Abstract
The aim of this study was to compare the effectiveness and safety of 2 surgical techniques that are used to treat proximal femoral fractures.
A systematic literature search (up to December 2014) was conducted in Medline, Embase, PubMed, and The Cochrane Central Register of Controlled Trials to screen for studies comparing proximal femoral nail antirotation (PFNA) with less invasive stabilization system–distal femur (LISS-DF) for proximal femoral fractures. Two authors independently assessed the methodological quality of the included studies and extracted data. Surgical information and postoperative outcomes were analyzed.
A total of 7 studies with 361 patients who satisfied the eligibility criteria included 3 randomized controlled trials and 4 case-controlled trials associated with PFNA versus LISS in treating proximal femoral fractures. Our results demonstrated that there was a significant reduction in hospital stay and time to weight-bearing ambulation and bone healing for PFNA compared with LISS (odds ratio [OR] −1.48, 95% confidence interval [CI] −2.92 to −0.05; OR −7.08, 95% CI −8.32 to −5.84; OR −2.71, 95% CI −4.76 to 0.67). No statistically significant difference was observed between the 2 groups for operative time, blood loss volume, Harris hip score, and incidence of complications.
Based on the results of this analysis, we inferred that PFNA is safer and more effective than reverse LISS-DF in patients undergoing osteosynthesis for proximal femoral fractures, and that PFNA is associated with reduced hospital stays and reduced time to weight-bearing ambulation and bone healing. Nonetheless, in certain cases in which PFNA is not suitable due to abnormal structure of the proximal femur or particularly unstable fractures, the LISS plate technique could be a useful alternative.
INTRODUCTION
Fractures of the proximal femur are commonly seen in orthopedic clinics, primarily in the older population, and the incidence may increase in the next several decades due to the aging global population.1 It is generally agreed that early operative intervention is the preferred treatment if the patient is in good physical condition because it allows for early rehabilitation and avoids the complications of long-term bed rest.2 Numerous internal fixation devices have been used to stabilize proximal femoral fractures, and all of these can be divided into the following 2 systems: intramedullary fixation and extramedullary fixation. Among the intramedullary systems, proximal femoral nail antirotation (PFNA) is currently one of the most effective strategies for treating proximal femoral fractures and can improve rotational and angular stability.3–5 Less invasive stabilization system–distal femur (LISS-DF) was initially designed for distal femoral fractures.6 Recently, a few studies have described its successful use in the treatment of intertrochanteric femoral fractures, and the clinical results have been satisfactory.7 Both techniques have certain mechanical or anatomical advantages and disadvantages. For the LISS-DF system, its structural shape has good adaptability to and angular stabilization with the anatomical proximal contour,8 whereas PFNA has superior biomechanical properties in sustaining axial load, thereby allowing the patient to bear weight at an earlier stage after surgery.9,10 Nonetheless, the PFNA method can induce additional surgical trauma to the proximal femur during reaming of the medullary cavity and by damaging the lateral cortex.5,11 In addition, this technique does not provide strong stabilization in patients with severe osteoporosis or complicated fractures involving intertrochanteric coronal splitting or reverse obliquity fractures, which can induce postoperative complications such as varus deformity and fixation failure.12
Several randomized controlled trials (RCTs) and non-RCTs have been conducted to compare PFNA with LISS-DF in treating proximal femoral fractures. However, no consensus has been reached regarding which of the 2 techniques leads to superior results and better clinical outcomes. Hence, the purpose of this meta-analysis is to evaluate the evidence from the RCT and non-RCT studies that have compared the safety and efficacy of PFNA and LISS-DF for treating patients with proximal femoral fractures.
METHODS
Search Strategy
To aggregate all of the relevant published studies, PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)-compliant searches of Medline, Embase, The Cochrane Central Register of Controlled Trials, Google Scholar, WanFang, and Chinese National Knowledge Infrastructure were carried out for all peer-reviewed studies published from January 1980 to December 2014 that compared PFNA with LISS-DF for treating proximal femoral fractures, and there were no language restrictions. The following medical subject headings (MeSH) and terms were used to achieve broad and specific searches: proximal femoral fractures and PFNA and LISS in combination with the Boolean operators AND or OR. Additional records were identified through other available databases according to the Cochrane Collaboration guidelines.
Eligibility Criteria
Studies were considered eligible for inclusion if they met the following criteria: study design—interventional studies (RCTs or non-RCTs); population—patients with proximal femoral fractures; and operative intervention—PFNA group and LISS group.
Exclusion Criteria
Patients were excluded from the meta-analysis if they had a neoplastic etiology (metastasis or myeloma), infection, congenital deformity, or mental disease.
Selection Criteria
Two reviewers independently screened the titles and abstracts for the eligibility criteria. Subsequently, the full text of the studies that potentially met the inclusion criteria were read, and the literature was reviewed to determine the final inclusion. Disagreements were resolved by consulting a third reviewer (XLM).
Data Extraction
All the titles and abstracts of the relevant studies were first independently categorized by 2 reviewers, and then the full-text articles that met the eligibility criteria were read and selected for inclusion. Whenever necessary, we contacted the authors of the articles to obtain missing data or further information. The detailed data include the title, year of publication, design of study (RCT or non-RCT), sample size, age and sex of participants, blinding method, surgical procedures, types of fixation implants, duration of follow-up, and outcome parameters. Any disagreements encountered were resolved by discussion.
