Abstract
Endoscopic submucosal dissection (ESD) has been accepted as a minimal invasive alternative to surgery for localized superficial gastrointestinal neoplasms recently. However, the procedure remains to be technically challenging and time consuming. A new dissecting knife with partially insulated tip has been recently developed with built-in injection capability. The purpose of this study was to investigate whether the efficiency of ESD procedure could be improved with this new device.
A total of 78 patients, who underwent ESD with gastric mucosal lesions including flat type polyps, adenoma or early gastric cancer, were randomly assigned to either ESD with O-type HybridKnife or conventional ESD knives without waterjet. Procedure time and related factors of ESD were analyzed.
ESD procedure time was 43.0 (interquartile range, IQR 27.0–60.0) minutes in HybridKnife group compared to 60.5 (IQR 44.0–86.3) minutes in the control group (P = 0.001). There was no difference in the clinical outcome and the adverse event rate. The former demonstrated more favorable results in lesions ≤4 cm of specimen size (P ≤ 0.0001) and when located in the distal stomach (P = 0.001), also in lesions with fibrosis (P = 0.008). Multivariate regression analysis showed that O-type Knife (P ≤ 0.0001), specimen size (P ≤ 0.0001), and fibrosis (P ≤ 0.0001) were independent predictors of procedure time.
The O-type HybridKnife yielded faster procedure time compared to the conventional knives in gastric ESD with a similar safety profile.
INTRODUCTION
Endoscopic submucosal dissection (ESD) has gained acceptance as the first line treatment option not only in East Asia including China, Japan and Korea, but also worldwide.1–4 Although clinical long-term outcome showed excellent results,5 ESD remains to be a technically challenging and time consuming procedure compared to other endoscopic resection methods including endoscopic mucosal resection (EMR).6,7 Modifications on devices and methods of ESD have been attempted. The HybridKnife, a new system which combines electrosurgical technology with a water-jet system (ERBEJET2; ERBE, Tübingen, Germany), allows rapidly injection of solutions into the submucosa to form a fluid cushion without exchanging instruments. It has been previously shown to be effective and safe in animal studies and clinical trials.8–11 Recently, a new type of HybridKnife (O-type HybridKnife, Figure 1) was developed with a partially insulated tip. However, little was known if the built-in injection capability would help to reduce ESD procedure time. In the present study, we conducted a randomized, controlled prospective study to evaluate the efficiency of O-type HybridKnife in gastric mucosal lesions compared to conventional ESD knives.
FIGURE 1.
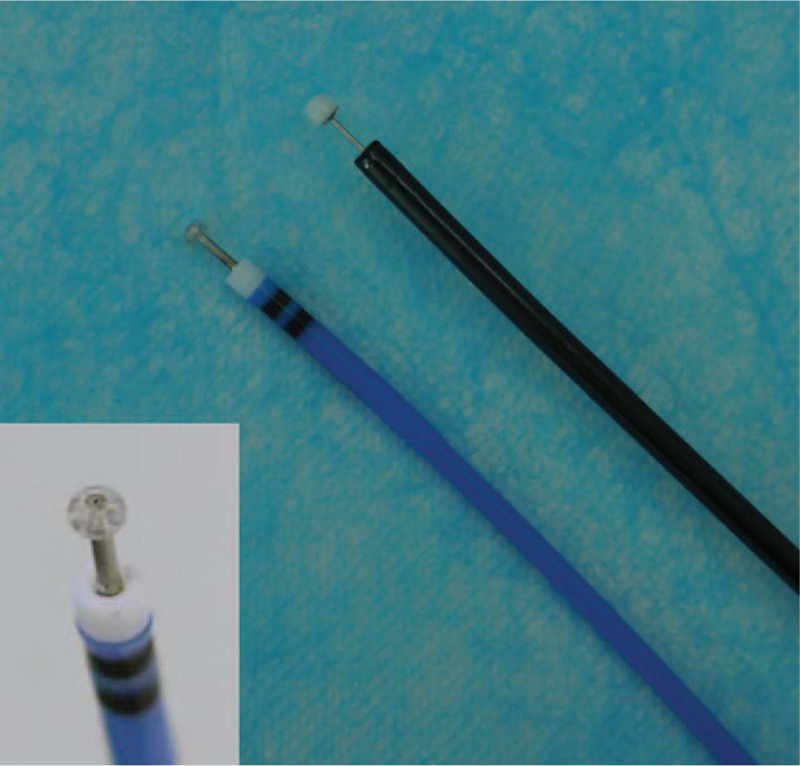
O-type HybridKnife. The larger figure demonstrates the side-by-side comparison of O-type HybridKnife to IT2 knife while the smaller insert highlights the tip of the HybridKnife, a circular insulated tip except for the center where the metal needle tip for injection went through. Marking, injection, mucosal cutting, submucosal dissection, and hemostasis can be performed with 1 device.
