Abstract
Lower urinary tract symptoms (LUTS)/benign prostatic hyperplasia (BPH) is common in adult men and can impair erectile function (EF). It was believed surgical treatments for this illness can improve EF due to the relief of LUTS while they were also reported harmed EF as heating or injury effect. Current network meta-analysis aimed to elucidate this discrepancy.
Randomized controlled trials (RCTs) were identified. Direct comparisons were conducted by STATA and network meta-analysis was conducted by Generate Mixed Treatment Comparison. Random-effects models were used to calculate pooled standard mean difference and 95% confidence intervals and to incorporate variation between studies.
Eighteen RCTs with 2433 participants were analyzed. Nine approaches were studied as transurethral resection of the prostate (TURP), plasmakinetic resection of the prostate (PKRP), plasmakinetic enucleation of the prostate (PKEP), Holmium laser enucleation of the prostate (HoLEP), Holmium laser resection of the prostate (HoLRP), photoselective vaporization of the prostate (PVP), Thulium laser, open prostatectomy (OP), and laparoscopic simple prostatectomy (LSP). In direct comparisons, all surgical treatments did not decrease postoperative International Index of Erectile Function (IIEF)-5 score except PVP. Moreover, patients who underwent HoLEP, PKEP, Thulium laser, and TURP had their postoperative EF significantly increased. Network analysis including direct and indirect comparisons ranked LSP at the highest position on the variation of postoperative IIEF-5 score, followed by PKRP, HoLEP, TURP, Thulium laser, PKEP, PVP, HoLRP, and OP. In subgroup analysis, only PVP was found lower postoperative EF in the short term and decreased baseline group, whereas TURP increased postoperative IIEF-5 score only for patients with normal baseline EF. However, HoLEP and PKEP showed pro-erectile effect even for patients with decreased baseline EF and short-term follow-up. Our novel data demonstrating surgical treatments for LUTS/BPH showed no negative impact on postoperative EF except PVP. Moreover, HoLEP and PKEP were found pro-erectile effect for all subgroups. New technologies, such as LSP, PKRP, and Thulium laser, were ranked at top positions in the network analysis, although they had no pro-erectile effect in direct comparison due to limited original studies or poor baseline EF. Therefore, further studies and longer follow-up are required to substantiate our findings.
Keywords: benign prostatic hyperplasia, erectile function, IIEF-5, lower urinary tract symptoms, prostate, surgical treatments
1. Introduction
Lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH) is one of the most common clinical complaints in adult men.[1] The prevalence of BPH is approximately 50% for men in their fifties and reaches to 80% for men over eighties,[2] and the incidence of LUTS is around 25% for men in their fifties or older.[3,4] Although LUTS/BPH is a benign disorder, it may affect physical health and have a significant impact on the quality of life (QoL).[5–7] Meanwhile, many men with LUTS/BPH have coexistent erectile dysfunction (ED),[8] suggesting that there might be a link between both conditions.[9,10] Indeed, in a cohort of men scheduled for the surgical management of LUTS/BPH, 36% with moderate LUTS/BPH and 94% with severe LUTS/BPH were found to have coexisting ED.[11] In recent decades, LUTS/BPH was regarded as an independent risk factor of ED in aging men.[12]
A lot of treatments for LUTS/BPH exist. Although oral therapies, used alone or combined, are effective, there are still as many as 30% patients requiring more invasive or surgical treatment options.[13] Surgical therapy is the optional treatment for patients with bothersome LUTS/BPH unwilling to try medical therapies, in cases where oral drugs were not effective, and in cases of complicated LUTS.[14] However, all accepted therapy regimens for LUTS/BPH can impact some aspects of sexual health,[15] leaving the prostate surgery a complicated problem on erectile function (EF). It is suggested that improvement of LUTS can also improve EF.[16] Indeed, EF was reported not to change in 84%, improve in 3% to 14%, and deteriorate in 0% to 16% after LUTS/BPH surgery.[16,17] Others assumed that operation technique or heating effect will damage corpus cavernosum nerve outside the prostate capsule and harm EF.[18]
There are a number of surgical approaches for LUTS/BPH in general, including transurethral resection of the prostate (TURP), transurethral incision of the prostate (TUIP), plasmakinetic resection of the prostate (PKRP, also known as bipolar-TURP), plasmakinetic enucleation of the prostate (PKEP), open prostatectomy (OP), laparoscopic simple prostatectomy (LSP), transurethral microwave therapy (TUMT), transurethral needle ablation (TUNA) of the prostate, Holmium laser enucleation (HoLEP), and Holmium laser resection (HoLRP) of the prostate, 532 nm (“Greenlight”) laser vaporization of the prostate, Diode laser vaporization of the prostate, Thulium laser, prostatic stents, intraprostatic ethanol injections, and intraprostatic botulinum toxin injections. Many systematic reviews have summarized the growing evidences supporting the use of these new techniques. However, most reviews and meta-analyses only paid attention to International Prostate Symptom Score (IPSS) scores, QoL, maximum flow rate, and operation time,[19–25] and few focused on their impact on EF.[26–28] One such meta-analysis assessed the effects of LUTS/BPH treatment on male EF; however, only binary variable was used and they just compared TURP with transurethral electrovaporization (TUEVP), Holmium laser treatment (HLT), and watchful waiting, which was thought insufficient.[26]
The aim of current study is to carry out a systematic review and network meta-analysis comparing the impact of different surgical treatments for LUTS/BPH on EF documented with International Index of Erectile Function-5 (IIEF-5) based on existing randomized controlled trials (RCTs) and ranking these regimens for practical consideration.
2. Materials and methods
2.1. Search strategy
We carried out a meta-analysis of RCTs that examined the impact of different LUTS/BPH surgical treatments on male EF. We systematically searched databases, including PUBMED (1966 to August 2015), EMBASE (1984 to August 2015), AMED (1985 to August 2015), CINAHL (1966 to August 2015).[29] The following key search terms were used: surgical treatment or transurethral resection of the prostate or TURP or plasmakinetic resection of the prostate or PKRP or bipolar-TURP or plasmakinetic enucleation of the prostate or PKEP or open prostatectomy or OP or laparoscopic simple prostatectomy or LSP or Holmium laser enucleation or HoLEP or Holmium laser resection or HoLRP or photoselective vaporization of the prostate or PVP or potassium-titanyl-phosphate or KTP or Thulium laser or transurethral incision of the prostate or TUIP or transurethral microwave therapy or TUMT or transurethral needle ablation or TUNA plus benign prostatic hyperplasia or benign prostatic enlargement plus erectile function or erectile dysfunction or international index of erectile function-5 or IIEF-5. In addition, we identified additional articles by manually searching the reference lists from other published review articles. The approval by an institutional review board was not required because this study was based on published studies.
2.2. Inclusion criteria
Two independent investigators (ZL, PC) conducted an initial screening of article titles and abstracts after removal of duplicate references. This process removed those articles that were clearly not relevant—such as letters, comments, reviews, ecological studies, animal studies, single case reports, and meta-analyses. Then, another 2 independent investigators (QM, HX) evaluated all potentially relevant articles based on full-text reviews using a structured flow chart and detailed guidelines to determine eligibility for inclusion. Any disagreements were settled by a third reviewer (ZL).
Studies were considered eligible if they met the following criteria: (1) the RCT must include 2 surgical treatments at least; (2) patients in RCTs must be diagnosed with LUTS/BPH and underwent surgical treatments; (3) the RCT must have postoperative IIEF-5 score; (4) IIEF-5 scores were recorded and the results were formed as patient number, mean ± standard deviation (SD); (5) sufficient data for analysis were provided; (6) full text could be accessed; (7) papers were published in English.
Studies were excluded if not met above inclusion criteria. Additionally, data were used only once if they were reported in other publications based on the same sample.
2.3. Quality assessment
The methodological quality of included studies was appraised with the Cochrane Collaboration bias appraisal tool.[30] In particular, the following factors were evaluated: (1) Adequate sequence generation? (2) Allocation concealment? (3) Binding? (4) Incomplete outcome data addressed? (5) Free of selective reporting? (6) Free of other bias?
