Abstract
Background
Alcohol and medications interactions are projected to increase due to the growth of older adults that are unsafely consuming alcohol and medications. Plus, aging adults who reside in rural areas are at the highest risk of experiencing medication interactions.
Objective
Estimate concurrent alcohol and medication (alcohol/medication) hospitalizations in adults 50+ years, comparing age groups and rural/urban regions.
Methods
Kentucky non-federal, acute care inpatient hospital discharge electronic records for individuals aged 50+ years from 2001 to 2012 were examined. Rate differences were estimated across age and regional strata. Differences in the underlying principal diagnosis, intent, and medications were also examined.
Results
There were 2,168 concurrent alcohol/medication hospitalizations among 50+ year olds identified. There was a 187% increase in alcohol/medication hospitalizations from 2001 (n=104) to 2012 (n=299). The per capita alcohol/medication hospitalization rate increased from 8.91 (per 100,000) in 2001 to 19.98 (per 100,000) in 2012, a 124 % increase. The characteristics of the hospitalizations included 75% principal diagnosis as medication poisoning, self-harm as the primary intent (55%) in 50–64 year olds, and unintentional intent (41%) in 65+ adults. Benzodiazepines were most often involved in the poisonings (36.5%).
Conclusions
Concurrent alcohol/medication hospitalizations in Kentucky are increasing among aging adults. Greater increases in rural areas and the 65+ aged adults were seen, although there were also higher alcohol/medication hospitalizations in urban and 50–64 aged adults. These findings indicate the need for public health prevention and clinical intervention to better educate and manage alcohol consuming older adults on safe medication and alcohol practices.
Keywords: Aging, alcohol, medication safety, mental health, substance misuse
1. INTRODUCTION
Prescription drug safety is a growing, yet undermanaged health issue. There has been a 24% increased risk of adverse drug reactions for older adults (1), and a 3000% increase in fatal medication errors related to alcohol and illicit drug use between 1983 and 2004 in the US, more so than deaths from either medication or alcohol/illicit drug use alone (2). Possible explanations for this increased risk of adverse drug events is the increase in older adults with concomitant use of alcohol and medications (3,4) the decreased medication metabolism with aging (5), and older adults being the highest consumers of medications (6). For instance, approximately 60% of adults use medications by age 60, nearing 90% by 80 years (7), and recent estimates indicating that among adults 65 years and older, 90% take at least one, 65% take three or more, and 39% take five or more prescription drugs (8) Additionally, 77% of 65+ years medication users take at least one alcohol-interactive medication (9).
Alcohol consumption is also fairly common with more than half of individuals report consuming alcohol in the past 30 days, 70% in the past year (10,11), and almost 88% reporting the consumption of alcohol in their lifetime (12). Excessive drinking is also fairly common in older adults, with almost 25% of older women and 50% of older men drinking above recommended drinking thresholds of 1+ drinks/day (13). Additionally, the risk of adverse alcohol events increase after the age of 50, due to decreases in gastric alcohol dehydrogenase, leading to raised blood alcohol concentrations in middle and old age (14,15). For instance, it has been estimated that older adults are hospitalized for alcohol-related complications as often as for myocardial infarctions (16) Furthermore, approximately half of 65+ year-old drinkers are consuming alcohol while also taking an alcohol interaction medication (17,18), with one-third consuming alcohol while having an alcohol sensitive condition (19). The combination of alcohol and medications can lead to: a) compromised medical treatment, b) injuries and negative health complexities (i.e., falls, cognitive impairment), and c) fatalities; thereby increasing morbidity, mortality, and health costs for older adults (2,20,21). Additionally, medication overdoses in older adults have been commonly associated with alcohol (22). Further concern comes from expected increases in drinking rates among future aging cohorts due to higher reported use of substances compared to earlier cohorts (23).
Such evidence lends support for the need to better understand recent trends of concurrent alcohol and medication (alcohol/medication) health incidents in aging adults. The development of programming to prevent concurrent alcohol/medication health incidents is considered a rural health priority (24), and aging adults who reside in rural areas are considered to be at highest risk of experiencing prescription drug misuse (25). This study sought to explore rural/urban differences due to existing evidence indicating rural health differences based on limited resources and accessibility (2628) greater burden of disease (29,30), and the rural culture of independence (31). In the present study, Kentucky hospital records were analyzed over time to: (a) estimate concurrent alcohol/medication hospitalization rates; (b) compare alcohol/medication hospitalization rates between urban and rural settings; (c) compare alcohol/medication hospitalization rates by age cohort between middle-aged (50–64 years) and older adults (65+ years) due to differences in health status and medication use. Greater concurrent alcohol/medication hospitalization rate increases are expected in older adults due to their greater medication use, and among rural adults due to their increased risks for medication misuse.
