Abstract
In the UK, treatment recommendations for patients with cancer are routinely made by multidisciplinary teams in weekly meetings. However, their performance is variable.
The aim of this study was to explore the underlying structure of multidisciplinary decision-making process, and examine how it relates to team ability to reach a decision.
This is a cross-sectional observational study consisting of 1045 patient reviews across 4 multidisciplinary cancer teams from teaching and community hospitals in London, UK, from 2010 to 2014. Meetings were chaired by surgeons.
We used a validated observational instrument (Metric for the Observation of Decision-making in Cancer Multidisciplinary Meetings) consisting of 13 items to assess the decision-making process of each patient discussion. Rated on a 5-point scale, the items measured quality of presented patient information, and contributions to review by individual disciplines. A dichotomous outcome (yes/no) measured team ability to reach a decision. Ratings were submitted to Exploratory Factor Analysis and regression analysis.
The exploratory factor analysis produced 4 factors, labeled “Holistic and Clinical inputs” (patient views, psychosocial aspects, patient history, comorbidities, oncologists’, nurses’, and surgeons’ inputs), “Radiology” (radiology results, radiologists’ inputs), “Pathology” (pathology results, pathologists’ inputs), and “Meeting Management” (meeting chairs’ and coordinators’ inputs). A negative cross-loading was observed from surgeons’ input on the fourth factor with a follow-up analysis showing negative correlation (r = −0.19, P < 0.001). In logistic regression, all 4 factors predicted team ability to reach a decision (P < 0.001).
Hawthorne effect is the main limitation of the study.
The decision-making process in cancer meetings is driven by 4 underlying factors representing the complete patient profile and contributions to case review by all core disciplines. Evidence of dual-task interference was observed in relation to the meeting chairs’ input and their corresponding surgical input into case reviews.
Keywords: database analysis, group decision-making, national health services, oncology, performance measurement
1. Introduction
1.1. Background
As a mandatory part of cancer care services in the UK, multidisciplinary team meetings (MDMs) comprise of diverse range of professionals—including surgeons, oncologists, radiologists, specialist cancer nurses, and pathologists.[1] Their purpose is to provide expert reviews of patient cases and formulate treatment recommendations, thus improving patient experience and ensuring well-coordinated delivery of safe, high-quality care. Although cancer guidelines support a multidisciplinary approach,[1] the empirical evidence of its effectiveness in terms of patient survival remains unclear,[2] and team performance across tumors is variable.[3] One pattern that keeps reemerging in recent studies is the skewed contribution to case reviews toward senior physicians and biomedical aspects of the disease; in contrast, cancer nurses’ input, patients’ comorbidities, and their psychosocial circumstances are underrepresented.[4–6] In line with this pattern, evidence from patient experience studies shows suboptimal experience of care often because of psychosocial circumstances not being adequately addressed and a “holistic” view of the patient not being considered by the healthcare providers.[7–8] Moreover, multidisciplinary team (MDT) members highlighted the importance of having a complete patient profile, as well as all participating disciplines in attendance, for effective decision-making.[9] Improving MDT working therefore is complex although highly important with the cancer incidence and costs of care being predicted to rise,[10–11] whereas the significant financial pressures on the healthcare remain.[12]
The National Cancer Action Team in England identified core domains essential for effective MDT working, including the team (e.g., attendance, team culture, training), infrastructure for meetings, organization and logistics, team governance, and finally, clinical decision-making process[13]—the latter being the primary focus of this article. Time pressures, cancer specialist nonattendance, lack of necessary information, poor consideration of patient wishes, and comorbidities,[9] as well as poor team climate[14] have all been reported to have negative impact on the team in MDMs. Correspondingly, the functional perspective of group decision-making posits that the internal factors coming from within the group (member composition, group size, interactions, culture, beliefs, attitudes, history among group members) and the external circumstances (time pressure, workload) both impact the way groups perform, with the group size and diversity being positively related to performance and range of abilities, and negatively related to effective processes and equality of participation.[15–16] This pattern is also evident in cancer MDMs.
