Abstract
Carotid intima-media thickness (IMT) has been one widely used index of early carotid atherosclerosis. We speculated that the influence of blood pressure variability (BPV) on early carotid atherosclerosis may be varied by the location of the carotid artery and diabetes history. Thus, the goal of this study was to evaluate the effects of BPV on early arteriosclerosis progression in different segments of the carotid artery for hypertension with and without diabetes.
A total of 148 hypertension patients who underwent 24 hours ambulatory blood pressure (BP) monitoring and carotid ultrasonography were enrolled in this study. Of them, 84 subjects were without diabetes, and 64 subjects were with diabetes. Short-term BPV during daytime, nighttime, and over 24 hours were evaluated through standard deviation (SD) and average real variability (ARV). We measured carotid IMT at left and right common carotid artery (CCA), carotid bulb, and the origin of the internal carotid artery (ICA). The associations between segment-specific measurements of carotid IMT and 24 hours ambulatory BPV were analyzed.
We found that IMT at the common carotid artery (CCA-IMT) and IMT at the internal carotid artery (ICA-IMT) were more closely associated with BPV than was carotid bulb IMT. In addition, for all subjects, BPV was clearly associated with left CCA-IMT but not with right CCA-IMT. Furthermore, in diabetes patients, nighttime systolic BPV was independently related to mean CCA-IMT (P < 0.01) and mean bulb IMT (P < 0.01). In contrast, in nondiabetes patients, daytime and 24 hours systolic BPV was positively associated with mean CCA-IMT (P < 0.05), but not independent after adjusting for baseline characteristics such as age and sex.
The findings of our study indicate a segment-specific association between carotid IMT and 24 hours ambulatory BPV, and the associations also vary according to the diabetes history. We conclude that BPV plays a distinct role in early carotid arteriosclerosis progression within different segments of the carotid artery, especially for the hypertensions with and without diabetes.
Keywords: atherosclerosis, blood pressure variability, carotid intima-media thickness, diabetes, nondiabetes
1. Introduction
Carotid intima-media thickness (IMT) has been one widely used index of early carotid atherosclerosis,[1–4] and it can be measured at distinct sites of the carotid artery, such as the common carotid artery (CCA), carotid bulb, and the origin of the internal carotid artery (ICA).[5] Moreover, IMT at the CCA, carotid bulb, and ICA can provide important predictive information on cardiovascular disease.[6]
Most previous studies have investigated the relationship between 24 hours ambulatory blood pressure variability (BPV) and increased carotid wall thickness to determine the clinic impact of BPV on target organ damage, early atherosclerosis, or cardiovascular events.[7–11] However, few studies have focused on explaining the effects of blood pressure (BP) and BPV on hemodynamic shear stress of the carotid vessel wall,[12] especially in the carotid bulb and ICA. On a related topic, several studies recently reported that the carotid artery in different segments had specific characteristics and were influenced by different risk factors.[13–15] Furthermore, the prevalence of arteriosclerosis plaques has been found to be artery related.[16] Most plaques develop at the left anterior descending coronary artery and carotid bulb.[16] In addition, the left and right carotid arteries have been shown to display different reactions to hemodynamic and biochemical changes.[17] Therefore, we speculated that blood flow would have distinct effects on each segment of the carotid artery wall when BP fluctuates because each artery segment has a different anatomical structure and hemodynamic. However, few studies have evaluated the relationship between increased wall thickness in different locations of the carotid artery and BPV. Clarifying this relationship should be able to help us understand the mechanism of segment-specific atherosclerosis progression, and this new understanding could be used in the prevention and treatment of early carotid atherosclerosis and its complications.
Considering diabetes is one of the most important risk factors for the atherosclerosis progression and BP fluctuation may have different effects on the increase of carotid artery wall. Thus, we clarified the patients into 2 groups according to their diabetes history. The aim of the present study was to thoroughly evaluate the effects of BPV on early arteriosclerosis progression in different segments of the carotid artery and to provide consistent and complementary information about the relationship between carotid IMT and 24 hours ambulatory BPV in these 2 different patient groups.
2. Materials and methods
2.1. Study design and population
A total of 165 patients recruited from outpatient clinic of the hospital were enrolled in this study. All these subjects were participating in the screening of stroke and they were without the known history of cerebrovascular disease or myocardial infarction. The inclusion criteria were that all the subjects were medically treated for hypertension and underwent 24 hours BP monitoring and carotid ultrasound examination. Information about age, sex, current smoking, and diabetes history was obtained through questionnaires. Diabetes patients were defined as those with a previously physician diagnosed diabetes history. We excluded the subjects whose valid BP measurements during 24 hours were <90%. Finally, 148 eligible patients were included in this study, of them, 64 patients were diabetes and 84 patients were nondiabetes. This study was approved by the ethics committee of the Second People's Hospital of Shenzhen, Shenzhen, China. Written informed consent was obtained from all subjects.
2.2. Ambulatory BP measurement
Ambulatory BP was recorded using a commercial device (Mobil-O-Graph® 24 hours ABP-Control), which was set to take a recording every 30 minutes during the daytime (7:00 a.m.–10:59 p.m.) and every 60 minutes at nighttime (7:00 a.m.–10:59 p.m.). All participants were instructed to maintain their normal daily activities and to keep their arms still at each time of cuff inflation. The BPV parameters researched in this study included daytime systolic BPV (SBPV), daytime diastolic BPV (DBPV), nighttime SBPV, nighttime DBPV, 24 hours SBPV, and 24 hours DBPV. All these parameters were evaluated using standard deviation (SD) and average real variability (ARV) indices.