Kentucky is an appropriate setting to explore alcohol/medication incidents, because it has a 12% prevalence rate for heavy/binge drinking, 29% of driving deaths involving alcohol, and a rate of 20 drug poisoning deaths per 100,000 population (32). Additionally, 14.4% of the state population is 65+ years of age, only slightly more than the 14.1% 2013 US Census estimate (33). The near balanced population distribution among rural (46%) and urban (54%) that exists in the state of Kentucky (34) was examined to explore regional differences. Alcohol/medication hospitalization prevention is especially important in the 54 Appalachian counties (out of 120) in Kentucky, where prescription drug abuse is among the highest in the nation (35).
2. METHODS
2.1 Study Design and Data Source
In the present study, Kentucky hospital records were analyzed over time to: (a) estimate concurrent alcohol/medication hospitalization rates; (b) compare alcohol/medication hospitalization rates between urban and rural settings; (c) compare alcohol/medication hospitalization rates by age cohort between middle-aged (50–64 years) and older adults (65+ years). Kentucky inpatient hospital discharge uniform billing electronic records for state residents 50 years and older treated in Kentucky non-federal, acute care facilities from 2001 to 2012 were analyzed. Annual alcohol/medication hospitalization rates were calculated based on the actual count of alcohol/medication hospitalization occurrences (episodes of care) that year per 100,000 corresponding population (according to 2001–2012 census estimates (36)). All personal identifiers were removed from the data by the maintaining agency prior to receipt, as per human subjects approval. The data were coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (37). For each episode of care, the data contained a principal diagnosis, up to 24 secondary diagnoses, and three designated external-cause-of-injury (E-code) fields. The principal diagnosis is the primary physiological clinical assessment for the patient’s hospitalization. The E-code describes both the mechanism and intent of a presenting injury, for appropriate diagnoses such as alcohol or medication poisoning incidents.
2.2 Study Variables
2.2.1 Concurrent Alcohol and Medication Incident Diagnosis
This study aimed to estimate the concurrent alcohol/medication hospitalization rates. However, to our knowledge there were no medical record data obtained that contains this exact collective diagnostic information. Based on previous research (38,39) an operational definition was adapted where a concurrent alcohol/medication case was classified as 1) any diagnosis of medication drug poisoning (ICD-9-CM codes 960–979) {excluding poisoning by illicit drugs (965.00, 965.01, 968.5, 969.6, 970.81)}; AND 2) at least one of the following alcohol diagnoses: toxic effect of ethyl alcohol (980.0), excessive blood level of alcohol (790.3), alcohol dependence syndrome (303), alcohol abuse (305.0), or alcohol withdrawn delirium (291.0). Because these are independent diagnoses, no causality can be confirmed; there is no data indicating whether the alcohol caused the medication poisoning, or the medication use causing the alcohol poisoning. As defined in the Injury Surveillance Workgroup on Poisoning’s consensus recommendations, medication drug poisoning are considered overdose injuries (40) and were classified by intent based on a listed medication overdose E-code in the range E850–E858 (unintentional); E950.0–E950.5 (self-harm); E962.0 (assault); and E980.0–E980.5 (undetermined) with medication (substance) involved during poisoning event.
2.2.3 Age Groups
This study sought to compare rates by age cohort between middle-aged (50–64 years) and older adults (65+ years). Examining 50+ year olds is also appropriate, as gastric alcohol dehydrogenase, the enzyme that is responsible for alcohol digestion function starts approximately declining at age 50 (15). Also, the 50 and 65 year age breakdown to differentiate middle-aged and older adults is commonly used differentiate older adults groups (41).
2.2.3 Rurality Designation
To examine rural and urban differences at the individual level, counties were designated as rural or urban according to the 2013 Rural-Urban Continuum Codes (42) by the Economic Research Service of the US Department of Agriculture. The classification scheme distinguishes by their population size and metro adjacency to assigns each county to one of nine categories. For this study, metro is synonymous with urban (codes 1–3) and non-metro (codes 4–9) with rural.
2.4 Statistical Analysis
Multivariate Poisson modeling was used to examine the effect of time and age on alcohol/medication hospitalization counts. Wald tests were used to assess rate differences by age group. The analysis also examined the principal diagnosis for alcohol/medication hospitalizations, the intent, and medications involved using Fisher’s exact and Wald tests for structure of the count data. Further, the differences and effect of rural/urban geographic strata (defined by county of residence) on the alcohol/medication hospitalization rate were analyzed using Fisher’s exact tests for the former and Poisson regression for the latter. A p-value less than 0.05 denoted statistical significance. Version 9.3 of SAS software (SAS Institute Inc., Cary, NC, USA), RStudio Version 0.98.501, and Excel Version 14.3.8 were used for analyses.
