Abstract
The present study was to analyze clinical outcome of Pauwels grade-3 femoral neck fractures treated by different surgical techniques. Potential risk factors associated with nonunion and osteonecrosis of the femoral head (ONFH) were investigated as well. The retrospective study comprised of 67 sequential patients treated between January 2008 and December 2011. Patients with Pauwels grade-3 femoral neck fractures were treated by operative reduction and internal fixation. Cannulated screws (CS) were used in 46 patients, dynamic hip screw plus CS (DHS+CS) in 14, and locking compression plate (LCP) for proximal femur in 7. Reduction quality was assessed according to Haidukewych criteria. Postoperative radiographic examinations were conducted to observe fracture healing. Fracture displacement, comminution, fashion of internal fixation, and the sliding effect were analyzed, regarding the incidence of nonunion and ONFH. All patients had a follow-up of 21.6 ± 6.0 months on average. The phenomenon of sliding effect was observed in 16 cases (23.9%). In terms of reduction quality, 64 cases were graded as excellent, 2 were good, and 1 was poor. ONFH was presented in 15 cases (22.4%) and nonunion was found in 8 (11.9%), with 1 patient had ONFH and nonunion concomitantly. Profound hip contour was preserved in 45 cases (67.2%). The fashion of internal fixation yielded different results regarding ONFH and nonunion, whereas the effects of fracture displacement, comminution, and the sliding effect were not significant. ONFH and nonunion were common complications following Pauwels grade-3 femoral neck fractures. Higher incidence of ONFH in DHS+CS and of nonunion in the LCP group should be noted.
Keywords: classification, femoral neck fractures, nonunion, osteonecrosis of the femoral head, Pauwels
1. Introduction
Femoral neck fracture is defined as a damage in the continuity of the femoral neck, which typically presents groin pain, shortening and external rotation of the involved lower limb.[1] The incidence is 63.3 per million in women and 27.7 per million in men in the United States.[2] Although multiple protocols of fracture care have been proposed, preservation of autologous hip via surgical intervention of internal fixation is the treatment of mainstream.[3–5] Osteonecrosis of the femoral head (ONFH), also known as avascular necrosis, is the final presentation due to insulting of the blood supply, and nonunion is failure of the fracture healing following the primary care within 6 months. ONFH and nonunion are 2 main complications, especially in young adults.[6,7]
The Pauwels’ classification of femoral neck fracture was introduced in 1935. The Pauwels classification categories femoral neck fractures into 3 grades according to the fracture angle, namely, the angle <30° as Pauwels grade 1, the angle between 30° and 50° as Pauwels grade 2, and the angle >50° as Pauwels grade 3 (Fig. 1).[8] Another method to category femoral neck fracture is Garden classification, which has 4 grades based on fracture displacement. Different from the Garden method with the greatest popularity, Pauwels’ classification is mainly based on morphological fracture line and does not consider other factors such as the displacement of fractured fragments. As a result, it is not used as widely as Garden's classification method. However, in the aspect of the biomechanics of fracture healing, Pauwels’ classification is of great value.[9,10] In Pauwels grade-1 femoral neck fracture, compression is predominant. However, in Pauwels grade 3, the shearing force dominates the microenvironment and is associated with a significant varus force, which usually results in fracture displacement and varus collapse. Given the implants cannot overcome the shearing until fracture healing, nonunion and implant failure is inevitable. The shearing force also harms the restoration of blood supply to the femoral head, yielding higher incidence of osteonecrosis of the femoral head (ONFH).
Figure 1.
