Abstract
The purpose of this study was to determine the effect of pregnancy on adnexal torsion (AT). We conducted a matched case-control study using the Korean Health Insurance Review and Assessment Service–National Inpatients Sample (HIRA-NIS) from 2009 to 2011. AT patients were defined as women with both a diagnostic code (N835) and a surgical code for AT. The AT patients were randomly matched 1:4 with women without AT by age and year of claim. In total, 545 AT cases and 2180 controls were enrolled from a total of 1,843,451 women. After adjustment for such covariates as age, pregnancy was found to be associated with a lower rate of AT (adjusted odds ratio 0.314, 95% confidence interval [CI] 0.237–0.416, P value <0.01) and ovarian hyperstimulation syndrome was associated with a higher rate of AT (adjusted odds ratio 20.091, 95% CI 3.607–111.908, P value <0.01). We found that pregnancy is a negative risk factor for AT. However, a further study is needed to elucidate the mechanisms underlying these results.
Keywords: adnexal torsion, incidence, ovarian cyst torsion, pregnancy
1. Introduction
Adnexal torsion (AT) is the fifth most common gynecologic surgical emergency. It accounts for 2.7% of such surgeries.[1] The incidence of AT among women of reproductive age was 9.9 per 100,000 women.[2] AT occurs when the ovary and the fallopian tube twist, resulting in the strangulation of the blood supply. After several hours of AT, the ovary can become necrotic.[1,3] Although there are several diagnostic tools for AT, the definitive diagnostic method is direct confirmation using laparoscopy.[3,4] The management of AT is emergency laparoscopy to uncoil the twisted ovary and tube.[3,5,6]
Pregnancy might be a risk factor of AT.[3,5] According to previous studies, 13.7% of patients with AT were pregnant.[7] The common causes of AT during pregnancy appear to be corpus luteum cysts or ovarian hyperstimulation syndrome (OHSS) associated with assisted reproductive technologies (ART).[8] Corpus luteum cysts are the most common cause of adnexal masses during pregnancy.[9] OHSS, which occurs in 16% of pregnant patients treated with ART, may increase the incidence of AT.[10] The risk of developing a corpus luteum cyst or OHSS declines steeply in the second trimester of pregnancy.[9–11] As a reflection of this, AT occurs more frequently in the first and early second trimesters than in the third trimester.[12,13]
However, the studies associated with these results were not large case-control studies; rather, they were case reports from several institutions.[5,7,9] In addition, few studies have directly compared either a pregnant group to a nonpregnant group.[12] Therefore, these studies cannot confirm the effect of pregnancy on the development of AT.
Using national registry data, we performed a matched case-control study to determine the effect of pregnancy on AT.
2. Materials and methods
The Korean National Health Insurance Service is a compulsory, single-payer social insurance system that covers almost the entire population (∼49 million people per year) living in the country.[14] For our matched case-control study, we analyzed the 2009 to 2011 claims data from the Korean Health Insurance Review and Assessment Service–National Inpatients Sample (HIRA-NIS), which is maintained by the Health Insurance Review and Assessment Service (HIRA; serial number: HIRA-NIS-2009-0066, 2010-0084, 2011-0063). HIRA-NIS was samples that used a probabilistic sample extraction method (sampling rate: 13% of the inpatients population, 1% of the outpatients population), stratified sampling (sex, age).[15] HIRA-NIS had been regularly updated each year. A detailed description of these data are provided in our previous study.[15,16]
AT patients were defined as women who had both a Korean Standard Classification of Diseases-5 (KCD-5), which had been revised from the International Statistical Classification of Diseases and Related Health Problems, diagnostic code N83.5 and a surgical code for AT (an integral variable of the HIRA-NIS). AT cases were determined according to individual episodes rather than the number of diagnosed patients. The cases were randomly matched 1:4 with patients without AT by age and year of claim (2009, 2010, 2011). Random sampling was performed using R statistical software (version 3.0.3; Vienna, Austria). Pregnancy was determined based on the diagnostic code for antenatal care (Z34.0–Z35.9 according to KCD-5) between January 2009 and December 2011. Patients with a diagnostic code for antenatal care followed by the diagnostic code for spontaneous abortion (O00-O08 according to KCD-5) were excluded. Pregnant patients with adnexal torsion were defined as those who had an adnexal torsion code and a surgical code on different days within 60 days of their antenatal care code. If the same patient underwent surgery for AT twice with an interval of 60 days or more, the surgeries were defined as separate episodes. We investigated whether a woman had ovarian hyperstimulation syndrome (OHSS) based on the presence of the diagnostic code for OHSS (N98.1 according to KCD-5) within 30 days prior to the occurrence of AT.