METHODS
Patients
From January 2013 to September 2014, 78 consecutive patients with eligible gastric lesions were recruited at Xijing Hospital of Digestive Diseases (Xi’an, China). The inclusion criteria for ESD were: 18 to 80 years of age; gastric flat type adenoma/polyps, biopsy confirmed early differentiated adenocarcinoma and high-grade intraepithelial neoplasia (HGIN) which were eligible for conventional ESD indications,12 or suspected localized mucosal lesions detected by endoscopy; tumor invasion within the mucosa or minute submucosal layers by endoscopic ultrasonography and computerized tomography; only parameters from the largest lesion would be taken into analysis if multiple lesions were removed. The exclusion criteria were: recent drug history of anticoagulant or antiplatelet agent within 7 days before operation; recurrent gastric cancer after endoscopic or surgical treatment; pregnant or breast-feeding patients. The study was approved by the institutional review board of our hospital and registered at Clinicaltrials.org (No. NCT01760070). All patients provided written informed consent. All coauthors had access to the study data and had reviewed and approved the final manuscript. According to our pilot data on procedure time (HybridKnife vs IT knife: 28.08 ± 14.05 min vs 40.50 ± 16.86 min),13 74 cases would be needed for each group at a power of 0.95 with a significance level (alpha) of 0.05 using an 1-sided 2-sample t test (Pass 11, Kaysville, UT). Therefore an estimation of 39 cases in each group would be enrolled to ensure the comparability. The patients who met the inclusion criteria and did not have any of the exclusion criteria were randomly allocated 1:1 to either the IT knife group or the HybridKnife group. A single study coordinator performed a simple fixed-allocation randomization process by using a table of random numbers.
ESD Procedures
Patients were sedated and intubated. ESD procedures were performed by a single endoscopist (Z.G. Liu) with experience of more than 100 cases on both HybridKnife (ERBE) and insulation-tipped diathermic knife (IT2 knife, Olympus Optical Co, Ltd, Tokyo, Japan), using a single-channel endoscope (GIF-Q260J; Olympus Optical Co). The IT2 knife was used in the control group since it was the most commonly used dissecting knife in ESD procedure and shared similar design with the HybridKnife. The O-type HybridKnife contains an insulated tip except for the center where the metal needle tip for injection went through (Figure 1). The procedure involved marking, injection, circumferential cutting, submucosal dissection, and hemostasis. A saline solution containing epinephrine (0.01 mg/ml) and minimal indigo carmine was used in both the HybridKnife group and the IT knife group. Circumferential cutting was made in the mucosa by using the Dual-Knife (KD-650L/Q, Olympus Optical Co) combined with either IT2 knife in IT knife group or O-type HybridKnife in the HybridKnife group. The submucosal layer was dissected mainly with either the IT knife or the O-type HybridKnife. Fibrosis was defined as the appearance of a white muscular structure without a blue transparent layer in the submucosal layer as previously reported.14 The Dual-Knife was used as assistance when submucosal fibrosis was severe. Endoscopic hemostasis was performed either with the dissecting knife or the hemostatic forceps (FD-410LR; Olympus Optical Co). After dissection, preventive endoscopic hemostasis was performed for any oozing or exposed vessel. The VIO generator (VIO 200D; ERBE) was used for all ESD procedures.