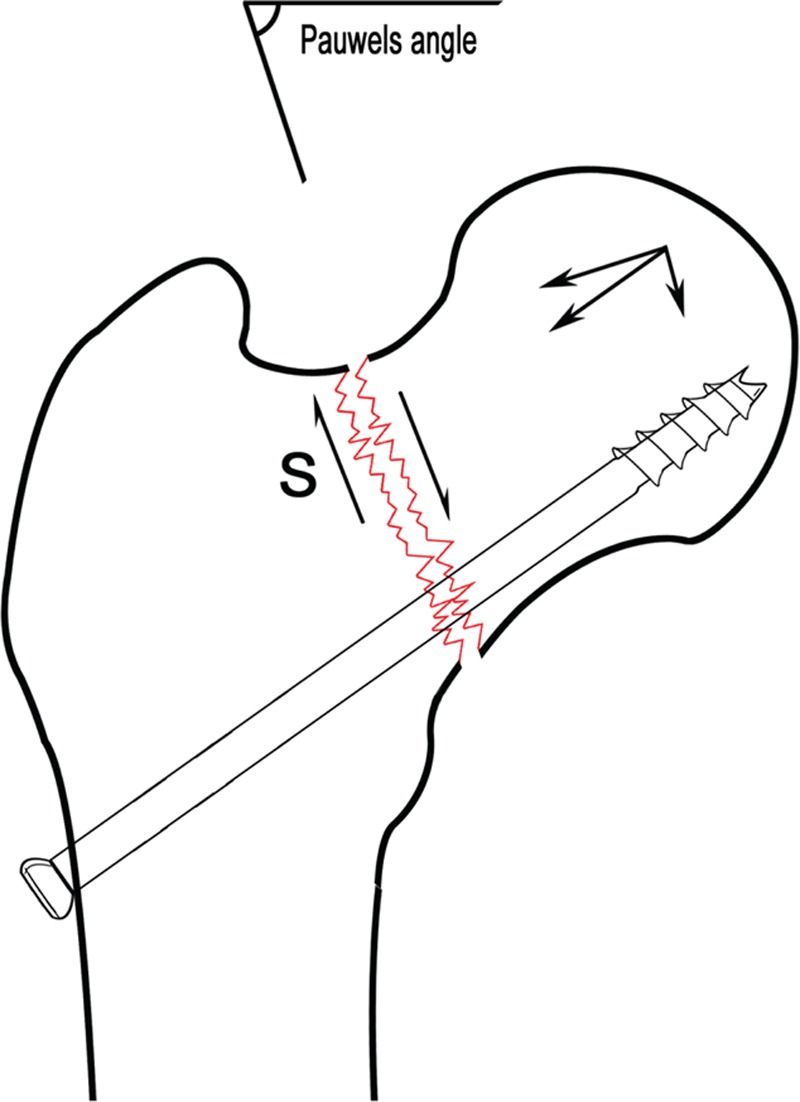
Schematic diagram of Pauwels angle. When the angle of the integrated projection of fracture line and horizontal line is >50°, the force between the fracture fragments mainly consists of shearing force (S), which is unfavorable to fracture healing.
Pauwels grade-3 femoral neck fracture is not common. There is still a lack of the gold standard concerning fracture care and fixation methods. Few studies reported the assessment of treatment and fewer literatures investigated the associated risk factors affecting the outcome. Therefore, we were encouraged to make a retrospective study of a series of patients, to evaluate the outcome and analyze associated underlying risk factors. We hypothesized that ONFH and nonunion were more frequently presented in Pauwels grade-3 femoral neck fractures.
2. Methods
Between January 2008 and December 2011, 67 cases of Pauwels grade-3 femoral neck fractures were surgically treated at Shanghai Jiao Tong University Affiliated Sixth People's Hospital. Pauwels angle could be measured based on the anterior-posterior (AP) view when there was no significant displacement and comminution. However, in the circumstance of obvious displacement or comminution, the fracture line was difficult to be recognized. In the scenario, the measurement of Pauwels angle should depend on the 3-dimensional computed tomography (3D-CT) or the AP radiogram after satisfactory reduction. Our inclusion criteria were as follows: trans-cervical femoral neck fractures; the injury-to-surgery interval (ISI) <3 weeks; normal structure with no history of hip joint diseases. Exclusion criteria included femoral neck fracture in children, basal and subcapital fractures, delayed femoral neck fractures, history of hip joint disease, and pathological fractures. The present study was approved by the ethics committee of Shanghai Sixth People's Hospital.
Closed reduction was attempted in all patients under general anesthesia on fracture table. Routine radiographic examinations following closed reduction, including AP and lateral views of the hip joint, were used to determine reduction quality, which was evaluated by Haidukewych criteria. Given the displacement is <2 mm and angulation in any planes is <5°, the reduction is graded as excellent. If the displacement is 2 to 5 mm and angulation in any planes is 5 to 10°, the reduction is graded as good. If the displacement is 5 to 10 mm and angulation in any planes is 10 to 20°, the reduction is graded as fair. If the displacement is >10 mm and angulation in any planes is >20°, the reduction is graded as poor.[11] Sixty-six cases in our study were closed reduced, and only 1 case underwent open reduction due to unsatisfactory closed reduction. According to the criteria, 64 cases were graded as excellent, 2 as good, and 1 as fair.