3. RESULTS
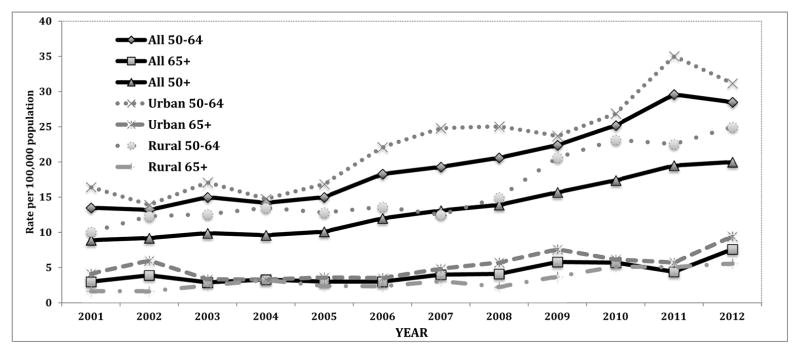
There were 2,168 concurrent alcohol/medication hospitalizations for subjects 50 years and older, treated in Kentucky acute care hospitals from 2001 to 2012. There was a 187.50% increase in the alcohol/medication hospitalizations from 2001 (n=104) to 2012 (n=299). The annual crude alcohol/medication hospitalization rate increased from 8.91 in 2001 to 19.98 in 2012, a 124.24% increase over the study period. The Poisson regression model identified a significant estimated increase of 9% (estimated incidence rate ratio (IRR): 1.09; 95% CI: 7% (1.07), 10% (1.10)) the alcohol/medication hospitalization rate per year. The crude rate for the 50–64 age group increased from 13.47 in 2001 to 28.49 in 2012, a 111.51% increase. The crude rate for the 65+ age group increased from 2.96 in 2001 to 7.65 in 2012, a 158.45% increase. Wald tests examining differences in alcohol/medication hospitalization rates indicated statistical significance (IRR: 1.09; 95% CI: 7% (1.07), 10% (1.10), P < 0.001) across age groups. Adults 65+ had significantly lower rates between 2001 and 2012 than 50–64 aged adults; the rates more than doubled over the time period for both groups (Figure 1). Poisson regression confirmed significant time and age effects on alcohol/medication hospitalization rates. Individuals aged 50–64 had 462% (IRR: 4.62; 95% CI: 408% (4.08), 524% (5.24)) the estimated occurrence rate of those aged 65+, adjusting for year of hospitalization. After adjusting for age, for each increase in year there was an estimated 8% increase (IRR: 1.08; 95% CI: 7% (1.07), 10% (1.10)) in the alcohol/medication hospitalization rate of the year prior.
Figure 1.
Concurrent Alcohol/Medication Hospitalization Rates Among 50+ Adults Residing in Kentucky, 2001–2012.
Principal Diagnosis Effects
Examining principal diagnoses over the 12-year study period, 74.72% of the identified alcohol/medication hospitalizations have a principal diagnosis of medication poisoning (Table 1). The number of alcohol/medication hospitalizations with a principal diagnosis of medication poisoning increased from 85 in 2001 to 225 in 2012, a 164.71% increase. Adults aged 65+ years had a significantly higher percentage of circulatory system and genitourinary diseases as principal diagnoses. Adults aged 50–64 had a higher percentage of drug/medication poisoning as the principal diagnosis. Overall, a principal diagnosis of mental disorder was listed in 14.94% of the cases, including 6.13% with episodic mood disorders, 1.80% with alcohol dependence, 1.06% with alcohol-induced mental disorders, 0.88% with non-dependent alcohol abuse, 0.83% with drug-induced mental disorder, 0.78% with adjustment reaction diagnosis, and 2.12% with other depressive mood disorders. Toxic effect of ethyl alcohol (diagnosis 980.0) was listed as principal diagnosis in 32 cases (1.48%).
Table 1.
Concurrent Alcohol/Medication Hospitalizations Among 50+ Adults Residing in Kentucky, by Principal Diagnosis.
| Principal diagnosis (ICD-9 codes) | Hospitalizations, 2001–2012 | ||
|---|---|---|---|
|
| |||
|
50–64a n=1885 (%) |
65+a n=283 (%) |
Fisher’s exact test P-value | |
| Mental disorders (290–319) | 287 (15.23) | 37 (13.07) | 0.37 |
| Diseases of the circulatory system (390–459) | 17 (0.90) | 7 (2.47) | 0.03 |
| Diseases of the respiratory system (460–519) | 42 (2.23) | 8 (2.83) | 0.52 |
| Diseases of the digestive system (520–579) | 24 (1.27) | <5b | -- |
| Diseases of the genitourinary system (580–629) | 6 (0.32) | 7 (2.47) | <.001 |
| Symptoms, signs, and ill-defined conditions (780–799) | 15 (0.80) | 6 (2.12) | 0.046 |
| Injury (800–959) | 7 (0.37) | <5 | -- |
| Poisoning by drugs, medicinal and biological substances (960–979) | 1428 (75.76) | 192 (67.84) | 0.01 |
| Toxic effects of substances chiefly nonmedicinal source (980–989) | 33 (1.75) | 9 (3.18) | 0.11 |
| Other diagnoses | 26 (1.38) | 10 (3.53) | 0.02 |
Note:
Patient’s age.
Counts less than 5 are suppressed by state data management policy.