2.3. Carotid artery ultrasound examination
Carotid ultrasonography was performed using a high-resolution ultrasound Doppler system (iU22, Philips Ultrasound, Bothell, WA). All patients were requested to lie in a supine position, with their head turned 45° away from the examined side. Scanning was carried out on the bilateral CCA, carotid bulb, and ICA at 3 angles (lateral, anterior, and posterior), whereas the IMT measurements and the number of plaques were recorded. Plaque was defined as either focal IMT >1.5 mm or IMT 50% thicker than the surrounding area.[18,19] The criteria for measuring IMT were as follows: (1) IMT at CCA was measured at the far wall of the blood vessel, 10 to 20 mm proximal to dilation of the carotid bifurcation; (2) the carotid bulb was measured at the carotid bifurcation; and (3) the IMT at ICA was measured over a distance of 10 to 20 mm from the bifurcation. Specifically, all these IMT values were measured at plaque-free segments of the blood vessel. If a plaque appeared at the measurement point, then an appropriate adjacent portion was chosen. The IMT value at each position was defined as the average of IMTs measured from 3 angles. Furthermore, the mean left and right IMT of each segment was also calculated.
2.4. Statistical analysis
Continuous variables with a normal distribution were expressed as the mean ± SD, and variables with a frequency distribution were presented as a percentage. Student's t test and nonparametric Mann–Whitney U test for independent samples were used to test the difference in means between the 2 groups. The 2-tailed Pearson's test was used to examine the correlation between IMT and the number of plaques, as well as the associations between carotid IMT and BPV. Finally, multiple linear regression analyses were carried out to determine the relative influence of BPV variables on increased carotid IMT. Segment-specific carotid IMT were considered as the dependent factors. The linear regression models were adjusted for baseline characteristics, which including age, sex, smoking, and heart disease. All statistical analyses were performed using the IBM SPSS 13.0 software package (SPSS Inc., Chicago IL). P value < 0.05 was considered statistically significant in all the analyses mentioned above.
3. Results
3.1. Characteristics of the subjects
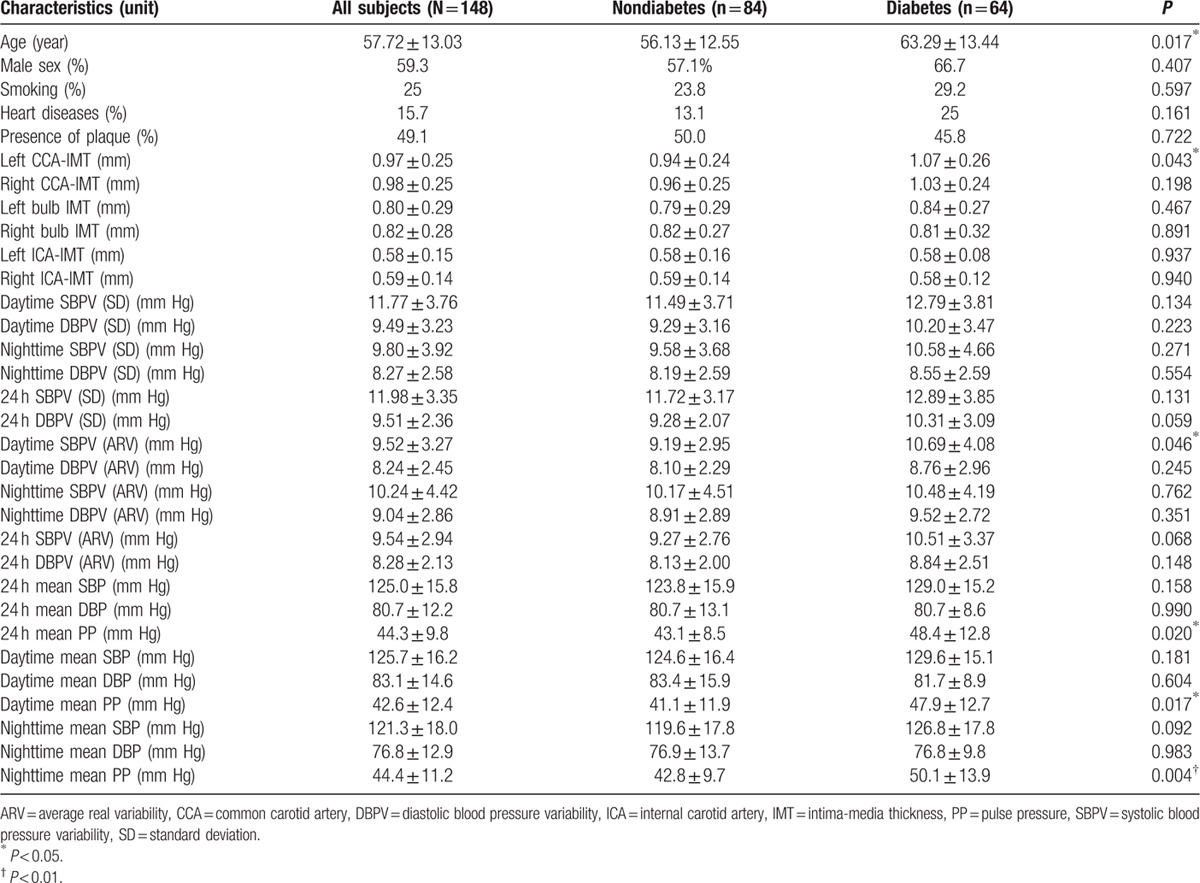
A total of 84 diabetes patients and 64 nondiabetes patients were included in this study. Table 1 describes their baseline characteristics, which included information on demographics, left and right IMTs at CCA, carotid bulb, ICA, BPV variables, and mean BP level. The table also presents statistical differences between the diabetes group and the nondiabetes group. The data showed that the diabetes patients were significantly older than the nondiabetes patients, and they had thicker CCA-IMT on the left side. Furthermore, diabetes patients had higher daytime SBPV (ARV index). Additionally, this table also shows that PP during daytime, nighttime, and 24 hours significantly differed between the 2 groups. Besides these variables, the 2 subgroups did not differ significantly in terms of other characteristics.
Table 1.
Baseline characteristics of all subjects.