Procedure time was defined as the time from marking of the lesion till complete removal of the specimen including hemostasis and other adverse event management. The submucosal dissection time was defined from completion of circumferential cutting till complete removal of the specimen excluding hemostasis and adverse event management. Nonsubmucosal dissection time was defined as total procedure time minus submucosal dissection time. Intra- and postoperative adverse events including abdominal pain, pneumonia, perforation, and bleeding were recorded. Patients were then carefully monitored for 3 days in hospital, oral food taking resumed at 24-hour postprocedure except for perforation cases, follow-up endoscopy was scheduled in 1 month after procedure. Delayed adverse events were also recorded at 1 month follow-up or when occurred.
Histological Analysis
The curability of ESD specimens was carefully evaluated histologically. Specimen slices at 2-mm intervals were investigated as described in detail elsewhere.12 R0 resection was defined as lesions in which en bloc removal was achieved with tumor-free lateral and vertical margins. Curative resection was considered if R0 resection was achieved with no lymphovascular infiltration and vertical submucosal invasion <500 μM.
Statistics
Quantitative variables were summarized by either the mean ± standard deviation (SD) for normally distributed data or the median and interquartile range (IQR) for skewed distribution. A preliminary univariate analysis was performed by using Chi-square test for comparison of categorical variables including gender, comorbidity, and histological diagnosis. The Student t test was used for continuous and normally distributed variables such as age. The Mann–Whitney U test was used to compare medians such as procedure time and lesion size if data were not normally distributed. Factors with a significant difference as determined by univariate analysis were included in the multivariate analysis by using a linear regression model. The natural (base e) logarithm of procedure time was used in regression due to the skewed distribution indicated by Shapiro–Wilk test. A P-value of <0.05 in each analysis was considered statistically significant. All statistical analyses were performed by using SPSS software, version 19.0 (SPSS, Inc., Chicago, IL).
