Abstract
Combination chemotherapy is widely exploited for enhanced cancer treatment in clinic. However, the traditional cocktail administration of combination regimens often suffers from varying pharmacokinetics among different drugs. The emergence of nanotechnology offers an unparalleled opportunity for developing advanced combination drug delivery strategies with the ability to encapsulate various drugs simultaneously and unify the pharmacokinetics of each drug. This review surveys the most recent advances in combination delivery of multiple small molecule chemotherapeutics using nanocarriers. The mechanisms underlying combination chemotherapy, including the synergistic, additive and potentiation effects, are also discussed with typical examples. We further highlight the sequential and site-specific co-delivery strategies, which provide new guidelines for development of programmable combination drug delivery systems. Clinical outlook and challenges are also discussed in the end.
Keywords: Chemotherapy, combination, cancer, nanocarriers, drug delivery
1. Introduction
Cancer is the prominent cause of death worldwide and treatment for cancer remains one of the most challenging problems[1-6]. Current cancer treatments in clinic mainly rely on surgical intervention, radiation therapy and chemotherapy[7, 8]. Surgery remains the main treatment for cancer in which the bulk of the tumor is removed but the peripheral part cannot be completely eradicated due to the poor cellular differentiation in most of tumors[9-12]. In addition, surgery-induced acceleration of tumor and metastatic growth has been concerned, probably caused by inflammatory response during wound healing[13]. On the other hand, Chemotherapy provides an essential auxiliary treatment, while the efficacy is far from satisfaction mainly due to the drug delivery problems, including various types of physiological barriers as well as drug resistance[14-18]. Additionally, traditional chemotherapeutic drugs often harm healthy cells and cause toxicity to the patient[19-25].
The drug delivery systems (DDS) are expected to achieve easy drug administration, enhanced drug accumulation at tumor site, minimized side effects and optimized therapeutic efficacy[1, 26-30]. By taking advantage of profound understanding of cellular and molecular complexity of cancer and the availability of versatile materials, including synthetic polymers[31-34], lipids[35-39], inorganic materials[40-43], and biomacromolecule scaffolds[44-49], the DDS capable of delivering chemotherapeutics to tumor site have been developed enormously[50-54]. The emergence of nanotechnology has made profound impact on combination drug delivery and nanoparticles have been introduced as the drug carriers to achieve efficient chemotherapeutics delivery for decades. Compared with the direct administration of free drugs, encapsulation of drugs in nanocarriers provides distinct advantages, including better drug solubility[55-57], improved pharmacokinetic[58, 59] and pharmacodynamic properties[60, 61], prolonged circulation time[62, 63], minimized side effects[64], and sustained drug release kinetics[65, 66]. Furthermore, nanocarriers can protect a drug from quick clearance by evading the reticuloendothelial system; thus a high blood circulation profile enables transport through biological barriers and increases the availability of drug at the targeted disease site[28]. To date, an impressive library of nanoscaled DDS has been designed with varying sizes, architecture and surface physicochemical properties[67-71]. Typical nanocarriers in combination chemotherapy include polymeric nanoparticles[72, 73], liposomes[74, 75] and inorganic nanoparticles[76, 77].