Outcomes of Interest
The data were independently selected by 2 reviewers, and agreement was achieved for all variables from all the included articles. The following clinical outcomes were recorded: duration of operation, loss of blood volume, bone healing time, time to weight-bearing, Harris hip score, and related complications such as deep vein thrombosis, infection, and fixation failure.
Assessment of Methodological Quality
Two strategies were used to assess the methodological quality of the studies. First, all studies that met the RCT criteria were assessed with the Cochrane Collaboration Risk of Bias Tool, which includes random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcomes assessment, incomplete outcome data, selective reporting, and other biases. Second, other non-RCTs were assessed with the Methodological Index for Nonrandomized Studies (MINORS). According to the Cochrane Collaboration recommendations, the methodological quality of eligible clinical trials was independently assessed by 2 reviewers. Any divergence was resolved through discussion. An arbiter (XLM) was consulted for reconciliation when no consensus could be achieved.
Statistical Analysis
All of the meta-analyses were performed with Review Manager software (RevMan Version 5.3, The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark). In each included study, the means and standard deviations were pooled into a weighted mean difference (WMD) and a 95% confidence interval (CI) for the continuous outcomes, and risk differences (or relative risks) and 95% CIs were calculated for dichotomous outcomes. A P value <0.05 was considered statistically significant. Statistical heterogeneity was assessed using the I2 value and chi-square test. The derivation of heterogeneity, if present, was analyzed according to the methodological quality, participant characteristics, and specific interventions. The WMD or standardized mean difference (SMD) was used for continuous outcomes in which a fixed-effect model was initially set, and if the P value of the heterogeneity test was <0.05 or I2 >50%, then the random-effects model was applied for data synthesis.
Ethical Review
All analyses were based on previous published studies which had given the ethical approval from the local institution; thus no more ethical approval and patient consent were required.
RESULTS
Search Results and Quality Assessment
A total of 158 titles and abstracts were preliminarily reviewed, and the details of the search and exclusion criteria are displayed in a flow diagram (Figure 1). We identified 7 studies that satisfied the eligibility criteria, including 3 RCTs and 4 CCTs associated with PFNA versus LISS-DF in treating proximal femoral fractures.13–19 Among them, there were 3 articles in English and 4 in Chinese. We applied the Cochrane Collaboration Risk of Bias Tool to evaluate the quality of the RCTs (Figure 2), and the MINORS assessment was used for non-RCTs (Table 1). The quality of the RCTs was acceptable, but 1 publication's score was relatively low due to its limited explanation of the details of randomization,14 and the remaining 2 RCTs15,16 reported that their methods of randomization were conducted through a sealed envelope or a computer-generated list, respectively. Moreover, some of the measurement data of 1 randomized article were invalid for our study.16 None of the included studies reported blinding of the surgeons, participants, or assessors, though 1 study mentioned that the randomization list was concealed from the surgeon.16 One study17 did not describe the baseline in detail, so we e-mailed the writer and received the data. All of the studies provided results for a minimum of 95% of the included patients.
FIGURE 1.
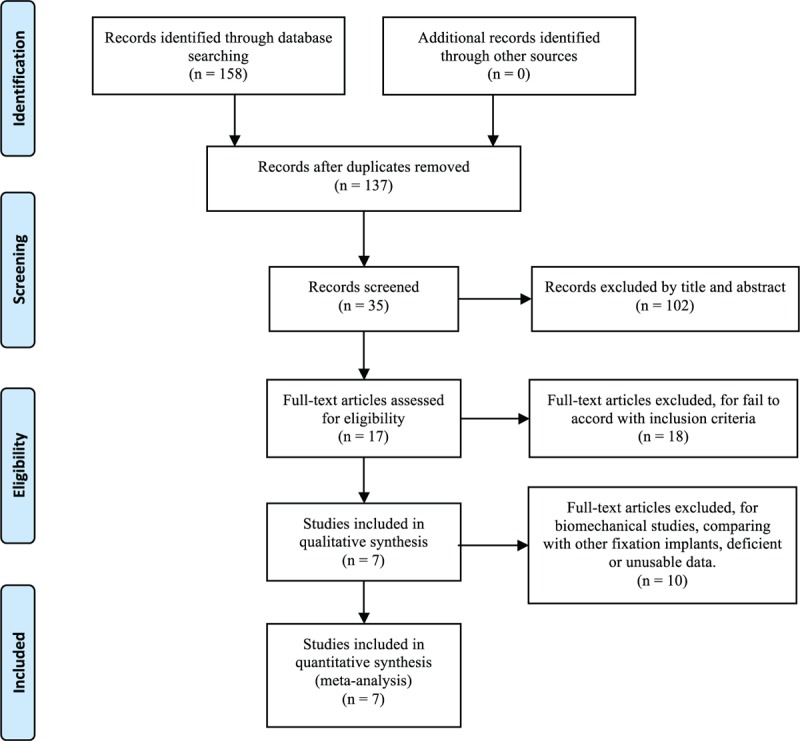
Guidelines flow diagram.
FIGURE 2.