3.2. Segment-specific prognostic significance
To examine the segment-specific prognostic significance of carotid IMT, we first estimated the association between IMTs and the number of plaques for all subjects. Figure 1 shows that all IMTs at the CCA, carotid bulb, and ICA strongly correlated with the number of plaques (r = 0.592, r = 0.670, r = 0.527; P < 0.001 for all). Among IMTs, IMT at the carotid bulb had the highest correlation coefficient (r = 0.670; P < 0.001). Figure 2 depicts the proportion of subjects with plaque according to quartiles of IMT measurements at individual sites. For all artery segments, the percentage of plaque formation increased from the lowest to the highest quartiles of IMT at each carotid artery segment. Moreover, an obvious increasing linear trend was observed for both CCA-IMT and bulb IMT that paralleled plaque prevalence.
Figure 1.
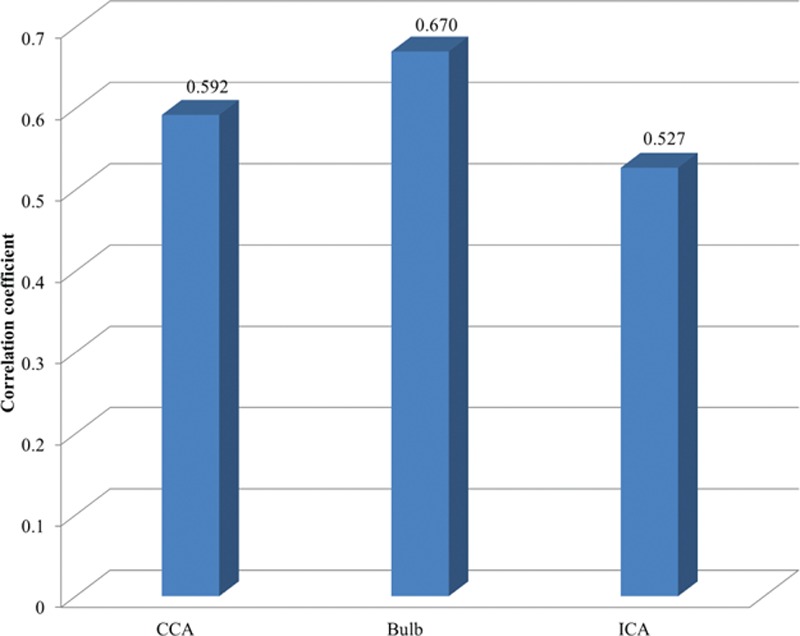
Correlation between IMT at 3 separate carotid artery segments and total number of carotid plaques. IMT = intima-media thickness.
Figure 2.
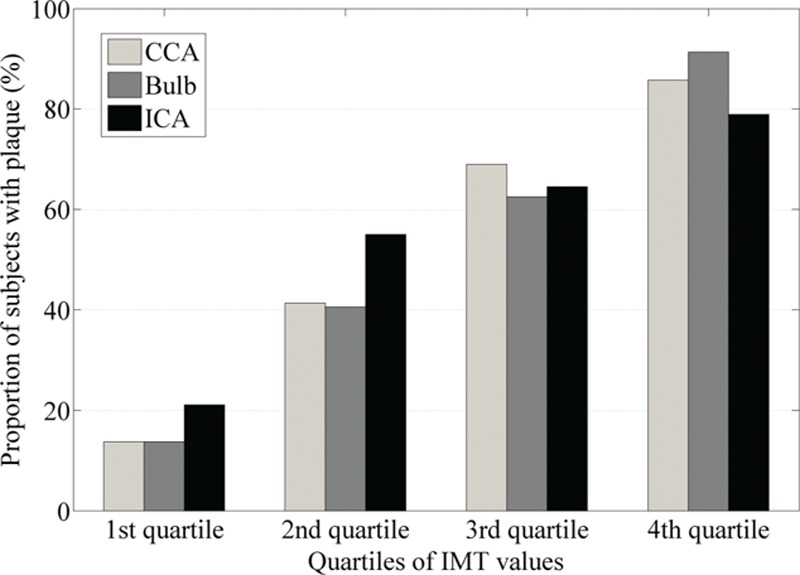
The proportion of subjects with plaque according to quartiles of IMT at CCA, carotid bulb and ICA. CCA = common carotid artery, ICA = internal carotid artery, IMT = intima-media thickness.
3.3. Bivariate analysis of BPV and IMT
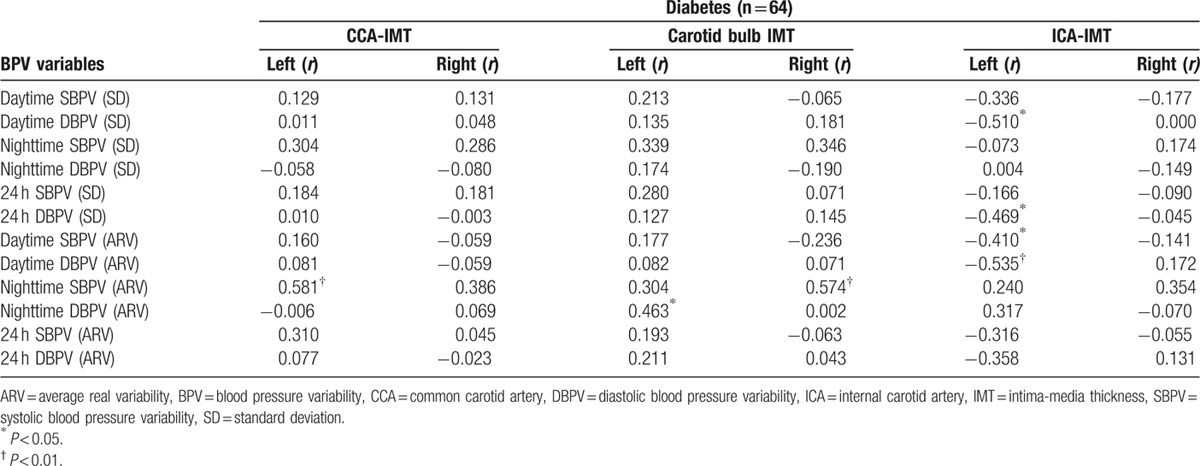
In our previous study, we found that the correlation between carotid IMT and ambulatory BPV differed in patients with and without diabetes.[20] Thus, for the present study, we divided patients into 2 subgroups according to their diabetes status and analyzed carotid artery segment-specific associations with BPV. Tables 2 and 3 show the correlations between carotid IMT and BPV variables for nondiabetes and diabetes patients, respectively. The significant correlation coefficients were marked in bold letters. For both groups, BPV variables were associated with left CCA-IMT but not right CCA-IMT. For nondiabetes patients, left CCA-IMT was associated with both daytime SBPV evaluated using the SD and ARV indices (r = 0.228, P = 0.037; r = 0.260, P = 0.017) and 24 hours SBPV evaluated using the ARV (r = 0.223, P = 0.041). For patients with diabetes, only nighttime SBPV estimated using the ARV index was associated with left CCA-IMT (r = 0.581, P = 0.003). In the carotid bulb IMT analysis, BPV correlated less with bulb IMT than with CCA-IMT. Only nighttime BPV using the ARV index was associated with bulb IMT in patients with diabetes (r = 0.463, P = 0.023 