More research is therefore needed to understand how the process of decision-making is currently structured in MDMs—whether this is at the service of promoting effective decision-making, and how it impacts team outcomes. For instance, evidence from MDMs shows that the chairing of the meeting tends to be led by one of the contributing disciplines, and predominantly by more senior surgical members of the team.[17] This, however, may not be an optimal set up. Evidence from cognitive psychology shows that the competition in dual-task performance (in the case of the MDM, chairing while contributing to case reviews) is detrimental to one or both tasks that are being undertaken simultaneously,[18] whereas evidence from patient safety and functional perspective shows that communication between healthcare professionals can be negatively affected by a steep authority gradient, which can emerge when a senior clinician chairs a MDM.[15,19–22] The latter finding is further supported by early social science research,[23–24] the results of which were subsequently used to improve team effectiveness in many industries, including aviation.[25]
1.2. Objectives
Our primary objectives were to examine the underlying structure of team decision-making during case reviews, investigating how the different elements of the decision process cluster together and to understand how it affects team outcome, that is, the team ability to reach a treatment decision/plan.
To achieve this, we conducted a series of analyses on a large multtumor database that was compiled using a novel validated instrument for the observational assessment of decision-making in cancer MDMs—namely, Metric for the Observation of Decision-Making in cancer MDTs, also known as, MDT-MODe.[4] Although tools have been developed to evaluate various aspects of MDM performance, to our knowledge, this is the only instrument designed specifically to measure the process of multidisciplinary decision-making.
2. Methods
2.1. Study design
This is a cross-sectional observational study that represents a secondary analysis of the data. Originally, the data were acquired through our center's ongoing research program in evaluating and improving MDT working across different tumors and was used to descriptively assess decision-making process within cancer teams using MDT-MODe. Since this was a secondary analysis, ethical approval was not required; however, at the time of data collection, ethical approvals were in place for all prospective evaluations.
2.2. Setting
The study recruited 4 independent cancer teams between 2010 and 2014 from 1 teaching university hospital (lung cancer team) and 3 large community hospitals (breast, colorectal, and urology cancer teams) of the London (UK) metropolitan area. Observations were conducted in real-time over 10 consecutive meetings within each MDT by 4 trained surgeon evaluators (breast = SA, colorectal = SMS, lung = SS, urological = BWL) who assessed the cancer team that corresponded to their clinical specialty. Reliability was assessed by having 4 surgeon evaluators score a subset of cases in pairs. The evaluators were not members of the MDT they were assessing.
2.3. Participants and study size
Participants were 4 multidisciplinary cancer teams with a total of 52 members, and an overall of 1045 individual case reviews discussed over a period of 10 weekly meetings respectively. Eligibility criteria for the study were defined as multidisciplinary cancer teams from the UK National Health Service (NHS) that represent 4 most common types of cancer (breast, lung urological and colorectal) and discuss patients referred to them for care planning recommendations. An availability sampling approach was used to identify teams that met eligibility criteria, whereas a set number of meetings within each team determined the number of case discussions for analysis.
2.4. Variables and measurements
Case reviews within each meeting and across all 4 cancer teams were assessed in the same manner by assessors who were clinicians specialized in the cancer they observed, and trained beforehand in the use of the MDT-MODe, a quantitative observational assessment tool (Fig. 1).[4] Training in the use of the tool is essential to be able to use it—this is a general principle for instruments assessing human factors in clinical environments, such that the evaluations produced have a degree of accuracy and can be meaningfully used.[29] The tool has been validated, and previously used to assess various cancer MDTs.[26–28] The instrument allows a trained evaluator (using the form shown in Fig. 1) to provide for each case review carried out by the MDT a standardized score on a 1 to 5 behaviorally anchored scale of the following variables in real-time:
Quality of information presented at the MDM as measured by 6 variables, namely, patient history, radiology results, pathology results, patient psychosocial aspects (i.e., psychological and social factors, including mental health difficulties, socioeconomic issues, and personal circumstances), comorbidity (i.e., medical history and performance status), and patients’ wishes or opinions regarding treatment.
Quality of multidisciplinary case review as measured by the contributions of 7 core disciplines, namely, chairperson, surgeon, oncologist, nurse, radiologist, histopathologist, and coordinator. Quality of MDT chairing is evaluated based on national guidelines for England,[13] which outline the core competencies that are important for chairing: meeting management, listening and communication, interpersonal relations, managing disruptive personalities and conflict, negotiations, facilitating effective consensual decision-making, and time management. Other MDT-members are rated on the basis of their clear contribution of their specialty to the case review.
Figure 1.