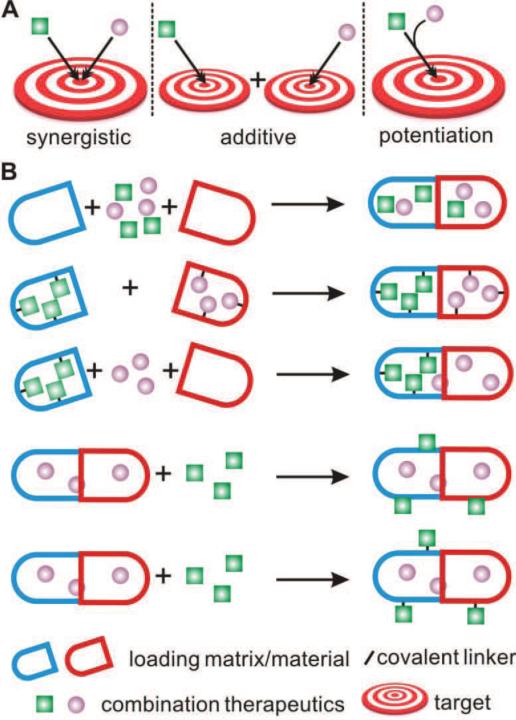
Due to the physiological complexity of the tumor, a single drug or even a stand-alone therapy strategy may not be sufficient for effective treatment[78, 79]. Combination chemotherapy, referring to the simultaneous administration of two or multiple therapeutic agents[80-83], is becoming increasingly important for achieving long-term prognosis and decreasing unwanted side effects[84-86]. Unlike monotherapy, combination chemotherapy can modulate different signaling pathways in cancer cells, cause synergetic responses, maximize the therapeutic effect and overcome drug resistance[87, 88]. As shown in Fig. 1A, the combination chemotherapy often achieves favorable outcomes through various mechanisms including synergistic effects, additive effects and potentiation effects. The discovery of new drug combinations and the development of novel drug combination systems can be facilitated when the specific mechanisms underlying activities have been fully elucidated. To fulfill effective delivery of multiple chemotherapeutics, the combination DDS can be designed through a variety of strategies (Fig. 1B) (Table 1). Loading of drugs into the nanoparticulate DDS can be achieved via the chemical conjugation, physical encapsulation or the combination of both methods. Partner drug can be covalently conjugated to the matrix and subsequently attached on the surface of drug-loading nanoparticle to form the combination DDS. Additionally, electrostatic interaction can also be applied to assemble combination DDS by taking advantage of opposed charged partner drugs and drugs-loading nanoparticles.
Fig. 1.
A. Schematic illustration of the mechanisms underlying combination chemotherapy, including synergistic effects, additive effects and potentiation effects. B. Popular implementations of co-encapsulating small molecular drugs in combination delivery systems. Drugs can be loaded into the co-delivery system through different implementations, including physical encapsulation + physical encapsulation, chemical conjugation + chemical conjugation, physical encapsulation + chemical conjugation, physical encapsulation + absorbance on the surface of formulation, physical encapsulation + conjugation on the surface of formulation (from top to down). The loading matrices/materials (in blue and red) can be either different or identical.
Table 1.
Summary of recently reported combination nanoparticulate drug delivery systems covered in this review.
| Implementation types | Nanocarrier approaches | Encapsulated drugs | Cancer types | Ref |
|---|---|---|---|---|
| Physical encapsulation + physical encapsulation | PLA nanoparticle | All-trans-retinoic acid (ATRA) + Dox | Breast tumors | 126 |
| Mesoporous silica nanoparticle | PTX + GEM | Pancreatic cancer | 146 | |
| PLGA nanoparticle | Tamoxifen (Tmx) + quercetin (QT) | Breast cancer | 150 | |
| Polymer-caged liposome nanobin | Pt + Dox | Ovarian cancer | 162 | |
| Mesoporous silica nanocapsule | CPT + Dox | Breast cancer | 164 | |
| PLGA nanoparticle | GEM + Pt | Bladder cancer | 166 | |
| Lipid bilayer coated silica nanoparticle | Dox + 5-FU + Pt | Liver cancer | 168 | |
| Lipid-polymer hybrid nanoparticle | 5-Fu + Oxa + CPT | Pancreatic carcinoma | 169 | |
| Liposome | Dox + curcumin | Melanoma | 171 | |
| Mesoporous Silica Nanoparticle | Dox + siRNA | Breast cancer | 181 | |
| Liposome | Erlotinib + Dox | Breast cancer and non–small cell lung cancer | 184 | |
| Physical encapsulation + chemical conjugation | PLGA nanoparticle | Dox + Dtxl | Prostate cancer | 56 |
| PLA nanoparticle | Pt(IV)] prodrug +Dtxl | Prostate cancer | 73 | |
| Nanocell composed of PLGA nanoparticle | Dox + Combretastatin A4 | Melanoma | 127 | |
| Telodendrimer nanoparticle | Pt + PTX | Ovarian cancer | 143 | |
| Dextran nanoparticle | Pt + Dox | Non-small cell lung cancer | 156 | |
| Polymeric nanoparticle | CPT + Dox | Non-small cell lung cancer | 165 | |
| Micelle | Dox + disulfiram (DSF) | Breast cancer | 174 | |
| Micelle | Dox + siRNA | Breast cancer | 182 | |
| PLGA nanoparticle | Pt prodrug + siRNA | Prostate Carcinoma | 183 | |
| Graphene | TRAIL + Dox | Non–small cell lung cancer | 190 | |
| Chemical conjugation + chemical conjugation | Micelle | Pt(IV) + PTX | Ovarian cancer, cervical cancer | 142 |
| Self-assembled nanoparticle | Chlorambucil (Cb) + irinotecan (Ir) | Breast cancer | 147 | |
| Polymeric nanoparticle | Dox + wortmannin (WOR) | Breast cancer | 163 | |