for nighttime DBPV and left bulb IMT; r = 0.574, P = 0.003 for nighttime SBPV and right bulb IMT). However, for the nondiabetes group, no BPV variables correlated with IMT in this segment of carotid artery. Similar to the analysis of CCA-IMT analysis, in the correlation analysis of ICA-IMT and BPV, differences in left and right artery segments were found. None of the BPV variables were associated with left ICA-IMT in the nondiabetes group. In contrast, daytime SBPV and 24 hours SBPV evaluated with the ARV and 24 hours SBPV evaluated with SD significantly correlated with right ICA-IMT (r = 0.232; r = 0.219; r = 0.232; P < 0.05 for all). However, for the diabetes group, all these associations pertained to the left side and showed negative correlation. Daytime SBPV and DBPV analyzed using ARV indices (r = −0.410, P = 0.047; r = −0.535, P = 0.007), both with daytime and 24 hours DBPV analyzed with the SD index (r = −0.469, P = 0.021; r = −0.510, P = 0.011) were negatively associated with left ICA-IMT, which was a different result from those for CCA and carotid bulb IMTs.
Table 2.
Correlation between different carotid IMTs and BPV for patients without diabetes.
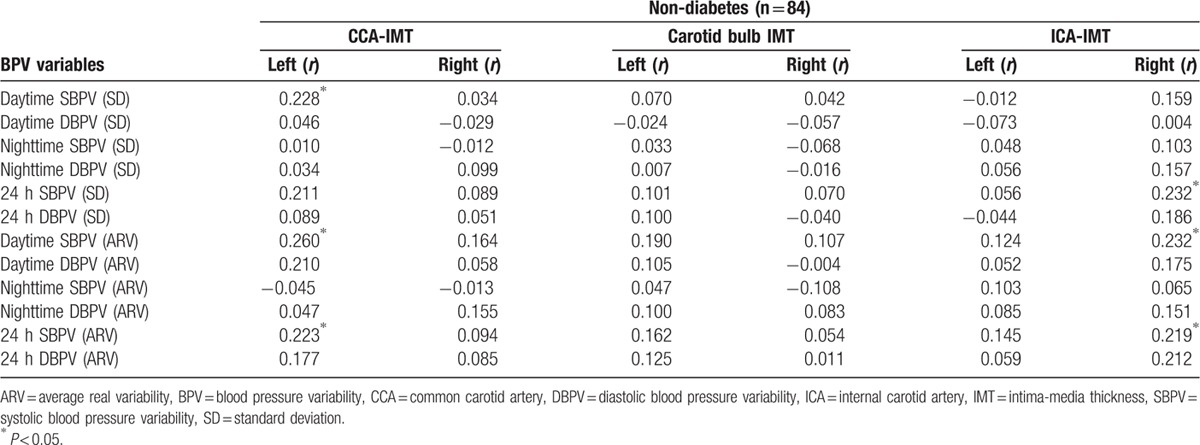
Table 3.
Correlation between different carotid IMTs and BPV for patients with diabetes.
Besides BPV variables, we also examined the correlation between the mean BP level and segment-specific carotid IMT. We only found that 24 hours mean DBP and daytime mean DBP were negatively correlated with mean ICA-IMT in the diabetes group (r = −0.518, P = 0.009; r = −0.540, P = 0.006, respectively). Besides these, no mean BP level were associated with carotid IMT.
Furthermore, we excluded the subjects with plaque to examine the relationship between BPV variables and initial thickening of the arterial wall. The significant results of nondiabetes are shown in Fig. 3. For nondiabetics, 24 hours and daytime SBPV/DBPV were correlated with the carotid IMT in 3 segments. However, for diabetics, only nighttime SBPV was related to the carotid CCA-IMT (r = 0.840, P < 0.001) and the correlation coefficients were higher than that in the above analysis.
Figure 3.
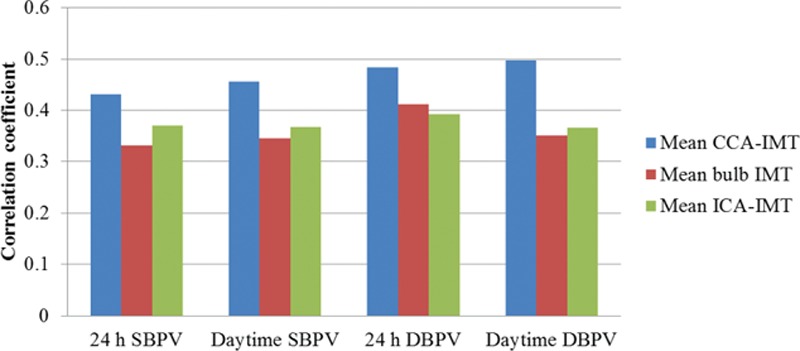
The correlation between BPV and mean IMT at 3 separate carotid artery segments in subjects without plaque. BPV = blood pressure variability, CCA = common carotid artery, DBPV = diastolic blood pressure variability, ICA = internal carotid artery, IMT = intima-media thickness, SBPV = systolic blood pressure variability.
