Abstract
Apolipoprotein B (apoB) has additional benefits over conventional lipid measurements in predicting future cardiovascular disease (CVD). We aimed to validate the clinical relevance of our equation to estimate apoB in a large-scale, prospective, community-based cohort study (Ansung-Ansan cohort study).
A total of 9001 Korean subjects were assessed. We excluded subjects with history of CVD (n = 228), taking lipid-lowering medications (n = 51), and those whose outcome data were not available (n = 33). Finally, a total of 8713 subjects (4126 men and 4587 women) with a mean age of 52.2 years were enrolled and followed up biannually for a mean 8.1 years.
At baseline, 24.9% of subjects were current smokers, 12.5% had diabetes, and 22.2% had hypertension. Incident case of CVD occurred in 600 of the study subjects (493 ischemic heart disease and 424 stroke). Independent variables included in the models were age, sex, waist circumference, current smoking, and presence of diabetes and hypertension. Both non-HDL cholesterol (HR per 1-SD [95% CI]; 1.13 [1.05–1.23], P = 0.002) and estimated apoB (HR per 1-SD [95% CI]; 1.14 [1.05–1.24], P = 0.001) were independently associated with the development of CVD; however, the LDL cholesterol level was not predictive of future CVD (HR per 1-SD [95% CI]; 1.07 [0.99–1.16], P = 0.08).
Both non-HDL cholesterol and estimated apoB level were independently associated with the development of CVD. Because LDL cholesterol has limited value to predict incident CVD, we recommend calculating non-HDL cholesterol or apoB with our equation to predict risk of incident CVD in the general Korean population.
Keywords: apolipoprotein B, cardiovascular disease, cohort study, ischemic heart disease, stroke
1. Introduction
Accumulating evidence suggests that apolipoprotein B (apoB) has additional benefits over conventional lipid measurements, such as serum low-density lipoprotein (LDL) cholesterol, for the assessment of future development of cardiovascular disease (CVD).[1–3] Despite this evidence, the serum apoB level is not routinely measured because of the additional cost. Recently, we developed a new equation to estimate serum apoB (apoBE) using the same serum total cholesterol, triglyceride, and high-density lipoprotein (HDL) cholesterol level used in Friedewald's equation to estimate LDL cholesterol. In this study, apoBE was accurate not only for the entire study population, but also for several subgroups, including patients with diabetes, those with atherogenic dyslipidemia, and those taking lipid-lowering agents. In addition, contrary to Friedewald's equation, our apoBE can be applied regardless of serum triglyceride range.[4]
Despite the strong approximation with directly measured apoB, it is still uncertain whether apoBE has clinical relevance in the prediction of the development of CVD. Therefore, the aim of this study was to validate the clinical relevance of apoBE in predicting future CVD and to compare the performance of the equation with LDL cholesterol level from Friedewald's equation using data from a large-scale, prospective, community-based cohort.
2. Materials and methods
2.1. Study subjects
Study subjects were individuals who participated in the Ansung–Ansan cohort study from 2001–2002 (baseline year) to 2011–2012 (fifth follow-up visit). The Ansung–Ansan cohort study is an ongoing study that began in 2001 to 2002 and involves biennial follow-up examinations. The design and baseline characteristics of the Ansung–Ansan cohort study have been published in previous studies.[5,6] In brief, residents of 2 South Korean communities (Ansung and Ansan) were recruited for this study. Eligibility criteria included an age of 40 to 69 years and residence within the borders of the survey area for at least 6 months before testing. In 2001 to 2002 (baseline year), 5018 of the 7192 eligible individuals in Ansung were surveyed using a cluster sampling method. A total of 15,580 individuals in Ansan were eligible, and 5020 were recruited using a random sampling method of the local telephone directory. In this study, 9001 subjects were analyzed after excluding 1037 subjects who did not visit their follow-up examinations. In addition, we further excluded subjects as follows: (1) those with history of CVD (n = 228); (2) those taking lipid-lowering medications (n = 51); and (3) those whose outcome data were not available (n = 33). Finally, a total of 8713 subjects without CVD history (4126 men and 4587 women; mean age, 52.2 years) were enrolled in the study. Subjects were followed for a mean of 8.1 years.