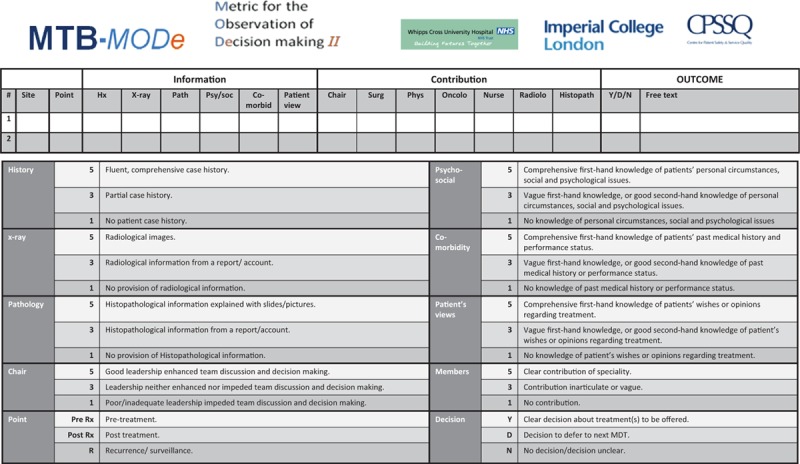
Metric for the observation of decision-making used to assess case discussions in cancer multidisciplinary team meetings.[4]
The outcome measure is a dichotomous variable (yes/no) that allows recording whether or not a clear treatment decision was reached for a patient (Fig. 1). In the statistical analysis, type of tumor was considered as a potential confounder. No other variables were included in the final model.
2.5. Bias
Efforts were made to address potential biases in the study. We addressed observer bias and had ensured reliability of evaluations on the MDT-MODe by having a subset of cases scored by the 4 clinical evaluators in pairs who were all trained and experienced in the use of the instrument. During data collection, each evaluator was blind to the other evaluators’ observations. All data were collated for analysis by a separate researcher (TS). We are aware that Hawthorne effect, that is, teams changing their usual behavior owing to being observed, is a natural limitation to observational studies, and in our study, MDT members were aware that they were being observed. In England, MDMs are commonly attended by visiting clinicians, students, researchers, clinical auditors as well as interns and residents on rotation. This means that in practice being “observed” in some way or other is rather common within these teams—and hence the presence of our study's clinical observers would not be overwhelming to the teams. We therefore believe that the presence of the observer, discreetly positioned at the back of the MDT meeting, would have had minimal impact on the proceedings of the meetings, particularly as the study occurred over a number of weeks (and thus allowed for acclimatization of the teams to the observers), and the evaluators were clinicians (specialized in the cancer that they observed), the presence of whom within the MDT is natural. We return to the Hawthorne effect issue in the discussion.
2.6. Statistical methods
Intra-class coefficient (ICC) analysis was initially used to assess reliability of evaluations. ICCs can range between 0 and 1, with higher values indicating better agreement between evaluators. A recent expert consensus has defined a reliability coefficient of 0.70 as a minimum value for data to be used for research purposes.[29]
Exploratory factor analysis (EFA) and logistic regression were subsequently carried out to assess the underlying structure of decision-making process during case reviews. The variables that were included in the EFA were individual items of information and specialist contribution quality as assessed by MDT-MODe. EFA extracted factors (using a regression method) were then entered in a multiple logistic regression model as predictor variables to assess their relation to the outcome, that is, team ability to reach a decision with 0 denoting no decision reached, and 1 decision reached. Variable representing individual teams within the sample (i.e., breast, lung, urology, and colorectal cancer teams) was also entered in the regression model as a covariate to examine its’ potential confounding effect. Significance was set at P < 0.05.
All analyses were carried out using SPSS® version 20.0 software (SPSS Inc, Chicago, IL), and there were no missing data.
3. Results
3.1. Descriptive analysis
The descriptive data for meeting characteristics are shown in Table 1. Representing the most common cancers in the UK, the sample consisted of overall 1045 case discussions across 4 teams within a NHS setting. The composition of health care personnel in MDTs did not significantly vary across groups. All teams consisted of a coordinator (administrator), chair and senior (Consultant/Attending level) cancer specialists, that is, surgeons, oncologists, radiologists, pathologists, and cancer nurses, with the exception of lung, wherein a chest physician was also present. Table 2 shows detailed descriptive data for the MDT-MODe variables across all 4 cancer teams.
Table 1.
Descriptive data of multidisciplinary team meetings observed.

Table 2.