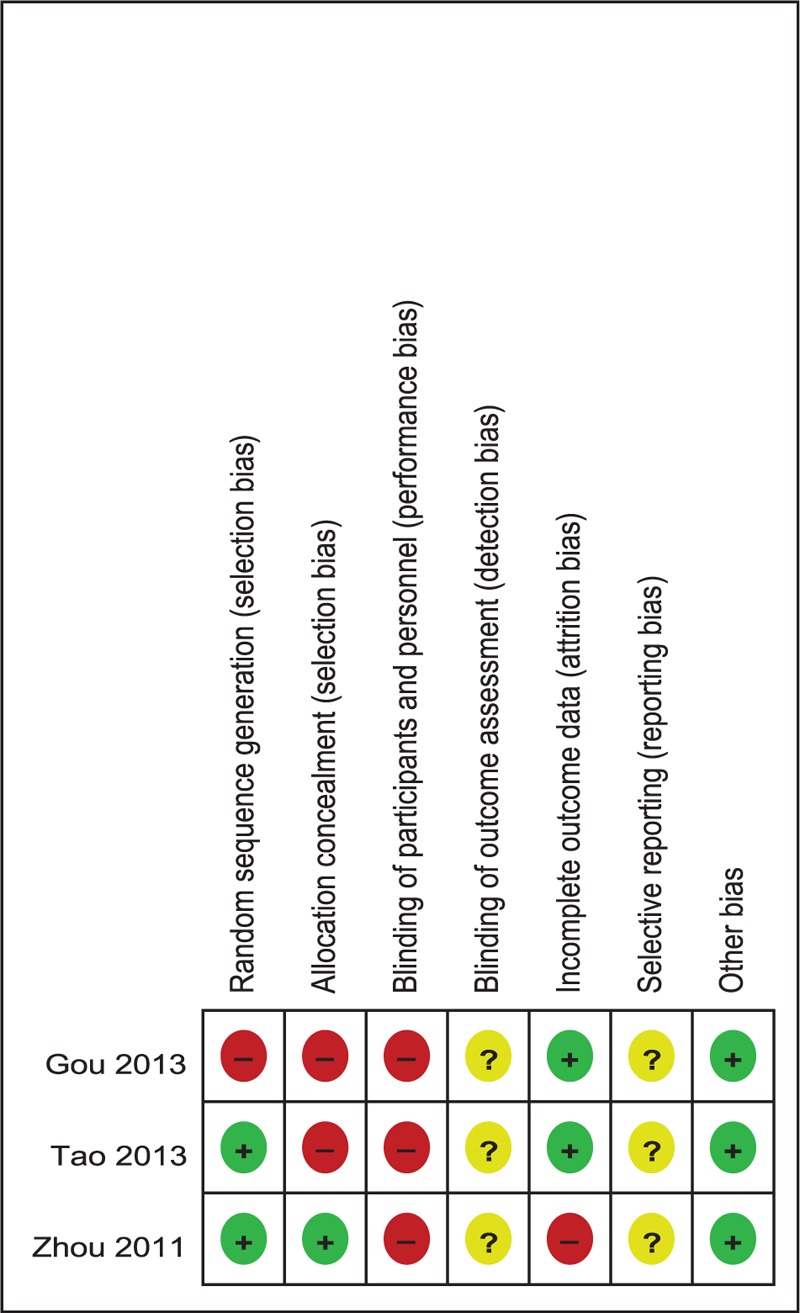
The summary of bias risk of randomized controlled trials.
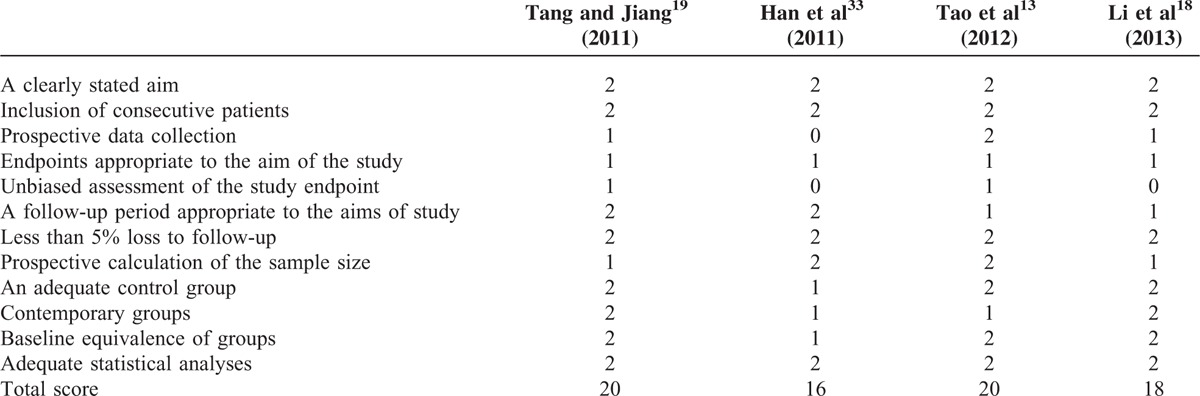
TABLE 1.