| Polymeric nanoparticle | Pt + Dox + CPT | Ovarian carcinoma | 170 | |
| Physical encapsulation + electrostatic absorbance | Micelle | PTX + Dox | Non-small cell lung cancer | 124 |
| Gel-liposome | TRAIL + Dox | Breast cancer | 189 |
In this review, nanocarrier-based combination delivery of cocktail small-molecular chemotherapeutics will be surveyed. The mechanisms underlying actions and co-delivery strategies for combination therapy, including synergistic combination effects, additive combination effects, and potentiation combination effects, will be summarized in details. We will further introduce the sequential and site-specific co-delivery strategies, which provide new insights for development of programmable combination drug delivery systems. Finally, the future opportunities and challenges of delivery of cocktail chemotherapeutics will be discussed.
2. Chemotherapy and combination chemotherapy in cancer
Cancer chemotherapy refers to using chemical substances to treat tumor[9, 89]. The history of chemotherapy could be traced back to 1940s when nitrogen mustards and antifolate drugs were first introduced[90, 91]. Since then, chemotherapy has played a vital role in the auxiliary treatment of cancer and gained extensive development. However, it is generally accepted that cancer is usually the result of a combination of interconnected disease pathways that may not be treated effectively with a single therapeutic agent or strategy[92-95]. The emergence of drug resistance and tumor recurrence is often associated with the single drug based cancer chemotherapy, mainly due to pathway overlapping[96], cross-talk[97] and neutralizing response[98, 99] that commonly occur with cancer monotherapy. Nowadays, the well-established combination therapy for cancer treatment provides effective solutions for the dilemma.
The combination chemotherapy has evolved into a reasonably scientific clinical treatment from the preliminary trials. Several important principles are involved in the combination chemotherapy, including non-overlapping toxicity, non-cross resistance and enhancement of tumor cell killing efficacy[100]. Traditional drug combinations for cancer therapy include methotrexate-based combinations, anthracyline-based combinations and paclitaxel (PTX)-based combinations[101, 102]. Methotrexate, an antimetabolite and antifolate drug, is often combined with cyclophosphamide and 5-fluorouracyl (5-FU) for traditional combination chemotherapy due to the capability of inhibiting the metabolism of folic acid[103, 104]. Anthracyline-based chemotherapeutics, including daunorubicin, doxorubicin (Dox), epirubicin, idarubicin and valrubicin, plays a vital role in combination with cyclophosphamide and 5-FU. Cyclophosphamide inhibits the DNA replication by forming intrastrand and interstrand DNA crosslinking[105], while 5-FU acts as a thymidylate synthase inhibitor to prevent DNA replication[106]. PTX-based combinations are another commonly used traditional chemotherapy. For example, PTX and cisplatin (Pt) were combined for advanced ovarian cancer therapy and PTX was also combined with carboplatin for advanced non-small cell lung cancer (NSCLC) in clinic[107-109]. Currently, new multi-drug combination chemotherapies or modifications of established regimes are being clinically tested and variations of the administration strategies are also explored to improve therapeutic efficacy with minimized side effects[110-112].
In addition to these clinical studies, exciting preclinical studies aiming at exploring new combinations strategies and improving combination effect have been developed. These new combination strategies provide new insights into the molecular and cellular mechanisms underlying the effects of combination treatments. For example, Dox and rapamycin co-delivery could effectively reverse chemotherapeutic drug resistance and re-establish growth and death patterns that are often misregulated in tumor cells. The tumor bearing animals treated with such combination chemotherapy exhibited a complete tumor remission, while the animals treated with rapamycin or Dox alone did not show any evidence of complete remission[113]. Additionally, with the development of nanotechnology, researchers recruited the nanoparticles for combination chemotherapy with the merits of co-encapsulation of hydrophobic and hydrophilic drugs[73], adjustable ratiometric drug loading, spatiotemporally controlled release behavior[114] and stimuli-responsive properties[115].