Each question was answered with “yes,” “no,” or “unclear,” and 3 reviewers (ZL, PC, and QM) assessed each trial. In case of disagreement, judgment was made through open discussion.
2.4. Data extraction
Two authors (ZL and PC) independently performed the data extraction. The data extracted for the analysis included the following: (1) the first author's name and the publication year; (2) operation type; (3) the time of follow-up and the patient number, IIEF-5 scores, and SD at each time point. Disagreements were resolved by consensus with another author (QM).
2.5. Statistical analysis
The direct comparisons of preoperative IIEF-5 with postoperative one for each procedure were meta-analyzed with STATA version 12.0 (StataCorp LP, College Station, TX).[31,32] Results were expressed as standard mean difference (SMD) for continuous outcomes with 95% confidence intervals (CIs). A “random-effects” statistical model was used. Statistical significance was set at P < 0.05. Tests for heterogeneity would be carried out using the chi-squared test with significance being set at P < 0.1; I2 would be used to estimate the total variation across studies. Low-level, moderate-level, and high-level heterogeneity was considered <25%, 25% to 50%, and >50%, respectively.[33]
Comparative effects of different surgical treatments were network-analyzed with the automated software Generate Mixed Treatment Comparison (GeMTC).[34] We created a consistency model by combining the effect of indirect and direct comparisons based on Bayesian approach to get an absolute effect and cumulative probability, which was used to rank different surgical treatments. Results are expressed as rank probability.
Subgroup analysis was first performed by stratifying different time points after operations, and then set by normal and decreased baseline IIEF-5 score. In the subgroup analysis, we pooled the effect of these subgroups separately, but in the analysis of the overall effect of each surgical procedure, we incorporated the data of different time points into one verum arm.
3. Results
3.1. Characteristics of included studies
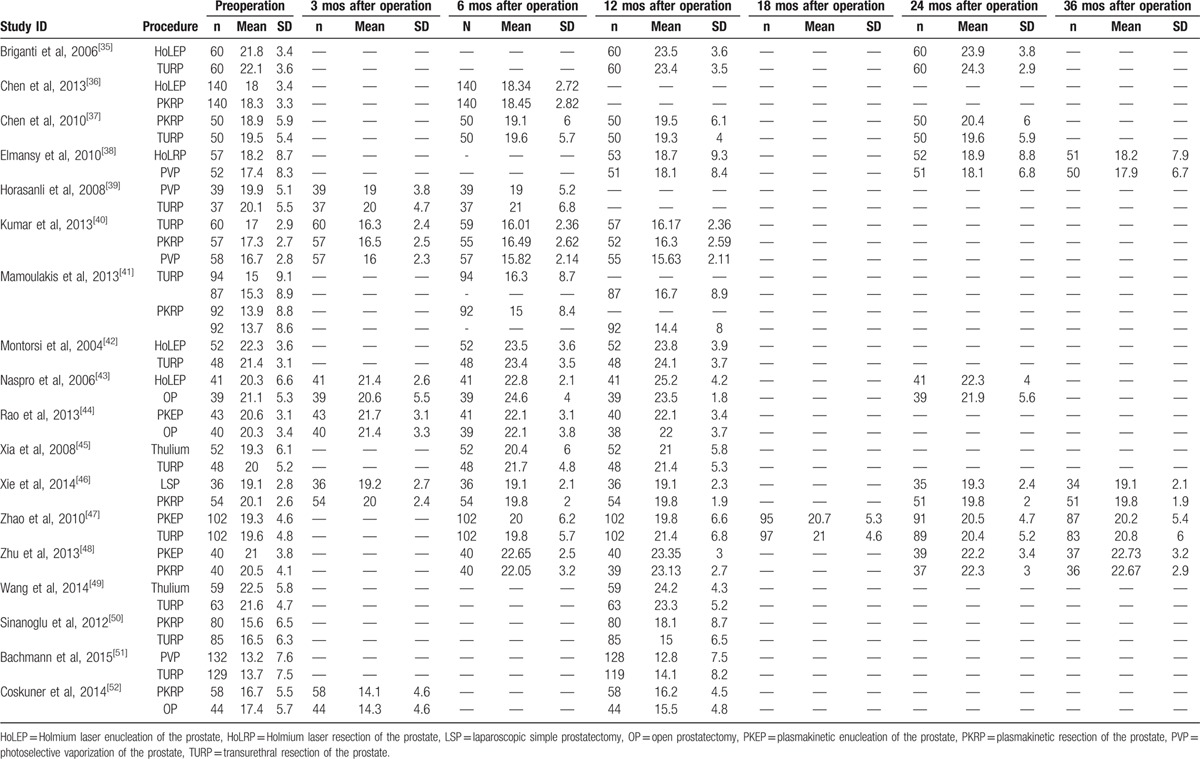
Using the database search strategy, a total of 813 records were retrieved from PubMed, Embase, AMED, and CINAHL. Eighteen RCTs with a total 2433 participants (mean age 67.53 years) finally met full inclusion criteria for current meta-analysis.[35–52]Figure 1 showed the flowchart of literature searches and Table 1 provided characteristics of the included trials. These studies were conducted in 7 different countries located in Europe, North America, and Asia. Current 9 kinds of surgical approaches, including TURP, PKRP, PKEP, LSP, HoLEP, HoLRP, PVP, Thulium laser, and OP, were covered in these trials. Surgical treatments such as TUIP, TUMT, and TUNA were not studied in the included RCTs and were excluded from the current review. Patients were followed up at 3, 6, 12, 18, 24, and 36 months. Table 2 provided detailed IIEF-5 scores before and after operation of each RCT with the mean pretreatment IIEF-5 score of 18.19, suggesting these patients suffered mild to severe erectile dysfunction (ED).
Figure 1.
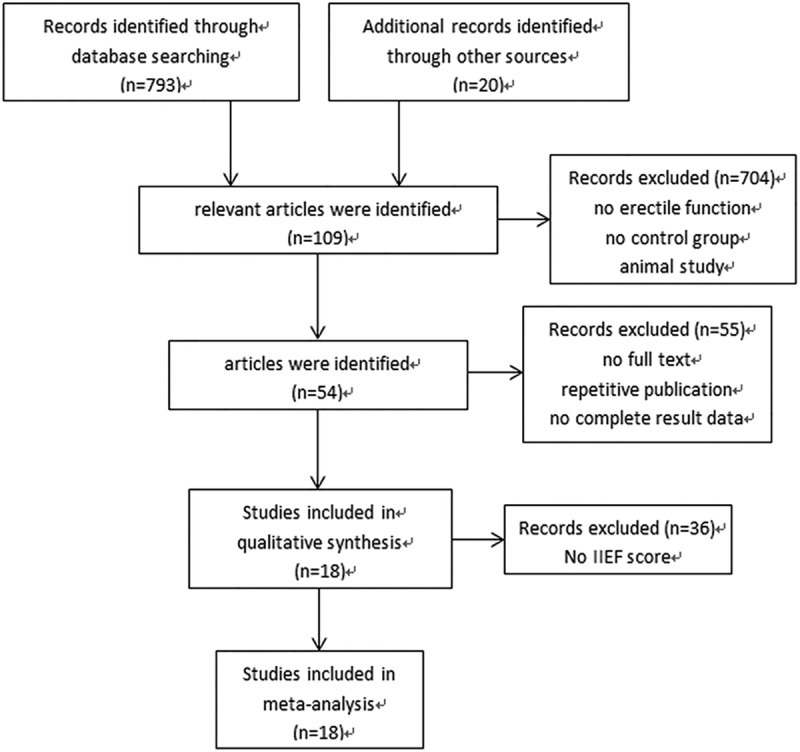
Flowchart of literature searches.
Table 1.
Characteristics of the included studies in meta-analysis.
