1.
Demographics of Patients With/Without COPD Who Underwent THR
Univariate Analysis
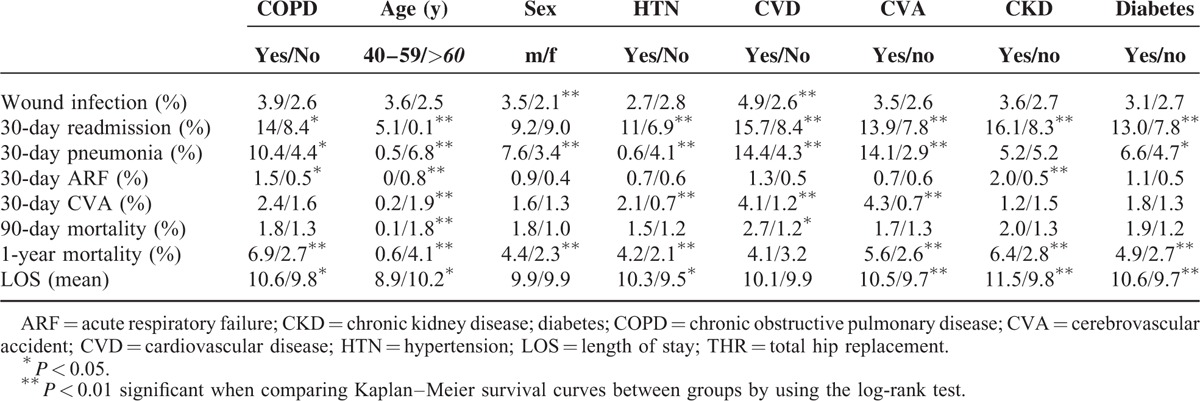
The COPD group had a significantly higher rate of complications than that of the non-COPD group (Table 2). The rates of 30-day readmission (14.0% vs 8.4%), 30-day pneumonia (10.4% vs 4.4%), 30-day ARF (1.5% vs 0.5%), 1-year mortality (6.9% vs 2.7%), and LOS (10.6% vs 9.8%) were higher in the COPD group than in the non-COPD group. In addition, possible risk factors for 8 other types of complications were examined. Age was associated with most complications except for wound infection. Sex was associated with would infection, 30-day pneumonia, and 1-year mortality. Most of the comorbidities (CVD, CVA, CKD, and diabetes) were significantly associated with 30-day readmission, 30-day pneumonia, 1-year mortality, and LOS.
TABLE 2.
Univariate Analysis for Risk Factors of Complications Following THR
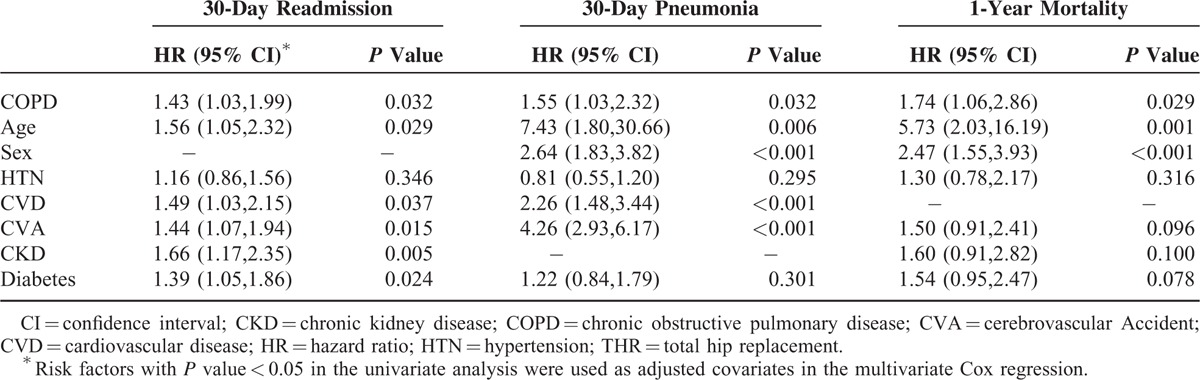
Multivariate Analysis
In the Cox regression analysis, the complication risks associated with COPD in the patients who received THR were analyzed by adjusting for the risk factors found to be significant from the univariate analysis (Table 3). After adjusting for age, HTN, CVD, CVA, CKD, and diabetes, the adjusted HR of 30-day readmission was 1.43 (95% CI = 1.03–1.99, P = 0.032) for the COPD group compared with the non-COPD group. After controlling for all risk covariates except CKD, the COPD group had a higher risk of 30-day pneumonia than the non-COPD group did (adjusted HR = 1.55; 95%, CI = 1.03–2.32, P = 0.032). Moreover, the adjusted HR for 1-year mortality was 1.74 (95% CI = 1.06–2.86, P = 0.029) for the COPD group compared with the non-COPD group after adjusting for all risk covariates except CVD.