Informed consent was obtained from all study subjects. The study protocol was approved by the ethics committee of the Korean Center for Disease Control and the Ajou University School of Medicine Institutional Review Board.
2.2. Clinical and biochemical parameters
Methodological explanations including anthropometric and biochemical measurements have been described in previous studies.[6,7] Collected blood samples were delivered and analyzed at a central laboratory (Seoul Clinical Laboratories, Seoul, Korea). Plasma glucose, total cholesterol, triglyceride, and HDL cholesterol levels were determined using a Hitachi 747 chemistry analyzer (Hitachi, Tokyo, Japan). The LDL cholesterol level was calculated using Friedewald's equation.
All subjects underwent a 75-g oral glucose tolerance test (OGTT) after a 8- to 14-hour overnight fast at study inclusion and biennially thereafter. The HbA1c level was measured using high-performance liquid chromatography (Variant II; BioRad Laboratories, Hercules, CA). Fasting plasma insulin concentration was determined using radioimmunoassay (LINCO kit; St Charles, MO). Insulin resistance was calculated using the homeostasis model assessment (HOMA-IR) as the product of fasting serum insulin (mU/L) and fasting plasma glucose (mg/dL) concentrations divided by 405.[8]
2.3. Definition
In the present study, diabetes mellitus was defined as one of the following: (1) fasting plasma glucose level ≥7.0 mmol/L (126 mg/dL); (2) 2-hour plasma glucose ≥11.1 mmol/L (200 mg/dL) after 75-g OGTT; (3) HbA1c level ≥6.5%; (4) use of oral antidiabetic agent or insulin; or (5) a self-reported history of diabetes.[9] Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, use of antihypertensive drugs, or self-reported history of hypertension. In this study, CVD was divided into ischemic heart disease (IHD) and stroke, and IHD included myocardial infarction and coronary heart disease. Incidence events were self-reported by interview-based questionnaires. The Framingham risk score was calculated using criteria on ATP III guidelines.[10]
Estimated apoB was calculated using an equation introduced in our previous study: ApoB = 0.65 × total cholesterol – 0.59 × HDL cholesterol + 0.01× triglyceride (if triglyceride ≤270 mg/dL)/ApoB = 25.6 + 0.58× total cholesterol – 0.38× HDL cholesterol – 0.06× triglyceride (if triglyceride >270 mg/dL)[4]. Our apoB equation has a coefficient of determination (R2) of 0.994 for directly measured apoB, and the residuals in the development, internal validation, and external validation datasets were randomly distributed around 0 with no clear trends.[4]
2.4. Statistical analysis
All data are expressed as the mean ± SD or as proportion. The Kaplan–Meier survival curve was used to compare the development of CVD according to the median value of LDL cholesterol or estimated apoB. Survival analyses were used to determine the associations between clinical measurements including lipid parameters and incidence of CVD. To compare these measurements, we calculated hazard ratios (HR) per 1-SD increment using a Cox proportional hazards model. Multivariate Cox proportional hazard regression analyses were performed to determine whether various lipid parameters were associated with incident CVD independent of age, sex, waist circumference, current smoking, diabetes, and hypertension. Harrel's C statistic was used to compare the performance of the models in predicting future outcomes. Analyses were performed using R version 2.14.2 (http://www.r-project.org). P values <0.05 were considered statistically significant.