Quality Assessment of Nonrandomized Trials
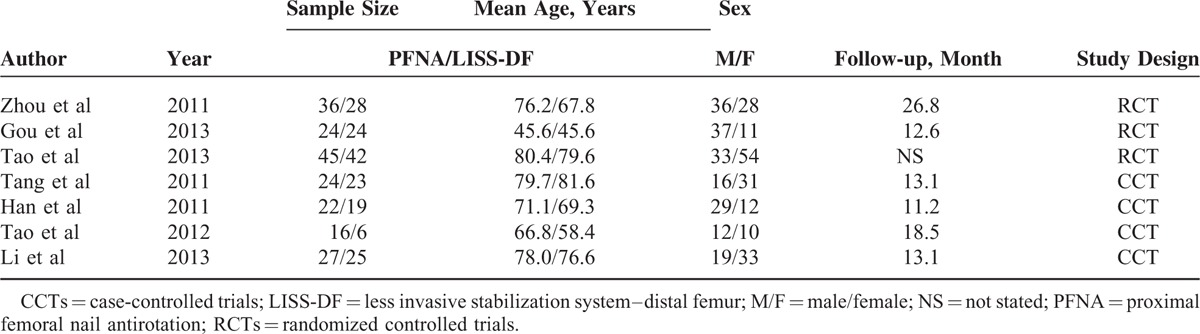
Demographic Characteristics
The demographic characteristics of the included studies are shown in Table 2. The characteristics of the enrolled patients are listed in Table 2. In total, 361 patients were eligible for our meta-analysis, with 194 patients who underwent PFNA and 176 patients who received LISS to treat proximal femoral fractures.
TABLE 2.
Characteristics of the Included Study
Duration of Operation
Based on 5 studies14,15,17–19 providing available data, we found that there was significant heterogeneity (χ2 = 33.87, df = 4, I2 = 88%, P < 0.00001). As depicted in Figure 3, the pooled results showed no significant difference between the 2 groups according to a random-effects model (WMD = −8.87, 95% CI −18.29 to 0.55, P = 0.07).
FIGURE 3.

Forest plot diagram showing weighted mean difference of operation time.
Loss of Blood Volume
Intraoperative blood loss was documented in 6 studies13–15,17–19 (Figure 4). A random-effects model was applied because statistical heterogeneity was found between the studies (χ2 = 13.55, df = 5, I2 = 63%, P = 0.02). The results indicated that there was no statistically significant difference between PFNA and LISS (WMD = −24.68, 95% CI −49.99 to 0.63, P = 0.06).
FIGURE 4.
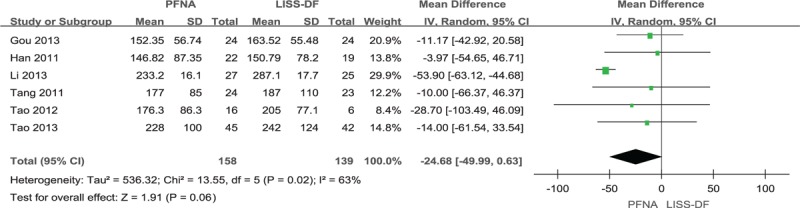
Forest plot diagram showing weighted mean difference of blood loss.
Bone-healing Time
Six studies13–15,17–19 reported the healing time associated with PFNA and LISS (Figure 5). The available data demonstrated that the time for bone healing was significantly shorter in the PFNA group compared with the LISS group (WMD = −2.71, 95% CI −4.76 to 0.67, P = 0.009). The pooled results showed significant heterogeneity (χ2 = 59.03, df = 5, I2 = 92%, P < 0.00001), and therefore, a random-effects model was used.
FIGURE 5.
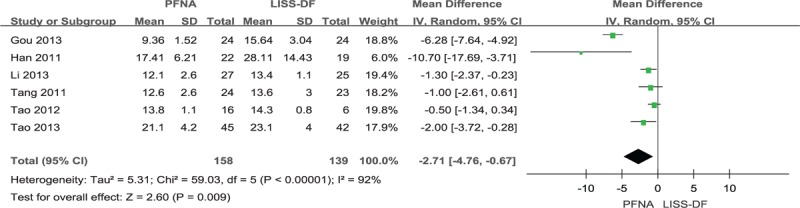
Forest plot diagram showing weighted mean difference of time of bone healing.
Time to Weight-bearing
Three studies13,14,17 stated the time to postoperative weight-bearing (Figure 6). Due to the heterogeneity of no significant difference (χ2 = 0.78, df = 2, I2 = 0%, P = 0.68), a fixed-effects model was adopted to pool the data. The pooled results revealed that there was a statistically significant difference between the 2 groups (WMD = −7.08, 95% CI −8.32 to −5.84, P < 0.00001).
FIGURE 6.
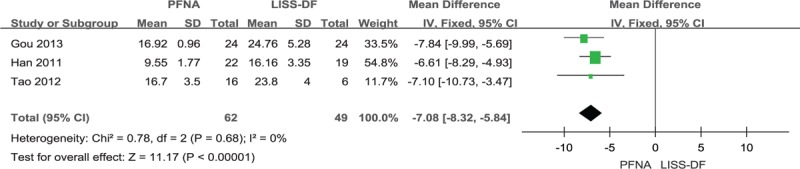
Forest plot diagram showing weighted mean difference of time to bear weight.
Hospital Time
There were 3 articles13,15,19 that documented the length of hospital stay (Figure 7). No significant heterogeneity was found in the pooled outcomes, so a fixed-effects model was utilized for our study (χ2 = 0.31, df = 2, I2 = 0%, P = 0.86). The difference between PFNA and LISS was significant (WMD = −1.48, 95% CI −2.92 to −0.05, P = 0.04).
FIGURE 7.
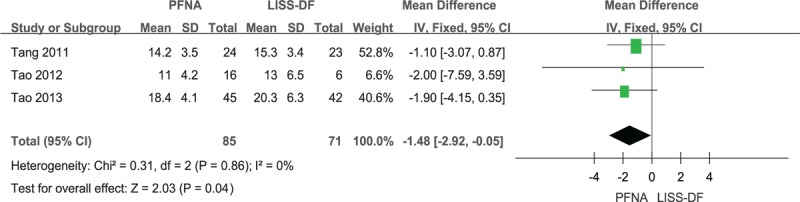
Forest plot diagram showing weighted mean difference of time in hospital.