TABLE 3.
Multivariate Analysis by Cox Regression of Complications Following THR
Cumulative Incidence Rate of Complications
Figure 2 shows the cumulative incidence curves of complications for the COPD and non-COPD groups. The log-rank test demonstrated significant differences in the complication risks between the COPD and non-COPD groups. The cumulative incidence curves of 30-day readmission, 30-day pneumonia, and 1-year mortality showed that the COPD group had significantly higher incidence rates than the non-COPD group did.
FIGURE 2.
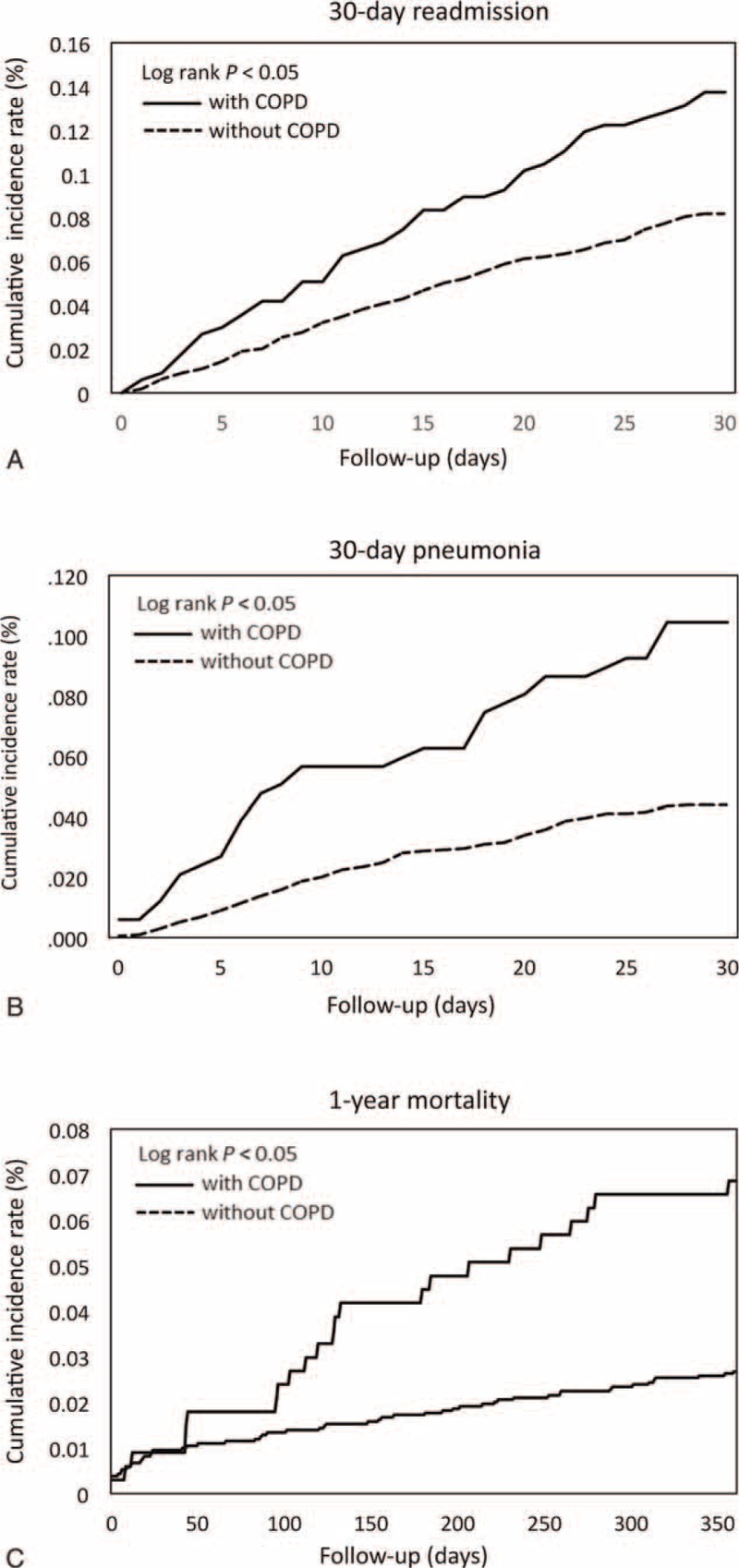
Cumulative incidence rates of complications as shown by (A) 30-day readmissions, (B) development of pneumonia within 30 days, and (C) 1-year mortality in patients with and without chronic obstructive pulmonary disease (COPD) after receiving total hip replacement. Significant differences in the complication risks between the 2 groups are shown by the log-rank test. The cumulative incidence curves show that the patients with COPD had a higher incidence rate than those without COPD did.
DISCUSSION
The mean age at the time of surgery in the COPD group was 75.88 years, which was older than the non-COPD group. In our study population of patients who had undergone THR, the mean age of the COPD group was greater than that of 75 years for THR patients in the general population determined in a previous study.13 The most common comorbidities in the COPD group were hypertension, followed by diabetes and cerebrovascular disease. Medical comorbidities were common among the COPD patients in our study, and their prevalences were higher than those reported in another study.14
COPD and Wound Infection
In our study, the percentage of patients who developed wound infection was 2.6% to 3.9% after undergoing hip replacement. The wound infection rate was higher in our study than that found in a previous retrospective study that used a Medicare database of patients identified between 1991 and 2008; that study found that the infection rate of hip replacement was about 1% in adults ≥65 