This study was approved by the Institutional Review Board of MizMedi Hospital. The personal information of all individuals was protected by using anonymized patient identification numbers. According to the Institutional Review Board guidelines, informed consent from all patients was not required because of anonymized patient identification numbers. HIRA was not related to the results of this study.
All statistical analyses, including analyses of the matching data, were performed using R statistical software (version 3.0.3; Vienna, Austria). A P value <0.05 was considered statistically significant. All statistical analyses were performed using 2-tailed tests. The chi-square test was used to compare differences between groups. After adjustments for age and OHSS, a logistic multivariate analysis was performed to determine the effects of pregnancy on AT. We used the mean imputation method for missing values.
3. Results
3.1. Selection of subjects
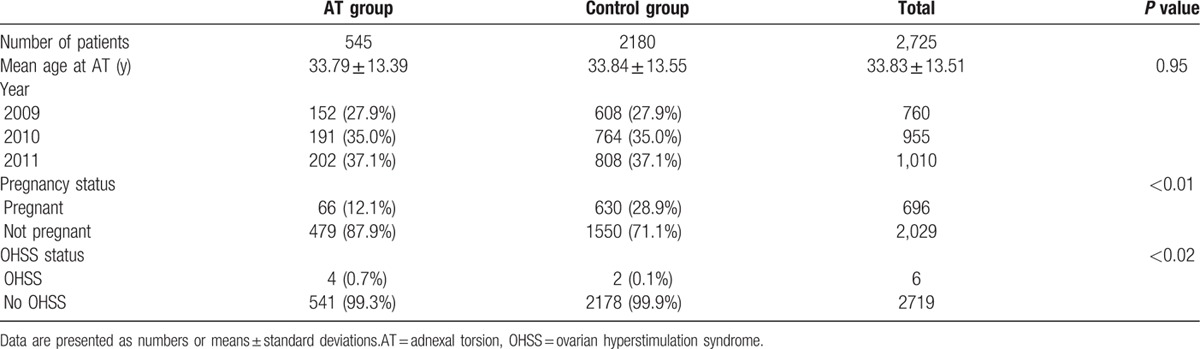
We selected a sample of 1,843,451 women from the HIRA-NIS database of ∼3 million individuals in 2009 to 2011. Among the sampled women, there were 545 cases of AT; 2180 controls were matched to these cases by age and sampling weights, with a match ratio of 1:4. A flowchart in Fig. 1 presents the process of patients’ inclusion. There was no recurrent adnexal torsion episode in AT cases. Demographic characteristics for cases and controls are presented as Table 1. The mean age was 33.79 ± 13.39 for cases and 33.84 ± 13.55 for controls.
Figure 1.
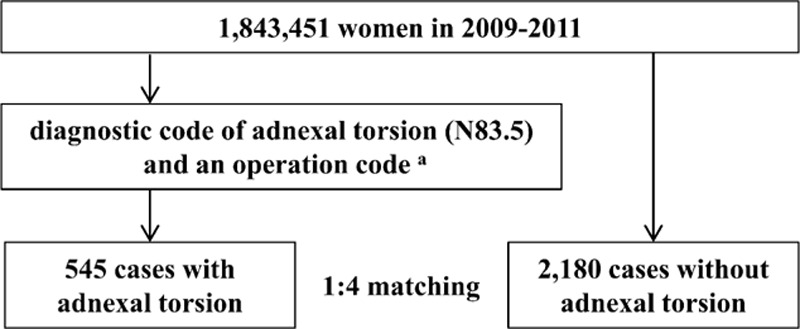
Flowchart about the selection procedure from the HIRA sample 2009 to 2011.
Table 1.
Characteristics of patients with adnexal torsion and the control group.
3.2. Univariate regression analysis
Pregnancy was associated with a lower rate of AT (odds ratio [OR] 0.339, 95% confidence interval [CI]; 0.258–0.446, P value <0.01). OHSS was associated with a higher rate of AT (OR 8.052, 95% CI; 1.469–44.121, P value 0.02) (Table 2).