RESULTS
Overall Clinical Outcomes
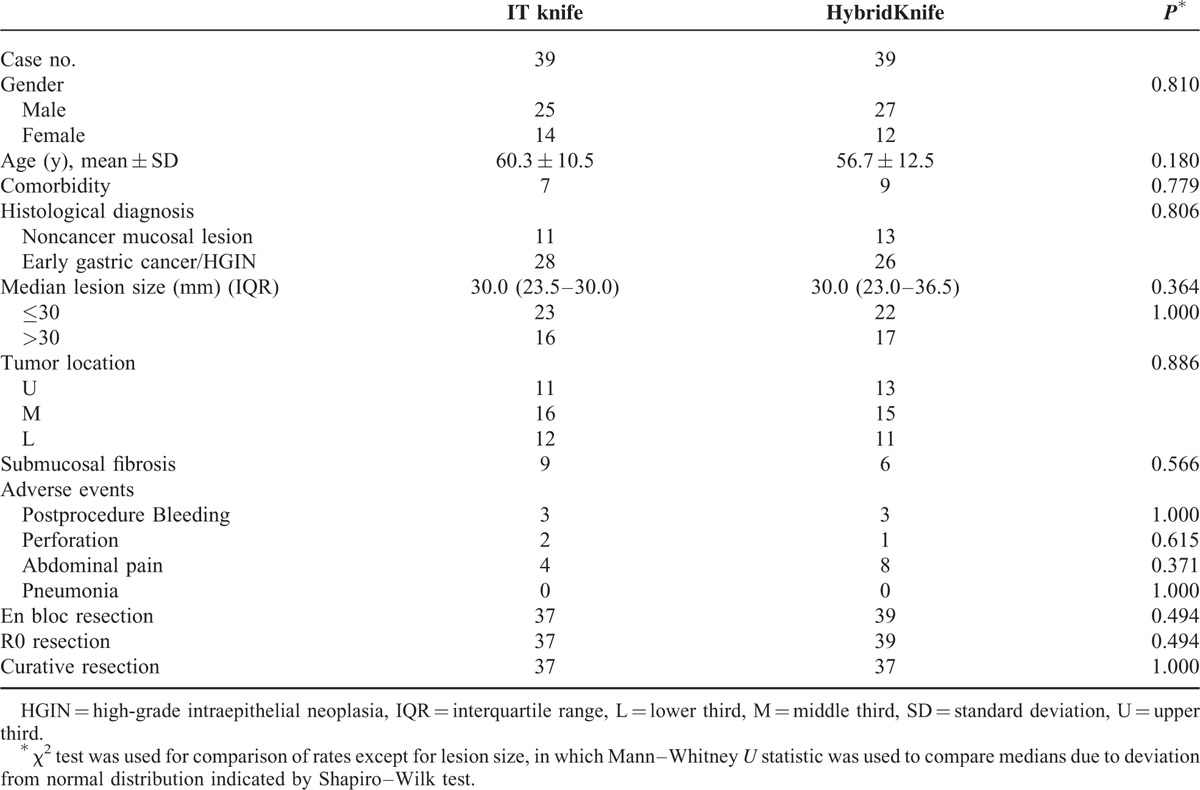
Between January 2013 and September 2014, 78 gastric ESDs were performed. Primary indications for ESD were early cancer and HGIN confirmed by biopsy (n = 40), suspected cancer lesion (n = 25), and gastric adenoma or flat type polyps (n = 13) (Figure 2). The mean (±SD) patient age was 58.5 ± 11.7 years old and 66.7% were male. Seventy-seven procedures were completed. Massive intraoperation bleeding occurred during ESD procedure in 1 patient. In this case the endoscopic procedure was stopped and conversion to open surgery was performed. The en bloc resection and R0 resection were achieved in 76 patients. Illustrative example of performing ESD by using HybridKnife is shown in Figure 3. Piecemeal resection was conducted in one case due to severe fibrosis of submucosal layer. ESD related adverse events were abdominal pain (n = 12), perforation (n = 3), and postprocedure bleeding (n = 6). The abdominal pain was usually mild and resolved within 48 hours after the procedure. Perforations were closed by metallic clips. Postprocedure bleeding and/or melena were noticed in 4 patients. Decreased hemoglobin concentration by more than 2 g/dL was observed in 2 more patients and emergent endoscopic hemostasis was carried out in 3 of these patients. All patients with postprocedure bleeding were safely managed by conservative treatments. Deep submucosal invasion was confirmed by pathology in two cases, therefore consecutive open surgical treatment was performed in these 2 patients. There was no difference between IT knife group and HybridKnife group on clinical outcomes and adverse event rates. Baseline characteristics and procedure outcomes are summarized in Table 1.
FIGURE 2.
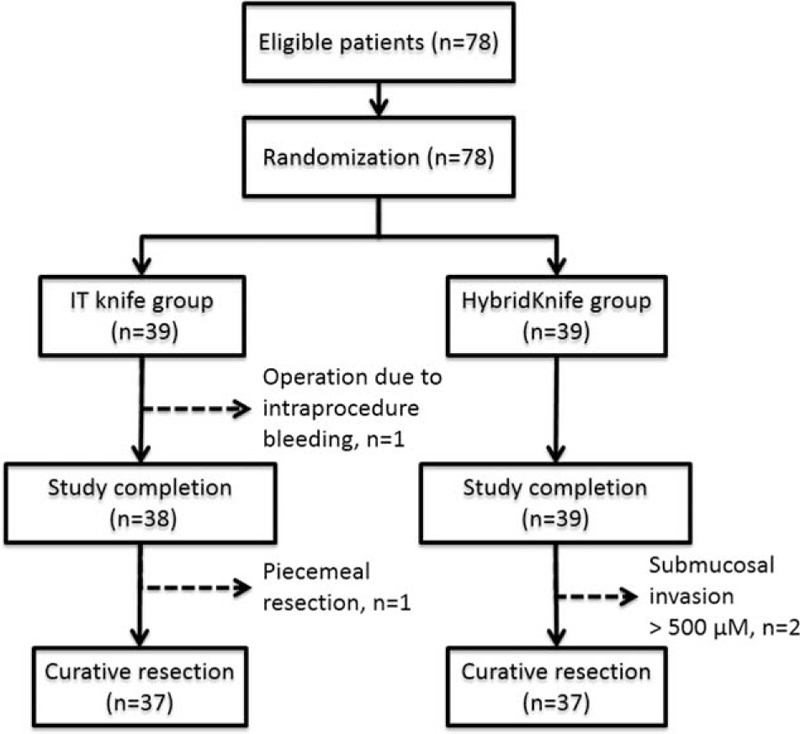
Flow chart of endoscopic submucosal dissection procedure time comparison. N, number of patients.
