Abstract
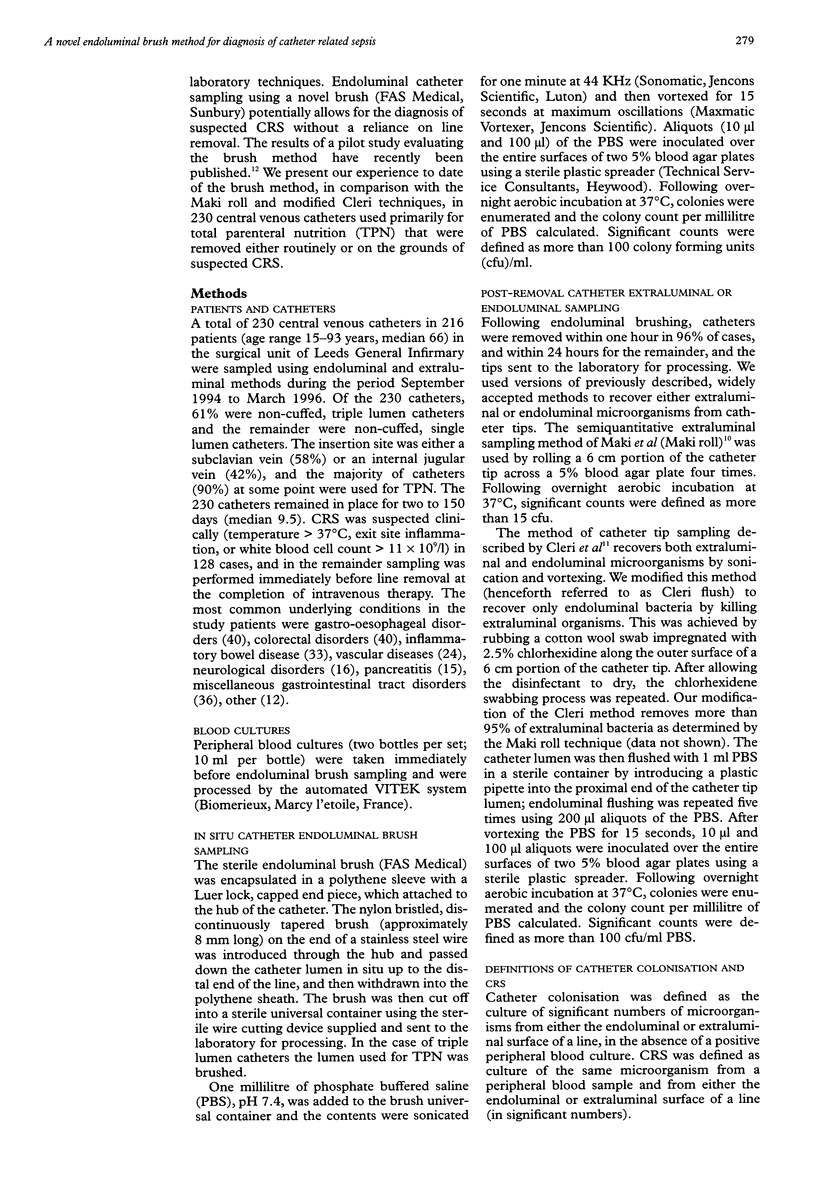
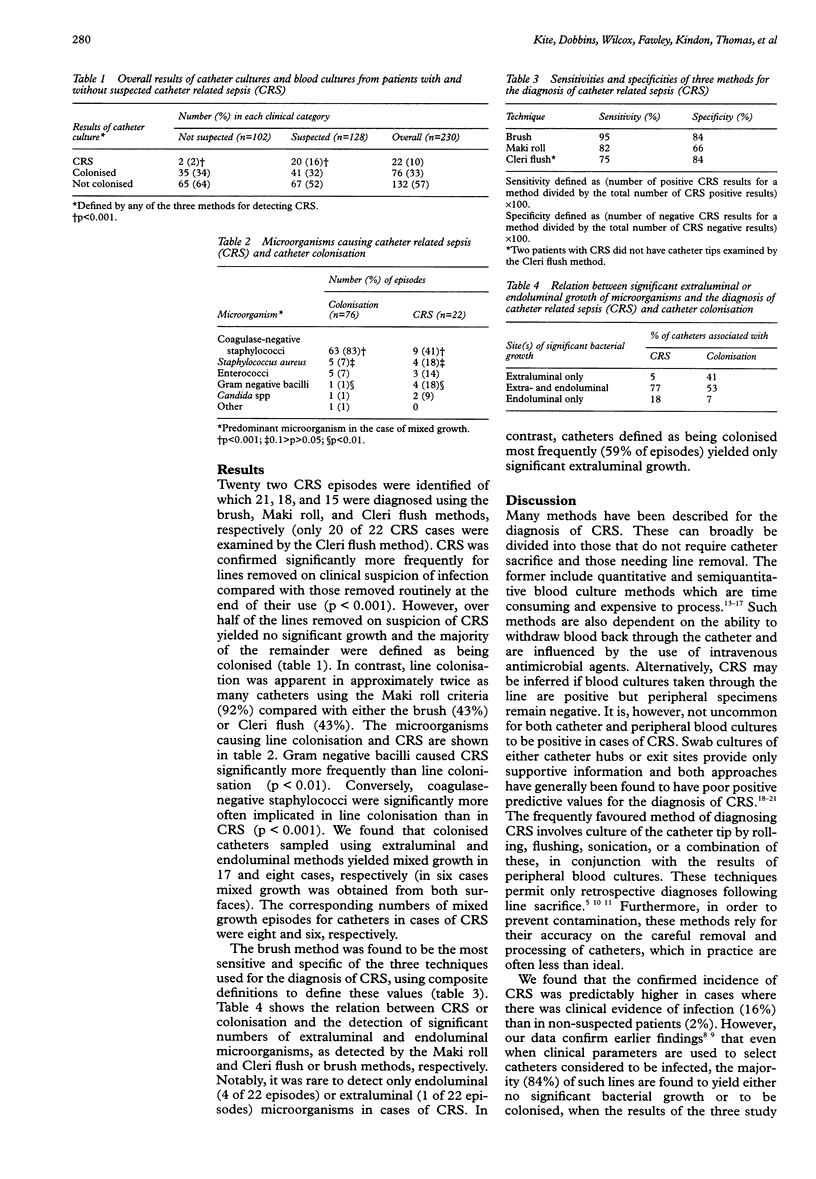
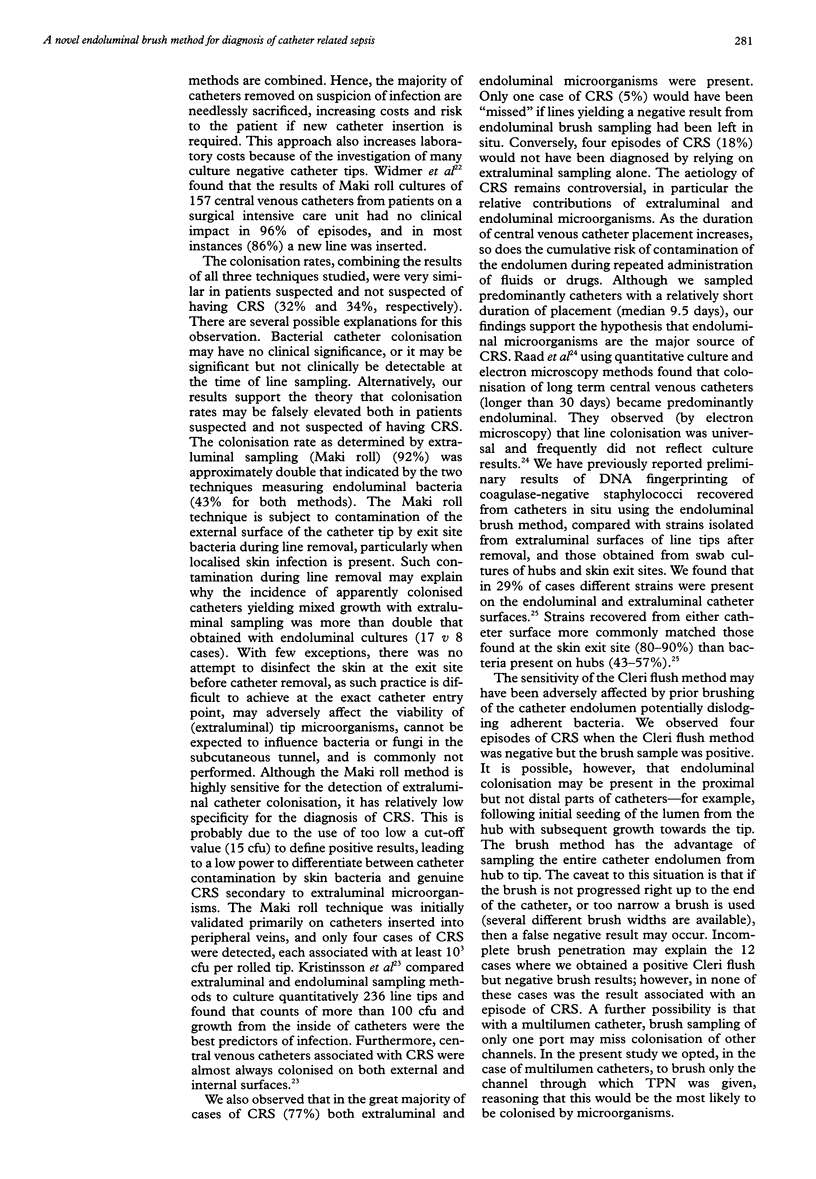
AIMS: To determine the accuracy of a novel endoluminal brush method for the diagnosis of catheter related sepsis (CRS), which is performed in situ and hence does not require line sacrifice. METHODS: 230 central venous catheters in 216 patients were examined prospectively for evidence of CRS or colonisation using an endoluminal brush method in conjunction with peripheral blood cultures. The results were compared with those obtained using methods that require line sacrifice: extraluminal sampling (Maki roll) or endoluminal sampling (modified Cleri flush) of microorganisms. RESULTS: Only 16% of 128 patients suspected clinically of having line associated infection were confirmed as having CRS. In addition, 2 of 102 patients not suspected of having line associated infection had CRS. Line colonisation was apparent in approximately twice as many catheters using the Maki roll criteria (92%) compared with either the endoluminal brush (43%) or Cleri flush (43%). Furthermore, colonised catheters sampled using the Maki roll technique yielded mixed growth twice as often as when examined by endoluminal methods (17 and 8 cases, respectively). It was rare to detect either only endoluminal (4 of 22 episodes) or extraluminal (1 of 22 episodes) microorganisms in cases of CRS. In contrast, catheters defined as being colonised most frequently (59% of episodes) yielded only significant extraluminal