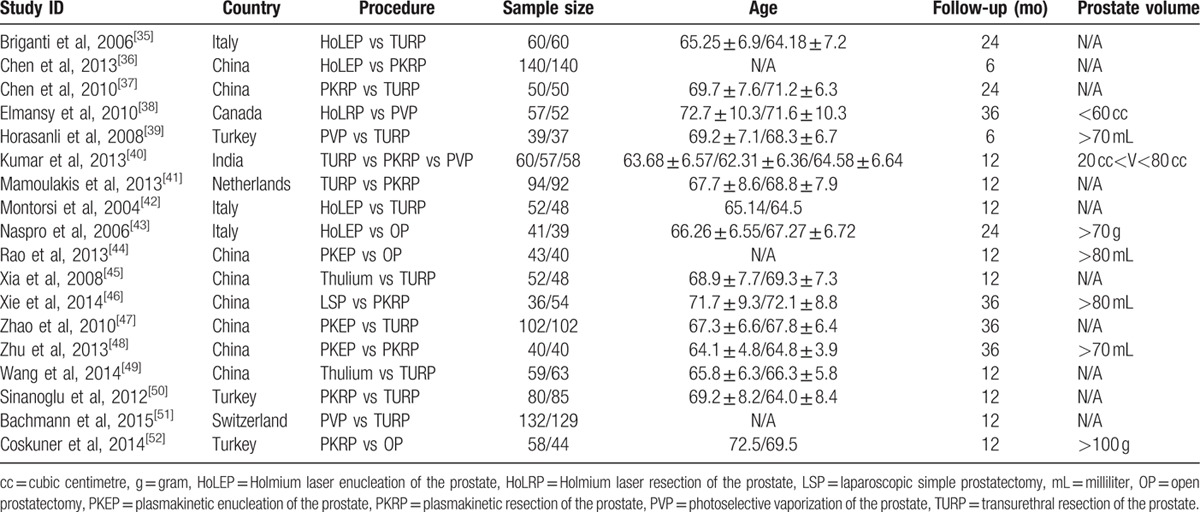
Table 2.
Detail data of each included RCT.
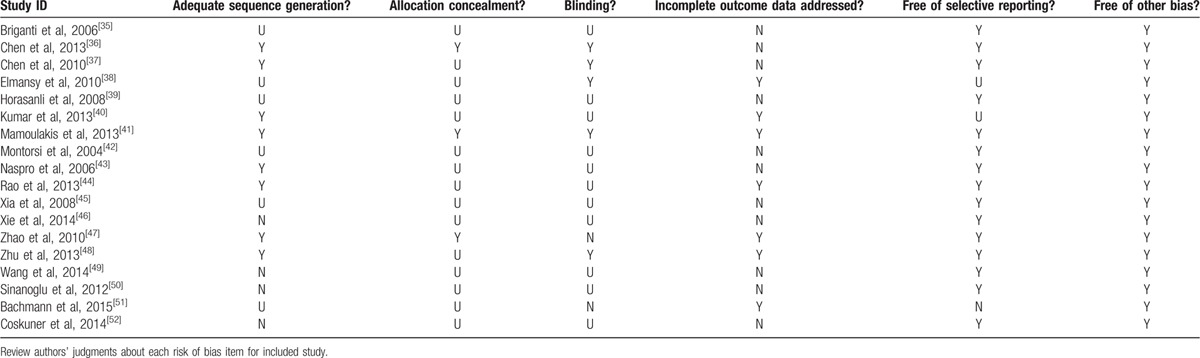
3.2. Risk of bias
As described in Table 3, 8 of 18 included studies had adequate randomization according to the Corchrane Collaboration bias appraisal tool. One study was randomized according to the odd and even hospital numbers. Three studies were retrospectively analyzed. The other 6 did not describe their randomization method. Only 3 studies showed methods of allocation concealment and the others did not describe their approaches. Blinding was reported in 5 studies, but blinding method was not described. Seven studies did not provided complete outcome data and one study did not report all design outcomes. All 18 studies were free of other bias.
Table 3.
Risk of bias summary.
3.3. Directly comparing post with pretreatment EF
There were 11 studies[35,37,39–42,45,47,49–51] including 24 direct comparisons of post-TURP IIEF-5 score with pre-TURP one. As shown in Fig. 2A, TURP significantly enhanced postoperative EF (P = 0.006, SMD = 0.15, 95% CI 0.04–0.26, I2 = 58.5%, P = 0.000). There were 8 studies[36,37,40,41,46,48,50,52] including 21 direct comparisons of post-PKRP IIEF-5 score with pretreatment one and there were 3 studies[44,47,48] including 12 direct comparisons for PKEP. As demonstrated in Fig. 2B, PKRP had no influence on EF (P = 0.545, SMD = 0.04, 95% CI −0.09 to 0.16, I2 = 59.9%, P = 0.000), whereas PKEP significantly increased postsurgery EF (P = 0.000, SMD = 0.29, 95% CI 0.19–0.39, I2 = 0.0%, P = 0.515). Laser technologies are widely used in prostate surgery. The present study covered HoLEP, HoLRP, PVP, and Thulium laser approaches, of which there were 4,[35,36,42,43] 1,[38] 4,[38–40,51] and 2[45,49] trials containing 9, 3, 9, and 3 direct post versus pretreatment comparisons, respectively. The pooled outcomes of all 4 kinds of laser technologies on EF were displayed in Fig. 2C, which suggested that HoLEP (P = 0.000, SMD = 0.40, 95% CI 0.24–0.56, I2 = 35.9%, P = 0.131) and Thulium laser (P = 0.016, SMD = 0.27, 95% CI 0.05–0.49, I2 = 0.0%, P = 0.851) had pro-erectile effect, whereas PVP (P = 0.045, SMD = −0.12, 95% CI −0.24 to −0.00, I2 = 0.0%, P = 0.458) deteriorated EF, and HoLRP (P = 0.682, SMD = 0.05, 95% CI −0.17 to 0.26, I2 = 0.0%, P = 0.956) showed no effect. The I2 for HoLEP indicated moderate-level heterogeneity and the I2 for HoLRP, PVP, and Thulium laser showed no heterogeneity. LSP mimics OP with less invasive. There were 3 studies[43,44,52] including 9 direct comparisons of post-OP IIEF-5 score with pre-OP one, and there was 1[46] study containing 5 direct comparisons for LSP. As shown in Fig. 2D, both OP (P = 0.220, SMD = 0.19, 95% CI −0.11 to 0.49, I2 = 76.3%, P = 0.000) and LSP (P = 0.831, SMD = 0.02, 95%CI −0.18 to 0.23, I2 = 0.0%, P = 0.999) had no impact on EF with high-level heterogeneity for OP and no heterogeneity for LSP. In general (Fig. 2A–D), all surgical approaches for LUTS/BPH except PVP did not decrease EF when directly comparing postoperative IIEF-5 score with preoperative one. Moreover, patients who underwent HoLEP, PKEP, Thulium laser, and TURP had their postoperative EF significantly increased.
Figure 2.