FIGURE 3.
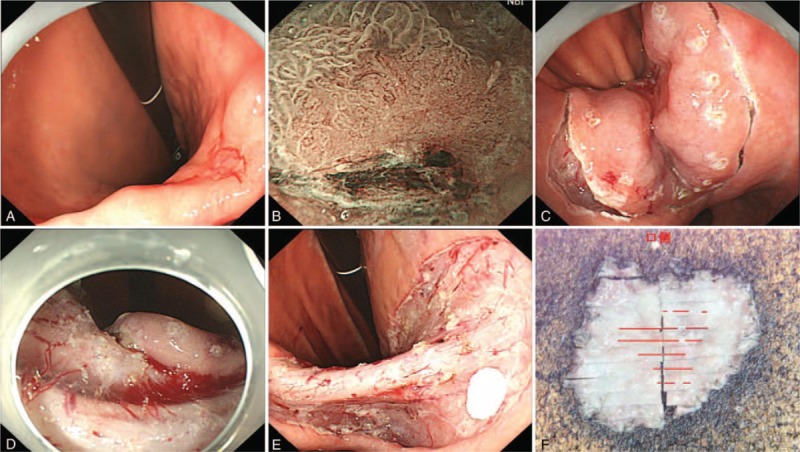
A representative ESD case treated with O-type HybridKnife. A superficial IIc + IIa type lesion located at the incisura angularis of stomach (A), surface and vascular changes and demarcation line could be visualized clearly by narrow band imaging (NBI) (B). After marking, circumferential cutting was made using the HybridKnife (C). The submucosa was dissected with a satisfactory fluid cushion (D), leaving a clean mucosal defect with supplying vessels close to muscularis propria intact (E). Histological analysis of resected specimen revealed a moderately differentiated intramucosal adenocarcinoma with clean lateral and vertical margins (F).
TABLE 1.
Baseline Characteristics and Procedure Outcomes of Patients
Difference in ESD Procedure Time According to Clinicopathological Factors
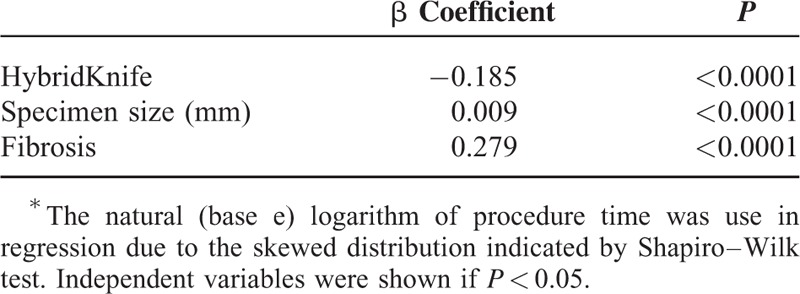
The procedure time showed a skewed distribution (P ≤ 0.0001) and thus medians and IQR were showed instead of means. The ESD procedure time was 43.0 (27.0–60.0) minutes in the HybridKnife group compared to 60.5 (44.0–86.3) minutes in control group (P = 0.001) (Table 2). The procedure of the HybridKnife was more efficient in comparison to the conventional ESD in lesions ≤4 cm of specimen size (P ≤ 0.0001) as well as if the surgical site is located at the distal stomach (P = 0.001), with either fibrosis or not (P = 0.008 and 0.017), and a histological diagnosis of cancer (P = 0.006) indicated by univariate analysis. When procedure time was further subdivided into submucosal dissection time and nonsubmucosal dissection time, both parameters showed a decrease over control (P = 0.003 and 0.005). Multivariate regression analysis with factors proven to be significant in univariate analysis showed that HybridKnife (P ≤ 0.0001), specimen size (P ≤ 0.0001), and fibrosis (P ≤ 0.0001) were independent predictors of procedure time (Table 3). Adjusted R-square value of the factors was 0.477.