Harris Hip Score
The results of a pooled statistical analysis of 5 studies13–15,18,19 are shown in Figure 8, and indicate that there was no statistically significantly heterogeneity (χ2 = 2.94, df = 4, I2 = 0%, P = 0.57). No significant difference was found between the 2 groups either (WMD = −0.79, 95% CI −1.64 to 0.06, P = 0.07).
FIGURE 8.
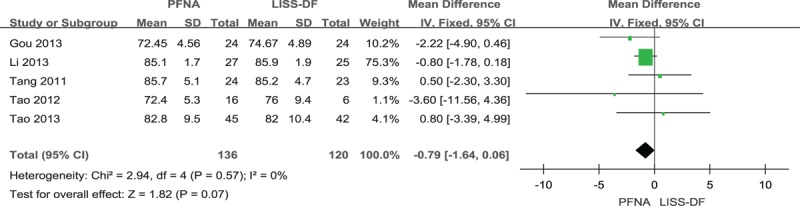
Forest plot diagram showing weighted mean difference of Harris scores.
Complications
Deep Vein Thrombosis
Five studies13–16,19 with 268 participants provided relevant data (Figure 9). Their summarized estimate of effect size did not show a statistically significant difference between the compared groups (RD = 0.01, 95% CI −0.04 to 0.06, P = 0.72). At the same time, no significant statistical heterogeneity was present (χ2 = 0.78, df = 4, I2 = 0%, P = 0.94).
FIGURE 9.
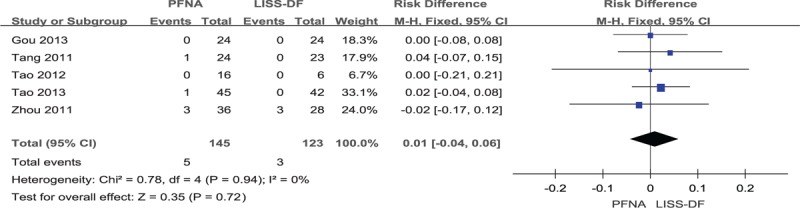
Forest plot diagram showing risk difference of deep venous thrombosis.
Infection
Data extracted from 6 studies13,16,18,19 (Figure 10), including 317 participants, substantiated that no statistically significant difference was found between PFNA and LISS (RD = −0.01, 95% CI −0.06 to 0.04, P = 0.71), with an absence of statistical heterogeneity (χ2 = 1.25, df = 5, I2 = 0%, P = 0.71).
FIGURE 10.
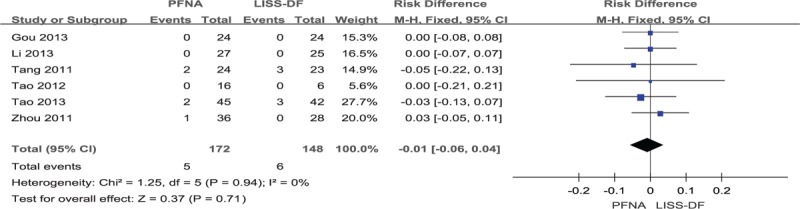
Forest plot diagram showing risk difference of infection.
Fixation Failure
Six studies13–15,17–19 provided data regarding fixation failure (Figure 11). The pooled estimate of information did not show a statistically significant difference between the compared groups (RD = −0.02, 95% CI −0.06 to 0.03, P = 0.44), and statistical heterogeneity was not present (χ2 = 3.90, df = 5, I2 = 0%, P = 0.56).
FIGURE 11.
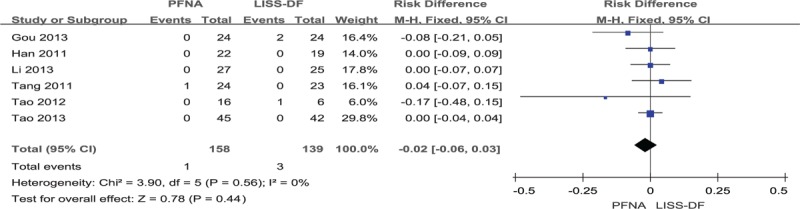
Forest plot diagram showing risk difference of fixation rate.
DISCUSSION
Early operative intervention is generally considered the preferred choice in treating proximal femoral fractures, not only because it reduces both mortality and morbidity but because it also allows for early ambulation and decreases the risks associated with prolonged bed rest. There are 2 types of internal fixation: extramedullary fixation and intramedullary fixation. Currently, intramedullary nails, such as those used in PFNA, are widely used in treating fractures because of a biological advantage, minimally invasive approach, and easy manipulation. However, clinical outcomes are not always satisfactory, and secondary fracture of the distal femur or even fixation failure may occur. LISS is an extramedullary fixation system, which was first designed by the AO group for stabilization of distal femoral and proximal tibial fractures, and combines the advantages of interlocked intramedullary nailing techniques and biological plating techniques into 1 system.20 Through a thorough search of all available publications, we found the earliest study reporting this technique's debut in treating proximal femoral fractures.21 In that case report, the initial motive for selecting LISS was that it was considered to be a temporary fixation until further fixation could be applied. However, it worked successfully as the definitive fixation device. Since that study, LISS has been recommended as an alternative treatment for proximal femoral fractures. According to previous studies, LISS has a clinical effect similar to that of intramedullary nailing. However, there has been no consensus concerning whether PFNA is an optimal operation compared with LISS. Therefore, we performed this meta-analysis to compare the advantages and disadvantages of the 2 devices to provide reliable evidence for clinicians in selecting the optimal treatment.