growth. Only one case of CRS (5%) would have been "missed" if lines yielding a negative result from endoluminal brush sampling had been left in situ. Conversely, four episodes of CRS (18%) would not have been diagnosed by relying on extraluminal sampling alone. CONCLUSIONS: Diagnosis of CRS by the endoluminal brush method can be achieved without line sacrifice and is more sensitive (95%) and specific (84%) than extraluminal sampling of the catheter tip by the Maki roll technique (82% and 66%, respectively).
Full text
PDF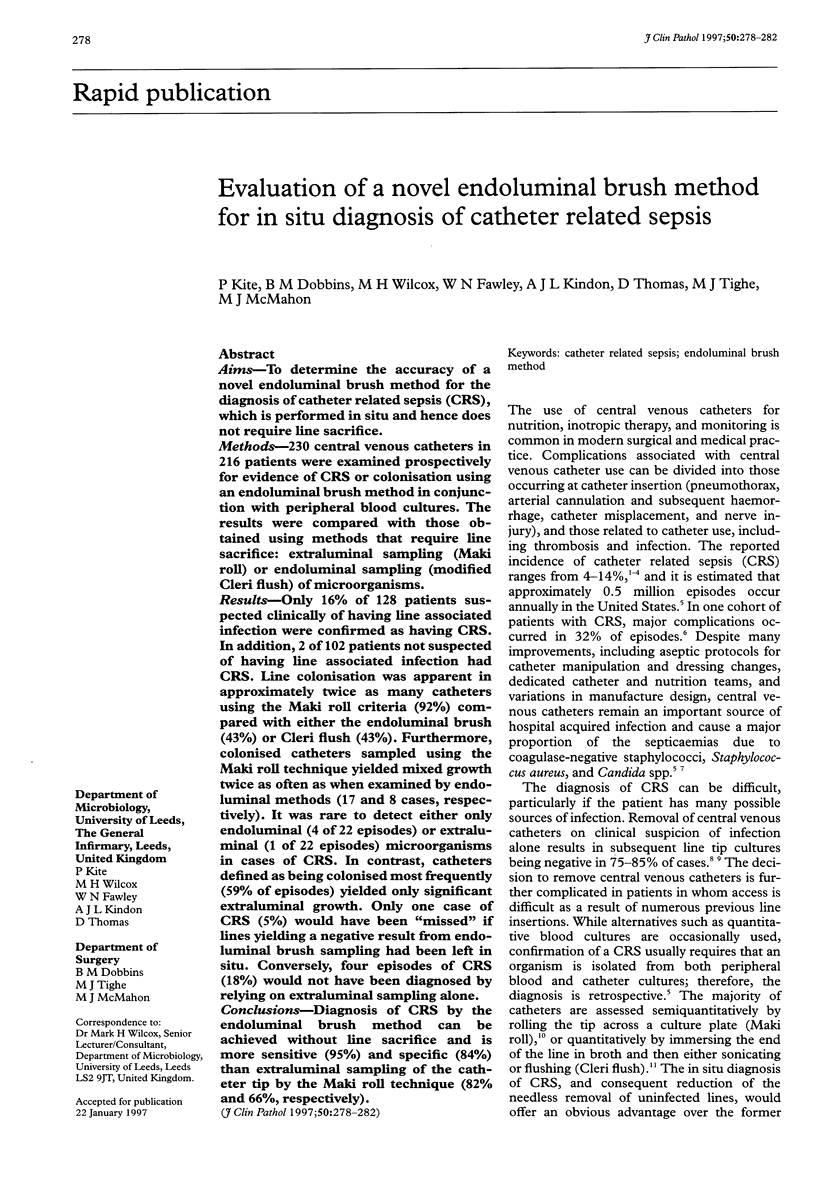
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnow P. M., Quimosing E. M., Beach M. Consequences of intravascular catheter sepsis. Clin Infect Dis. 1993 Jun;16(6):778–784. doi: 10.1093/clind/16.6.778. [DOI] [PubMed] [Google Scholar]
- Bozzetti F., Terno G., Bonfanti G., Gallus G. Blood culture as a guide for the diagnosis of central venous catheter sepsis. JPEN J Parenter Enteral Nutr. 1984 Jul-Aug;8(4):396–398. doi: 10.1177/0148607184008004396. [DOI] [PubMed] [Google Scholar]
- Cercenado E., Ena J., Rodríguez-Créixems M., Romero I., Bouza E. A conservative procedure for the diagnosis of catheter-related infections. Arch Intern Med. 1990 Jul;150(7):1417–1420. [PubMed] [Google Scholar]
- Cleri D. J., Corrado M. L., Seligman S. J. Quantitative culture of intravenous catheters and other intravascular inserts. J Infect Dis. 1980 Jun;141(6):781–786. doi: 10.1093/infdis/141.6.781. [DOI] [PubMed] [Google Scholar]