TABLE 2.
Univariate Analysis of Factor Related With Procedure Time
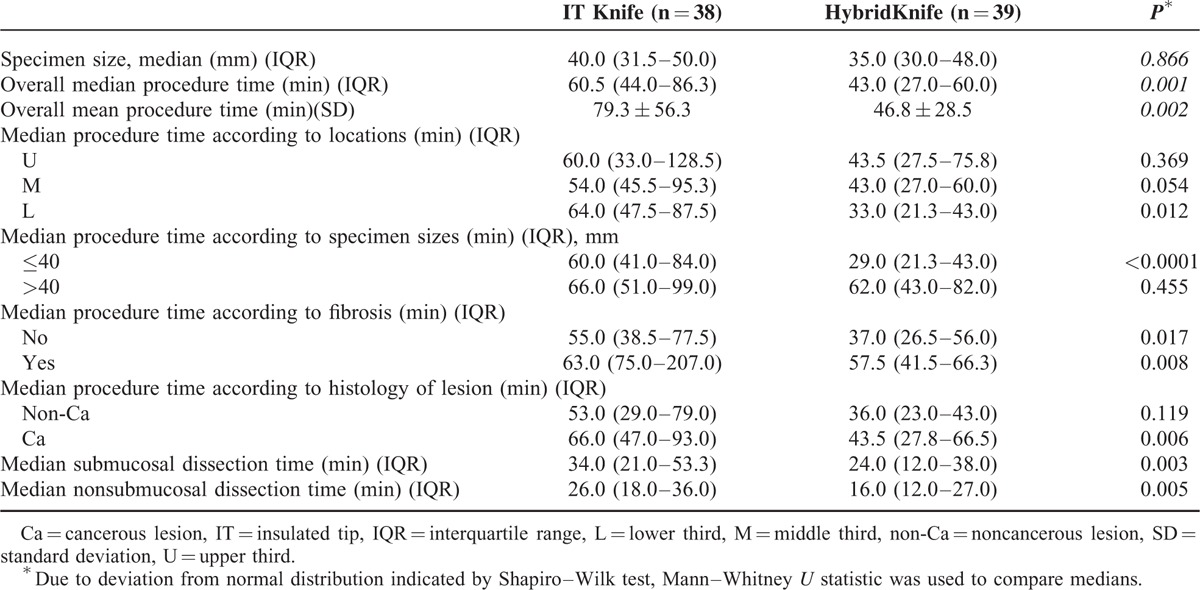
TABLE 3.
Linear Regression Model of Risk Factors of Log Procedure Time∗
DISCUSSION
With the development of endoscopic screening and surveillance, the detection rate is steadily increasing for early gastric lesions including precancerous lesions and early cancer. ESD has emerged to be one of the first-line treatment options because of its minimally invasiveness and still high rate of en bloc resection.15 ESD in early gastric cancer usually demonstrated an excellent outcome when confined to mucosal layer. However, despite of the advancement of technology and devices, ESD remains to be a technically challenging and time consuming procedure.16 It would be essential to find solutions to improve the efficiency of the procedure.