years of age. In that study, wound infections were those evaluated during the index hospital stay and those requiring readmissions in the primary or revision total hip arthroplasty cohort.13 In our study, wound infections were those assessed not only during the hospitalization period but also during outpatient treatment. The high rate of wound infection was probably because of the less stringent inclusion criteria in our study than those in the previous study.
Earlier studies have reported that risk factors for prosthetic joint infection included National Nosocomial Infection Surveillance System risk scores of 1 or 2, previous native joint infection or arthroplasty, surgical site infection, malignancy history, advanced age, diabetes mellitus, obesity, poor nutrition, skin disease, and pre-existing joint disease.15–17 Our findings suggest that COPD is not associated with an increased risk of prosthetic hip joint infection.
COPD and Readmission
Readmission to the hospital after an operation, including THR, increases medical expenditures and is an undesirable outcome. A previous study used administrative data to identify hospital readmissions occurring ≤90 days of discharge after THR. Primary THR was associated with a 5% unplanned readmission rate at 90 days in the general population, and the risk factors included the type of procedure, hospital stay >5 days, cardiac valvular disease, diabetes with end-organ complications, and substance abuse.18 Other studies have shown that the factors associated with readmission in general medical patients included inpatient use of narcotics or corticosteroids and conditions affecting major organ systems, including COPD and systemic conditions (coagulopathy, body weight loss, anemia, and fluid and electrolyte imbalance).19,20 In our study, we found that the rates for readmission and postoperative pneumonia were higher in the patients with COPD than in the patients without COPD after THR, which suggests that physicians should pay greater attention to postoperative care of patients with COPD after THR.