3.4. Multiple regression analysis
Multiple regression analysis was performed using stepwise selection to estimate the associations between carotid IMT and BPV. Mean CCA-IMT, carotid bulb IMT, and ICA-IMT were dependent factors for both diabetes and nondiabetes patients. The BPV variables significantly correlated with each segment of carotid IMT in Tables 2 and 3 were considered independent factors for the corresponding model. As only mean ICA-IMT was correlated with mean BP, 24 hours mean DBP and daytime mean DBP were added into model 6 as the independent factors. Besides, all the statistical models were adjusted for age, sex, current smoking, and heart disease. Table 4 shows the results of the multiple regression analysis. Models 1 to 3 show the multiple regression analysis results for nondiabetes patients. Models 4 to 6 describe the regression analysis functions pertaining to patient with diabetes. These results showed the segment-specific associations between carotid IMT and BPV. For nondiabetes patients, the results in model 1 showed that age and smoking correlated in a linear fashion with mean CCA-IMT (P < 0.001 for both). In model 2, mean carotid bulb IMT was the dependent factor, and only age remained in the model (P = 0.003). However, in model 3, age (P = 0.001) and sex (P = 0.002) were the factors correlated with increased mean ICA-IMT.
Table 4.
Adjusted multiple regression analyses of factors associated with segment-specific measurements of carotid IMT.
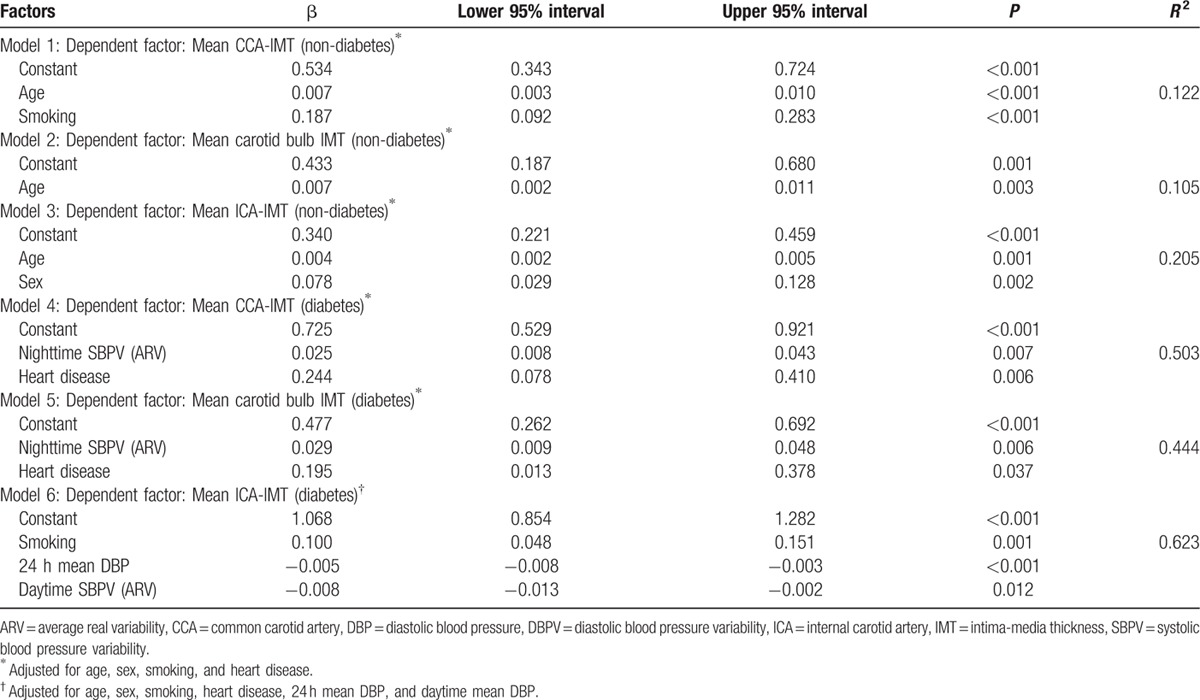
The results for diabetes patients differed entirely. Models 4 and 5 had similar results in which, instead of age and sex, nighttime SBPV using the ARV index (P = 0.007 for model 4, P = 0.006 for model 5) and heart disease (P = 0.006 for model 4, P = 0.037 for model 5) were significantly associated with mean CCA-IMT and carotid bulb IMT. In model 6, age was also not found to be an independent factor in the model. However, smoking (P = 0.001) and 24 hours mean DBP (P < 0.001) and daytime SBPV (ARV) (P = 0.012) were the factors in this model which evaluated the increased mean ICA-IMT. Among these models, all the linear models pertaining to patients with diabetes had better linear fitting than did the models for nondiabetes patients.
4. Discussion
Our study provided fresh insight into the influence of 24 hours ambulatory BPV on early carotid atherosclerosis in hypertension with and without diabetes. Early carotid atherosclerosis was evaluated using different segments of carotid IMT measurements in the asymptomatic individuals. It contributed 3 major findings. First, ambulatory BPV variables were closely associated with segment-specific measures of carotid IMT, which were revealed not only in different sites of the carotid artery, but also in the bilateral carotid artery. Second, the associations uncovered varied in patients with and without diabetes. In patients with diabetes, nighttime SBPV was an independent risk factor related to CCA-IMT and carotid bulb IMT. In nondiabetes patients, daytime and 24 hours SBPV was positively associated with CCA-IMT and ICA-IMT. However, they could not explain the progression of carotid IMT after adjusting for baseline characteristics. Third, although different segments of the carotid artery had similar prognostic significance for early arteriosclerosis or plaque prevalence, the underlying mechanisms of BPV for increasing vessel wall thickness may have been different.