Previous reports suggested that submucosal lesion size, location, invasion depth, submucosal fibrosis, perforation, and ulcer finding of lesion were risk factors for a longer procedure time.5,17,18 Since submucosal deep invasion, perforation, and ulcer finding of lesion were relatively rare events in our study, and limited case number would not allow many parameters in comparison, only lesion size, location, and submucosal fibrosis were taking into account. Our study suggested that the device factor might also influence the procedure time. The application of the HybridKnife results in a 28.9% increase on the efficiency of ESD performance while maintaining similar safety profile compared to ESD with conventional knives without integrated water-jet function for injection. The improvement was more significant at technically easier locations such as lower stomach or lesions smaller than 4 cm leading to the assumption that the submucosal fluid cushion was the most prominent factor to influence the procedure time of ESD. When it came to larger lesions and difficult locations including cardia and fundus of stomach, additional influencing factors might be more predominant such as the skill level of the operator. The HybridKnife was also useful with the existence of submucosal fibrosis. This seems logical since the rapid switching between injection and cutting would help to maintain a satisfactory submucosal fluid cushion all times during the procedure. It was not clear why there was a significant reduction of the procedure time in patients with cancerous lesions, but no reduction in noncancerous lesions with univariate analysis. However, this factor was ruled out during multivariate analysis. Probably the histology of lesions correlated with other independent factors such as the submucosal fibrosis or size of lesion.
Originally we considered the improvement of the HybridKnife on ESD procedure time would largely come from simplifying the submucosal dissection process, however, when procedure time were further subdivided into submucosal dissection time and nonsubmucosal dissection time, that is, procedure time minus submucosal dissection time, both showed significant improvement for the HybridKnife group over the IT knife group. This might partially result from the design of tip of the O-type HybridKnife. The noninsulated center of the tip can be used to mark the lesion margin, cut forward, and carry out hemostasis, while the shaft could cut laterally. The all-in-one design saves the time to exchange different devices.
The HybridKnife allows rapid and all time injection to minimize the exchange of devices and to a safe cutting plane within the submucosal layer by on-demand injection. Previous literature also reported that the use of the HybridKnife might reduce adverse event rates.19,20 Yahagi et al21 found that the HybridKnife resulted in an almost 5-fold reduction of the perforation rate in their comparative animal study (25% vs 5.5%, P = 0.035). However, adverse events including bleeding and perforation were both relatively rare events in our comparative study, no significant reduction could be revealed.
Several limitations of this study are noteworthy. First, the study contains a limited number of cases. To better compare the difference between ESD procedures, only patients with gastric lesions were enrolled in this trial. Therefore it was not possible to include more cases during a relatively short time frame. Second, a double-blind design is not possible to apply to this randomized controlled trial, and the knowing of device might serve as a bias. Third, the procedure was conducted by a single operator who was familiar with both of the devices in a single tertiary hospital. We considered technical parameters could be better controlled by this; however, it also raised the question if the improvement can be generalized. And how many cases needed to be performed before technically stabilization. Therefore, it will be necessary to assess whether these improvements can be seen across different endoscopists and hospitals with different settings.
In conclusion, the HybridKnife and the IT knife were equally effective and safe for successful en bloc resection of early gastric lesions. The HybridKnife appears to offer an advantage over the conventional knives without included water injection majority in terms of procedure time. More randomized controlled clinical trials are necessary to confirm these findings.
Footnotes
Abbreviations: EMR = endoscopic mucosal resection, ESD = endoscopic submucosal dissection, HGIN = high-grade intraepithelial neoplasia, IQR = interquartile range.
This study was supported by National Natural Science Foundation of China (no. 81172096 and 81372387).