COPD and Complications After THR
The actual risk of myocardial infarction after THR is a matter of debate. From a retrospective, nationwide cohort study in Denmark, the risk of acute myocardial infarction increased about 25-fold in patients who underwent THR relative to the risk in the controls in the first 2 postoperative weeks, and the risk was about 5-fold at 2 to 6 weeks after THR.21 Another study showed that the risk of acute myocardial infarction did not increase within 1 year after THR relative to that of controls and there was no significant difference in the rates after 1 year between the THR patients and controls.22 The increased risk of myocardial infarction after THR may be related to thromboembolism or hemodynamic change during the surgical procedure or to arrhythmias and hypoxia during anesthesia.23,24 In our study, only 1 patient had a myocardial infarction after THR. The possible reasons for the low risk of myocardial infarction in our study were the low incidence of venous thromboembolism after operation in Asian populations25 and that the surgeon may have selected patients who were healthy enough to receive THR.
COPD places a patient at risk of developing pneumonia and is one of the most common comorbidities in pneumonia patients. Pneumonia is a serious condition and increases the risk of respiratory failure in patients with COPD and leads to higher mortality in these patients than that in those without COPD.26 Our study also demonstrated that the patients with COPD had a higher risk of postoperative pneumonia after THR than those without COPD did, and there was also significant difference in the risk of acute respiratory failure. Patients with COPD have a higher risk of pneumonia and acute respiratory failure after THR, so chest care after surgery to reduce the risk of pneumonia is important in these patients.
COPD and Thromboembolism After THR
The risk of thromboembolism is high in patients undergoing orthopedic surgery, and a greater risk of mortality was found among patients with pulmonary embolisms.27,28 Many studies have shown the high prevalence of venous thromboembolism, including deep vein thrombosis and pulmonary embolism, in patients with COPD and acute exacerbations,29–31 but venous thromboembolism is less likely to occur in Asian countries than in Western countries, not only during hospitalization but also after orthopedic surgery.32 The mechanism for this phenomenon is not clear and requires further investigation. In our studies, the risk of venous thromboembolism has been very low after THR in patients with COPD (data not shown) and was comparable to the risk shown in previous studies, which suggests a lower risk of venous thromboembolism in Asian patients even after high-risk orthopedic surgery.
COPD and Mortality After THR
In our study, the mortality rate at 90 days after THR was between 1.3 and 1.8%, and there was no significant difference in the rates between the patients with or without COPD. These results differed from those in another study in which the inpatient mortality risk at 90 days was 18.3% after hemiarthroplasty for hip fracture in patients with advanced age (≥85 years) and the 90-day mortality for patients aged 65 to 84 years was 9.8%.33 Old age and multiple comorbidities increase the risk of poor outcomes after THR. Many retrospective studies have demonstrated that age was an independent risk factor for higher mortality rates after THR for a period of 1 year from the date of operation.34–37
We found that the 1-year mortality rate was higher in patients with COPD after THR than in those without COPD. COPD may have an important role in long-term outcomes of patient who have undergone THR. Further interventions, including medication and rehabilitation, that focus on patients with COPD may help reduce morbidity and improve survival.
Limitations
There were some limitations in our study. First, we had no information about the severity of osteoporosis. Second, we also lacked laboratory data, including pulmonary function and dyspnea scale values. Although disease severity was not classified, we generally assessed postoperative complications during long-term follow-up of patients with COPD, results that have not been reported previously. A prospective study based on clinical and laboratory data would be necessary to verify the effect of disease severity on long-term prognosis after THR in patients with COPD.
CONCLUSIONS
This longitudinal analysis of national administrative data showed a number of complications and outcomes in patients with COPD after THR. Our study provides important information to healthcare professionals given that THR is a common orthopedic procedure, the incidence of COPD increases rapidly with age.
In our study, we found that the rates for readmission and postoperative pneumonia and the 1-year mortality rate were higher in the patients with COPD than in the patients without COPD after THR. It is important for caregivers to reduce the risk of developing pneumonia in patients with COPD. Further study on reducing long-term mortality after THR is needed.