After successful reduction, an incision was made from the lateral side of hip based on the fashion of internal fixation. Cannulated screws (CS, 7.3 mm, Depuy) were used in 46 patients, dynamic hip screw plus CS (DHS+CS, Depuy) was used in 14 and locking compression plate (LCP, Yinzi) for proximal femur was used in 7. For Pauwels grade-3 femoral neck fracture with comminution, if there were critical separated bone fragment unreduced, we chose DHS+CS or LCP as implants. Otherwise, CS was the first choice. Cannulated screws could be arranged as either regular triangle or inverted triangle style. CS should be about 5 mm close to the subchondral bone. When stabilized with DHS+CS, the CS should parallel to the slide screw. Tip apex distance (TAD) altogether in the AP view and lateral view should be <20 mm. The direction of the screws was not necessarily parallel when fixed with LCP. Generally, 3 to 4 screws were adequate to fix the proximal fragments (Fig. 2).
Figure 2.
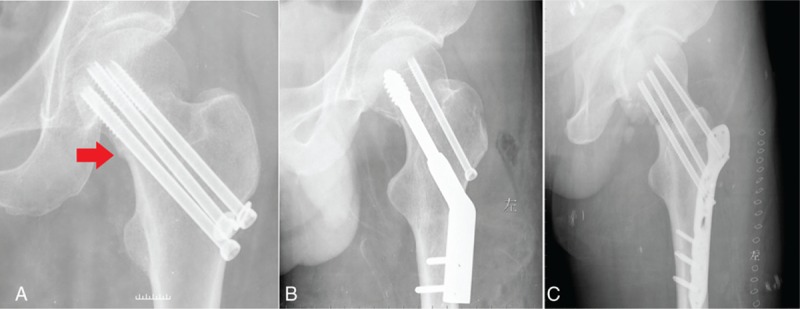
Three types of internal fixation for Pauwels grade-3 femoral neck fractures. (A) Parallel cannulated screws (CS). The step, which was caused by the sliding effect during screwing, was arrowed. (B) Dynamic hip screw plus cannulated screws (DHS+CS). (C) Locking compression plate (LCP) for proximal femur. CS = cannulated screws; DHS = dynamic hip screw; LCP = locking compression plate.
It should be noted that pulling force during screwing was not perpendicular to the fracture line, as showed in Fig. 1. Therefore, the shearing force paralleling to the fracture line might lead to minor (<2 mm) to moderate (2–5 mm) loss of reduction, although an anatomical reduction was achieved previously. We named the phenomenon “sliding effect” (Fig. 1). Indeed, multiple guide pins could prevent the sliding effect. However, in the scenario of osteoporosis and considerable comminution, the sliding effect could overwhelm the prevention effect. The step, as showed in Fig. 2A, could be observed by intraoperative imaging.
Postoperatively, low-molecular-weight heparin was used to prevent deep vein thrombosis. Postoperative analgesia was also initiated to facilitate functional exercise. Lower extremity muscle strength and range of motion of the hip joint could get started from the first day postoperatively. Weight bearing was not permitted within 8 to 12 weeks, to prevent adverse effects of shearing force.
AP and lateral imaging of the involved hip joint were taken 1, 6, 12 months postoperatively to assess fracture healing. For suspicious cases of nonunion, 3D-CT of the hip was helpful for differentiation. Nonunion was considered when fracture healing was not achieved within 6 months. ONFH and its stage were determined based on Ficat–Arlet criteria.[12] The presence of uneven density, narrowed hip joint space, and deformed head indicated different stages of ONFH. In the scenario of CS or DHS+CS fashion, fracture healing was primary, and there was no obvious callus. The continuity of trabecular formation, hip pain disappearance, and sound walking ability indicated fracture healing. Comminuted fracture healed in the way of secondary healing. There was callus formation, and it could be easily identified on plain radiogram.
All numerical data were described as mean ± standard deviation. Crosstabs were tested using Fisher's exact test or Pearson Chi-square test (with continuity correction). When P value was <0.05, it was considered statistically different. Data input and statistical analysis were done with IBM SPSS 20.0.