- Gil R. T., Kruse J. A., Thill-Baharozian M. C., Carlson R. W. Triple- vs single-lumen central venous catheters. A prospective study in a critically ill population. Arch Intern Med. 1989 May;149(5):1139–1143. [PubMed] [Google Scholar]
- Kristinsson K. G., Burnett I. A., Spencer R. C. Evaluation of three methods for culturing long intravascular catheters. J Hosp Infect. 1989 Oct;14(3):183–191. doi: 10.1016/0195-6701(89)90034-0. [DOI] [PubMed] [Google Scholar]
- Liñares J., Sitges-Serra A., Garau J., Pérez J. L., Martín R. Pathogenesis of catheter sepsis: a prospective study with quantitative and semiquantitative cultures of catheter hub and segments. J Clin Microbiol. 1985 Mar;21(3):357–360. doi: 10.1128/jcm.21.3.357-360.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki D. G., Weise C. E., Sarafin H. W. A semiquantitative culture method for identifying intravenous-catheter-related infection. N Engl J Med. 1977 Jun 9;296(23):1305–1309. doi: 10.1056/NEJM197706092962301. [DOI] [PubMed] [Google Scholar]
- Michel L., McMichan J. C., Bachy J. L. Microbial colonization of indwelling central venous catheters: statistical evaluation of potential contaminating factors. Am J Surg. 1979 Jun;137(6):745–748. doi: 10.1016/0002-9610(79)90085-0. [DOI] [PubMed] [Google Scholar]
- Padberg F. T., Jr, Ruggiero J., Blackburn G. L., Bistrian B. R. Central venous catheterization for parenteral nutrition. Ann Surg. 1981 Mar;193(3):264–270. doi: 10.1097/00000658-198103000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paya C. V., Guerra L., Marsh H. M., Farnell M. B., Washington J., 2nd, Thompson R. L. Limited usefulness of quantitative culture of blood drawn through the device for diagnosis of intravascular-device-related bacteremia. J Clin Microbiol. 