Table 2.
Multivariate analysis of pregnancy and OHSS status with adnexal torsion.
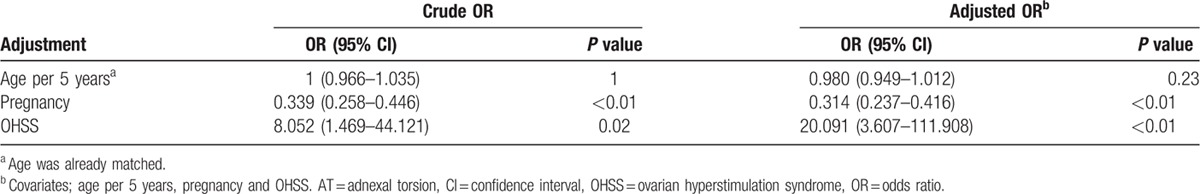
3.3. Multivariate regression analysis
After adjustment for age and OHSS, pregnancy was associated with a lower rate of AT (OR 0.314, 95% CI; 0.237–0.416, P value <0.01). After adjustment for covariates, OHSS was associated with a higher rate of AT (OR 20.091, 95% CI; 3.607–111.908, P value <0.01) (Table 2).
4. Discussion
According to previous studies, pregnancy is a known risk factor for AT.[3,5] The effect of pregnancy on AT may be related to the presence of a corpus luteum cyst or to ART.[9–11] Although it is impossible to determine whether these factors cause AT in pregnancy, the recurrence rate of AT is 2-fold higher in pregnant patients compared with nonpregnant patients.[12]
However, the result of the present study differs from conventional belief. This study revealed that pregnant patients had a lower incidence of AT compared with nonpregnant patients. This difference in findings can be explained by the fact that previous studies were case series rather than cross-sectional or case-control studies.[5,7,9,12] Therefore, in previous studies, it is impossible to confirm an association between AT and pregnancy.
The reason for the association between lower rates of AT and pregnancy cannot be determined precisely. Nonetheless, it may be explained by bias caused by preconception examinations. As described above, corpus luteum cysts and OHSS are risk factors for AT.[8–10] Transvaginal ultrasound is a basic assessment tool used in preconception and infertility work-ups.[17,18] In South Korea, in particular, the cost of a single obstetric ultrasound examination is low, from 10 to 120 U.S. dollars.[19] Therefore, the accessibility of ultrasonography is relatively high in South Korea. If a disease such as ovarian tumor is found during the work-up, attempts to become pregnant can be delayed until the disease has been treated. The treatment of ovarian tumors before attempting pregnancy decreases the risk of a corpus luteum cyst or OHSS.
In our study, the prevalence of AT was higher among patients with OHSS, but the precise reason for this result could not be determined. Considering previous studies, it is likely that ovarian masses are affected by OHSS.[20] However, the results of several studies of the relationship between AT and OHSS have been inconsistent. According to 1 study, the AT rate was 11-fold higher among patients undergoing ART.[20] In particular, the occurrence of AT during pregnancy after ART was higher than the occurrence during nonpregnancy after ART.[10] Conversely, another study showed that ART had no effect on AT.[21] Our result showed that OHSS may be a risk factor for AT. However, this analysis should be carefully analyzed reaching statistical significance because OHSS cases based on a total of only 6 cases.
There are several limitations to our study. First, it is impossible to confirm a causal relationship because of preconception bias. Therefore, it would be an error to interpret our result as indicating that pregnancy reduces the incidence of AT. Second, this study was based on the use of diagnostic codes, and errors related to code input are possible. To overcome this limitation, we confirmed an AT diagnosis if a case had both a surgical and a diagnostic code for AT. Third, this study did not analyze AT by trimester of pregnancy. Therefore, it is impossible to know whether trimester affects the incidence of AT.
In conclusion, we found that the incidence of AT was lower during pregnancy compared with nonpregnancy. However, a further study is needed to identify and elucidate the causal relationship between AT and pregnancy.