3. Results
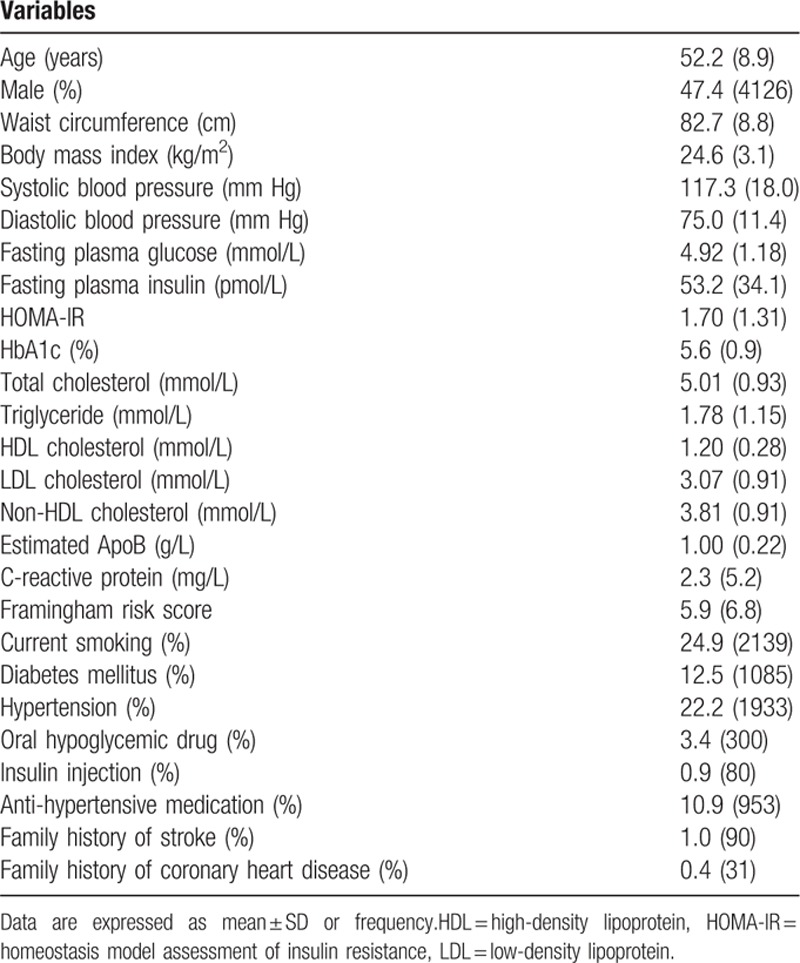
Table 1 depicts baseline characteristics of the study population. The mean age was 52.2 years, and 47.4% of the subjects were male. The mean body mass index (BMI) was 24.6 kg/m2 and fell into the category of overweight. At baseline, 24.9% of subjects were current smokers, 12.5% had diabetes, and 22.2% had hypertension.
Table 1.
Baseline characteristics.
Incident CVD occurred in 600 of the study subjects (493 IHD and 424 stroke) during the mean 8.1-year follow-up, leading to a cumulative incidence of 6.9%. In univariate Cox proportional hazard regression analysis, a variety of conventional risk factors, including age, BMI, waist circumference, blood pressures, HOMA-IR, and presence of diabetes and hypertension, were associated with the development of CVD. Among all lipid measurements, non-HDL cholesterol (HR per 1-SD increment [95% CI]; 1.24 [1.15–1.34], P < 0.001) and estimated apoB (HR per 1-SD increment [95% CI]; 1.24 [1.15–1.34], P < 0.001) levels showed the strongest associations with the development of CVD, and their HRs were identical. However, the LDL cholesterol level showed a somewhat weaker association with the development of CVD compared with non-HDL cholesterol or estimated apoB level (HR per 1-SD increment [95% CI]; 1.11 [1.03–1.12], P = 0.008) (Table 2). In addition, when the subjects were divided into 2 groups according to median levels, estimated apoB was discriminative earlier than LDL cholesterol for the development of incident CVD (Fig. 1). Similarly, in a separate analysis, non-HDL cholesterol and estimated apoB levels were more powerful predictors of future IHD and stroke than was the LDL cholesterol level.
Table 2.
Univariate Cox proportional hazard regression analysis.