Descriptive data of the scores on the MDT-MODe across cancer teams.

3.2. Reliability of evaluations: ICCs
Interevaluator agreement was assessed via ICCs on a randomly selected subset of the observed cases (N = 273, 26% of the total cohort). High reliability was obtained across all tumors: breast ( median ICC = 0.92 [range 0.27–1.00]); colorectal (median ICC = 0.83 [range 0.69–0.96]); lung (median ICC = 0.86 [range 0.71–0.99]); and urological (median ICC = 0.71 [range 0.31–0.87]). This finding means that all 4 surgeon evaluators were consistent in their use of the MDT-MODe instrument across evaluated cases. The full intrarater reliability matrix for all individual items across all 4 cancer teams is provided as the Supplementary data table.
3.3. Anatomy of decision-making: EFA
To assess the underlying structure of the decision-making process in MDM, an EFA was applied to the 13 MDT-MODe items. All the criteria for factor analysis were met—sample size was adequate (KMO = 0.67), and the variables sufficiently intercorrelated, (X2(78) = 3329.18, P < 0.001), with none of the coefficients being particularly large or zero. Based on Kaiser criterion (eigen values for the first 6 factors were 2.99, 2.11, 1.34, 1.19, 0.95, 0.89), Scree plot, and clinical considerations, 4 factors were extracted and rotated to simple structure via the oblique Promax algorithm with the Kappa parameter set to 4. Oblique rotation was chosen because it is considered a more accurate, reproducible solution, allowing the factors to correlate.[30] The 4 factors together explained 59% of the variance in the 13 MDT-MODe items. All items were well represented in the extracted 4 factors, with an average communality of 0.59. The best represented items were radiologists’ input, h2 = 0.84, pathologists’ input, h2 = 0.83, radiological information, h2 = 0.83, and pathological information, h2 = 0.84, whereas the least well-represented item was chair's input h2 = 0.39.
Table 3 presents the resulting factor pattern matrix. The highest-loading variables on the first factor were patient views on the treatment options (0.70), oncologists’ input into case discussion (0.67), nurses’ input into case discussion (0.65), and patient psychosocial aspects (0.60). Accordingly, this factor was labeled “Holistic and Clinical inputs,” representing patients’ holistic and clinical needs. The highest-loading variables on the second factor were patient radiological information presented to the team (0.91) and radiologists’ input into case discussion (0.93). Accordingly, this factor was labeled ‘Radiology’, representing radiological profile of patients’ disease. The highest-loading variables on the third factor were patient pathological information presented to the team (0.90) and pathologists’ input into case discussion (0.96). Accordingly, this factor was labeled “Pathology,” representing pathological profile of patients’ disease. The highest-loading variables on the fourth factor were coordinator's (0.68) and meeting chair's (0.61) inputs into case discussion. Accordingly, this factor was labeled “Meeting Management,” representing the management of case discussions within the meeting (chair), and general management and organization of cases for discussion (coordinator). Figure 2 shows a graphical representation of the 4-factor model.
Table 3.
Rotated factor loadings based on exploratory factor analysis of 13 items of the MDT-MODe.
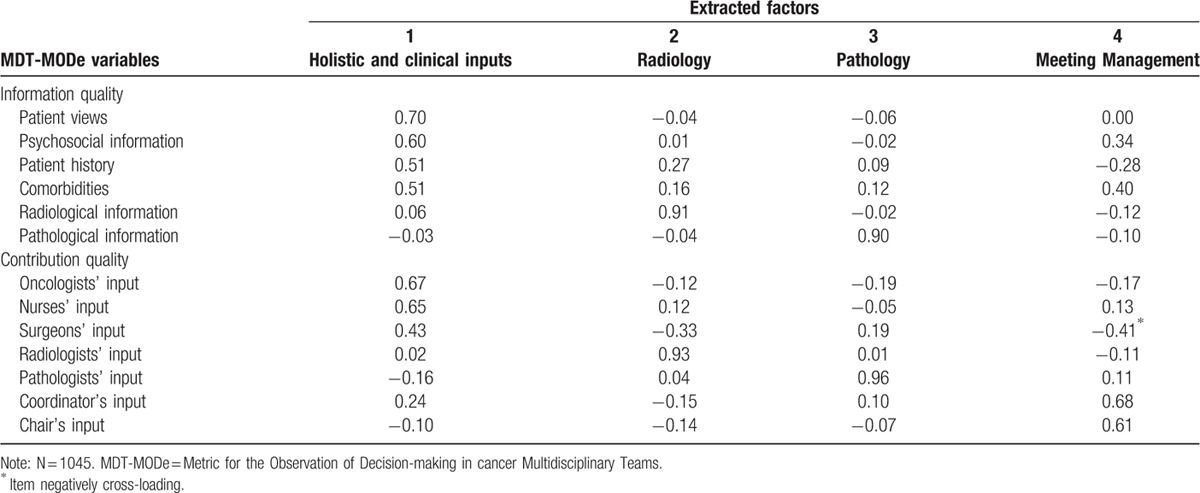
Figure 2.