Footnotes
Abbreviations: ART = assisted reproductive technologies, AT = adnexal torsion, CI = confidence interval, HIRA-NIS = The Korean Health Insurance Review and Assessment Service–National Inpatients Sample, KCD-5 = Korean Standard Classification of Diseases-5, OHSS = ovarian hyperstimulation syndrome, OR = odds ratio.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Hibbard LT. Adnexal torsion. Am J Obstet Gynecol 1985;152:456–61. [DOI] [PubMed] [Google Scholar]
- [2].Yuk J-S, Kim LY, Shin J-Y, et al. A national population-based study of the incidence of adnexal torsion in the Republic of Korea. Int J Gynaecol Obstet 2015;129:169–70. [DOI] [PubMed] [Google Scholar]
- [3].Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol 2006;49:459–63. [DOI] [PubMed] [Google Scholar]
- [4].Huchon C, Panel P, Kayem G, et al. Does this woman have adnexal torsion? Hum Reprod 2012;27:2359–64. [DOI] [PubMed] [Google Scholar]
- [5].Krissi H, Shalev J, Bar-Hava I, et al. Fallopian tube torsion: laparoscopic evaluation and treatment of a rare gynecological entity. J Am Board Fam Med 2001;14:274–7. [PubMed] [Google Scholar]
- [6].Chapron C, Capella-Allouc S, Dubuisson JB. Treatment of adnexal torsion using operative laparoscopy. Hum Reprod 1996;11:998–1003. [DOI] [PubMed] [Google Scholar]
- [7].Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med 2001;38:156–9. [DOI] [PubMed] [Google Scholar]
- [8].Hasiakos D, Papakonstantinou K, Kontoravdis A, et al. Adnexal torsion during pregnancy: report of four cases and review of the literature. J Obstet Gynaecol Res 2008;34(4 pt 2):683–7. [DOI] [PubMed] [Google Scholar]
- [9].Kumari I, Kaur S, Mohan H, et al. Adnexal masses in pregnancy: a 5-year review. Aust N Z J Obstet Gynaecol 2006;46:52–4. [DOI] [PubMed] [Google Scholar]
- [10].Mashiach S, Bider D, Moran O, et al. Adnexal torsion of hyperstimulated ovaries in pregnancies after gonadotropin therapy. Fertil Steril 1990;53:76–80. [DOI] [PubMed] [Google Scholar]
- [11].Zanetta G, Mariani E, Lissoni A, et al. A prospective study of the role of ultrasound in the management of adnexal masses in pregnancy. BJOG 2003;110:578–83. [PubMed] [Google Scholar]
- [12].Hasson J, Tsafrir Z, Azem F, et al. Comparison of adnexal torsion between pregnant and nonpregnant women. Am J Obstet Gynecol 2010;202:536.e1–6. [DOI] [PubMed] [Google Scholar]
- [13].Chang S-D, Yen C-F, Lo L-M, et al. Surgical intervention for maternal ovarian torsion in pregnancy. Taiwan J Obstet Gynecol 2011;50:458–62. [DOI] [PubMed] [Google Scholar]
- [14].h-well NHIS. http://www.nhis.or.kr/static/html/wbd/g/a/wbdga0302.html Accessed May 29, 2016. [Google Scholar]
- [15].Kim L, Kim J-A, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health 2014;36:e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yuk J-S, Kim YJ, Hur J-Y, et al. Association between socioeconomic status and ectopic pregnancy rate in the Republic of Korea. Int J Gynaecol Obstet 2013. [DOI] [PubMed] [Google Scholar]
- [17].Roholamin S, Shahraki AD, Esteki M. When uterus sonography is needed in preconception consult? Adv Biomed Res 2013;2:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].ESHRE Capri Workshop Group. Diagnosis and management of the infertile couple: missing information. Hum Reprod Update 2004;10:295–307. [DOI] [PubMed] [Google Scholar]
- [19].Shin Hong K, Soonman K. A development of a cost accounting system for ultrasonography in a secondary hospital. Korean J Health Econ Policy 2007;13:137–61. [Google Scholar]
- [20].Gelbaya TA. Short and long-term risks to women who conceive through in vitro fertilization. Hum Fertil 2010;13:19–27. [DOI] [PubMed] [Google Scholar]
- [21].Yen C-F, Lin S-L, Murk W, et al. Risk analysis of torsion and malignancy for adnexal masses during pregnancy. Fertil Steril 2009;91:1895–902. [DOI] [PubMed] [Google Scholar]