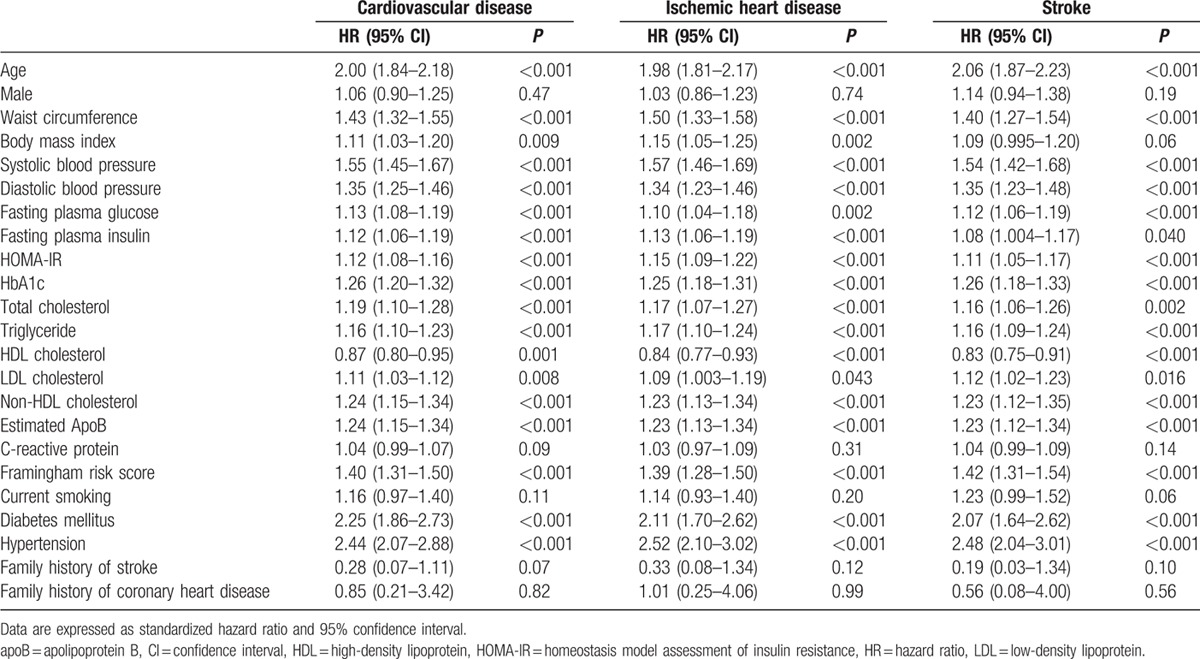
Figure 1.
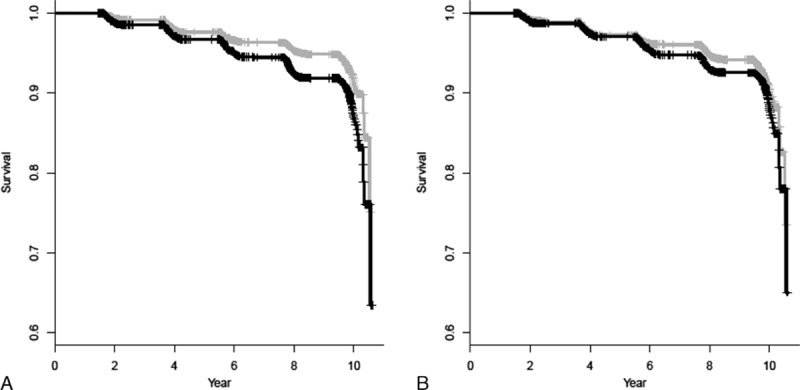
Kaplan–Meier survival curve for development of cardiovascular disease according to median estimated apoB (A, P < 0.001) and LDL cholesterol (B, P = 0.017) levels. Black and gray lines represent the upper and lower median for corresponding variables, respectively. LDL = low-density lipoprotein.