Acknowledgment
The authors express their sincere gratitude to Mr. Jun-You Liao (Department of Industrial Engineering and Management, National Yunlin University of Science and Technology) for his effort in organizing data and assisting statistical analysis.
Footnotes
Abbreviations: CI = confidence interval, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CVA = cerebrovascular accident, CVD = cardiovascular disease, DM = diabetes mellitus, HR = hazard ratio, LHID = Longitudinal Health Insurance Database, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database, SD = standard deviation, THR = total hip replacement.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Ionescu AA, Schoon E. Osteoporosis in chronic obstructive pulmonary disease. Eur Respir J 2003; 22 suppl 46:64s–75s. [DOI] [PubMed] [Google Scholar]
- 2.Jorgensen NR, Schwarz P. Osteoporosis in chronic obstructive pulmonary disease. Curr Opin Pulm Med 2008; 14:84–92. [DOI] [PubMed] [Google Scholar]
- 3.Gross NJ. Extrapulmonary effects of chronic obstructive pulmonary disease. Curr Opin Pulm Med 2001; 7:122–127. [DOI] [PubMed] [Google Scholar]
- 4.Gan WZ, Man SFP, Senthilselvan A, et al. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 2004; 59:574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gluck O, Colic G. Recognizing and treating glucocorticoid induced osteoporosis in patients with pulmonary disease. Chest 2004; 125:1859–1876. [DOI] [PubMed] [Google Scholar]
- 6.Antonelli Incalzi R, Caradonna P, Ranieri P, et al. Correlates of osteoporosis in chronic obstructive pulmonary disease. Resp Med 2000; 94:1079–1084. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int 1992; 2:285–289. [DOI] [PubMed] [Google Scholar]
- 8.Anakwe RE, Middleton SD, Jenkins PJ, et al. Total hip replacement in patients with hip fracture: a matched cohort study. Trauma Acute Care Surg 2012; 73:738–742. [DOI] [PubMed] [Google Scholar]
- 9.Arozullah AM, Khuri SF, Henderson WG, et al. Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 2001; 135:847–857. [DOI] [PubMed] [Google Scholar]
- 10.Smetana GW. Preoperative pulmonary evaluation. N Engl J Med 1999; 340:937–944. [DOI] [PubMed] [Google Scholar]
- 11.Trayner E, Jr, Celli BR. Postoperative pulmonary complications. Med Clin North Am 2001; 85:1129–1139. [DOI] [PubMed] [Google Scholar]
- 12.Wu CC, Hsu TW, Chang CM, et al. Age-adjusted Charlson comorbidity index scores as predictor of survival in colorectal cancer patients who underwent surgical resection and chemoradiation. Medicine (Baltimore) 2015; 94:e431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolf BR, Lu X, Li Y, et al. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am 2012; 94:e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapoor A, Labonte AJ, Winter MR, et al. Risk of venous thromboembolism after total hip and knee replacement in older adults with comorbidity and co-occurring comorbidities in the Nationwide Inpatient Sample (2003-2006). BMC Geriatrics 2010; 10:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berbari E, Hanssen A, Duffy M, et al. Risk factors for prosthetic joint infection: case-control study. Clin Infect Dis 1998; 27:1247–1254. [DOI] [PubMed] [Google Scholar]
- 16.Wilson M, Kelley K, Thornhill T. Infection as a complication of total knee-replacement arthroplasty. Risk factors and treatment in sixty-seven cases. J Bone Joint Surg Am 1990; 72:878–883. [PubMed] [Google Scholar]
- 17.Zimmerli W. Infection and musculoskeletal conditions: prosthetic-joint-associated infections. Best Pract Res Clin Rheumatol 2006; 20:1045–1063. [DOI] [PubMed] [Google Scholar]