Diagram depicting the underlying components of decision-making processes in cancer multidisciplinary team meetings.
As evident from Table 3, 1 variable, namely, surgeons’ input, cross-loads positively (0.43) on “Holistic and Clinical inputs, ” and negatively (−0.41) on “Meeting Management.” Since surgeons in our sample also chaired the meetings, thus undertaking 2 tasks simultaneously, we further explored the relationship between the 2 using Spearman correlational analysis. A significant negative association was found between surgeons’ and chairs’ inputs to case reviews (r = −0.19, P < 0.01), indicating that as the surgeons’ inputs increased, the chairs’ inputs decreased. In contrast, the relationship between surgeons’ and coordinators’ inputs was nonsignificant (r = −0.04, P > 0.05). It is reasonable to conclude, therefore, that the negative cross-loading in the EFA is driven by the negative surgeon–chair association. This finding is in line with the theory of dual task interference,[18] as discussed later.
Factor inter-correlations were generally low at r = 0.26 or less. The full factor inter-correlation matrix is available upon request from the corresponding author.
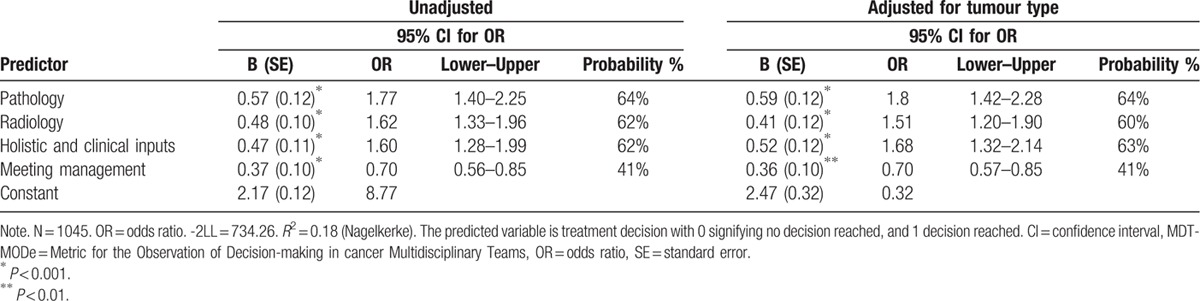
3.4. Predictors of outcome: logistic regression
To explore the relation between the 4 factors and the outcome variable, namely, the team ability to reach a treatment decision on first case review, we performed a multiple logistic regression analysis. After adjusting for tumor type, all 4 factors, including “Holistic and Clinical inputs” (Wald(1) = 17.88, P < 0.001), “Radiology” (Wald(1) = 12.01, P < 0.001), “Pathology” (Wald(1) = 23.22, P < 0.001), and “Meeting Management” (Wald(1) = 12.30, P < 0.001) were significantly related to the treatment decision. To facilitate interpretation, we converted the odds ratios into probability percentages, using the following formula: odds/(odds + 1) × 100 = probability %.[31] We found that “Holistic and Clinical” inputs, “Radiology,” and “Pathology” contributed the most to the probability of the team to reach a treatment decision for a patient (Table 4).
Table 4.
Logistic regression predicting treatment decision from the extracted factors of the MDT-MODe.
4. Discussion
4.1. Summary
The current study used multivariate statistical methods to gain a better understanding of the anatomy of group decision-making in cancer MDMs, and how it relates to team ability to reach treatment recommendation. We showed that the decision-making process in cancer MDMs is driven by 4 underlying factors—namely, “Holistic and Clinical inputs,” “Pathology,” “Radiology,” and “Meeting Management.” These were all significantly predictive of team ability to reach a treatment decision on first case review. The inputs of chairs (who were surgeons in our sample) were shown to compete with their corresponding disciplinary contributions to case reviews at the detriment of the meeting management—that is, as surgeons’ input to case reviews increased, chair's input decreased.