3. Results
There were 49 males and 18 females, with an average age of 47.7 ± 13.1 years (range, 17–75 years), of which 48 cases were associated with left side and 19 with right side. In terms of Garden classification, 10 cases were Garden II with no obvious displacement, whereas 57 patients were Garden III/IV. Comminution was found in 27 cases, in the posterior-inferior or anterior-inferior of the femoral neck, whereas the other 40 cases were relatively intact. The average ISI was 2.3 ± 0.8 days (range, 1–4 days). Sixty-six patients had closed reduction, and only 1 fracture was reduced via Smith–Peterson approach. The patients got an average follow-up of 21.6 ± 6.0 months (range, 12–36 months).
3.1. Nonunion and ONFH
ONFH was presented in 15 cases (22.4%) and nonunion was found in 8 (11.9%), including 1 patient with ONFH and nonunion concomitantly. The other 45 cases acquired sound fracture healing and profound hip contour (67.2%).
According to Garden's classification, of the 15 cases with ONFH, 14 cases belonged to the Garden III/IV group, whereas 1 case was Garden II. All 8 cases of nonunion were from Garden III/IV. In terms of comminution of the fracture site, 7 cases of ONFH had comminution and the other 8 cases are intact. Two cases of nonunion had comminuted fractures and the other 6 cases had intact. In terms of fixation, 8 cases of ONFH were stabilized with CS, 7 with DHS+CS. Five cases of nonunion were stabilized with CS, 3 with LCP (Fig. 3). There were no ONFH in the LCP group and no nonunion in the DHS+CS group.
Figure 3.
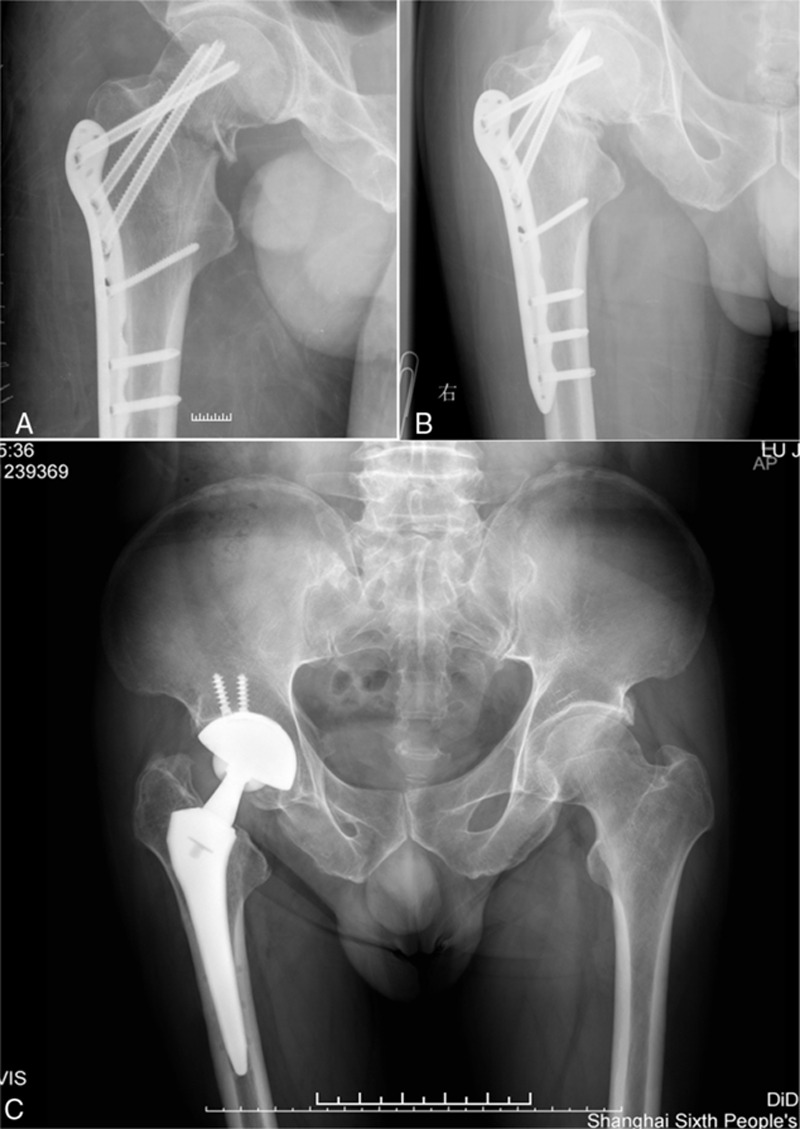
Nonunion in a patient with Pauwels grade-3 femoral neck fractures. (A) Proximal femoral LCP was used for the Pauwels grade-3 and comminuted femoral neck fracture. Anatomical reduction and rigid fixation was achieved. (B) Nonunion developed 9 months later, with shortening of the neck and sclerosis of the fracture site. (C) Total hip arthroplasty was performed on finally to solve the nonunion. LCP = locking compression plate.