R.H. and H.Y. contributed equally to this work.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Soetikno R, Kaltenbach T, Yeh R, et al. Endoscopic mucosal resection for early cancers of the upper gastrointestinal tract. J Clin Oncol 2005; 23:4490–4498. [DOI] [PubMed] [Google Scholar]
- 2.Probst A, Golger D, Arnholdt H, et al. Endoscopic submucosal dissection of early cancers, flat adenomas, and submucosal tumors in the gastrointestinal tract. Clin Gastroenterol Hepatol 2009; 7:149–155. [DOI] [PubMed] [Google Scholar]
- 3.Maple JT, Abu Dayyeh BK, et al. ASGE Technology Committee. Endoscopic submucosal dissection. Gastrointest Endosc 2015; 81:1311–1325. [DOI] [PubMed] [Google Scholar]
- 4.Kim MY, Cho JH, Jain P, et al. ESD around the world: Asia. Gastrointest Endosc Clin N Am 2014; 24:283–293. [DOI] [PubMed] [Google Scholar]
- 5.Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc 2009; 69:1228–1235. [DOI] [PubMed] [Google Scholar]
- 6.Cao Y, Liao C, Tan A, et al. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 2009; 41:751–757. [DOI] [PubMed] [Google Scholar]
- 7.Lian J, Chen S, Zhang Y, et al. A meta-analysis of endoscopic submucosal dissection and EMR for early gastric cancer. Gastrointest Endosc 2012; 76:763–770. [DOI] [PubMed] [Google Scholar]
- 8.von Renteln D. Endoscopic submucosal dissection—just add water(jet)? Endoscopy 2014; 46:843–844. [DOI] [PubMed] [Google Scholar]
- 9.Schumacher B, Charton JP, Nordmann T, et al. Endoscopic submucosal dissection of early gastric neoplasia with a water jet-assisted knife: a Western, single-center experience. Gastrointest Endosc 2012; 75:1166–1174. [DOI] [PubMed] [Google Scholar]
- 10.Fukami N, Ryu CB, Said S, et al. Prospective, randomized study of conventional versus HybridKnife endoscopic submucosal dissection methods for the esophagus: an animal study. Gastrointest Endosc 2011; 73:1246–1253. [DOI] [PubMed] [Google Scholar]
- 11.Zhou PH, Schumacher B, Yao LQ, et al. Conventional vs. waterjet-assisted endoscopic submucosal dissection in early gastric cancer: a randomized controlled trial. Endoscopy 2014; 46:836–843. [DOI] [PubMed] [Google Scholar]
- 12.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 2011; 14:101–112. [DOI] [PubMed] [Google Scholar]
- 13.Liu Z, Zhang X, Guo X, et al. Sa1393 O-type hybrid knife shortens the dissection time of gastric endoscopic submucosal dissection in a pilot perspective trial. Gastrointest Endosc 2013; 77:AB189. [Google Scholar]
- 14.Higashimaya M, Oka S, Tanaka S, et al. Outcome of endoscopic submucosal dissection for gastric neoplasm in relationship to endoscopic classification of submucosal fibrosis. Gastric Cancer 2013; 16:404–410. [DOI] [PubMed] [Google Scholar]
- 15.Gotoda T, Iwasaki M, Kusano C, et al. Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg 2010; 97:868–871. [DOI] [PubMed] [Google Scholar]
- 16.Neuhaus H. Endoscopic submucosal dissection in the upper gastrointestinal tract: present and future view of Europe. Dig Endosc 2009; 21 (Suppl. 1):S4–S6. [DOI] [PubMed] [Google Scholar]
- 17.Ahn JY, Choi KD, Choi JY, et al. Procedure time of endoscopic submucosal dissection according to the size and location of early gastric cancers: analysis of 916 dissections performed by 4 experts. Gastrointest Endosc 2011; 73:911–916. [DOI] [PubMed] [Google Scholar]
- 18.Nagata N, Honda M, Kobayakawa M, et al. Mycobacterium lentiflavum ileitis using aspirated intestinal fluid during endoscopy in HIV-infected patient. Dig Endosc 2011; 23:271–272. [DOI] [PubMed] [Google Scholar]
- 19.Lingenfelder T, Fischer K, Sold MG, et al. Combination of water-jet dissection and needle-knife as a hybrid knife simplifies endoscopic submucosal dissection. Surg Endosc 2009; 23:1531–1535. [DOI] [PubMed] [Google Scholar]
- 20.Kaehler GF, Sold MG, Fischer K, et al. Selective fluid cushion in the submucosal layer by water jet: advantage for endoscopic mucosal resection. Eur Surg Res 2007; 39:93–97. [DOI] [PubMed] [Google Scholar]
- 21.Yahagi N, Neuhaus H, Schumacher B, et al. Comparison of standard endoscopic submucosal dissection (ESD) versus an optimized ESD technique for the colon: an animal study. Endoscopy 2009; 41:340–345. [DOI] [PubMed] [Google Scholar]