4.2. Limitations
We have used observational data with participants being aware that they were being evaluated; hence, we cannot rule out observer biases and the Hawthorne effect. This is a natural limitation to all observational evaluations, and in our dataset, we used blinded clinical evaluators (the presence of whom within a MDT is natural) and a previously validated tool, ensuring satisfactory inter-assessor reliability. Further, the nature of MDT-MODe may not do justice to the complex roles of the MDT chairperson and coordinator. This is being addressed via a more detailed evaluation scale we are currently constructing for chairing skills.[33] Although we have made an attempt to control for the confounding effects of tumor type, we acknowledge that our data are derived from different institutions and MDTs, and that team culture including different values, beliefs. and attitudes could influence outcomes[16]. This may have affected institutional versus team-specific or tumor-specific factors impacting on team decision-making. In a similar vein, conscious or unconscious preferences for treatment may be embedded into individual specialists’ decision-making; ideally, these should also be factored into the decision-making “model” of the MDM as they are likely to be a stable feature of each individual physician's decision style. Our study was not designed to address all of these complexities, which would have rendered its scope unfeasible. Future work should therefore explore a large stratified sample of cases across hospitals and tumors to further validate our findings, and also the intraindividual physician preferences for treatment options. Such research would offer further understanding of how these differences affect multidisciplinary decision-making process.
4.3. Overall interpretation
Previous research has shown that clinical decision-making process is an essential part of effective MDT working.[13] Our findings build on this by showing that the decision-making process in MDMs is driven by 4 underlying factors representing all core disciplines and the complete patient profile—both essential for the teams’ ability to reach a decision. In a recent study, MDT members reported the importance of member attendance, availability of patient information, considerations of patient comorbidities, patient choices, and their current state of health for decision-making.[9] Our article corroborates this finding by showing that in order for the team to be able to reach a treatment recommendation on first case review, all participating disciplines and the complete patient profile are necessary. This is also in line with the functional perspective of group decision-making, which links the diversity of groups with better performance and range of abilities, although at the expense of effective processes and equality of participation[15]—a pattern previously observed in MDMs.[4–6] Quality improvement efforts, therefore, could consider focusing on the factors identified by our study, and assessing them against team processes (e.g., social loafing, blocking, shared information bias), quality of decisions made, and patient satisfaction.
Moreover, our finding of negative surgeon-chair's input association whereby the surgeons’ inputs into case review increase as the chairs’ inputs decrease, is in line with the theory of dual task interference, which shows that the competition in dual-task performance is at the detriment of one or both tasks.[18] In our sample, chairing was led by the surgical specialty that is also required to provide input into case reviews; these are both demanding cognitive tasks. Our study shows that providing both types of input at the same time appears to be at the expense of the coordination of the meeting. More specifically, when surgical input into case reviews increases, the chair's input decreases. This is an important finding because such internal factors emanating from within the group can affect the way the team performs.[15] What is more, this finding can spur strategies for improving MDM practice. For instance, assigning a chairing role to a clinically noncontributing individual (e.g., MDT leads from other specialties, or cancer managers), trained in team management skills may allow the contributing members to focus solely on case reviews and clinical decision-making. Alternatively, rotating the chairing duty during a MDM could allow different team members to chair when their direct input is not required. Also, experienced specialist nurses could potentially take on this role.[32]
4.4. Further research
One question that was directly raised by our findings relates to chairing and dual-task interference. Studies should look specifically into the impact of having one of the contributing disciplines in the MDT chair the meeting, and test alternative options for meeting leadership that address the burden of the chairing task to the clinical decision-making. A second question for future research to address relates to the effects of authority gradients on team decision-making process. Authority gradients were first defined in aviation where it was observed that differences in seniority and authority impede effective communication between pilots and co-pilots,[22] and the concept was subsequently introduced to medicine in the Institute of Medicine Report, To Err Is Human.[21] Although dual-task interference is a valid and tested theory that should be investigated further within MDMs, one cannot ignore that meetings are attended by >1 person from each specialty. This begs the question as to what is the effect of the chair's authority gradient on information exchange and contributions to case reviews from other members of the chair's discipline. Additionally, this effect should also be explored in relation to the other disciplines within the team since nurses, for example, have traditionally lower team status. The negative impact of authority gradients on communication between healthcare professionals and on patient safety has been well-documented,[15,19–22] and classic social science research had showed the detrimental effects of blind obedience that such gradients can create.[23–24] To illustrate, in a recent interview with MDT members regarding the effectiveness of their meetings, 1 doctor reported: “I am always amazed how very able staff can be so passive”[14]. Having an effectively trained leader and a respectful team climate that balance out the authority gradients and encourages inputs from all contributing members and disciplines may help improve the decision-making process and guard against potential team biases.