3. Mechanism underlying combination chemotherapy
Understanding of the molecular and cellular mechanisms of combination chemotherapy provides guidelines to assist the discovery of new combination candidates and new combination strategies. Multiple chemotherapeutics can function in the same or different pathways, and their regulation results into different effects via drug-targets interaction, target-target overlapping, pathway-pathway crosstalk and drug-drug interaction[116]. In addition, the treatment efficacy can be compromised if negative regulation of drug combination and neutralizing responses happen, leading to drug resistance[101, 117]. Thus, specific mechanisms of action of partner drug and combination chemotherapy strategies need to be fully elucidated for the rational design to achieve optimal efficacy.
When two drugs are administrated simultaneously, the combination of their therapeutic effects can generate the combinatorial effect with higher, equal to or lower than the summed effects of the partner drugs. The combination is pharmacodynamically synergistic when the effect is greater than the summed effect of the individual drugs and the target of the each drug is located at the different sites or different pathways; the combination effect is additive when the effect is greater than or equal to the summed effect of the partner drugs and each individual drug takes effects at the same target or the same pathway; potentiation effects can be produced on the circumstance that the therapeutic effect/activity of one drug is enhanced or the side effect is reduced by another drug via regulation of its absorption, distribution, metabolism and excretion (ADME)[101, 118].
The synergistic, addictive and potentiation drug combinations have been particularly explored through “nanomedicine” to achieve a variety of favorable outcomes, including decreased dosage of partner drugs, enhanced efficacy, prevention of the development of drug resistance, and reduction of unwanted side effects. In this part, these three typical combination effects mechanisms underlying the co-delivery strategies are summarized in the light of recent developments.
3.1. Synergistic combination effects
The synergistic combination effects refer to the complementary actions of drug combination by targeting multiple sites of a pathway or different pathways, resulting in collective regulation of targeting activity and simultaneous enhancement of the positive effects or reduction of negative effects[119]. To fully demonstrate the synergistic effects underlying combination chemotherapy, the most widely used small-molecular drugs—Dox and PTX are selected as model chemotherapeutics to illustrate the synergistic mechanism.
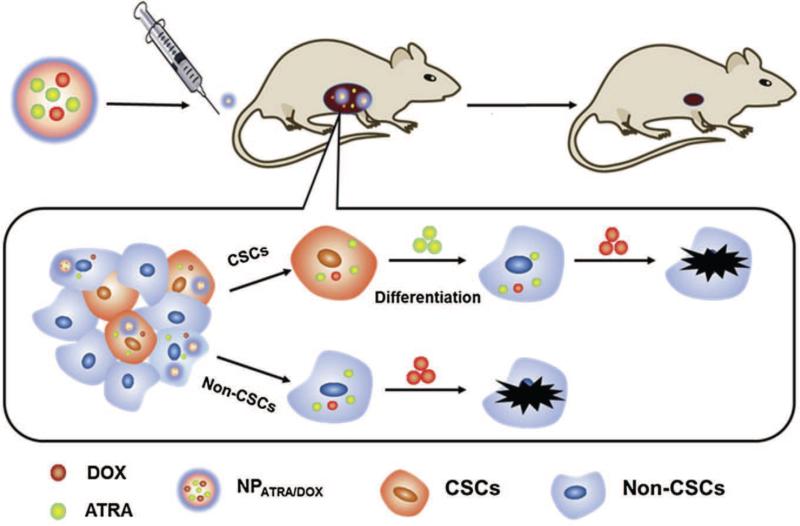
Dox, a member of the anthracycline-based chemotherapeutics, is one of the first chemotherapeutics for cancer treatment and utilized in treatment of a variety of cancers, including breast cancer, myeloma, lung cancer, glioma, leukemias, and lymphoma[120, 121]. However, Dox is known to cause a well-described severe cardiotoxicity, which is dose-dependent[122, 123]. The combination drug delivery strategies have therefore attracted broad attentions and achieved enormous developments in combination with other chemotherapeutics for synergetic effect to reduce unwanted severe side effects associated with Dox[124, 125]. Sun et al. reported an approach to co-deliver all-trans-retinoic acid (ATRA) and Dox for cancer therapy, especially for synergetic inhibition of cancer stem cells (CSCs) (Fig. 2)[126]. ATRA, a powerful differentiating agent, inhibits multiple signaling pathways that are critical for stem cell maintenance. However, ATRA does not present obvious cytotoxicity and tumor inhibition capability when administrated alone. In their study, it was demonstrated that co-delivery of ATRA and Dox could differentiate and inhibit the proliferation of tumor cells by delivering chemotherapeutics to both non-CSCs and CSCs. Meanwhile, a decreased systemic toxicity was achieved, which was enabled by the reduction of the concentration of required Dox at equal therapeutic efficacy. By taking advantage of this combination DDS, the accumulation of chemotherapeutics was significantly enhanced in tumor tissues and CSCs, resulting in remarkable suppression of tumor growth while reducing the incidence of CSCs in a synergistic manner. Additionally, it was found that the percentage of the CSCs population in ATRA-Dox-NP-treated group (1.7%) significantly decreased when compared with that of groups treated with Dox-NP (8.1%) and ATRA-NP (2.8%), indicating the synergistic effects in CSCs inhibition.