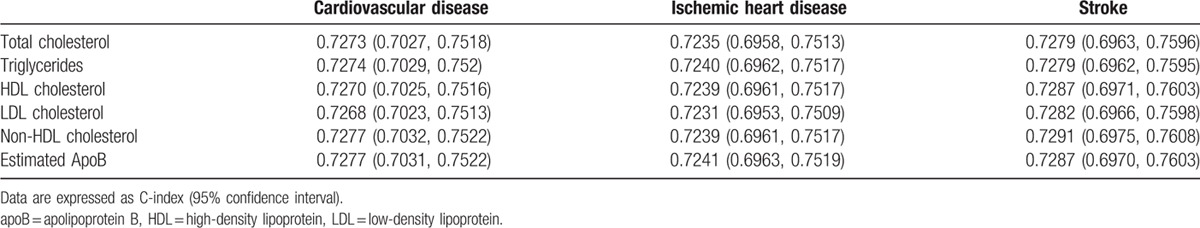
The results of the multivariate Cox regression analysis are shown in Table 3. Independent variables included in the models were age, sex, waist circumference, current smoking, and presence of diabetes and hypertension. Both non-HDL cholesterol (HR per 1-SD increment [95% CI]; 1.13 [1.05–1.23], P = 0.002) and estimated apoB (HR per 1-SD increment [95% CI]; 1.14 [1.05–1.24], P = 0.001) were associated with the development of CVD independent of the aforementioned risk factors. In addition, both non-HDL cholesterol and estimated apoB showed significant independent associations with future IHD and stroke, and the hazard ratios were comparable. However, the LDL cholesterol level was not predictive of any cardiovascular outcome in this analysis (Table 3). In addition, no difference in performance between the non-HDL cholesterol model and the estimated apoB model in predicting future outcomes (Table 4).
Table 3.
Multivariate Cox proportional hazard regression analysis of lipid parameters.
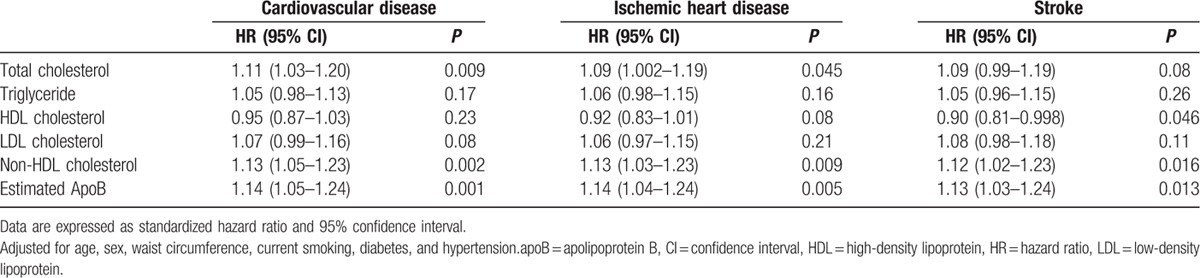
Table 4.
C statistics for future cardiovascular outcomes.
4. Discussion
In the current prospective, community-based, cohort study performed in 8713 subjects from a general Korean population, our newly developed equation to estimate apoB, which was calculated from total cholesterol, triglyceride, and HDL cholesterol levels, was predictive of future CVD independent of other well-established risk factors including age, sex, waist circumference, current smoking, and presence of diabetes and hypertension during 8.1 years of follow-up. In addition to the association with CVD, estimated apoB was predictive of both incident IHD and stroke when the outcomes were analyzed separately.