4.5. Generalizability
Although this is a large-scale study for its nature (based on in-vivo observations), generalizability of our findings may be limited to the most common cancer MDTs within the NHS. Replication and assessment of the generalizability of the current findings to other cancer MDTs, in particular the lower-frequency cancers, needs to be examined to determine the extent of which they apply to them.
5. Conclusion
As our results demonstrate for the first time, MDT decisions in most common cancers are driven by 4 underlying factors encompassing all participating disciplines and a complete patient profile. It seems that all of these elements are necessary for the collective decision-making ability of a team. We also demonstrated a negative relationship between chairs’ inputs and their corresponding disciplinary clinical input, possibly indicating dual-task interference. Further research could profitably investigate how chairing and authority gradients affect team interactions and contributions to case review in MDMs with a view to improving service quality and group decision-making in a natural context.
Acknowledgments
The authors thank all participating MDTs and their members for their time and commitment.
Footnotes
Abbreviations: MDM = Multidisciplinary team meeting, MDT = Multidisciplinary team, MDT-MODe = Metric for the Observation of Decision-making in cancer Multidisciplinary Teams, MTB = Multidisciplinary tumor board.
Authorship: NS is the Director of London Safety & Training Solutions Ltd, which provides team skills training and advice on a consultancy basis in hospitals and training programs in the UK and internationally.
Funding: Financial support for this study was provided entirely by the UK's National Institute for Health Research (NIHR) via the Imperial Patient Safety Translational Research Centre. Sevdalis's research is funded by the NIHR via the ‘Collaboration for Leadership in Applied Health Research and Care South London’ at King's College Hospital NHS Foundation Trust, London, UK. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. Sevdalis is also a member of King's Improvement Science, which is part of the NIHR CLAHRC South London and comprises a specialist team of improvement scientists and senior researchers based at King's College London. Its work is funded by King's Health Partners (Guy's and St Thomas’ NHS Foundation Trust, King's College Hospital NHS Foundation Trust, King's College London and South London and Maudsley NHS Foundation Trust), Guy's and St Thomas’ Charity, the Maudsley Charity and the Health Foundation. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
The authors report no conflicts of interest.
References
- [1].The Department of Health. Manual for cancer services. London, UK: The Department of Health; 2004. [Google Scholar]
- [2].Hong NJ, Wright EF, Gagliardi AR, Paszat LF. Examining the potential relationship between multidisciplinary cancer care and patient survival: an international literature review. J Surg Oncol 2010;1022:125–34. [DOI] [PubMed] [Google Scholar]
- [3].The Department of Health. National peer review report: Cancer services 2012/2013. London, UK: The Department of Health; 2013. [Google Scholar]
- [4].Lamb BW, Wong HWL, Vincent C, et al. Teamwork and team performance in multidisciplinary cancer teams: development of an observational assessment tool. BMJ Qual Saf 2013;20:849–56. [DOI] [PubMed] [Google Scholar]
- [5].Lamb BW, Green JSA, Benn J, et al. Improving decision-making in multidisciplinary tumor boards: prospective longitudinal evaluation of multicomponent intervention for 1,421 patients. J Am Coll Surg 2013;2173:412–20. [DOI] [PubMed] [Google Scholar]
- [6].Lamb BW, Sevdalis N, Benn J, et al. Multidisciplinary cancer team meeting structure and treatment decisions: a prospective correlational study. Ann Surg Oncol 2013;20:715–22. [DOI] [PubMed] [Google Scholar]
- [7].The Department of Health. Cancer patient experience survey 2011/2012- national report. London, UK: The Department of Health; 2012. [Google Scholar]