Fig. 2.
Schematic of the co-delivery of ATRA and Dox to eliminate both CSCs and non-CSCs. Reprinted with permission from [126].
Another emerging implementation to decrease Dox-associated side effect via synergistic combination effect is to combine traditional Dox-based chemotherapy with anti-angiogenesis agents that inhibit tumor blood vessel growth and cut the supply of nutrition and oxygen to tumor. For example, Sengupta et al. developed a nanocell drug delivery system, which was comprised of a core nanoparticle protected by an pegylated-lipid-based shell[127]. Two drugs—Combretastatin A4 and Dox were co-encapsulated in the nanocell and released out sequentially. The release of Combretastatin A4 from the outer shell could shut down the vascularization of tumor. The core of the nanoparticle, which was trapped inside the tumor, then released Dox. A synergistic combination effect with a rapid collapse of tumor blood vessels and inhibition of proliferation of tumor cells both in vitro and in vivo was achieved via the nanocell-based co-delivery system.
PTX, extracted from the bark of the western yew tree—Taxus brevifolia[128], is another widely used chemotherapeutic. The mechanism underlying the action of PTX relies on the interference with the normal breakdown of microtubules during the cell division[129-131]. PTX has been approved by FDA for treating a number of different tumors, including breast cancer, lung cancer, head and neck cancer, gastrointestinal cancer, and ovarian cancer[132]. Small-molecular PTX has limited aqueous solubility. To improve solubility and realize in vivo delivery, PTX was initially formulated as a Cremophor/ethanol-based solution (marketed as Taxol)[133, 134]. The major drawback of Cremophor/ethanol-based PTX solution is the potential induction of an acute hypersensitivity reaction, resulting in severe allergic responses[135, 136]. Nanocarriers for the delivery of PTX have drawn increasing interest for their ability to deliver PTX in the optimal dose with enhanced solubility. However, the monotherapy often results in the drug resistance of cancer cells, which plays a vital role in the failure of clinical cancer treatment. Nowadays, the interest of using PTX as the therapeutic agent has shifted to the combination with other anticancer chemotherapeutics[137, 138]. For example, a nanoparticulate DDS comprised of an amphiphilic methoxy poly(ethylene glycol)-b-poly(L-glutamic acid)-b-poly(L-lysine) triblock copolymer and deoxycholate (mPEsG-b-PLG-b-PLL/DOCA) decoration was developed to co-deliver anticancer drugs—PTX and Dox[124]. The micelle nanoparticles self-assembled from the amphiphilic copolymers provided three different domains with distinct functions: prolonged circulation time enabled by PEG chain, encapsulation of Dox via electrostatic interactions, and loading of PTX in hydrophobic deoxycholate modified copolymer. The synergistic effect in the induction of A549 human lung adenocarcinoma cell apoptosis was achieved by the co-delivery formulation and evidenced by in vitro cytotoxicity assays. Ex vivo fluorescence imaging revealed that co-delivery DDS selectively targeted and efficiently accumulated at the tumor site in vivo. Furthermore, Wang et al. reported a core-shell nanoparticle co-encapsulated with PTX and Dox, which were doubly emulsified from an amphiphilic copolymer methoxy poly(ethylene glycol)-poly(lactide-coglycolide) (mPEG-PLGA)[125]. Enhanced uptake of both drugs by cancer cells and simultaneously promoted drug release was obtained in in vitro cellular experiments. Additionally, the co-delivery DDS suppressed tumor cells growth more efficiently than the single delivery of either Dox or PTX at the same concentrations, which was evidenced by the reduced tumor size that was 3.2-fold, 6.3-fold and 2.4-fold smaller than that treated with Dox, PTX and combination of free Dox and PTX, respectively.