Seven clinical trials were included in this meta-analysis, including 3 RCTs and 4 CCTs. Two RCTs16,17 stated that the randomization was generated by a computer-assisted program and a sealed envelope, respectively, and the other studies14 did not provide the details. Only 1 study16 blinded the surgeons, so an expectation bias and potential type II statistical error may affect this meta-analysis. The baseline data of the all included publications were available and intact. However, an intention-to-treat analysis was not mentioned. Thus, all these negative methodological factors should be taken into consideration when reviewing the findings of the current study.
Two previous studies, by Tao et al15 and Zhou et al16 showed that operative time was longer in the LISS group compared with the PFNA group, but our study showed no significant difference between the 2 groups for operative time. Tao et al's explanation was that their department was skilled at PFNA and lacked experience in reverse LISS. The interpretation in our study may have differed due to the varied types and degrees of fractures in the included studies. Moreover, another potential cause of this inconsistency is that there is no standard procedure for reverse LISS in treating proximal femoral fractures.
Six studies13–15,17–19 mentioned intraoperative blood loss. Although each study showed that the blood loss volume with PFNA was less than with LISS, our research found no significant difference (P = 0.06) in blood loss between the 2 groups. Yin22 found that the LISS group received an increased number of blood transfusions and noted that an open surgical technique was the main cause for this significant difference. Moreover, we noted longer incision lengths in the LISS group, which might be an additional explanation.
Bone healing time was recorded in 6 studies.13–15,17–19 The outcome of our research indicated that the LISS group had significantly longer fracture-healing times compared with the PFNA group. Furthermore, 3 articles15–17 stated the time to postoperative weight-bearing, and the results showed that the PFNA group achieved weight-bearing ambulation earlier than the LISS group. In a previous biomechanical comparison study of intramedullary devices and extramedullary devices, Zlowodzki et al23 reported that the fixation strength of LISS was 13% greater for axial loading and 45% weaker for torsional loading compared with intramedullary nailing. However, Kim et al24 suggested that the fixation strength of LCP-DF was 250% weaker for axial loading and similar for ultimate displacement compared with PFN. These studies implied that PFNA allow patients to bear partial weight at an earlier stage not only because it can sustain a large axial load but because it can also enhance its bone purchase by compacting cancellous bone with a helical blade. Although fixation by multiple screws locked with the LISS plate provides a rigid structure to prevent screw loosening and pull-out,25 some studies have noted that weight-bearing too early may cause stress concentration and thus potentially lead to fixation failure.8 Therefore, exercise with partial weight-bearing was only permitted when a callus bridged the fracture ends in patients who were treated with reverse LISS-DF. It is possible that this postponement led to a loading environment that was not conducive to fracture union, and hence, bone healing and time to weight-bearing were delayed.
Three studies13,15,19 mentioned length of hospital stay. Our meta-analysis found that compared with the LISS group, the PFNA group had significantly shorter hospital stays. Based on the above discussion, it can be inferred that early weight-bearing exercise may promote postoperative recovery, which reduces hospital stay. Moreover, the varied physical status and fracture types of patients should also be taken into consideration.
For recovery of hip joint function after surgery, 5 studies13–15,18,19 reported results by using the Harris hip score. In our study, no significant difference was found between the PFNA and LISS groups. This result could be due to the different follow-up times and lack of data regarding postoperative rehabilitation. Furthermore, that delayed weight-bearing activity and bone healing in the LISS group might influence the functional status should also be taken into consideration.
Deep vein thrombosis is relatively uncommon after lower limb surgery, but if it does occur, the results can be devastating in terms of prognosis and survival.26 Although LISS relied on minimally invasive surgery to reduce soft tissue damage and protect the blood supply,20 our results showed no significant difference in the occurrence of deep vein thrombosis, with 3.45% in the PFNA group versus 2.44% in the LISS group. However, this finding could have been affected by the limited sample size.
Regarding the risk of infection, impairment of the medullary cavity might have increased the risk of infection with PFNA, whereas in the LISS groups, the risk of infection might have been increased because of longer incisions, which might have led to more wound exposure. Our study showed that there was no significant difference in infection incidence between the PFNA and LISS groups. However, injury severity, intraoperative performance, and postoperative nursing may have influenced the stability of the pooled results.
The most controversial topic concerning proximal femoral fractures is the choice of implants, that is, which have superior therapeutic efficacy and fewer complications. Several studies10,20,23,27 have investigated the fixation strength of different devices, and the tests revealed that, except for maximal axial load, LISS has mechanical properties similar to intramedullary nails. Because of this axial load weakness, some authors28–32 have advocated PFNA as an optimal fixation device for treating proximal femoral fractures because it not only provides strong axial stability and secure bone purchase in the femoral neck-head but also has a low rate of complications. Although PFNA is commonly used to treat proximal femoral fractures, results have not always been satisfactory when the fracture extended to both the greater trochanter and lateral cortex or involved reverse obliquity fractures, which can increase the risk of acetabular penetration, blade loosening, nail breakage, or hip varus deformity.33–36 Meanwhile, Han et al17 believed that the reverse LISS technique could produce better results in those unstable fractures by forming a rigid structure to maintain the neck-shaft angle and prevent screw sliding and pull-out. Regarding fixation failure rates, the pooled results showed that LISS had no significant advantages over PFNA. Because fixation failure can be delayed, the different times recorded among the included studies may potentially introduce bias, and hence, a larger follow-up assessment may be required.