- [8].Institute of Medicine. Cancer care for the whole patient: meeting psychosocial health needs. Washington DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- [9].Jalil R, Ahmed M, Green JSA, et al. Factors that can make an impact on decision-making and decision implementation in cancer multidisciplinary teams: An interview study of the provider perspective. Int J Surg 2013;11:389–94. [DOI] [PubMed] [Google Scholar]
- [10].Mistry M, Parkin DM, Ahmad AS, et al. Cancer incidence in the UK: projections to the year 2030. Br J Cancer 2011;105:1795–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].World Health Organisation. World cancer report 2014: International Agency for Research on Cancer. France: World Health Organisation; 2014. [Google Scholar]
- [12].NHS England. Everyone counts: planning for patients 2014/2015 to 2018/2019. NHS England; 2014. [Google Scholar]
- [13].National Cancer Action Team. The characteristics of an effective multidisciplinary team (MDT). London, UK: National Cancer Action Team; 2010. [Google Scholar]
- [14].Raine R, Xanthopoulou P, Wallace I, et al. Determinants of treatment plan implementation in multidisciplinary team meetings for patients with chronic diseases: a mixed-methods study. BMJ Qual Saf 2014;doi:10.1136/bmjqs-2014–002818 [published Online First: 09 June 2014]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Poole MS, Hollingshead AB. Theories of small groups: interdisciplinary perspectives. London, UK: Sage Publications Ltd; 2005. [Google Scholar]
- [16].Hall P. Interprofessional teamwork: Professional cultures as barriers. J Interprof Care 2009;19:188–96. [DOI] [PubMed] [Google Scholar]
- [17].Lamb BW, Brown K, Nagpal K, et al. Quality of care management decisions by multidisciplinary cancer teams: a systematic review. Ann Surg Oncol 2011;18:2116–25. [DOI] [PubMed] [Google Scholar]
- [18].Kanheman D. Attention and effort. Englewood Cliffs, NJ: Prentice-Hall; 1973. [Google Scholar]
- [19].Vincent C. Patient safety. Oxford, UK: Wiley-Blackwell, BMJ Books; 2010. [DOI] [PubMed] [Google Scholar]
- [20].Francis R. Freedom to speak up. UK: Quality Commission; 2015. [Google Scholar]
- [21].Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Institute of Medicine Report. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- [22].Cosby KS, Croskerry P. Profiles in patient safety: authority gradients in medical error. Acad Emerg Med 2004;1112:1341–5. [DOI] [PubMed] [Google Scholar]
- [23].Ash SE. Guetzkow H. Effects of group pressure upon the modification and distortion of judgment. Groups, Leadership and Men. Pittsburgh: Carnegie Press; 1951. 177–90. [Google Scholar]
- [24].Milgram S. Behavioural study of obedience. J Abnorm Soc Psych 1963;67:371–8. [DOI] [PubMed] [Google Scholar]
- [25].Helmereich RL. On error management: lessens from aviation. BMJ 2000;320:781–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Gandamihardja T, McInerney S, Soukup T, et al. Improving team working within a breast MDT: An observational approach. Eur J Surg Oncol 2014;405:604. [Google Scholar]
- [27].Jalil R, Akhter W, Lamb BW, et al. Validation of team performance assessment of multidisciplinary tumor boards. J Urol 2014;1923:891–8. [DOI] [PubMed] [Google Scholar]
- [28].Lamb BW, Green JS, Benn J, et al. Improving decision making in multidisciplinary tumor boards: Prospective longitudinal evaluation of a multicomponent intervention for 1,421 patients. J Am Coll Surg 2013;2173:412–20. [DOI] [PubMed] [Google Scholar]
- [29].Hull L, Arora S, Symons NR, et al. Delphi expert consensus panel. Training faculty in nontechnical skill assessment: national guidelines on program requirements. Ann Surg 2013;2582:370–5. [DOI] [PubMed] [Google Scholar]
- [30].Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract Assess Res Eval 2005;10: [Google Scholar]
- [31].Grimes DA, Schulz KF. Making sense of odds and odds ratios. Obstet Gynecol 2008;1112:423–6. [DOI] [PubMed] [Google Scholar]
- [32].McGlynn B, White L, Smith K, et al. A service evaluation describing a nurse-led prostate cancer service in NHS, Ayrshire and Arran. Int J of Urol Nurs 2014;83:166–80. [Google Scholar]
- [33].Jalil R, Akhter W, Sevdalis N, et al. Chairing and leadership in cancer MDTs: Development and evaluation of an assessment tool. Euro Urol 2013;126:132–3. [Google Scholar]