Several, but not all, epidemiologic studies and clinical trials have demonstrated that both non-HDL cholesterol and apoB are superior to LDL cholesterol in predicting future development of CVD[1–3]; however, there is much debate over whether apoB has additional clinical benefit in predicting future CVD over non-HDL cholesterol.[11,12] In a meta-analysis of 12 reports including 233,455 subjects and 22,950 events, apoB was the most potent marker of cardiovascular risk (relative risk ratio, 1.43; 95% CI, 1.35–1.51), LDL cholesterol was the least potent (relative risk ratio, 1.25; 95% CI, 1.18–1.33), and non-HDL cholesterol was intermediate (relative risk ratio, 1.34; 95% CI, 1.24–1.44).[1] However, another meta-analysis based on 91,307 participants (including 4499 cases) from 22 studies found that HRs for coronary heart disease were similar between apoB (HR, 1.58; 95% CI, 1.39–1.79) and non-HDL cholesterol (HR, 1.59; 95% CI, 1.36–1.85).[13] In the present study, estimated apoB (HR per 1-SD [95% CI]; 1.14 [1.05–1.24], P = 0.001) and non-HDL cholesterol (HR per 1-SD [95% CI]; 1.13 [1.05–1.23], P = 0.002) showed almost identical association with incident CVD and had similar risk for both incident IHD and stoke. In addition, there was no difference in performance between the non-HDL cholesterol model and the estimated apoB model in predicting future CVD, ischemic heart disease, or stroke. Therefore, it appears that our equation to estimate apoB has comparable predictive ability for future CVD. Collectively, estimated apoB can be used to predict a diverse spectrum of vascular events, and its performance was grossly similar to that of non-HDL cholesterol. It has also been suggested that there is no difference between apoB and non-HDL cholesterol in predicting CVD risk in a healthy, low-risk group in which a relatively small number of subjects would have increased numbers of small dense LDL particles, the group in which apoB has a greater predictive value.[11]
Based on our observations, it is possible that lipid parameters are not powerful predictors for incident CVD in the Korean population compared with other ethnic groups. In our study, adjusted HR of non-HDL cholesterol and estimated apoB for cardiovascular outcomes ranged from 1.12 to 1.14, somewhat lower than those noted in the 2 aforementioned meta-analyses. In addition, most of the conventional lipid parameters were not associated with future cardiovascular outcome in this analysis. In particular, LDL cholesterol was not associated with future CVD, IHD, or stroke. Rather, total cholesterol was associated mainly with IHD, and HDL cholesterol showed an inverse association with future development of stroke. Although we cannot explain clearly the reason for the null association between LDL cholesterol and incident CVD, we offer the following as plausible explanations. First, it has been suggested that the association between the LDL cholesterol level and the development of CVD is not strong in Asians as it is in Caucasians. In a community-based, prospective cohort study of CVD performed in 4696 Japanese men and women, the LDL cholesterol level was not associated with future myocardial infarction or cerebral infarction in either men or women during an 11.9-year follow-up. LDL cholesterol was associated with incident myocardial infarction only when data from men and women were combined and LDL cholesterol level was in the highest quintile (≥3.91 mmol/L in men and ≥4.23 mmol/L in women)[14]. In addition, among 8131 residents from 4 Japanese communities who had no history of CVD, the LDL cholesterol level could not predict future myocardial infarction or total coronary heart disease in either men or women after adjustment for potential confounding factors within low-to-moderate mean LDL cholesterol level (<3.08 mmol/L). The mean LDL cholesterol level of our study subjects falls into this category (mean LDL cholesterol of 3.07 mmol/L).[15] Furthermore, a meta-analysis of 32 cohort studies performed in the Asia-Pacific region showed that calculated LDL cholesterol was a relatively poor predictor of future CVD and coronary heart disease compared with lipid parameters including triglycerides, HDL cholesterol, and non-HDL cholesterol.[16] Second, robust adjustment for other risk factors of future CVD including current smoking, hypertension, and diabetes might dilute the association between LDL cholesterol and the development of cardiovascular outcomes. Third, our study subjects were recruited from community-based residents. Eight years of follow-up might not be long enough to reveal the association between LDL cholesterol and incident CVD in such a healthy population.
This study has some limitations. First, we did not directly measure apoB level. Thus, it was not possible to compare the performance of estimated apoB from our equation and directly measured apoB in the prediction of CVD. However, we demonstrated the accuracy of our equation not only with internal validation, but also with external validation. Moreover, the equation can be used in diverse subgroups of patients including those with diabetes, atherogenic dyslipidemia, and those taking lipid-lowering agents. Therefore, we expect that apoB estimated with our equation approximates direct apoB in our study population. Second, our study subjects were generally healthy, as they were selected from a community-based general population. A negligible proportion of the subjects had history of CVD (2.5%) or took lipid-lowering medications (0.6%), and we could not validate the performance of our equation in these critical subgroups. Therefore, our results cannot be generalized to subjects with diverse cardiovascular risk and clinical conditions. Third, in this study, cardiovascular outcomes were assessed by questionnaire, which can result in bias. Lastly, our apoBE was developed and validated using data from a Korean population. Thus, it is uncertain whether this measure is also valid in other ethnic groups. However, in our previous study, we validated the accuracy of our apoBE using data from NHANES 2007 to 2008 for other ethnicities. As a result, the residuals were randomly distributed around 0, and no trend was observed.[4] This indicates that estimated apoB from apoBE predicts directly measured apoB without bias in other ethnic groups. Despite the limitations, we conducted this study with a large community-based population and showed that it is reasonable to calculate apoB with our equation without additional cost to measure direct apoB level in order to predict incident CVD for relatively healthy subjects without previous CVD.