- 18.Schairer WW, Sing DC, Vail TP, et al. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res 2014; 472:464–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nazima A, Arpana V, Judith M, et al. Redefining readmission risk factors for general medicine patients. J Hosp Med 2011; 6:54–60. [DOI] [PubMed] [Google Scholar]
- 20.Silverstein MD, Qin H, Mercer SQ, et al. Risk factors for 30-day hospital readmission in patients ≥65 years of age. Proc (Bayl Univ Med Cent) 2008; 21:363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lalmohamed A, Vestergaard P, Klop C, et al. Timing of acute myocardial infarction in patients undergoing total hip or knee replacement. Arch Intern Med 2012; 172:1229–1235. [DOI] [PubMed] [Google Scholar]
- 22.Klop C, de Vries F, Lalmohamed A, et al. Risk of myocardial infarction in Dutch patients following discharge for total hip/knee replacement and matched controls: a population-based cohort study. OA Epidemiol 2013; 1:6. [Google Scholar]
- 23.Hofmann S, Huemer G, Kratochwill C, et al. Pathophysiology of fat embolisms in orthopedics and traumatology. Orthopade 1995; 24:84–93. [PubMed] [Google Scholar]
- 24.Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). J Am Coll Cardiol 2002; 39:542–553. [DOI] [PubMed] [Google Scholar]
- 25.Lee WS, Kim KI, Lee HJ, et al. The incidence of pulmonary embolism and deep vein thrombosis after knee arthroplasty in Asians remains low: a meta-analysis. Clin Orthop Relat Res 2013; 471:1523–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Restrepo MI, Mortensen EM, Pugh JA, et al. COPD is associated with increased mortality in patients with community-acquired pneumonia. Eur Respir J 2006; 28:346–351. [DOI] [PubMed] [Google Scholar]
- 27.Collins R, Scrimgeour A, Yusuf S, et al. Reduction in fatal pulmonary embolism and venous thrombosis by perioperative administration of subcutaneous heparin. Overview of results of randomized trials in general, orthopedic, and urologic surgery. N Engl J Med 1988; 318:1162–1173. [DOI] [PubMed] [Google Scholar]
- 28.Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999; 353:1386–1389. [DOI] [PubMed] [Google Scholar]
- 29.Gunen H, Gulbas G, In E, et al. Venous thromboemboli and exacerbations of COPD. Eur Respir J 2010; 35:1243–1248. [DOI] [PubMed] [Google Scholar]
- 30.Stein PD, Beemath A, Meyers FA, et al. Pulmonary embolism and deep venous thrombosis in hospitalized adults with chronic obstructive pulmonary disease. J Cardiovasc Med (Hagerstown) 2007; 8:253–257. [DOI] [PubMed] [Google Scholar]
- 31.Tan KK, Koh WP, Chao AK. Risk factors and presentation of deep venous thrombosis among Asian patients: a hospital-based case-control study in Singapore. Ann Vasc Surg 2007; 21:490–495. [DOI] [PubMed] [Google Scholar]
- 32.Jameson SS, Khan SK, Baker P, et al. A national analysis of complications following hemiarthroplasty for hip fracture in older patients. Q J Med 2012; 105:455–460. [DOI] [PubMed] [Google Scholar]
- 33.Koval KJ, Skovron ML, Aharonoff GB, et al. Predictors of functional recovery after hip fracture in the elderly. Clin Orthop Relat Res 1998; 348:22–28. [PubMed] [Google Scholar]
- 34.Parvizi J, Ereth MH, Lewallen DG. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg 2004; 86:1983–1988. [DOI] [PubMed] [Google Scholar]
- 35.Björkelund KB, Hommel A, Thorngren KG, et al. Factors at admission associated with 4 months outcome in elderly patients with hip fracture. AANA J 2009; 77:49–58. [PubMed] [Google Scholar]
- 36.Hindmarsh DM, Hayen A, Finch CF, et al. Relative survival after hospitalisation for hip fracture in older people in New South Wales, Australia. Osteoporos Int 2009; 20:221–229. [DOI] [PubMed] [Google Scholar]
- 37.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013; 380:2095–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]