Intent Effects
Examining intent, the majority (52.77%) of the medication poisonings were classified as intentional self-harm (i.e., suicide attempt, Table 2). Overall, unintentional medication poisonings was classified in 24.86% of cases, undetermined intent in 12.92% of cases, with missing intent in 9.46% of the hospitalizations. There was a significantly higher percentage of medication poisonings due to self-harm among middle-agers compared to the 65+ age group. The 65+ age group had significantly more unintentional medication poisonings compared to 50–64 age group.
Table 2.
50+ Adult Concurrent Alcohol/Medication Hospitalizations in Kentucky by Intent of the Medication Poisoning, 2001–2012.
| Intent (ICD-9 codes) | 50–64 Year Olds (n=1885) N (%) |
65+ Year Olds (n=283) N (%) |
Fisher’s exact test P-value |
|---|---|---|---|
| Self-Harm (Self-Inflicted Injury) | 1043 | 101 | <.001 |
| E950.0–950.5 | (55.33) | (35.69) | |
| Unintentional (Accidental Poisoning) | 424 | 115 | <.001 |
| E850.0–858.0 | (22.49) | (40.64) | |
| Undetermined Intent | 243 | 37 | 0.92 |
| E980.0–980.5 | (12.89) | (13.07) | |
| Missing Intent Code | 175 | 30 | 0.51 |
| (9.28) | (10.60) |
Medication Effects
Examining the medications involved in the poisoning hospitalization (Table 3), benzodiazepines were most often involved (35.84%), with similar levels across the age groups. Combination of prescription opioids and benzodiazepines were reported in 7.27% of the medication poisonings among patients aged 50–64 and in 5.30% in 65+. Anticoagulants were involved in significantly more poisonings in patients 65+ and antidepressants, barbiturates, sedatives, and hypnotics were present in significantly more poisonings among middle-agers.
Table 3.
Concurrent Alcohol/Medication Hospitalizations by Medication Type Contributing to the Poisoning Among 50+ Adults in Kentucky, 2001–2012.
| Medication type (ICD-9 codes) | 50–64a (n=1885) N (%) |
65+a (n=283) N (%) |
Fisher’s exact test P-value |
|---|---|---|---|
| Nonopioid analgesics, Antipyretics, and Antirheumatics | 219 | 29 | 0.55 |
| E850(.3–.8), 965(.1–.8) | (11.62) | (10.25) | |
| Opiates/Opioids | 294 | 47 | 0.66 |
| E850(.0–.2), 965.0: | (15.60) | (16.61) | |
| Subcategory: Methadone | 40 | 6 | 1.00 |
| E850.1, 965.02 | (2.12) | (2.12) | |
| Antidepressants, barbiturates and other antiepileptics, sedative, hypnotics, and psychotropic drugs not elsewhere classified E851–E853, E854(.0–.2,.8), E855.0, E950(.1–.3), E980(.1–.3), 966, 967, 969, 970(.0,.1,.89 |
1218 | 160 | 0.01 |
| (64.62) | (56.54) | ||
| Subcategory: Benzodiazepines | 688 | 89 | 0.11 |
| E853.2, 969.4 | (36.50) | (31.45) | |
| Subcategory: Psychostimulants | 25 | --b | -- |
| E854.2, 969.7 | (1.33) | ||
| Anticoagulants | 21 | 8 | 0.04 |
| 964.2 | (1.11) | (2.83) |
Note.
Patient’s age.
Counts and Percentages less than 5 are suppressed by state data management policy.
Rural Effects
Adjusting for rural/urban region, the estimated increase in alcohol/medication hospitalizations rate each year was 1.09 times (95% CI: 1.07, 1.10; P < .001) that of the previous year. Accounting for the alcohol/medication hospitalization year, older urban patients had an estimated 46% (IRR: 1.46; 95% CI: 34% (1.34), 60% (1.60)) incidence rate compared to older rural adults. Examining rural-urban differences, findings indicated that there was a 220.00% increase in alcohol/medication hospitalizations from 2001 (n=35) to 2012 (n=112) in older rural adults; a smaller increase of 171.01% was found for urban adults (2001: n=69; 2012: n=187). When comparing the annual crude rates, older rural adults experienced a 162.32% increase from 2001 (6.37 per 100,000) to 2012 (16.71 per 100,000), while older urban adults experienced a 102.15% increase (11.16 per 100,000 in 2001 and 22.56 per 100,000 in 2012). Further, urban middle-aged adults had significantly higher alcohol/medication hospitalization rates than their rural counterparts in 5 of the 12 years under study (2001, 2006–2008, 2011), while urban adults age 65+ only had a significantly higher rate in 1 year (2002) compared to rural adults 65+ (Figure 1).