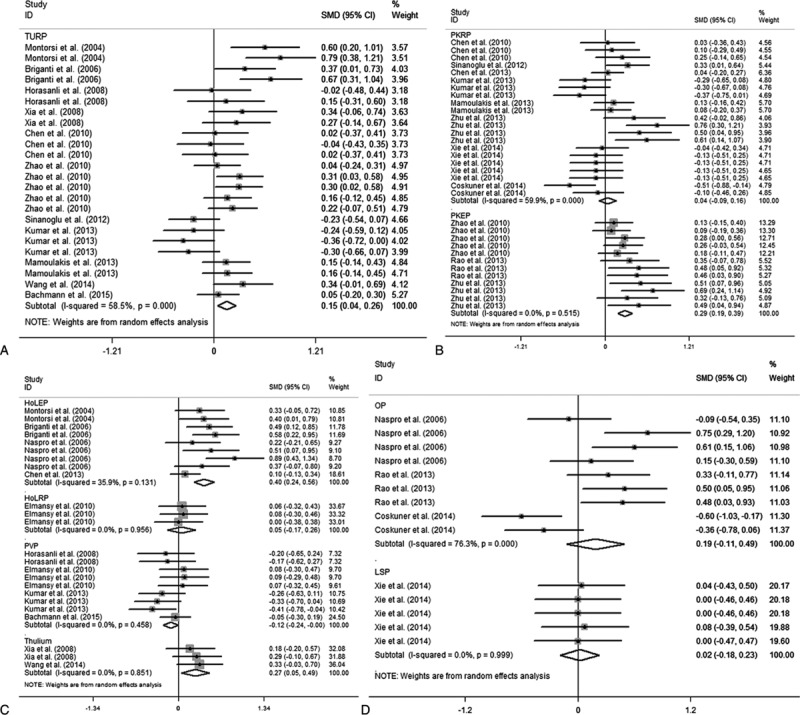
A, Forest plot for the association of post-TURP versus pre-TURP IIEF-5 score. The association was indicated as standard mean difference (SMD) estimate with the corresponding 95% confidence interval (CI). The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function.B, Forest plot for the association of postoperative versus preoperative erectile function of PKRP and PKEP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. C, Forest plot for the association of postoperative versus preoperative erectile function of HoLEP, HoLRP, PVP, and Thulium laser. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. D, Forest plot for the association of postoperative versus preoperative erectile function of open prostatectomy and LSP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. HoLEP = Holmium laser enucleation of the prostate, HoLRP = Holmium laser resection of the prostate, LSP = laparoscopic simple prostatectomy, OP = open prostatectomy, PKEP = plasmakinetic enucleation of the prostate, PKRP = plasmakinetic resection of the prostate, PVP = photoselective vaporization of the prostate, TURP = transurethral resection of the prostate.
3.4. Network comparison and analysis
Network analysis included direct and indirect comparisons (Fig. 3A). As shown in Fig. 3B, cumulative probability was used to rank all 9 surgical treatments. Among all treatments, LSP ranked highest on the variation of postoperative IIEF-5 score, followed by PKRP, HoLEP, TURP, Thulium laser, PKEP, PVP, HoLRP, and OP. The network outcomes of LSP, HoLRP, and Thulium laser should be identified uncertain as they only compared with other one treatment, or they were not enclosed in the comparative circle (Fig. 3A).
Figure 3.
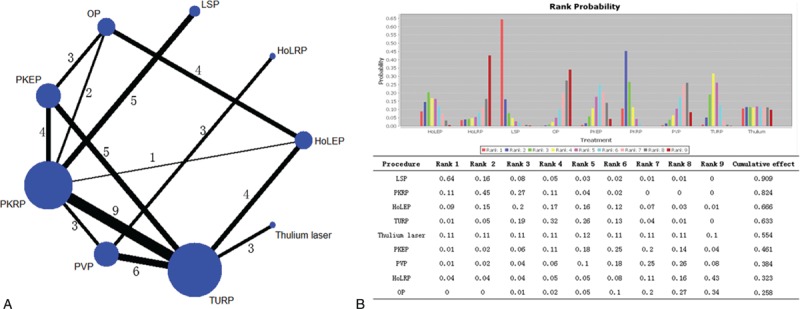
A, Comparison network of included studies. The size of each point estimates the number of each procedure. The font-weight of each line estimates the number of study which links 2 procedures. B, Rank probability of each procedure from network analysis. Rank 1 is the best result for a given outcome; rank 9 is the worst result for a given outcome. The size of the histogram bar is proportional to the probability of achieving that particular rank for the outcome. HoLEP = Holmium laser enucleation of the prostate; HoLRP = Holmium laser resection of the prostate, LSP = laparoscopic simple prostatectomy, OP = open prostatectomy, PKEP = plasmakinetic enucleation of the prostate, PKRP = plasmakinetic resection of the prostate, PVP = photoselective vaporization of the prostate, TURP = transurethral resection of the prostate.
3.5. Subgroup analysis
Short-term group was followed up at 3 and 6 months including 8 surgical approaches. Direct comparison and meta-analysis were carried out. As shown in Fig. 4A, patients who underwent PVP suffered a decreased postoperative EF (P = 0.014, SMD = −0.25, 95% CI −0.45 to −0.05, I2 = 0.0%, P = 0.949), whereas patients underwent HoLEP (P = 0.009, SMD = 0.22, 95% CI 0.06–0.39, I2 = 0.0%, P = 0.402) and PKEP (P = 0.002, SMD = 0.31, 95% CI 0.12–0.50, I2 = 4.2%, P = 0.372) had an increased postoperative IIEF-5 score. And these outcomes were reliable as suggested by the I2. Other 5 treatments showed no effect on EF. Long-term group was followed up at 12, 18, 24, and 36 months including 9 surgical approaches. Direct comparison and meta-analysis showed all aforementioned 9 kinds of surgical approaches for LUTS/BPH do not decrease EF when directly comparing postoperative IIEF-5 score with preoperative one (Fig. 4B and C). Moreover, patients who underwent HoLEP (P = 0.000, SMD = 0.53, 95% CI 0.35–0.71, I2 = 0.0%, P = 0.483), PKEP (P = 0.000, SMD = 0.28, 95% CI 0.16–0.40, I2 = 0.1%, P = 0.428), Thulium laser (P = 0.021, SMD = 0.31, 95% CI 0.05–0.58, I2 = 0.0%, P = 0.861), and TURP (P = 0.004, SMD = 0.20, 95% CI 0.06–0.33, I2 = 60.6%, P = 0.001) had an increased postoperative IIEF-5 score. Other 5 treatments showed no effect on EF.
Figure 4.
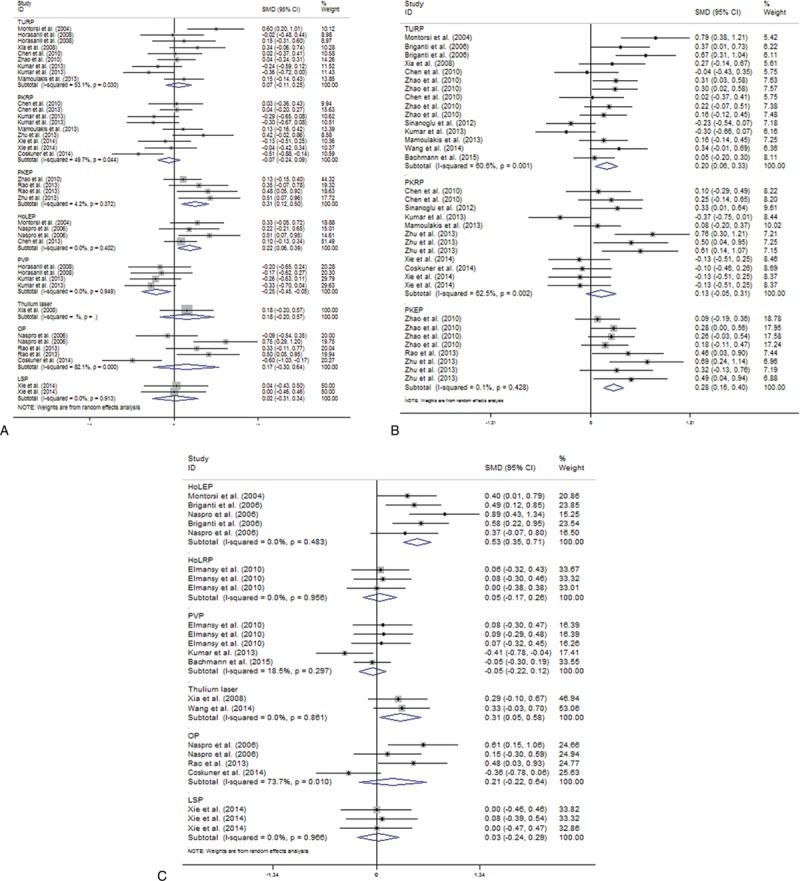
A, Forest plot of short-term subgroup analysis for the association of postoperative versus preoperative erectile function of 8 involved procedures. The association was indicated as standard mean difference (SMD) estimate with the corresponding 95% confidence interval (CI). The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. B, Forest plot of long-term subgroup analysis for the association of postoperative versus preoperative erectile function of TURP, PKRP, and PKEP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. C, Forest plot of long-term subgroup analysis for the association of postoperative versus preoperative erectile function of HoLEP, HoLRP, PVP, Thulium laser, OP, and LSP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. HoLEP = Holmium laser enucleation of the prostate, HoLRP = Holmium laser resection of the prostate, LSP = laparoscopic simple prostatectomy, OP = open prostatectomy, PKEP = plasmakinetic enucleation of the prostate, PKRP = plasmakinetic resection of the prostate, PVP = photoselective vaporization of the prostate, TURP = transurethral resection of the prostate.