There are several potential limitations of this meta-analysis, which are listed as follows:
Only 7 publications met the eligibility criteria, which may have influenced on our conclusions.
The quality of the trials was acceptable, except that 1 RCT did not state the randomized method in detail, and in some of the trials, the demographic characteristics were unclear, which may introduce bias into the results.
There were invalid or ambiguous data of outcomes in 2 articles, which inhibited our ability to adequately perform all of our analyses.
The existence of publication bias, which is common to all meta-analyses, may have been unavoidable in our study.
However, this is the first systematic review to compare the advantages and disadvantages of PFNA and LISS in treating proximal femoral fractures. High-quality clinical trials are required to compare the optimality between PFNA and LISS. To some extent, the present study is meaningful for both clinical treatment and fundamental research.
CONCLUSIONS
The present meta-analysis indicates that compared with reverse LISS-DF, PFNA can reduce hospital stay and shorten time to weight-bearing ambulation and bone healing in treating proximal femoral fractures. In summary, the use of PFNA is safer and more effective than reverse LISS-DF in patients undergoing osteosynthesis for proximal femoral fractures. Nonetheless, in certain cases in which PFNA is not suitable due to abnormal structure of the proximal femur or particularly unstable fractures, such as damage involving the greater trochanter or lateral femoral cortex, the LISS plate technique could be a useful alternative.
Footnotes
Abbreviations: CCTs = case-controlled trials, LISS-DF = less invasive stabilization system–distal femur, MINORS = Methodological Index For Nonrandomized Studies, non-RCTs = nonrandomized controlled trials, PFNA = proximal femoral nail antirotation, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCTs = randomized controlled trials.
XJ and YW contributed equally to this work.
Authors’ contributions: XJ and XLM conceived and designed the study. XJ, JXM, and YW performed the study. CBZ, ZH, and LS analyzed the data. XJ, CW, and JXM wrote the manuscript. All authors read and approved the final manuscript.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Kannus P, Parkkari J, Sievanen H, et al. Epidemiology of hip fractures. Bone 1996; 18 (1 Suppl):57–63. [DOI] [PubMed] [Google Scholar]
- 2.Ma CH, Tu YK, Yu SW, et al. Reverse LISS plates for unstable proximal femoral fractures. Injury 2010; 41:827–833. [DOI] [PubMed] [Google Scholar]
- 3.Liu Y, Tao R, Liu F, et al. Mid-term outcomes after intramedullary fixation of peritrochanteric femoral fractures using the new proximal femoral nail antirotation (PFNA). Injury 2010; 41:810–817. [DOI] [PubMed] [Google Scholar]
- 4.Mereddy P, Kamath S, Ramakrishnan M, et al. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury 2009; 40:428–432. [DOI] [PubMed] [Google Scholar]
- 5.Simmermacher RK, Ljungqvist J, Bail H, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury 2008; 39:932–939. [DOI] [PubMed] [Google Scholar]
- 6.Kregor PJ, Stannard JA, Zlowodzki M, et al. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma 2004; 18:509–520. [DOI] [PubMed] [Google Scholar]
- 7.Ozkaya U, Bilgili F, Kilic A, et al. Minimally invasive management of unstable proximal femoral extracapsular fractures using reverse LISS femoral locking plates. Hip Int 2009; 19:141–147. [DOI] [PubMed] [Google Scholar]
- 8.Yao C, Zhang CQ, Jin DX, et al. Early results of reverse less invasive stabilization system plating in treating elderly intertrochanteric fractures: a prospective study compared to proximal femoral nail. Chin Med J (Engl) 2011; 124:2150–2157. [PubMed] [Google Scholar]
- 9.Marti A, Fankhauser C, Frenk A, et al. Biomechanical evaluation of the less invasive stabilization system for the internal fixation of distal femur fractures. J Orthop Trauma 2001; 15:482–487. [DOI] [PubMed] [Google Scholar]
- 10.Zlowodzki M, Williamson S, Zardiackas LD, et al. Biomechanical evaluation of the less invasive stabilization system and the 95-degree angled blade plate for the internal fixation of distal femur Fractures in human cadaveric bones with high bone mineral density. J Trauma 2006; 60:836–840. [DOI] [PubMed] [Google Scholar]
- 11.Lin YB, Li RB, Xiong GS, et al. Treatment of middle-up part long-segment femoral fracture with long proximal femoral nail antirotation”. Orthopaed Surg 2015; 7:138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Windolf J, Hollander DA, Hakimi M, et al. Pitfalls and complications in the use of the proximal femoral nail. Langenbecks Arch Surg 2005; 390:59–65. [DOI] [PubMed] [Google Scholar]
- 13.Tao ZG, Wei SW, Zhao YM, et al. A comparative study of three treatments of unstable intertrochanteric fracture. Chin J Orthopaed Trauma 2012; 14:108–112. [Google Scholar]