In conclusion, the estimated apoB level from our equation was independently associated with future development of cardiovascular outcomes, and the predictive power for incident CVD was comparable to that of non-HDL cholesterol. In addition, although our equation used the same lipid measures with Friedewald's equation, it showed a stronger association with future CVD than did any other lipid measures including LDL cholesterol and can be applied regardless of triglyceride range. Based on our observations, LDL cholesterol has limited value to predict the development of CVD in Koreans.
Footnotes
Abbreviations: ApoB = apolipoprotein B, ApoBE = apolipoprotein B equation, BMI = body mass index, CVD = cardiovascular disease, HOMA = homeostasis model assessment, IHD = ischemic heart disease, OGTT = oral glucose tolerance test.
Y-CH and C-YP contributed equally to this study.
The authors have no conflicts of interest to disclose.
References
- [1].Sniderman AD, Williams K, Contois JH, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes 2011;4:337–45. [DOI] [PubMed] [Google Scholar]
- [2].Kastelein JJ, van der Steeg WA, Holme I, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation 2008;117:3002–9. [DOI] [PubMed] [Google Scholar]
- [3].McQueen MJ, Hawken S, Wang X, et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet 2008;372:224–33. [DOI] [PubMed] [Google Scholar]
- [4].Hwang YC, Ahn HY, Lee WJ, et al. An equation to estimate the concentration of serum apolipoprotein B. PLoS One 2012;7:e51607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cho NH, Jang HC, Choi SH, et al. Abnormal liver function test predicts type 2 diabetes: a community-based prospective study. Diabetes Care 2007;30:2566–8. [DOI] [PubMed] [Google Scholar]
- [6].Cho NH, Chan JC, Jang HC, et al. Cigarette smoking is an independent risk factor for type 2 diabetes: a four-year community-based prospective study. Clin Endocrinol 2009;71:679–85. [DOI] [PubMed] [Google Scholar]
- [7].Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr 2008;87:1455–63. [DOI] [PubMed] [Google Scholar]
- [8].Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9. [DOI] [PubMed] [Google Scholar]
- [9].The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–97. [DOI] [PubMed] [Google Scholar]
- [10].National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421. [PubMed] [Google Scholar]
- [11].Sniderman AD. Apolipoprotein B versus non-high-density lipoprotein cholesterol: and the winner is. Circulation 2005;112:3366–7. [DOI] [PubMed] [Google Scholar]
- [12].Ramjee V, Sperling LS, Jacobson TA. Non-high-density lipoprotein cholesterol versus apolipoprotein B in cardiovascular risk stratification: do the math. J Am Coll Cardiol 2011;58:457–63. [DOI] [PubMed] [Google Scholar]
- [13].Di Angelantonio E, Sarwar N, Perry P, et al. Emerging Risk Factors Collaboration. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009;302:1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Okamura T, Kokubo Y, Watanabe M, et al. Low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol and the incidence of cardiovascular disease in an urban Japanese cohort study: the Suita study. Atherosclerosis 2009;203:587–92. [DOI] [PubMed] [Google Scholar]
- [15].Imano H, Noda H, Kitamura A, et al. Low-density lipoprotein cholesterol and risk of coronary heart disease among Japanese men and women: the Circulatory Risk in Communities Study (CIRCS). Prev Med 2011;52:381–6. [DOI] [PubMed] [Google Scholar]
- [16].Barzi F, Patel A, Woodward M, et al. A comparison of lipid variables as predictors of cardiovascular disease in the Asia Pacific region. Ann Epidemiol 2005;15:405–13. [DOI] [PubMed] [Google Scholar]