1989 Jul;27(7):1431–1433. doi: 10.1128/jcm.27.7.1431-1433.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell C., Kudsk K. A., Kulich P. A., Mandelbaum J. A., Fabri P. J. Effect of frequent guidewire changes on triple-lumen catheter sepsis. JPEN J Parenter Enteral Nutr. 1988 Sep-Oct;12(5):462–464. doi: 10.1177/0148607188012005462. [DOI] [PubMed] [Google Scholar]
- Prager R. L., Silva J., Jr Colonization of central venous catheters. South Med J. 1984 Apr;77(4):458–461. doi: 10.1097/00007611-198404000-00012. [DOI] [PubMed] [Google Scholar]
- Raad I., Costerton W., Sabharwal U., Sacilowski M., Anaissie E., Bodey G. P. Ultrastructural analysis of indwelling vascular catheters: a quantitative relationship between luminal colonization and duration of placement. J Infect Dis. 1993 Aug;168(2):400–407. doi: 10.1093/infdis/168.2.400. [DOI] [PubMed] [Google Scholar]
- Ruderman J. W., Morgan M. A., Klein A. H. Quantitative blood cultures in the diagnosis of sepsis in infants with umbilical and Broviac catheters. J Pediatr. 1988 May;112(5):748–751. doi: 10.1016/s0022-3476(88)80695-4. [DOI] [PubMed] [Google Scholar]
- Ryan J. A., Jr, Abel R. M., Abbott W. M., Hopkins C. C., Chesney T. M., Colley R., Phillips K., Fischer J. E. Catheter complications in total parenteral nutrition. A prospective study of 200 consecutive patients. N Engl J Med. 1974 Apr 4;290(14):757–761. doi: 10.1056/NEJM197404042901401. [DOI] [PubMed] [Google Scholar]