Group of normal baseline IIEF-5 score included studies by Briganti et al,[35] Montorsi et al,[42] and Wang et al,[49] which had the IIEF-5 score over 21, suggesting free of preoperative ED. Direct comparison and meta-analysis of this group were carried out. As displayed in Fig. 5A, patients who underwent TURP (P = 0.000, SMD = 0.54, 95% CI 0.37–0.71, I2 = 2.3%, P = 0.393) and HoLEP (P = 0.000, SMD = 0.46, 95% CI 0.27–0.64, I2 = 0.0%, P = 0.813) had an increased postoperative IIEF-5 score, and the I2 suggested these outcomes are reliable. There was only 1 study of Thulium laser which could not be analyzed by meta-analysis. Other 6 treatments were not included in this group. Group of decreased baseline IIEF-5 score covered all 9 surgical approaches with 15 articles.[36–41,43–48,50–52] As shown in Fig. 5(B–E), patients who underwent TURP (P = 0.188, SMD = 0.06, 95% CI −0.03 to 0.15, I2 = 32.7%, P = 0.084), PKRP (P = 0.545, SMD = 0.04, 95% CI −0.09 to 0.16, I2 = 59.9%, P = 0.000), HoLRP (P = 0.682, SMD = 0.05, 95% CI −0.17 to 0.26, I2 = 0.0%, P = 0.956), Thulium laser (P = 0.093, SMD = 0.23, 95% CI −0.04 to 0.51, I2 = 0.0%, P = 0.709), OP (P = 0.220, SMD = 0.19, 95% CI −0.11 to 0.49, I2 = 76.3%, P = 0.000), and LSP (P = 0.831, SMD = 0.02, 95% CI −0.18 to 0.23, I2 = 0.0%, P = 0.999) had no effect on EF, whereas patients who underwent HoLEP (P = 0.006, SMD = 0.39, 95% CI 0.11–0.66, I2 = 60.6%, P = 0.038) and PKEP (P = 0.000, SMD = 0.29, 95% CI 0.19–0.39, I2 = 0.0%, P = 0.515) had an increased postoperative IIEF-5 score. Moreover, PVP (P = 0.045, SMD = −0.12, 95% CI −0.24 to −0.00, I2 = 0.0%, P = 0.458) had a negative effect.
Figure 5.
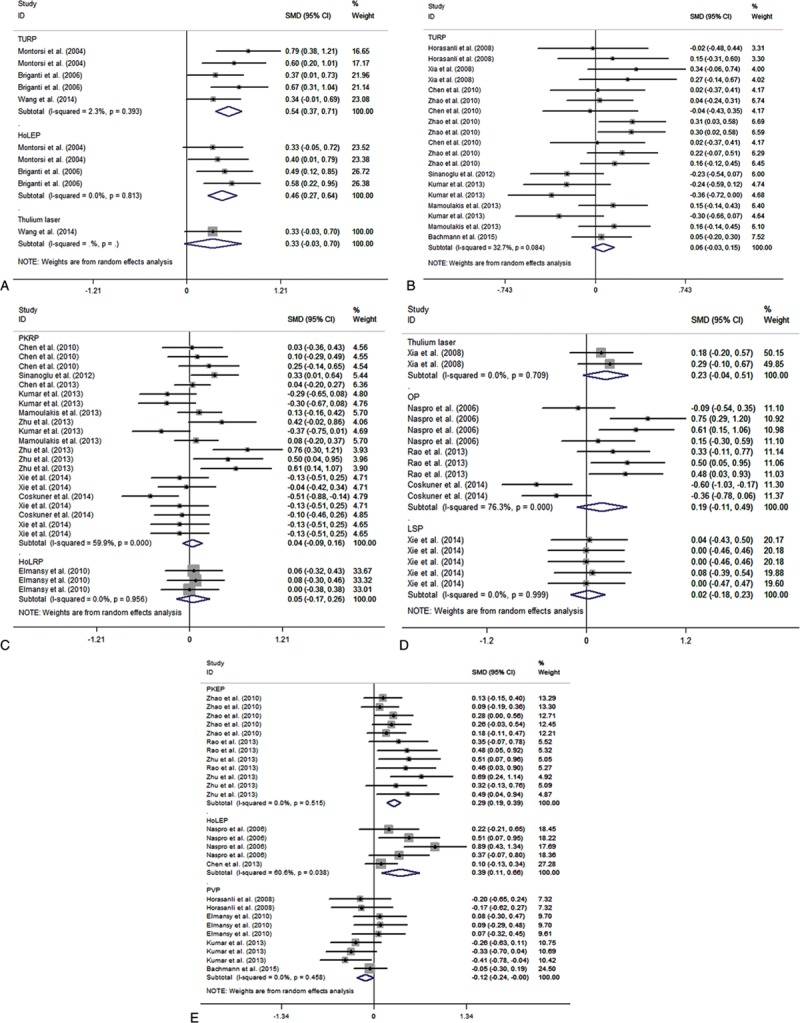
A, Forest plot of normal baseline IIEF-5 score for the association of postoperative versus preoperative erectile function of three involved procedures. The association was indicated as standard mean difference (SMD) estimate with the corresponding 95% confidence interval (CI). The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. B, Forest plot of decreased baseline IIEF-5 score for the association of postoperative versus preoperative erectile function of TURP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased risk of erectile function. C, Forest plot of decreased baseline IIEF-5 score for the association of postoperative versus preoperative erectile function of PKRP and HoLRP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. D, Forest plot of decreased baseline IIEF-5 score for the association of postoperative versus preoperative erectile function of Thulium laser, OP, and LSP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. E, Forest plot of decreased baseline IIEF-5 score for the association of postoperative versus preoperative erectile function of PKEP, HoLEP, and PVP. The association was indicated as SMD estimate with the corresponding 95% CI. The SMD estimate of each study is marked with a solid black square. The size of the square represents the weight that the corresponding study exerts in the meta-analysis. SMD less than 0 indicates decreased erectile function. HoLEP = Holmium laser enucleation of the prostate, LSP = laparoscopic simple prostatectomy, OP = open prostatectomy, PKEP = plasmakinetic enucleation of the prostate, PVP = photoselective vaporization of the prostate, TURP = transurethral resection of the prostate.
4. Discussion
Most men are likely to be faced with LUTS/BPH as early as in their fourth decade.[53] There are growing evidences that LUTS/BPH and ED are frequently co-associated.[9,10,54,55] Indeed, the mean IIEF-5 score of 2433 participants in the current review is less than 19, suggesting they had moderate to severe ED, which is consistent with the results reported by Miner et al[12]. Several common pathophysiological mechanisms have been proposed to underlie both LUTS/BPH and ED, including reduced nitric oxide (NO) and cyclic guanosine monophosphate (cGMP) signaling, increased Ras homolog gene family member A (RhoA)/Rho-associated protein kinase (ROCK) signaling, autonomic hyperactivity, and pelvic atherosclerosis.[9,54] Thus, it is not hard to understand that surgical treatments for BPH can improve LUTS, and also EF concomitantly.[15,54] However, surgery itself will harm EF due to erectile nerve and vascular injury along with psychological factors.[18] The injuries include operative procedure and heating effect of electrode and laser.[18] Some studies suggested that postoperative ED was associated with the integrity of prostate capsule[56] which is just crossed by the cavernous nerve.[56] Bleeding also helps to harm EF. If local blood loss reduced, the operator can have a better view and make less stanching and damage.[36]
Therefore, it is quite controversial for the influence of prostate surgery on EF. TURP is the golden standard procedure for LUTS/BPH. For 644 patients, Muntener et al[57] found that post-TURP EF was improved by 30%, whereas it deteriorated by 20%. OP is generally performed for large prostate. An Italian study reported the post-OP EF and orgasm of 60 men did not change significantly according to IIEF surveys.[58] PVP vaporizes obstructing prostatic tissue with high-energy laser and its effect on EF is still under investigation. Paick et al examined the IIEF score of 45 men before and after PVP treatment. EF improved by 3.4 to 30 points.[59] However, a French study suggested EF appeared to be maintained after PVP,[60] whereas Bruyere et al[61] indicated a significantly decreased EF after PVP. Kuntz et al[62] randomized 200 patients to HoLEP or TURP and observed similar change of EF after 1 year follow-up. Meng et al[63] showed HoLEP did not affect EF through a RCT of 108 patients.