Several studies have investigated the associations between carotid IMT and traditional risk factors, such as age, sex, body mass index, and BP.[13,21] Nguyen et al have reported the association between progression of segment-specific carotid IMT and traditional risk factors such as age, race, glucose, cholesterol, and BP level.[22] However, the influence of BPV on different carotid artery locations has been scantly studied. Thus, our present study explored the associations between BPV and segment-specific measurements of carotid IMT. We found that CCA-IMT and ICA-IMT had stronger associations with BPV than did carotid bulb IMT. In addition, in all subjects, BPV was clearly associated with left CCA-IMT but not right CCA-IMT. These results support our hypothesis that BPV has distinct effects on different sites of carotid IMT and may lead to segment-specific early atherosclerosis progression. Possible explanations for these results are listed as follows.
First, the CCA is an elastic artery, the carotid bulb is situated in a transitional zone between elastic and muscular artery types,[23] and the ICA is a muscular artery.[24] Therefore, the mechanisms through which foam-cell lesions form are different at these carotid sites,[24] thereby contributing to differences in atherosclerosis expression. Second, the left CCA stems directly from the aortic arch and is affected by aortic arch pressure. The right CCA stems from the innominate artery, which is an extension of the ascending aorta, and is subject to significant pressure from ascending aortic blood flow.[17] Thus, segment-specific associations might account for these hemodynamic and anatomical differences. Luo et al[17] also proposed this hypothesis and found that left carotid IMT was associated mainly with blood biochemical indices, whereas right carotid IMT correlated mainly with hemodynamic parameters. Another study found that CCA-IMT, carotid bulb IMT, and ICA-IMT showed segment-specific associations with cardiovascular risk factors in young white and black men and women. Fasting glucose and diastolic BP had higher correlations with CCA than for other segments.[13] These studies support our view on segment-specific associations. Thus, we conclude that BPV plays a distinct role in arteriosclerosis progression within the different segments of the carotid artery.
Many studies have investigated the relationship between BPV and carotid IMT but reported inconsistent results. Several studies found that daytime or/and 24 hours SBPV was positively associated with increased carotid IMT, early atherosclerosis, or organ damage.[25–29] Other studies suggested that only nighttime variability in SBP, but not daytime variability in SBP, was related to carotid atherosclerosis or cardiovascular outcomes.[30,31] A recent study reported that time rate of BP variation but not ambulatory BPV was correlated with carotid IMT.[32] These controversial results may have arisen from differences in patient population selection, BPV index, sample size, study endpoints, and other factors. In our previous study,[20] we found that, for the nondiabetes patients, SBP fluctuations during daytime and during a 24 hours period were significantly associated with increased CCA-IMT. In the present study, we divided patients into 2 subgroups: nondiabetes and diabetes. We found that for diabetes patients, nighttime SBPV was strongly associated with CCA-IMT and carotid bulb IMT and was independently correlated with mean CCA-IMT and bulb IMT after adjusting for age, sex, smoking, and heart disease. In contrast, for hypertension patients without diabetes, daytime and 24 hours SBPV had a positive significant correlation with CCA-IMT and ICA-IMT. However, they were not remained in the adjusted regression models. Not only was BPV associated with increased IMT, but nighttime BPV and daytime BPV had distinct associations with IMT according to patient population. This finding is in line with the study of Eguchi et al,[33] who found that instead of diurnal BP variation, nighttime SBPV was a strong independent predictor of cardiovascular events in patients with type 2 diabetes. However, the relationship between IMT and BPV in patients without diabetes has not been extensively examined. We can only speculate that BPV has different mechanisms of action on artery alteration in individuals with and without diabetes. Moreover, these results indicate that for nondiabetes patients, nighttime SBPV can be as significant a predictor for increased carotid IMT. All these findings will enhance our understanding of the progression of arteriosclerosis in these 2 groups, and they promise to provide a fresh perspective on prevention and treatment of early carotid atherosclerosis and its complications.
Our study also provided evidence that different segments of the carotid artery have similar prognostic significance for arteriosclerosis or the prevalence of plaque. This evidence corroborates the conclusions of Damiano et al.[6] In addition, we found that carotid bulb IMT and CCA-IMT were associated more closely with the number of plaques than was ICA-IMT. The results implied how atherosclerosis manifests within different arteries. Dalager et al established that, owing to its structure, the carotid bifurcation could easily develop foam-cell lesions and lipid core plaques from an early stage. Furthermore, this study clarified that the carotid bulb is a common site of plaque development.[16] Accordingly, the wall thickness at this site is greater when more plaques form. This observation could explain our result that carotid bulb IMT correlated more closely with the number of plaques. In a related finding, Bots et al found that CCA-IMT could predict atherosclerosis formation elsewhere in the carotid artery, such as at the bifurcation and the near and far walls of the distal CCA.[34] Their findings agree with our results about the linear correlation between increased CCA-IMT and the percentage of plaque prevalence. Thus, we conclude that CCA-IMT and bulb IMT have higher prognostic significance for plaque prevalence than do IMTs measured at ICA.
Several other findings of our study deserve to be briefly discussed. First, the results from Tables 2 and 3 showed that the ARV index had higher correlation coefficient with carotid IMT, especially in the patients without plaque. Thus, we concluded that the ARV index had better prognostic significance for evaluating the increased carotid IMT. This finding is consistent with the conclusion of Mena et al,[35] who reported that the ARV index showed better prognostic significance for organ damage and cardiovascular risk than did the SD index. Hansen et al also indicated that although both daytime BPV (using the SD index) and 24 hours BPV (using the ARV index) were useful measures, BPV estimated using the SD index over 24 hours was not.[36] Thus, the ARV index is a more reliable measurement for BPV. Second, we discussed whether BPV was an independent factor for predicting increased carotid IMT at different sites, an idea that had proven controversial based on the results of previous studies.[7,37,38] In our multiple regression analysis, we adjusted for age, sex, smoking, and heart disease, and found that various risk factors influenced segment-specific carotid IMT. For nondiabetes patients, age was a factor in all the regression models. However, for diabetes patients, heart disease and smoking were risk factors for increased carotid artery wall thickness. The mean BP level did not contribute for the progression of the carotid artery wall, except for the ICA-IMT. The increased ICA-IMT can be explained both by 24 hours mean DBP and daytime SBPV. Third, mean daytime DBP and daytime SBPV showed a strong negative correlation with mean ICA-IMT, and this association persisted even after adjusting for baseline characteristics. Lastly, we examined the relations between BPV and carotid IMT in patients without plaque. In Sander's study published in Circulation,[25] they investigated the relationship between circadian BP pattern and progression of early carotid. It is a follow-up study, and all the patients were >55 years old. In their research, early atherosclerosis was defined as an age-adjusted IMT>1.5 mm. In our study, IMT>1.5 mm indicated the presence of plaque, which is the early sighs of the atherosclerosis. However, in our results shown in Fig. 3, BPV is highly correlated with the increased carotid IMT before the plaque formation. Maybe it will provide a possible pattern to predict the carotid atherosclerosis in the early stage.