- Salzman M. B., Isenberg H. D., Shapiro J. F., Lipsitz P. J., Rubin L. G. A prospective study of the catheter hub as the portal of entry for microorganisms causing catheter-related sepsis in neonates. J Infect Dis. 1993 Feb;167(2):487–490. doi: 10.1093/infdis/167.2.487. [DOI] [PubMed] [Google Scholar]
- Snydman D. R., Gorbea H. F., Pober B. R., Majka J. A., Murray S. A., Perry L. K. Predictive value of surveillance skin cultures in total-parenteral-nutrition-related infection. Lancet. 1982 Dec 18;2(8312):1385–1388. doi: 10.1016/s0140-6736(82)91281-8. [DOI] [PubMed] [Google Scholar]
- Stamm W. E. Infections related to medical devices. Ann Intern Med. 1978 Nov;89(5 Pt 2 Suppl):764–769. doi: 10.7326/0003-4819-89-5-764. [DOI] [PubMed] [Google Scholar]
- Tighe M. J., Kite P., Fawley W. N., Thomas D., McMahon M. J. An endoluminal brush to detect the infected central venous catheter in situ: a pilot study. BMJ. 1996 Dec 14;313(7071):1528–1529. doi: 10.1136/bmj.313.7071.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widmer A. F., Nettleman M., Flint K., Wenzel R. P. The clinical impact of culturing central venous catheters. A prospective study. Arch Intern Med. 1992 Jun;152(6):1299–1302. [PubMed] [Google Scholar]
- Wing E. J., Norden C. W., Shadduck R. K., Winkelstein A. Use of quantitative bacteriologic techniques to diagnose catheter-related sepsis. Arch Intern Med. 1979 Apr;139(4):482–483. [PubMed] [Google Scholar]