Aforementioned studies are well-performed. But they only investigated 2 surgical treatments. Most of the trials compared the various minimally invasive surgical therapies for symptomatic BPH with the “golden standard”—TURP.[56,64] Meanwhile, validated questionnaires such as IIEF were not used in many of these studies, and few studies provided baseline EF, making compiling data difficult to evaluate the impact of each procedure on EF. Moreover, fewer systematic reviews and meta-analyses were carried out. One such meta-analysis by Zong et al[26] compared TURP with watchful waiting, TUEVP, and HLT. They showed that TURP had a less negative effect on male EF when compared with TUEVP, but did not differ from HLT. However, this review included inadequate surgical approaches and binary variable were used. Furthermore, no subgroup analysis was made. The present review is the first network meta-analysis that compares current 9 surgical treatments directly and indirectly with objective variable of IIEF-5 score.
With direct comparison, we found that all procedures except PVP did not decrease EF. Patients undergoing PKRP, HoLRP, LSP, and OP had their EF unchanged, whereas those undergoing TURP, PKEP, HoLEP, and Thulium laser treatment had increased postoperative IIEF-5 score. After PVP, EF was observed to reduce. The penetration depth of Thulium laser, Holmium laser, and 532 nm green light laser is 0.25, 0.4, and 0.8 mm, respectively.[65] Thus, there would be more damage to EF with PVP due to deeper penetration. Heating effect also contributes to harm EF. When vaporizing, damage of external tissue and vessel occurs with turning into steam and micro blasting. Indeed, patients undergoing TURP, PKEP, HoLEP, and Thulium laser treatment have their EF significantly improved. The basic procedure for HoLEP and PKEP is enucleation, which mimics open prostatectomy, mechanically removing adenoma of prostate within its capsule,[47] with less heating effect and damage to blood vessels when compared with resection. In addition, enucleation was shown to have less bleeding with sealing the root of blood vessel on the capsule and morcelling the enucleated adenoma in a relatively constant pressure environment.[36,47] As mentioned above, Thulium laser penetrates most superficially. But current review included only 2 studies. Thus, further studies will be required to substantiate its effect on EF. In the present meta-analysis, several studies investigated the influence of OP and LSP on EF, because OP and LSP have to incise the bladder neck (Freyer method) or the prostate capsule (Millin method), which may destroy the integrity of the prostate capsule, resulting in the injury of erectile nerves and vessels.[66] Resection with PKRP and HoLRP may result in more aforementioned heating damage. Therefore, the relief of LUTS/BPH with PKRP, HoLRP, LSP, and OP could counteract their negative effect on EF, which could finally keep the postoperative IIEF-5 score unchanged. Again, more RCTs and longer duration of follow-up are needed for these new technologies.
In our subgroup analysis, only post-PVP EF was decreased in the short-term group, whereas it no change was observed in the long-term follow-up. Also, post-TURP IIEF-5 score was found not to change in the short-term group, but increase in the long-term group. These suggest that harmed EF can be improved with time. Tscholl et al[67] had reported that some of patients can recover from postsurgery ED. Wasson et al[68] also showed that if there was neuropraxia, EF might be expected to improve continuously with time. Moreover, when followed up for no more than 12 months, PKEP and HoLEP still significantly increased EF, indicating both procedures per se resulted in least invasive influence on EF. Subgroups were further set according to baseline IIEF-5 score. In the present review, there were only 3 trials with normal baseline EF investigating 3 approaches, including TURP, HoLEP, and Thulium laser. The former 2 procedures had their postoperative IIEF-5 score significantly increased, and Thulium laser could not be analyzed as only 1 study was performed. Therefore, normal baseline IIEF-5 score is important for preserving or recovering postoperative EF as suggested by Althof et al.[69] For patients with decreased baseline IIEF-5 score, HoLEP and PKEP still can improve postoperative EF, whereas TURP, PKRP, HoLRP, Thulium laser, OP, and LSP showed no change of EF with post-PVP IIEF-5 even lowered. Therefore, it further and consistently demonstrated that enucleation is the least invasive procedure for EF, and PVP could not be considered as the most harmful treatment for EF.
Apart from direct comparison, we tried to rank all 9 surgical treatments with network analysis and found LSP ranked highest on the variation of postoperative IIEF-5 score, followed by PKRP, HoLEP, TURP, Thulium laser, PKEP, PVP, HoLRP, and OP. But the network outcomes of LSP, HoLRP, and Thulium laser should be identified as uncertain, because they were compared with only 1 treatment, or they were not enclosed in the comparative circle (Fig. 2E). It is interesting that PKRP is ranked the second, although bipolar resection showed no effect on EF in direct comparison, which could be attributed to decreased baseline IIEF-5 score. As the golden standard procedure, TURP was also highly ranked. Although the previous studies reported that the depth of electric current penetration in PK systems are 3 to 4-fold lower compared with PKRP,[50] TURP, instead of PKRP, significantly improved postoperative EF in general comparison and for patients with long-term follow-up or normal baseline IIEF-5 score. Preoperative EF could contribute to this discrepancy. Again, more studies are required to justify these new technologies, such as LSP and PKRP, which maybe truly less invasive on EF.
The overall quality of the included studies is acceptable. Only 1 study was randomized according to the odd and even hospital numbers. Three studies were retrospectively analyzed and judgment “no” for the assessment of adequate sequence generation was given to these trials. Most studies did not describe their allocation method in details and this might be a risk factor for the methodological quality. Also, most studies did not report their blinding quality. The trial design scheme of the included studies could be divided into 2 types. The first design had participants randomized to different surgical treatments and then EF was evaluated. The second design was a retrospective study with participants who had already undergone surgery. The different trial design schemes might be a source of the heterogeneity in the analysis of IIEF score. However, other outcome measures demonstrated good homogeneity.
Consistent with all meta-analyses, some caveats are pertinent. Publication bias could influence the results because negative trials are less likely to be published. Potential selection biases can influence the homogeneity of groups, and relatively small sample sizes can limit the statistical power to identify true associations.
5. Conclusions
Our novel data demonstrated that 9 surgical treatments for LUTS/BPH studied in the current review did not decrease postoperative IIEF-5 score except PVP. Moreover, HoLEP and PKEP showed pro-erectile effect even for patients with decreased baseline EF and short-term follow-up. TURP, the golden standard procedure, also improved post-TURP IIEF-5 for patients followed up over 12 months or having normal baseline EF. Only PVP showed negative effect on EF, but it was observed only in the short term and decrease baseline group, and it also showed no effect on EF in the long-term follow-up. New technologies, such as LSP and PKRP, ranked the first and the second in the network analysis and showed promising less negative effect on EF, although they had no pro-erectile effect in direct comparison due to limited original studies or poor baseline IIEF-5 score. Therefore, further studies and longer follow-up are required to substantiate our findings.
Acknowledgment
The authors thank Yi Guo who is an epidemiologist at school of public health in Wuhan University for his help to guide and ensure all analysis.