Finally, some limitations of our study should be acknowledged. First, this was a cross-sectional descriptive design, and therefore we could not infer the cause-and-effect relationship between BPV and increased IMT or plaque formation. Second, we measured nighttime BP once per hour, so this frequency of reading provided limit BP data for computing BPV. Third, the number of subjects in our study was limited, especially for patients with diabetes. We referred to several small sample studies and similar studies,[39–41] the conclusion is reasonable although the limited data. However, further study with a large-scale patient population is still needed to verify our results.
5. Conclusions
The present study provided initial data about the relationship between ambulatory BPV and different carotid segment IMTs in hypertension with and without diabetes. Its findings indicate that for all subjects, the association between bilateral carotid IMT and ambulatory BPV had clear differences that appeared not only in different carotid artery segments, but also in the left and right carotid artery. We speculate that these phenomena resulted from different anatomical structures and hemodynamic. However, scant evidence is available to verify this hypothesis. Thus, a further study is needed to explore the effects of BPV on arteriosclerosis progression.
Footnotes
Abbreviations: ARV = average real variability, BP = blood pressure, BPV = blood pressure variability, CCA = common carotid artery, CCA-IMT = IMT at the common carotid artery, DBP = diastolic blood pressure, DBPV = diastolic blood pressure variability, ICA = internal carotid artery, ICA-IMT = IMT at the internal carotid artery, IMT = carotid intima-media thickness, PP = pulse pressure, SBP = systolic blood pressure, SBPV = systolic blood pressure variability, SD = standard deviation.
Funding: this work was supported in part by the STS project of Chinese Academy of Sciences (KFJ-EW-STS-097), Guangdong Image-guided Therapy Innovation Team (2011S013), Shenzhen Innovation Funding (SGLH20150213143207911, JCYJ20140901003939025, SGLH20131010110119871, GJHZ20140415152115754, JCYJ20151030151431727, JCYJ20140414170821190 and SGLH20150216172854731) and Shenzhen science and technology innovation Funding (CXZZ20140909004122087).
The authors have no conflicts of interest to disclose.
References
- [1].Polak JF, Pencina MJ, O’Leary DH, et al. Common carotid artery intima-media thickness progression as a predictor of stroke in multi-ethnic study of atherosclerosis. Stroke 2011;42:3017–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Haley AP, Forman DE, Poppas A, et al. Carotid artery intima-media thickness and cognition in cardiovascular disease. Int J Cardiol 2007;121:148–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: The Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol 1997;146:483–94. [DOI] [PubMed] [Google Scholar]
- [4].O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med 1999;340:14–22. [DOI] [PubMed] [Google Scholar]
- [5].Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim carotid intima-media thickness consensus (2004–2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis 2007;23:75–80. [DOI] [PubMed] [Google Scholar]
- [6].Baldassarre D, Hamsten A, Veglia F, et al. Measurements of carotid intima-media thickness and of interadventitia common carotid diameter improve prediction of cardiovascular events: results of the IMPROVE (Carotid Intima Media Thickness [IMT] and IMT-Progression as Predictors of Vascular Events in a High Risk European Population) Study. J Am Coll Cardiol 2012;60:1489–99. [DOI] [PubMed] [Google Scholar]
- [7].Sega R, Corrao G, Bombelli M, et al. Blood pressure variability and organ damage in a general population: results from the PAMELA study (Pressioni Arteriose Monitorate E Loro Associazioni). Hypertens 2002;39(2 pt 2):710–4. [DOI] [PubMed] [Google Scholar]
- [8].Mancia G, Parati G, Hennig M, et al. Relation between blood pressure variability and carotid artery damage in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens 2001;19:1981–9. [DOI] [PubMed] [Google Scholar]
- [9].Garcia-Garcia A, Garcia-Ortiz L, Recio-Rodriguez JI, et al. Relationship of 24-h blood pressure variability with vascular structure and function in hypertensive patients. Blood Press Monit 2013;18:101–6. [DOI] [PubMed] [Google Scholar]
- [10].Su DF, Miao CY. Blood pressure variability and organ damage. Clin Exp Pharmacol Physiol 2001;28:709–15. [DOI] [PubMed] [Google Scholar]
- [11].Su TC, Lee YT, Chou S, et al. Twenty-four-hour ambulatory blood pressure and duration of hypertension as major determinants for intima-media thickness and atherosclerosis of carotid arteries. Atherosclerosis 2006;184:151–6. [DOI] [PubMed] [Google Scholar]
- [12].Mancia G, Grassi G. Mechanisms and clinical implications of blood pressure variability. J Cardiovasc Pharmacol 2000;35(7 suppl 4):S15–9. [DOI] [PubMed] [Google Scholar]
- [13].Polak JF, Person SD, Wei GS, et al. Segment-specific associations of carotid intima-media thickness with cardiovascular risk factors: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Stroke 2010;41:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Espeland MA, Evans GW, Wagenknecht LE, et al. Site-specific progression of carotid artery intimal-medial thickness. Atherosclerosis 2003;171:137–43. [DOI] [PubMed] [Google Scholar]
- [15].Schott LL, Wildman RP, Brockwell S, et al. Segment-specific effects of cardiovascular risk factors on carotid artery intima-medial thickness in women at midlife. Arterioscler Thromb Vasc Biol 2004;24:1951–6. [DOI] [PubMed] [Google Scholar]