- 14.Gou Q, Yang ZY. PFNA and negative LISS plate in treatment of proximal femoral fractures compared effect. China Health Industry 2014; 9:1–2. [Google Scholar]
- 15.Tao R, Lu Y, Xu H, et al. Internal fixation of intertrochanteric hip fractures: a clinical comparison of two implant designs. Scientific World J 2013; 2013:834825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F, Zhang ZS, Yang H, et al. Less invasive stabilization system (LISS) versus proximal femoral nail anti-rotation (PFNA) in treating proximal femoral fractures: a prospective randomized study. J Orthop Trauma 2012; 26:155–162. [DOI] [PubMed] [Google Scholar]
- 17.Han N, Sun GX, Li ZC, et al. Comparison of proximal femoral nail antirotation blade and reverse less invasive stabilization system-distal femur systems in the treatment of proximal femoral fractures. Orthop Surg 2011; 3:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li J, Huang JH, Huo WL, et al. Efficacy analysis of reverse LISS and PFNA treatment of intertrochanteric fractures. Med Information 2013; 28:115–117. [Google Scholar]
- 19.Tang SL, Jiang C. Comparison of the effect of inverted less invasive stabilization system (LISS) and proximal femoral nail anti-rotation (PFNA) in the treatment of complex unstable intertrochanteric fracture in aged. China J Orthopaed Traumatol 2011; 24:366–369. [PubMed] [Google Scholar]
- 20.Davis BC, McConda DB, Hubbard DF, et al. Biomechanical evaluation of proximally placed femoral less-invasive stabilization system plates. Am J Orthop (Belle Mead NJ) 2015; 44:E54–E57. [PubMed] [Google Scholar]
- 21.Pryce LJ, Ashcroft GP. Reverse LISS plating for proximal segmental femoral fractures in the polytrauma patient: a case report. Injury 2007; 38:235–239. [DOI] [PubMed] [Google Scholar]
- 22.Yin ZG, Zhang JB, Gong KT. Cost-effectiveness of diagnostic strategies for suspected scaphoid fractures. J Orthop Trauma 2015; 29:e245–e252. [DOI] [PubMed] [Google Scholar]
- 23.Zlowodzki M, Williamson S, Cole PA, et al. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma 2004; 18:494–502. [DOI] [PubMed] [Google Scholar]
- 24.Kim JW, Oh CW, Byun YS, et al. A biomechanical analysis of locking plate fixation with minimally invasive plate osteosynthesis in a subtrochanteric fracture model. J Trauma 2011; 70:E19–E23. [DOI] [PubMed] [Google Scholar]
- 25.Ozkan K, Turkmen I, Sahin A, et al. A biomechanical comparison of proximal femoral nails and locking proximal anatomic femoral plates in femoral fracture fixation: a study on synthetic bones. Indian J Orthop 2015; 49:347–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shbaklo H, Kahn SR. Long-term prognosis after deep venous thrombosis. Curr Opin Hematol 2008; 15:494–498. [DOI] [PubMed] [Google Scholar]
- 27.Yang Y, Ma X, Ma J, et al. Biomechanical research of less invasive stabilization system and dynamic condylar screw in fixing subtrochanteric fractures of femur. Chin J Reconstruct Surg 2012; 26:1213–1217. [PubMed] [Google Scholar]
- 28.Fensky F, Nuchtern JV, Kolb JP, et al. Cement augmentation of the proximal femoral nail antirotation for the treatment of osteoporotic pertrochanteric fractures: a biomechanical cadaver study. Injury 2013; 44:802–807. [DOI] [PubMed] [Google Scholar]
- 29.Sahin EK, Imerci A, Kinik H, et al. Comparison of proximal femoral nail antirotation (PFNA) with AO dynamic condylar screws (DCS) for the treatment for unstable peritrochanteric femoral fractures. Eur J Orthop Surg Traumatol 2014; 24:347–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sermon A, Boner V, Schwieger K, et al. Biomechanical evaluation of bone-cement augmented Proximal Femoral Nail Antirotation blades in a polyurethane foam model with low density. Clin Biomech (Bristol, Avon) 2012; 27:71–76. [DOI] [PubMed] [Google Scholar]
- 31.Shen L, Zhang Y, Shen Y, et al. Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res 2013; 99:377–383. [DOI] [PubMed] [Google Scholar]
- 32.Tang P, Hu F, Shen J, et al. Proximal femoral nail antirotation versus hemiarthroplasty: a study for the treatment of intertrochanteric fractures. Injury 2012; 43:876–881. [DOI] [PubMed] [Google Scholar]
- 33.Helin M, Pelissier A, Boyer P, et al. Does the PFNA nail limit impaction in unstable intertrochanteric femoral fracture? A 115 case-control series. Orthop Traumatol Surg Res 2015; 101:45–49. [DOI] [PubMed] [Google Scholar]
- 34.Seyhan M, Turkmen I, Unay K, et al. Do PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures? A prospective clinical study. J Orthop Sci 2015. [DOI] [PubMed] [Google Scholar]
- 35.Takigami I, Ohnishi K, Ito Y, et al. Acetabular perforation after medial migration of the helical blade through the femoral head after treatment of an unstable trochanteric fracture with proximal femoral nail antirotation (PFNA): a case report. J Orthop Trauma 2011; 25:e86–e89. [DOI] [PubMed] [Google Scholar]
- 36.Zhou JQ, Chang SM. Failure of PFNA: helical blade perforation and tip-apex distance. Injury 2012; 43:1227–1228. [DOI] [PubMed] [Google Scholar]