Footnotes
Abbreviations: BPH = benign prostatic hyperplasia, cGMP = cyclic guanosine monophosphate, CI = confidence interval, ED = erectile dysfunction, EF = erectile function, GeMTC = Generate Mixed Treatment Comparison, HLT = Holmium laser treatment, HoLEP = Holmium laser enucleation of the prostate, HoLRP = Holmium laser resection of the prostate, IIEF = International Index of Erectile Function, IPSS = International Prostate Symptom Score, KTP = potassium-titanyl-phosphate, LSP = laparoscopic simple prostatectomy, LUTS = lower urinary tract symptoms, NO = nitric oxide, OP = open prostatectomy, PKEP = plasmakinetic enucleation of the prostate, PKRP = plasmakinetic resection of the prostate, PVP = photoselective vaporization of the prostate, QoL = quality of life, RCT = randomized controlled trial, ROCK = Rho-associated protein kinase, SD = standard deviation, SMD = standard mean difference, TUEVP = transurethral electrovaporization of the prostate, TUIP = transurethral incision of the prostate, TUMT = transurethral microwave therapy, TUNA = transurethral needle ablation, TURP = transurethral resection of the prostate.
ZL, PC, and JW contributed equally to this work.
Authorship: All authors have fulfilled all conditions required for authorship. ZL, QM, XHW, and XHZ conceived and designed the study. PC, HX, JW, and XW performed the electronic search, selected studies, extracted data, and performed quality assessment. ZL and XHZ analyzed data and conducted meta-analysis. ZL, PC, XW, and XHZ supervised the research, and edited and drafted revisions to the article.
Funding: XHZ is supported by National Natural Science Foundation of China (N.81270843 and N.81160086).
The authors report no conflicts of interest.
References
- [1].Gratzke C, Bachmann A, Descazeaud A, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 2015;67:1099–109. [DOI] [PubMed] [Google Scholar]
- [2].Vuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol 2015;22(5 suppl 1):1–6. [PubMed] [Google Scholar]
- [3].Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet 1991;338:469–71. [DOI] [PubMed] [Google Scholar]
- [4].Chute CG, Panser LA, Girman CJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol 1993;150:85–9. [DOI] [PubMed] [Google Scholar]
- [5].Sexton CC, Coyne KS, Kopp ZS, et al. The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA, UK and Sweden: EpiLUTS. Br J Urol Int 2009;103suppl 3:12–23. [DOI] [PubMed] [Google Scholar]
- [6].Barry MJ, Cantor A, Roehrborn CG, et al. Relationships among participant international prostate symptom score, benign prostatic hyperplasia impact index changes and global ratings of change in a trial of phytotherapy in men with lower urinary tract symptoms. J Urol 2013;189:987–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kupelian V, McVary KT, Kaplan SA, et al. Association of lower urinary tract symptoms and the metabolic syndrome: results from the Boston Area Community Health Survey. J Urol 2009;182:616–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Rosen R, Altwein J, Boyle P, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 2003;44:637–49. [DOI] [PubMed] [Google Scholar]
- [9].McVary KT. Erectile dysfunction and lower urinary tract symptoms secondary to BPH. Eur Urol 2005;47:838–45. [DOI] [PubMed] [Google Scholar]
- [10].Kohler TS, McVary KT. The relationship between erectile dysfunction and lower urinary tract symptoms and the role of phosphodiesterase type 5 inhibitors. Eur Urol 2009;55:38–48. [DOI] [PubMed] [Google Scholar]
- [11].Ozayar A, Zumrutbas AE, Yaman O. The relationship between lower urinary tract symptoms (LUTS), diagnostic indicators of benign prostatic hyperplasia (BPH), and erectile dysfunction in patients with moderate to severely symptomatic BPH. Int Urol Nephrol 2008;40:933–9. [DOI] [PubMed] [Google Scholar]
- [12].Miner M, Rosenberg MT, Perelman MA. Treatment of lower urinary tract symptoms in benign prostatic hyperplasia and its impact on sexual function. Clin Therapeut 2006;28:13–25. [DOI] [PubMed] [Google Scholar]
- [13].Roehrborn CG. Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Med Clin N Am 2011;95:87–100. [DOI] [PubMed] [Google Scholar]
- [14].Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 2013;64:118–40. [DOI] [PubMed] [Google Scholar]
- [15].Jung JH, Jae SU, Kam SC, et al. Correlation between Lower Urinary Tract Symptoms (LUTS) and sexual function in benign prostatic hyperplasia: impact of treatment of LUTS on sexual function. J Sex Med 2009;6:2299–304. [DOI] [PubMed] [Google Scholar]
- [16].Kassabian VS. Sexual function in patients treated for benign prostatic hyperplasia. Lancet 2003;361:60–2. [DOI] [PubMed] [Google Scholar]
- [17].Leliefeld HH, Stoevelaar HJ, McDonnell J. Sexual function before and after various treatments for symptomatic benign prostatic hyperplasia. Br J Urol Int 2002;89:208–13. [DOI] [PubMed] [Google Scholar]
- [18].Gu RZ, Xia SJ. Surgical options for benign prostatic hyperplasia: impact on sexual function and risk factors. Natl J Androl 2011;17:837–41. [PubMed] [Google Scholar]
- [19].Arai Y, Aoki Y, Okubo K, et al. Impact of interventional therapy for benign prostatic hyperplasia on quality of life and sexual function: a prospective study. J Urol 2000;164:1206–11. [PubMed] [Google Scholar]
- [20].Ahyai SA, Gilling P, Kaplan SA, et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol 2010;58:384–97. [DOI] [PubMed] [Google Scholar]
- [21].Cornu JN, Ahyai S, Bachmann A, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 2015;67:1066–96. [DOI] [PubMed] [Google Scholar]
- [22].Thangasamy IA, Chalasani V, Bachmann A, et al. Photoselective vaporisation of the prostate using 80-W and 120-W laser versus transurethral resection of the prostate for benign prostatic hyperplasia: a systematic review with meta-analysis from 2002 to 2012. Eur Urol 2012;62:315–23. [DOI] [PubMed] [Google Scholar]
- [23].Lourenco T, Pickard R, Vale L, et al. Alternative approaches to endoscopic ablation for benign enlargement of the prostate: systematic review of randomised controlled trials. Br Med J 2008;337:a449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Biester K, Skipka G, Jahn R, et al. Systematic review of surgical treatments for benign prostatic hyperplasia and presentation of an approach to investigate therapeutic equivalence (non-inferiority). Br J Urol Int 2012;109:722–30. [DOI] [PubMed] [Google Scholar]
- [25].Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. Eur Urol 2009;56:798–809. [DOI] [PubMed] [Google Scholar]
- [26].Zong HT, Peng XX, Yang CC, et al. The impact of transurethral procedures for benign prostate hyperplasia on male sexual function: a meta-analysis. J Androl 2012;33:427–34. [DOI] [PubMed] [Google Scholar]
- [27].Frieben RW, Lin HC, Hinh PP, et al. The impact of minimally invasive surgeries for the treatment of symptomatic benign prostatic hyperplasia on male sexual function: a systematic review. Asian J Androl 2010;12:500–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hatzimouratidis K, Amar E, Eardley I, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol 2010;57:804–14. [DOI] [PubMed] [Google Scholar]
- [29].Yin X, Xiao Y, Li F, et al. Prognostic role of neutrophil-to-lymphocyte ratio in prostate cancer: a systematic review and meta-analysis. Medicine 2016;95: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Dhalwani NN, Tata LJ, Coleman T, et al. Completeness of maternal smoking status recording during pregnancy in United Kingdom primary care data. PloS One 2013;8:e72218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Chen P, Zhang W, Wang X, et al. Lycopene and risk of prostate cancer. Medicine 2015;94: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Br Med J 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].van Valkenhoef G, Lu G, de Brock B, et al. Automating network meta-analysis. Res Synth Meth 2012;3:285–99. [DOI] [PubMed] [Google Scholar]