3.2. Potential risk factors
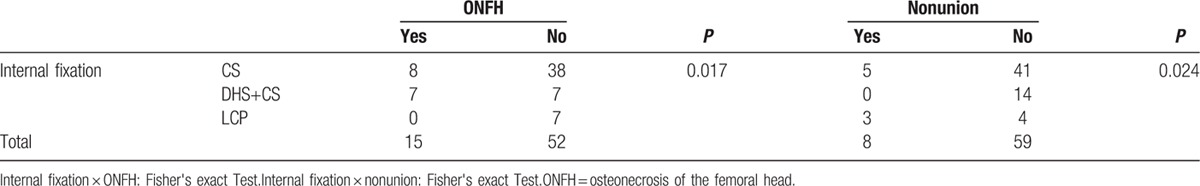
Fracture displacement, which was evaluated by Garden methods, did not show a significant effect on ONFH (P = 0.543) and nonunion (P = 0.463) between types I/II and III/IV fractures (Table 1). In terms of fracture comminution, it seemed that comminuted femoral neck fracture did not affect the occurrence of ONFH and nonunion (Table 2). However, it was revealed that the fashion of internal fixation might yield statistical differences among 3 treatment groups. Half of patients in the DHS+CS group had ONFH, whereas no ONFH in the LCP group (P = 0.017). In contrast, nonunion developed in 3 of 7 patients treated by LCP, whereas none was found when treated by DHS+CS (P = 0.024) (Table 3).
Table 1.
The relationship between Garden classification and ONFH, nonunion of femoral neck fractures.
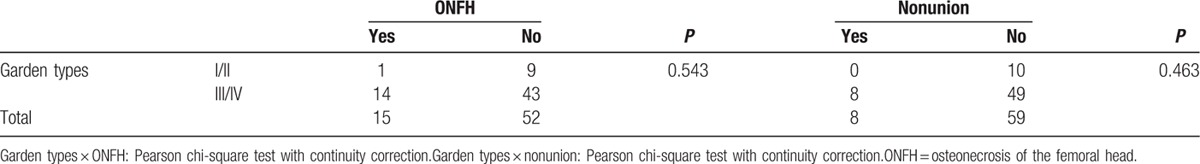
Table 2.
The relationship between fracture comminution and ONFH, nonunion of femoral neck fractures.
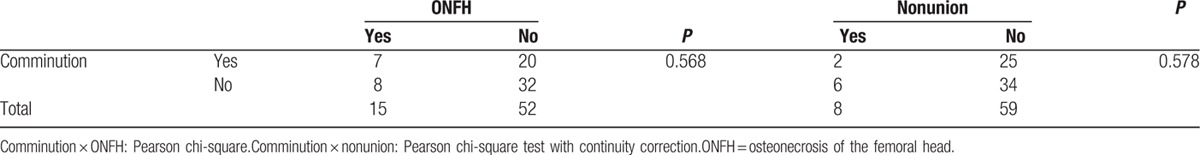
Table 3.
The relationship between fashion of internal fixation and ONFH, nonunion of femoral neck fractures.
3.3. Sliding effect
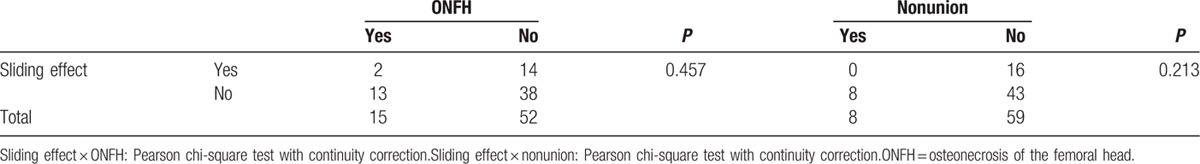
We named the loss of reduction during the screwing sliding effect, due to biomechanical property of Pauwels grade-3 fractures. The phenomenon of sliding effect was observed in 16 cases (23.9%). In terms of ONFH, 2 patients having sliding effect had ONFH finally, whereas 14 patients having a sliding effect did not (P = 0.457). For nonunion, 16 patients having a sliding effect did not have nonunion, whereas 8 patients without a sliding effect had nonunion (P = 0.213). The sliding effect did not affect ONFH and healing of femoral neck fractures (Table 4).