Over the 12-year period, urban adults age 50–64 had the highest alcohol/medication hospitalization rate (23.0 per 100,000), followed by rural adults age 50–64 (16.5 per 100,000, data not shown). Both rural and urban adults age 65+ had lower alcohol/medication hospitalization rates than their ‘younger’ counterparts (3.1 per 100,000 and 5.4 per 100,000, respectively). When categorized by age (either 50–64 or 65+), urban adults had significantly higher alcohol/medication hospitalization rates compared to rural adults (50–64: P < 0.001; 65+: P < 0.0001). Comparing age groups among rural adults, those aged 50–64 had a significantly higher alcohol/medication hospitalization rate compared to aged 65+ adults (P < 0.001, data not shown). A similar result was found for urban patients (P < 0.001).
4. DISCUSSION
Findings indicated an increase in concurrent alcohol/medication hospitalizations among aging adults (aged 50+) in Kentucky, approximately 124% from 2001–2012. The increase was seen in both 50–64 aged adults with a 112% increase and 159% increase in the 65+ aged adults, with aged 50–64 year olds having 4.6 times the estimated rate of those aged 65+. The characteristics of the hospitalizations were chiefly medication poisonings, self-harm intent in middle-agers and accidental intent in older adults, with the involvement of benzodiazepines. There were increases over time in both rural and urban regions, with greater increase in the rural regions despite lower overall rates. Greater increases in rural areas and the 65+ aged adults were noted, yet there were higher rates in urban and 50–64 aged adults. This increase is similar to those identified in past studies examining national samples (2,38). Unique to this study was a focus on aging adults with the exclusion of an illicit drug use; accordingly the study results are focused on medication drug poisonings in middle and older adults. This evidence indicates a great need to address and prevent concurrent alcohol/medication incidents in hospital and community settings, and developing and using evidence based interventions in the area of alcohol and medication management. This case is particularly true for middle-agers that are aging into old age, as this study indicates that greater prevalence of alcohol/medication hospitalizations.
While the objective of the current study was not to identify causal mechanisms of alcohol/medication hospitalization rate change, the growth in alcohol/medication hospitalizations can be conceptually explained by 1) continuous alcohol consumption across the lifespan; 2) the aging of the baby boomers, with more liberal substance use behaviors; and 3) increased medication use with age. Specifically, research has indicated that alcohol consumption continues through old age despite guidelines to decrease drinking with age and disease onset, to no more than no more 1 drink per day (43). Also with the aging of the baby boomers comes a stronger culture of substance use including alcohol use (44). Another possible contributor to the growth of alcohol/medication hospitalizations, is the increase in medication use with aging without a matching increase in medication safety measures (6,7).
The rise in alcohol/medication hospitalizations make the case for increased public health attention and interventions to promote alcohol and medication safety in aging adults. Increased medication and regular alcohol use have not translated into medication safety health promotion priorities (45). Consequently, another explanation for the alcohol/medication hospitalization growth can be a result of limited knowledge about the dangers of combined alcohol and medication use (45). A medication safety health promotion campaign should address this issue by focusing on the health risks and outcomes associated with combined alcohol and medication use, including how alcohol consumption reduces medication compliance (46,47). In the US, the need for increased alcohol use screenings and medication instructions provided by pharmacists has been acknowledged when prescribing alcohol-interacting medications (21,48)
The growth in alcohol/medication hospitalizations can also be conceptually explained as a plausible mental health treatment crisis as indicated by mental disorders being the second most common identified principal diagnoses with self-harm being the most frequent intention in this study for middle-agers. For middle and older adults, mental illness can be particularly detrimental because it is under recognized, misrepresented, and under treated (49). Only half of all patients needing psychiatric treatment actively engage in recommended treatment regimens, and consequently experience increased morbidity and mortality, including suicide (50). Furthermore, alcohol and medications are often used to self-medicate underlying mental illness (51). There is also evidence that rural residents with a mental health disorder are at increased likelihood of also meeting criteria for a substance use disorder (52). Addressing mental health in rural areas is however challenging due to limitations in formal and informal medical care, including mental health management resources (53). In this context, there is a need for an increased focus on promoting high quality treatment and community living for individuals experiencing mental health issues in both rural and urban areas to prevent alcohol/medication hospitalization growth.
These results indicate that alcohol/medication hospitalizations have dramatically increased across middle and older adults in both rural and urban communities, however findings in this study need to be considered within some limitations. The results were based only on cases within Kentucky. However, research conducted in Kentucky is generalizable to at least 16.6 million Americans who also reside in similar Appalachian environments (54). Another limitation to consider is that the statistical analysis assumed independence of observations, which may not necessarily be the case because the study dataset only recorded number of occurrences, not the number of unique individuals. Future research needs to track validated unique individuals to verify the current results (55). Also as a caveat of the analysis, the study database only obtained up to nine diagnoses prior to 2005 and up to 25 diagnoses from 2005 forward. Therefore, data from 2001–2004 may have been underreported compared to 2005–2012 data. This underreporting in the earlier years could considerably contribute to the apparent increased alcohol/medication hospitalization rates, however graphic trends between 2005–2012 continued to show increasing trajectories. Also, the study analysis combined intentional with unintentional poisoning in the analysis. Future research should consider separately analyzing and comparing the risk factors within a larger database. Separate analysis for intentional with unintentional poisoning could also better explain the source of the increase. For example, a greater increase in intentional could indicate a mental health crisis and a greater increase in unintentional could indicate an educational/training problem. Finally there was no estimate of alcohol intake other than a diagnosis of alcohol morbidity in the current study. To obtain a more accurate understanding of alcohol and medication interactions future research should collect concurrent alcohol behaviors. Furthermore, to better understand trends, future research should examine causality between alcohol and medication poisoning, and compare concurrent trends between alcohol/medication hospitalization vs. alcohol and medication independent poisoning trends for middle-aged and older adults.