- [16].Dalager S, Paaske WP, Kristensen IB, et al. Artery-related differences in atherosclerosis expression: implications for atherogenesis and dynamics in intima-media thickness. Stroke 2007;38:2698–705. [DOI] [PubMed] [Google Scholar]
- [17].Luo X, Yang Y, Cao T, et al. Differences in left and right carotid intima-media thickness and the associated risk factors. Clin Radiol 2011;66:393–8. [DOI] [PubMed] [Google Scholar]
- [18].Sinning C, Kieback A, Wild PS, et al. Association of multiple biomarkers and classical risk factors with early carotid atherosclerosis: results from the Gutenberg Health Study. Clin Res Cardiol 2014;103:477–85. [DOI] [PubMed] [Google Scholar]
- [19].Fernández-Ortiz A, Jiménez-Borreguero LJ, Peñalvo JL, et al. The Progression and Early detection of Subclinical Atherosclerosis (PESA) study: rationale and design. Am Heart J 2013;166:990–8. [DOI] [PubMed] [Google Scholar]
- [20].Xiong HH, Wu D, Tian XH, et al. The relationship between the 24 h blood pressure variability and carotid intima-media thickness: a compared study. Comput Math Methods Med 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Rundek T, Blanton SH, Bartels S, et al. Traditional risk factors are not major contributors to the variance in carotid intima-media thickness. Stroke 2013;44:2101–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Nguyen QM, Toprak A, Xu JH, et al. Progression of segment-specific carotid artery intima-media thickness in young adults (from the Bogalusa Heart Study). Am J Cardiol 2011;107:114–9. [DOI] [PubMed] [Google Scholar]
- [23].McGill HC, Arias-Stella J, Carbonell LM. General findings of the International Atherosclerosis Project. Lab Invest 1968;18:498–502. [PubMed] [Google Scholar]
- [24].Janzen J. The microscopic transitional zone between elastic and muscular arteries. Arch Mal Coeur Vaiss 2004;97:909–14. [PubMed] [Google Scholar]
- [25].Sander D, Kukla C, Klingelhofer J, et al. Relationship between circadian blood pressure patterns and progression of early carotid atherosclerosis: a 3-year follow-up study. Circulation 2000;102:1536–41. [DOI] [PubMed] [Google Scholar]
- [26].Zakopoulos NA, Tsivgoulis G, Barlas G, et al. Time rate of blood pressure variation is associated with increased common carotid artery intima-media thickness. Hypertens 2005;45:505–12. [DOI] [PubMed] [Google Scholar]
- [27].Ciobanu AO, Gherghinescu CL, Dulgheru R, et al. The impact of blood pressure variability on subclinical ventricular, renal and vascular dysfunction, in patients with hypertension and diabetes. Madica 2013;8:129–36. [PMC free article] [PubMed] [Google Scholar]
- [28].Kikuya M, Hozawa A, Ohokubo T, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertens 2000;36:901–6. [DOI] [PubMed] [Google Scholar]
- [29].Sander D, Klingelhofer J. Diurnal systolic blood pressure variability is the strongest predictor of early carotid atherosclerosis. Neurology 1996;47:500–7. [DOI] [PubMed] [Google Scholar]
- [30].Pringle E, Phillips C, Thijs L, et al. Systolic blood pressure variability as a risk factor for stroke and cardiovascular mortality in the elderly hypertensive population. J Hypertens 2003;21:2251–7. [DOI] [PubMed] [Google Scholar]
- [31].Eguchi K, Hoshide S, Schwartz JE, et al. Visit-to-visit and ambulatory blood pressure variability as predictors of incident cardiovascular events in patients with hypertension. Am J Hypertens 2012;25:962–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Manios E, Michas F, Stamatelopoulos K, et al. Short-term beat-to-beat but not ambulatory blood pressure variability is correlated to carotid intima-media thickness. Blood Press Monit 2014;19:288–93. [DOI] [PubMed] [Google Scholar]
- [33].Eguchi K, Ishikawa J, Hoshide S, et al. Night time blood pressure variability is a strong predictor for cardiovascular events in patients with type 2 diabetes. Am J Hypertens 2009;22:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Bots ML, Hofman A, deJong PTVM, et al. Common carotid intima media thickness as an indicator of atherosclerosis at other sites of the carotid artery: the Rotterdam Study. Ann Epidemiol 1996;6:147–53. [DOI] [PubMed] [Google Scholar]
- [35].Mena L, Pintos S, Queipo NV, et al. A reliable index for the prognostic significance of blood pressure variability. J Hypertens 2005;23:505–11. [DOI] [PubMed] [Google Scholar]
- [36].Hansen TW, Thijs L, Li Y, et al. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8938 subjects from 11 populations. Hypertens 2010;55:1049–57. [DOI] [PubMed] [Google Scholar]
- [37].Kikuya M, Hozawa A, Ohokubo T, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertens 2000;36:901–6. [DOI] [PubMed] [Google Scholar]
- [38].Nagai M, Hoshide S, Ishikawa J, et al. Visit-to-visit blood pressure variations: new independent determinants for cognitive function in the elderly at high risk of cardiovascular disease. J Hypertens 2012;30:1556–63. [DOI] [PubMed] [Google Scholar]
- [39].Ozguven I, Ersoy B, Ozguven A, et al. Factors affecting carotid intima media thickness predicts early atherosclerosis in overweight and obese adolescents. Obes Res Clin Pract: 2010;4:e41–8. [DOI] [PubMed] [Google Scholar]
- [40].Schoenenberger AW, Erne P, Ammann S, et al. Prediction of hypertensive crisis based on average, variability and approximate entropy of 24-h ambulatory blood pressure monitoring. J Hum Hypertens 2007;22:32–7. [DOI] [PubMed] [Google Scholar]
- [41].Kawai T, Ohishi M, Kamide K, et al. Differences between daytime and nighttime blood pressure variability regarding systemic atherosclerotic change and renal function. Hypertens Res 2013;36:232–9. [DOI] [PubMed] [Google Scholar]