Table 4.
The relationship between sliding effect and ONFH, nonunion.
4. Discussion
Although femoral neck fractures are more frequently seen in the elderly, worse clinical outcomes are gained in the young due to the nature of high-energy induction.[13,14] Both ONFH and nonunion are notorious complications, although great endeavor has been made in past decades, the prognosis of femoral neck fractures in the young is not improved fundamentally.
Shearing force is unfavorable for fracture healing. Most investigators focused on delayed union or nonunion of Pauwels grade-3 femoral neck fracture. Liporace and colleagues surgically treated 76 cases of Pauwels grade-3 femoral neck fractures during 1993 to 2005. Sixty-one patients (62 fractures) conformed to follow-up until fracture healing or revision operation. The average follow-up was 24 months. Thirty-seven fractures were stabilized by CS, 25 by fixed-angle devices (DHS, antegrade intramedullary nail, DCS). The reduction quality was good to excellent in 95% of the cases (59/62). Three cases got poor reduction. Of the 59 well-reduced fractures, the nonunion rate was 14%, whereas 2 of the 3 poor reduced fractures developed nonunion. As to the devices, the nonunion rate was 19% in CS and 8% in fixed-angle devices. ONFH developed in 11% cases.[15] Although the rate of implant failure is lower in fixed-angle devices, there was no statistical significance for the limitation of patient number. Therefore, the optimal fashion of internal fixation for Pauwels grade-3 femoral neck fracture was still undetermined. Interestingly, proximal femur osteotomy could be applied to transform Pauwels grade-3 femoral neck fracture to Pauwels grade-2 or grade-1. Consequently, the shearing stress could also turn into compressive force, which is favorable to fracture healing.[16,17]
Rupprecht compared biomechanical property of Pauwels grade-3 femoral neck fractures stabilized by Intertan, CS, and DHS.[18] Although it was unable to restore the mechanical strength of the proximal femur by any kind of the devices, Intertan had some kind of mechanical advantage over CS and DHS. In our opinion, it was of little significance to compare the mechanical strength of the devices in vitro. First of all, any device will fail if the fracture developed delayed union or nonunion, even with the most powerful mechanical strength. Second, it is still of great doubt whether greater mechanical strength yields better fracture healing. Additionally, the biological environment should be taken into consideration, which is as important as mechanics to fracture healing.
The optimal surgical method and ideal implant for Pauwels grade-3 femoral neck fracture is still inconclusive.[19–23] Pauwels grade-3 femoral neck fracture treatment should be based on the individual characteristics of patient and fracture feature. Factors including fracture displacement, comminution, invasion of operation, meanwhile, surgeon's experience should also be taken into consideration. In the present study, we used CS, DHS+CS, and LCP as implants. CS fixation is quite easy and minimally invasive. CS with partial screw thread can provide compressive force for the fracture fragments, resulting in primary healing with absolute stability. However, some critical points should be noted in Pauwels grade-3 fractures. First, weight bearing should be delayed. Early weight bearing will produce tremendous stress, leading to implant failure, nonunion and varus deformity. Second, inclusion criteria should be subcapital and trans-cervical fractures. For basal femoral neck fractures with comminution or osteoporosis, CS fixation is not appropriate, especially in Pauwels grade-3 femoral neck fracture. Additionally, spatial distribution of CS in the neck is rather important. Currently, inverted triangle fixation is widely accepted. The bottom of the screw should be close to the calcar femorale. Actually, compressive force produced by screws is not perpendicular to the fracture line when treating Pauwels grade-3 femoral neck fracture with CS. As shown in Fig. 1, the compression is the component of pulling force produced by screwing. However, the other component is parallel to the fracture line, known as shearing stress, which can yield the sliding effect. This effect is the most important factor causing intra-operative loss of reduction. Multiple screws fixation can resist this effect; however, powerful force generated by the screw close to the calcar femorale can lead to cut off between counter screws and the bone, decreasing the fixation strength, especially in the circumstance of osteoporosis and comminution. It can resist rotation as well as the slippery slope effect when stabilizing Pauwels grade-3 femoral neck fracture by DHS, together with 1 CS. DHS+CS is also one kind of convenient fixation method. For the femoral neck fracture close to the base, DHS+CS can provide sufficient fixation strength. We used LCP for proximal femur in a few cases for its large invasiveness and high cost. However, the characteristic of multiangle fixation can provide stable mechanic environment for fracture healing after perfect reduction, especially in the scenario of comminuted cases. In this case, fixation with CS can cause loss of reduction, varus deformity. There should be <4 screws across the fracture line in order to prevent deteriorating blood supply of the femoral head.