In conclusion, there is a growing wave of hospitalizations in Kentucky involving concurrent alcohol/medication use among adults aged 50 years and older. As a result, there is a need for interventions that can reduce alcohol and medication interactions in middle and older adults, particularly those adults that reside in rural regions. Future research needs to explore the increase in alcohol and medication use nationally and globally in aging adults, while considering more diverse populations, using unique individual cases, and developing, evaluating, and disseminating effective interventions across rural and urban areas to combat concurrent alcohol/medication health incidents.
KEY POINTS.
Increase in concurrent alcohol and medication hospitalizations among middle and older adults (aged 50+) in Kentucky, seen in both 50–64 and 65+ aged adults and both rural and urban regions, with greater increase in the rural regions despite lower overall rates.
Concurrent Alcohol and medication hospitalizations were chiefly self-harm medication poisonings and benzodiazepines were most often involved.
Alcohol and medication safety practices need to be enhanced for middle and older adults.
Acknowledgments
Funding
This work was supported by the National Institute of Health grant.
Footnotes
Declaration of interest: The authors report no declarations of interest.
References
- 1.Onder G, Landi F, Della, et al. Moderate alcohol consumption and adverse drug reactions among older adults. Pharmacoepidemiol Drug Saf. 2002;11(5):385–392. doi: 10.1002/pds.721. [DOI] [PubMed] [Google Scholar]
- 2.Phillips DP, Barker GE, Eguchi MM. A steep increase in domestic fatal medication errors with use of alcohol and/or street drugs. Arch Intern Med. 2008;168(14):1561–1566. doi: 10.1001/archinte.168.14.1561. [DOI] [PubMed] [Google Scholar]
- 3.Qato DM, Alexander GC, Conti RM, et al. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300:2867–2878. doi: 10.1001/jama.2008.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aira M, Hartikainen S, Sulkava R. Community prevalence of alcohol use and concomitant use of medication--a source of possible risk in the elderly aged 75 and older? Int J Geriatr Psychiatry. 2005;20(7):680–685. doi: 10.1002/gps.1340. [DOI] [PubMed] [Google Scholar]
- 5.Hayflick L. How and why we age. New York, NY: Ballantine Books; 1996. [Google Scholar]
- 6.Center for Substance Abuse Treatment. Substance Abuse Among Older Adults. Treatment Improvement Protocol (TIP) Series, Number 26. Rockville, MD: Substance Abuse and Mental Health Services Administration; 1998. (DHHS Publication No. (SMA) 98–3179) [PubMed] [Google Scholar]
- 7.Ihara E, Summer L, Shirey L. Challenges for the 21st Century: Chronic and Disabling Conditions. 5. Washington, DC: Center on an Aging Society, Georgetown University; 2002. Prescription drugs: a vital component of health care; pp. 1–5. Retrieved from http://ihcrp.georgetown.edu/agingsociety/pdfs/rxdrugs.pdf. [Google Scholar]
- 8.National Center for Health Statistics. Health, United States, 2014: With Special Feature on Adults Aged 55–64. Hyattsville, MD: 2015. Health, United States. Retrieved from http://www.cdc.gov/nchs/hus/special.htm. [PubMed] [Google Scholar]
- 9.Pringle KE, Ahern FM, Heller DA, et al. Potential for alcohol and prescription drug interactions in older people. J Am Geriatr Soc. 2005;53(11):1930–1936. doi: 10.1111/j.1532-5415.2005.00474.x. [DOI] [PubMed] [Google Scholar]
- 10.Zanjani F, Downer BG, Kruger TM, et al. Alcohol effects on cognitive change in middle-aged and older adults. Aging Mental Health. 2013;7(1):12–23. doi: 10.1080/13607863.2012.717254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS Prevalence & Trends Data [online] 2015 Retrieved from http://wwwdev.cdc.gov/brfss/brfssprevalence/
- 12.NIAAA. Alcohol Facts and Statistics. 2012 Retrieved from http://pubs.niaaa.nih.gov/publications/AlcoholFacts&Stats/AlcoholFacts&Stats.htm.