- [35].Briganti A, Naspro R, Gallina A, et al. Impact on sexual function of holmium laser enucleation versus transurethral resection of the prostate: results of a prospective, 2-center, randomized trial. J Urol 2006;175:1817–21. [DOI] [PubMed] [Google Scholar]
- [36].Chen YB, Chen Q, Wang Z, et al. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year followup. J Urol 2013;189:217–22. [DOI] [PubMed] [Google Scholar]
- [37].Chen Q, Zhang L, Fan QL, et al. Bipolar transurethral resection in saline vs traditional monopolar resection of the prostate: results of a randomized trial with a 2-year follow-up. Br J Urol Int 2010;106:1339–43. [DOI] [PubMed] [Google Scholar]
- [38].Elmansy HM, Elzayat E, Elhilali MM. Holmium laser ablation versus photoselective vaporization of prostate less than 60 cc: long-term results of a randomized trial. J Urol 2010;184:2023–8. [DOI] [PubMed] [Google Scholar]
- [39].Horasanli K, Silay MS, Altay B, et al. Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology 2008;71:247–51. [DOI] [PubMed] [Google Scholar]
- [40].Kumar A, Vasudeva P, Kumar N, et al. A prospective randomized comparative study of monopolar and bipolar transurethral resection of the prostate and photoselective vaporization of the prostate in patients who present with benign prostatic obstruction: a single center experience. J Endourol 2013;27:1245–53. [DOI] [PubMed] [Google Scholar]
- [41].Mamoulakis C, Skolarikos A, Schulze M, et al. Bipolar vs monopolar transurethral resection of the prostate: evaluation of the impact on overall sexual function in an international randomized controlled trial setting. Br J Urol Int 2013;112:109–20. [DOI] [PubMed] [Google Scholar]
- [42].Montorsi F, Naspro R, Salonia A, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol 2004;172(5 Pt 1):1926–9. [DOI] [PubMed] [Google Scholar]
- [43].Naspro R, Suardi N, Salonia A, et al. Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24-month follow-up. Eur Urol 2006;50:563–8. [DOI] [PubMed] [Google Scholar]
- [44].Rao JM, Yang JR, Ren YX, et al. Plasmakinetic enucleation of the prostate versus transvesical open prostatectomy for benign prostatic hyperplasia >80 mL: 12-month follow-up results of a randomized clinical trial. Urology 2013;82:176–81. [DOI] [PubMed] [Google Scholar]
- [45].Xia SJ, Zhuo J, Sun XW, et al. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol 2008;53:382–9. [DOI] [PubMed] [Google Scholar]
- [46].Xie JB, Tan YA, Wang FL, et al. Extraperitoneal laparoscopic adenomectomy (Madigan) versus bipolar transurethral resection of the prostate for benign prostatic hyperplasia greater than 80 ml: complications and functional outcomes after 3-year follow-up. J Endourol 2014;28:353–9. [DOI] [PubMed] [Google Scholar]
- [47].Zhao Z, Zeng G, Zhong W, et al. A prospective, randomised trial comparing plasmakinetic enucleation to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: three-year follow-up results. Eur Urol 2010;58:752–8. [DOI] [PubMed] [Google Scholar]
- [48].Zhu L, Chen S, Yang S, et al. Electrosurgical enucleation versus bipolar transurethral resection for prostates larger than 70 ml: a prospective, randomized trial with 5-year followup. J Urol 2013;189:1427–31. [DOI] [PubMed] [Google Scholar]
- [49].Wang Y, Shao J, Lu Y, et al. Impact of 120-W 2-mum continuous wave laser vapoenucleation of the prostate on sexual function. Lasers Med Sci 2014;29:689–93. [DOI] [PubMed] [Google Scholar]
- [50].Sinanoglu O, Ekici S, Tatar MN, et al. Postoperative outcomes of plasmakinetic transurethral resection of the prostate compared to monopolar transurethral resection of the prostate in patients with comorbidities. Urology 2012;80:402–6. [DOI] [PubMed] [Google Scholar]
- [51].Bachmann A, Tubaro A, Barber N, et al. A European multicenter randomized noninferiority trial comparing 180 W GreenLight XPS laser vaporization and transurethral resection of the prostate for the treatment of benign prostatic obstruction: 12-month results of the GOLIATH study. J Urol 2015;193:570–8. [DOI] [PubMed] [Google Scholar]
- [52].Coskuner ER, Ozkan TA, Koprulu S, et al. The role of the bipolar plasmakinetic TURP over 100 g prostate in the elderly patients. Int Urol Nephrol 2014;46:2071–7. [DOI] [PubMed] [Google Scholar]
- [53].Taylor JM, Desouza R, Wang R. Common approach to managing lower urinary tract symptoms and erectile dysfunction. Asian J Androl 2008;10:45–53. [DOI] [PubMed] [Google Scholar]
- [54].Gacci M, Eardley I, Giuliano F, et al. Critical analysis of the relationship between sexual dysfunctions and lower urinary tract symptoms due to benign prostatic hyperplasia. Eur Urol 2011;60:809–25. [DOI] [PubMed] [Google Scholar]
- [55].Andersson KE, de Groat WC, McVary KT, et al. Tadalafil for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: pathophysiology and mechanism(s) of action. Neurourol Urodyn 2011;30:292–301. [DOI] [PubMed] [Google Scholar]
- [56].Kwon JS, Lee JW, Lee SW, et al. Comparison of effectiveness of monopolar and bipolar transurethral resection of the prostate and open prostatectomy in large benign prostatic hyperplasia. Korean J Urol 2011;52:269–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Muntener M, Aellig S, Kuettel R, et al. Sexual function after transurethral resection of the prostate (TURP): results of an independent prospective multicentre assessment of outcome. Eur Urol 2007;52:510–5. [DOI] [PubMed] [Google Scholar]
- [58].Gacci M, Bartoletti R, Figlioli S, et al. Urinary symptoms, quality of life and sexual function in patients with benign prostatic hypertrophy before and after prostatectomy: a prospective study. Br J Urol Int 2003;91:196–200. [DOI] [PubMed] [Google Scholar]
- [59].Paick JS, Um JM, Kim SW, et al. Influence of high-power potassium-titanyl-phosphate photoselective vaporization of the prostate on erectile function: a short-term follow-up study. J Sex Med 2007;4:1701–7. [DOI] [PubMed] [Google Scholar]
- [60].Bruyere F. The relationship between photoselective vaporization of the prostate and sexual function. Curr Urol Rep 2011;12:261–4. [DOI] [PubMed] [Google Scholar]
- [61].Bruyere F, Puichaud A, Pereira H, et al. Influence of photoselective vaporization of the prostate on sexual function: results of a prospective analysis of 149 patients with long-term follow-up. Eur Urol 2010;58:207–11. [DOI] [PubMed] [Google Scholar]
- [62].Kuntz RM, Ahyai S, Lehrich K, et al. Transurethral holmium laser enucleation of the prostate versus transurethral electrocautery resection of the prostate: a randomized prospective trial in 200 patients. J Urol 2004;172:1012–6. [DOI] [PubMed] [Google Scholar]
- [63].Meng F, Gao B, Fu Q, et al. Change of sexual function in patients before and after Ho:YAG laser enucleation of the prostate. J Androl 2007;28:259–61. [DOI] [PubMed] [Google Scholar]
- [64].Berardinelli F, Hinh P, Wang R. Minimally invasive surgery in the management of benign prostatic hyperplasia. Italian J Urol Nephrol 2009;61:269–89. [PubMed] [Google Scholar]
- [65].Dolowy L, Krajewski W, Dembowski J, et al. The role of lasers in modern urology. Central Eur J Urol 2015;68:175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Kaiho Y, Nakagawa H, Saito H, et al. Nerves at the ventral prostatic capsule contribute to erectile function: initial electrophysiological assessment in humans. Eur Urol 2009;55:148–54. [DOI] [PubMed] [Google Scholar]
- [67].Tscholl R, Largo M, Poppinghaus E, et al. Incidence of erectile impotence secondary to transurethral resection of benign prostatic hyperplasia, assessed by preoperative and postoperative Snap Gauge tests. J Urol 1995;153:1491–3. [PubMed] [Google Scholar]
- [68].Wasson JH, Reda DJ, Bruskewitz RC, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med 1995;332:75–9. [DOI] [PubMed] [Google Scholar]
- [69].Althof SE, Buvat J, Gutkin SW, et al. Sexual satisfaction in men with erectile dysfunction: correlates and potential predictors. J Sex Med 2010;7(1 pt 1):203–15. [DOI] [PubMed] [Google Scholar]