Reciprocal cooperation of mechanical and biological environment is critical to fracture healing, especially for femoral neck fracture. Even with the strongest devices, it will eventually go failure without progressing healing. In our series of patients, time to weight bearing is quite conservative. Delayed full weight bearing can reduce the impact of shearing stress and benefit callus formation, provided good reduction and strong fixation. However, orthopedic surgeons are incapable to improve the biological environment of femoral neck fracture. Above all, satisfactory reduction and sophisticated fixation remain the predominant issues in the care of femoral neck fractures. Although nonunion is the significant complication of Pauwels grade-3 femoral neck fracture, ONFH also attracts great attention.[24–26]
Due to the rarity of Pauwels grade-3 femoral neck fracture, we collected a limited number of patients. We found no statistical significance regarding fracture displacement, comminution, and the sliding effect within 3 treatment groups. More cases should be collected via a multicentric study to further demonstrate the competition. The patients in our study got an average follow-up of 21.6 months. It is necessary to extend follow-up time to observe the outcome in a longer duration. It should be noted that injury-to-surgery interval within 3 weeks is a debatable factor associated with the final outcome.[27–29] The average ISI in the present study was 2.3 days (range, 1–4 days), which was not considered as the variant thereafter. Furthermore, the reduction quality is the recognized determinant for incidences of ONFH and nonunion.[30] In the present study, 65 fractures were graded as excellent following closed/open reduction according to Haidukewych criteria, and the other 2 were good. Therefore, the reduction quality was also not taken into statistical consideration.
In conclusion, ONFH and nonunion are common complications in Pauwels type-3 femoral neck fractures. CS, DHS+CS, as well as LCP can be used as fixation methods; however, special attention should be paid on higher incidence of ONFH in DHS+CS and of nonunion in the LCP group.
Footnotes
Abbreviations: 3D-CT = three-dimensional computed tomography, AP = anteroposterior, CS = cannulated screw, DHS = dynamic hip screw, ISI = injury-to-surgery interval, LCP = locking compression plate, ONFH = osteonecrosis of the femoral head, TAD = tip apex distance.
Funding: this work was supported by a fund from SMC-Chenxing Plan for Young Investigators at Shanghai Jiao Tong University. The funder has no role in the study design and manuscript preparation.
The authors report no conflicts of interest.
References
- [1].Zuckerman JD. Hip fracture. N Eng J Med 1996;334:1519–25. [DOI] [PubMed] [Google Scholar]
- [2].Kannus P, Parkkari J, Sievänen H, et al. Epidemiology of hip fractures. Bone 1996;18:57S–63S. [DOI] [PubMed] [Google Scholar]
- [3].Ye Y, Hao J, Mauffrey C, et al. Optimizing stability in femoral neck fracture fixation. Orthopedics 2015;38:625–30. [DOI] [PubMed] [Google Scholar]
- [4].Samsami S, Saberi S, Sadighi S, et al. Comparison of three fixation methods for femoral neck fracture in young adults: experimental and numerical investigations. J Med Biol Eng 2015;35:566–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wang C, Xu GJ, Han Z, et al. Correlation between residual displacement and osteonecrosis of the femoral head following cannulated screw fixation of femoral neck fractures. Medicine 2015;94:e2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Davidovitch RI, Jordan CJ, Egol KA, et al. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma 2010;68:236–42. [DOI] [PubMed] [Google Scholar]
- [7].Gurusamy K, Parker MJ, Rowlands TK. The complications of displaced intracapsular fractures of the hip: the effect of screw positioning and angulation on fracture healing. J Bone Joint Surg Br 2005;87:632–4. [DOI] [PubMed] [Google Scholar]
- [8].Bartoníček J. Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma 2001;15:358–60. [DOI] [PubMed] [Google Scholar]