- 13.Moos RH, Schutte KK, Brennan PL, et al. Older adults’ alcohol consumption and late-life drinking problems: a 20-year perspective. Addiction. 2009;104(8):1293–1302. doi: 10.1111/j.1360-0443.2009.02604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanson VL. Technology skill and age: What will be the same 20 years from now? Universal Access in the Information Society. 2011;10(4):443–452. [Google Scholar]
- 15.Seitz HK, Egerer G, Simanowski UA, et al. Human gastric alcohol dehydrogenase activity: effect of age, sex, and alcoholism. Gut. 1993;34(10):1433–1437. doi: 10.1136/gut.34.10.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams W, Yuan Z, Barborial JJ, et al. Alcohol-related hospitalizations of elderly people. JAMA. 1993;270:1222–1225. [PubMed] [Google Scholar]
- 17.Immonen S, Valvanne J, Pitkälä KH. The prevalence of potential alcohol-drug interactions in older adults. Scand J Prim Health Care. 2013;31(2):73–78. doi: 10.3109/02813432.2013.788272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cousins G, Galvin R, Flood M, et al. Potential for alcohol and drug interactions in older adults: evidence from the Irish longitudinal study on ageing. BMC Geriatrics. 2014;14:57. doi: 10.1186/1471-2318-14-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnes AJ, Moore AA, Xu H, et al. Prevalence and correlates of at-risk drinking among older adults: the project SHARE study. J Gen Intern Med. 2010;25(8):840–846. doi: 10.1007/s11606-010-1341-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barry PJ, Gallagher P, Ryan C. Inappropriate prescribing in geriatric patients. Curr Psychiatry Rep. 2008;10(1):37–43. doi: 10.1007/s11920-008-0008-3. [DOI] [PubMed] [Google Scholar]
- 21.Jalbert JJ, Quilliam BJ, Lapane KL. A profile of concurrent alcohol and alcohol-interactive prescription drug use in the US population. J Gen Intern Med. 2008;23(9):1318–1323. doi: 10.1007/s11606-008-0639-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ødegård E, Rossow I. Alcohol and non-fatal drug overdoses. Eur Addict Res. 2004;10(4):168–172. doi: 10.1159/000079838. [DOI] [PubMed] [Google Scholar]
- 23.Patterson TL, Jeste DV. The potential impact of the baby-boom generation on substance abuse among elderly persons. Psychiatr Serv. 1999;50:1184–1188. doi: 10.1176/ps.50.9.1184. [DOI] [PubMed] [Google Scholar]
- 24.Averill JB. Priorities for action in a rural older adults study. Fam Community Health. 2012;35(4):358–372. doi: 10.1097/FCH.0b013e318266686e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shannon LM, Havens JR, Mateyoke-Scrivner A, et al. Contextual differences in substance use for rural Appalachian treatment-seeking women. Am J Drug Alcohol Abuse. 2009;35(2):59–62. doi: 10.1080/00952990802441394. [DOI] [PubMed] [Google Scholar]
- 26.Baernholdt M, Yan G, Hinton I, et al. Quality of life in rural and urban adults 65 years and older: findings from the National Health and Nutrition Examination survey. J Rural Health. 2012;28(4):339–347. doi: 10.1111/j.1748-0361.2011.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erwin PC, Fitzhugh EC, Brown KC, et al. Health disparities in rural areas: the interaction of race, socioeconomic status, and geography. J Health Care Poor Underserved. 2010;21(3):931–945. doi: 10.1353/hpu.0.0336. [DOI] [PubMed] [Google Scholar]
- 28.Wallace AE, Lee R, Mackenzie TA, et al. A longitudinal analysis of rural and urban veterans’ health-related quality of life. J Rural Health. 2010;26(2):156–163. doi: 10.1111/j.1748-0361.2010.00277.x. [DOI] [PubMed] [Google Scholar]
- 29.O’Connor A, Wellenius G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health. 2012;126(10):813–820. doi: 10.1016/j.puhe.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 30.Simmons LA, Huddleston-Casas CA, Morgan KA, et al. Mixed methods study of management of health conditions in rural low-income families: implications for health care policy in the USA. Rural Remote Health. 2012;12:1879. [PubMed] [Google Scholar]
- 31.Duggleby WD, Penz K, Leipert BD, et al. ‘I am part of the community but..’ The changing context of rural living for persons with advanced cancer and their families. Rural Remote Health. 2011;11(3):1733. [PubMed] [Google Scholar]
- 32.University of Wisconsin Population Health Institute. County Health Rankings 2015: Excessive Drinking. 2015 Retrieved from http://www.countyhealthrankings.org.
- 33.United States Census Bureau. State and County Quick Facts. 2015 Retrieved from http://quickfacts.census.gov/qfd/index.html.
- 34.State Health Facts. Demographics and the Economy. 2015 Retrieved from http://kff.org/statedata/
- 35.U.S. Department of Health and Human Services. Addressing Prescription Drug Abuse in the United States: Current Activities and Future Opportunities, Behavioral Health Coordinating Committee Prescription Drug Abuse Subcommittee. 2012 Retrieved from http://www.cdc.gov/drugoverdose/pdf/hhs_prescription_drug_abuse_report_09.2013.pdf.