- [9].Collinge CA, Mir H, Reddix R. Fracture morphology of high shear angle “vertical” femoral neck fractures in young adult patients. J Orthop Trauma 2014;28:270–5. [DOI] [PubMed] [Google Scholar]
- [10].Luttrell K, Beltran M, Collinge C. Preoperative decision-making in the treatment of high-angle “vertical” femoral neck fractures in young adult patient. J Orthop Trauma 2014;28:e221–5. [DOI] [PubMed] [Google Scholar]
- [11].Haidukewych GJ, Rothwell WS, Jacofsky DJ, et al. Femoral neck fractures in patients between the ages of fifteen and fifty years. J Bone Joint Surg Am 2004;86:1711–6. [DOI] [PubMed] [Google Scholar]
- [12].Steinberg ME, Steinberg DR. Classification systems for osteonecrosis: an overview. Orthop Clin N Am 2004;35:273–83. [DOI] [PubMed] [Google Scholar]
- [13].Wang SH, Yang JJ, Shen HC, et al. Using a modified Pauwels method to predict the outcome of femoral neck fracture in relatively young patients. Injury 2015;46:1969–74. [DOI] [PubMed] [Google Scholar]
- [14].Slobogean GP, Sprague SA, Scott T, et al. Management of young femoral neck fractures: is there a consensus? Injury 2015;46:435–40. [DOI] [PubMed] [Google Scholar]
- [15].Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am 2008;90:1654–9. [DOI] [PubMed] [Google Scholar]
- [16].Eid A. Valgus osteotomy for delayed presentation of femoral neck fractures Pauwels grade III. J Orthop Trauma 2010;24:115–9. [DOI] [PubMed] [Google Scholar]
- [17].Said GZ, Farouk O, Said H. Valgus intertrochanteric osteotomy with single-angled 130° plate fixation for fractures and non-unions of the femoral neck. Int Orthop 2010;34:1291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rupprecht M, Grossterlinden L, Ruecker AH, et al. A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: the Intertan versus cannulated screws or a dynamic hip screw. J Trauma 2011;71:625–34. [DOI] [PubMed] [Google Scholar]
- [19].Kunapuli SC, Schramski MJ, Lee AS, et al. Biomechanical analysis of augmented plate fixation for the treatment of vertical shear femoral neck fractures. J Orthop Trauma 2015;29:144–50. [DOI] [PubMed] [Google Scholar]
- [20].Su EP, Su SL. Femoral neck fractures: a changing paradigm. Bone Joint J 2014;96-B:43–7. [DOI] [PubMed] [Google Scholar]
- [21].Heetveld MJ, Raaymakers EL, Luitse JS, et al. Rating of internal fixation and clinical outcome in displaced femoral neck fractures. A prospective multicenter study. Clin Orthop Relat Res 2006;454:207–13. [DOI] [PubMed] [Google Scholar]
- [22].Probe R, Ward RW. Internal fixation of femoral neck fractures. J Am Acad Orthop Surg 2006;14:565–71. [DOI] [PubMed] [Google Scholar]
- [23].Bhandari M, Tornetta P, III, Hanson B, et al. Optimal internal fixation for femoral neck fractures: multiple screws of sliding hip screws? J Orthop Trauma 2009;23:403–7. [DOI] [PubMed] [Google Scholar]
- [24].Lu-Yao GL, Keller RB, Littenberg B, et al. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am 2009;76:15–25. [DOI] [PubMed] [Google Scholar]
- [25].Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res 2007;458:175–9. [DOI] [PubMed] [Google Scholar]
- [26].Ly TV, Swiontkowski MF. Treatment of femoral neck fractures in young adults. J Bone Joint Surg Am 2008;90:2254–66. [PubMed] [Google Scholar]
- [27].Papakostidis C, Panagiotopoulos A, Piccioli A, et al. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury 2015;46:459–66. [DOI] [PubMed] [Google Scholar]
- [28].Samuel AM, Russo GS, Lukasiewicz ML, et al. Surgical treatment of femoral neck fractures after 24 hours in patients between the ages of 18 and 49 is associated with poor inpatient outcome: an analysis of 1361 patients in the National Trauma Data Bank. J Orthop Trauma 2016;30:89–94. [DOI] [PubMed] [Google Scholar]
- [29].Gao YS, Ai ZS, Zhu ZH, et al. Injury-to-surgery interval does not affect postfracture osteonecrosis of the femoral head in young adults: a systematic review. Eur J Orthop Surg Traumatol 2013;23:203–9. [DOI] [PubMed] [Google Scholar]
- [30].Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral neck fractures: current management. J Orthop Trauma 2015;29:121–9. [DOI] [PubMed] [Google Scholar]