- 36.United States Census Bureau. [Accessed September 24, 2013];Population Estimates – People and Households. Available at: http://www.census.gov/popest/index.html.
- 37. [Accessed September 7, 2013];International Classification of Diseases, 9th Revision, Clinical Modification, (ICD-9-CM) (6). Available at http://icd9cm.chrisendres.com/index.php.
- 38.White AM, Hingson RW, Pan IJ, et al. Hospitalizations for alcohol and drug overdoses in young adults ages 18–24 in the United States, 1999–2008: results from the Nationwide Inpatient Sample. Journal Studies Alcohol Drugs. 2011;72(5):774–786. doi: 10.15288/jsad.2011.72.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.White AM, MacInnes E, Hingson RW, et al. Hospitalizations for suicide-related drug poisonings and co-occurring alcohol overdoses in adolescents (ages 12–17) and young adults (ages 18–24) in the United States, 1999–2008: results from the Nationwide Inpatient Sample. Suicide Life Threatening Behavior. 2013;43(2):198212. doi: 10.1111/sltb.12008. [DOI] [PubMed] [Google Scholar]
- 40.Safe States. Consensus recommendations for national and state poisoning surveillance: report from the Injury Surveillance Workgroup (ISW7) Atlanta: Safe States; 2012. Also available from: : http://www.safestates.org/?page=ISWReports [cited 2014 Mar 7] [Google Scholar]
- 41.Blazer DG, Wu LT. Patterns of tobacco use and tobacco-related psychiatric morbidity and substance use among middle-aged and older adults in the United States. Aging Ment Health. 2012;16(3):296–304. doi: 10.1080/13607863.2011.615739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.United States Department of Agriculture Economic Research Service. Rural-Urban Continuum Codes. Washington, DC: [Accessed September 7, 2013]. Available at http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx#.UiuKHhYTHzI. [Google Scholar]
- 43.Moos RH, Schutte KK, Brennan PL, et al. Older adults’ alcohol consumption and late-life drinking problems: a 20-year perspective. Addiction. 2009;104(8):1293–302. doi: 10.1111/j.1360-0443.2009.02604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duncan DF, Nicholson T, White JB, et al. The baby boomer effect: changing patterns of substance abuse among adults ages 55 and older. Journal Aging Social Policy. 2010;22(3):237–248. doi: 10.1080/08959420.2010.485511. [DOI] [PubMed] [Google Scholar]
- 45.Zanjani F, Hoogland A, Downer B. Alcohol and Prescription Drug Safety in Older Adults. Drug, Healthcare, Patient Safety. 2013;5:13–27. doi: 10.2147/DHPS.S38666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glasglow N, Morton LW, Johnson NE. Critical issues in rural health. Ames, IO: Blackwell Publishing; 2004. [Google Scholar]
- 47.Fitzgerald N, Watson H, McCaig D, et al. Developing and evaluating training for community pharmacists to deliver interventions on alcohol issues. Pharmacy World Science. 2009;31(2):149–153. doi: 10.1007/s11096-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 48.Hale KM, Murawski MM, Huerta J. Pharmacist roles in combating prescription drug abuse. Journal American Pharmacists Association. 2009;49(5):589–592. doi: 10.1331/JAPhA.2009.09531. [DOI] [PubMed] [Google Scholar]
- 49.Mitchell AJ, Rao S, Vaze A. Do primary care physicians have particular difficulty identifying late-life depression? A meta-analysis stratified by age. Psychotherapy Psychosomatic. 2010;79(5):285–294. doi: 10.1159/000318295. [DOI] [PubMed] [Google Scholar]
- 50.Agyapong VI, Rogers C, Machale S, et al. Factors predicting adherence with psychiatric follow-up appointments for patients assessed by the liaison psychiatric team in the emergency department. International Journal Psychiatry Medicine. 2010;40(2):217–228. doi: 10.2190/PM.40.2.g. [DOI] [PubMed] [Google Scholar]
- 51.Harris KM, Edlund MJ. Self-medication of mental health problems: new evidence from a national survey. Health Services Research. 2005;40(1):117–134. doi: 10.1111/j.1475-6773.2005.00345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simmons LA, Havens JR. Comorbid substance and mental disorders among rural Americans: results from the National Comorbidity Survey. Journal of Affect Disorders. 2007;99(1–3):265–271. doi: 10.1016/j.jad.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 53.Parr H, Philo C. Rural mental health and social geographies of caring. Social Cultural Geography. 2003;4(4):471–488. [Google Scholar]
- 54.Murray CJ, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Medicine. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Perry IJ, Corcoran P, Fitzgerald AP, et al. The Incidence and Repetition of Hospital-Treated Deliberate Self Harm: Findings from the World’s First National Registry. PLOS One. 2012;7(2):1–7. doi: 10.1371/journal.pone.0031663. [DOI] [PMC free article] [PubMed] [Google Scholar]