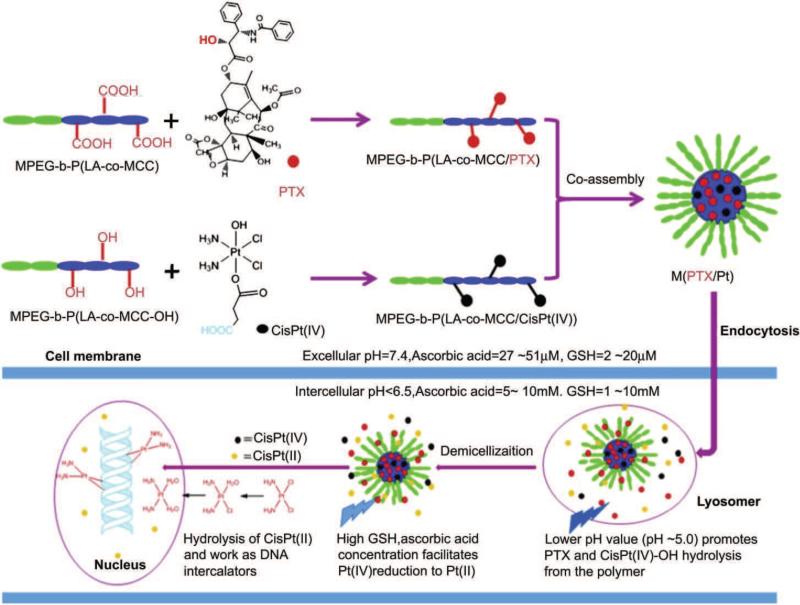
In addition to Dox, Pt is often co-delivered with PTX to achieve synergistic antitumor effect. Pt, one of the most potent antitumor agents, causes DNA damage by the interaction with DNA to form intrastrand crosslinked DNA adducts[139]. Pt has always been combined with PTX in clinical and preclinical treatment of gynecological tumors, such as ovarian and cervical cancers[140, 141]. For example, Xiao et al. co-encapsulated the Pt prodrug and PTX in a nanomicelle (Fig. 3)[142], which could selectively release Pt upon redox and PTX via acid hydrolysis after endocytosis by cancer cells. In vitro 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay showed that the IC50 of Pt alone and PTX alone were 27.2 μM and 58.3 μM, respectively, whereas the IC50 of Pt and PTX in the co-delivery system were 16.7 μM and 1.67 μM against SKOV-3 cells. The decreased drug concentrations of Pt and PTX in combination therapy indicated a synergistic effect. Additionally, in vivo study displayed that Pt prodrug and PTX co-encapsulated DDS displayed more efficacious inhibition of U14 tumor growth and reduced systemic toxicity compared to small-molecular drug combinations. In another study, Cai et al. developed a telodendrimer-based nanocarrier for co-delivery of PTX and Pt to treat ovarian cancer[143]. In their system, a three-layered linear-dendritic telodendrimer micelle (TM) was synthesized by introducing carboxylic acid groups in the adjacent layer for Pt complexation and conjugating cholic acids in the interior layer of telodendrimer for PTX encapsulation. A strong synergistic anticancer effect was gained with decreased IC50 values of PTX and Pt (loading ratio of 1:2), respectively. After administration in the ovarian cancer SKOV-3 xenografted nude mice, the clearance rate of PTX/Pt-TM was about 20-fold lower than that of free drugs and the accumulation of PTX/Pt-TM was 4-fold higher than that of free drug Pt, which resulted in enhanced antitumor efficacy compared to the free drug combination or nanoparticle loaded with a single drug.
Fig. 3.
Preparation of the PTX and Pt co-delivery micelle and the anti-cancer mechanism underlying the combination effects. Reprinted with permission from [142].
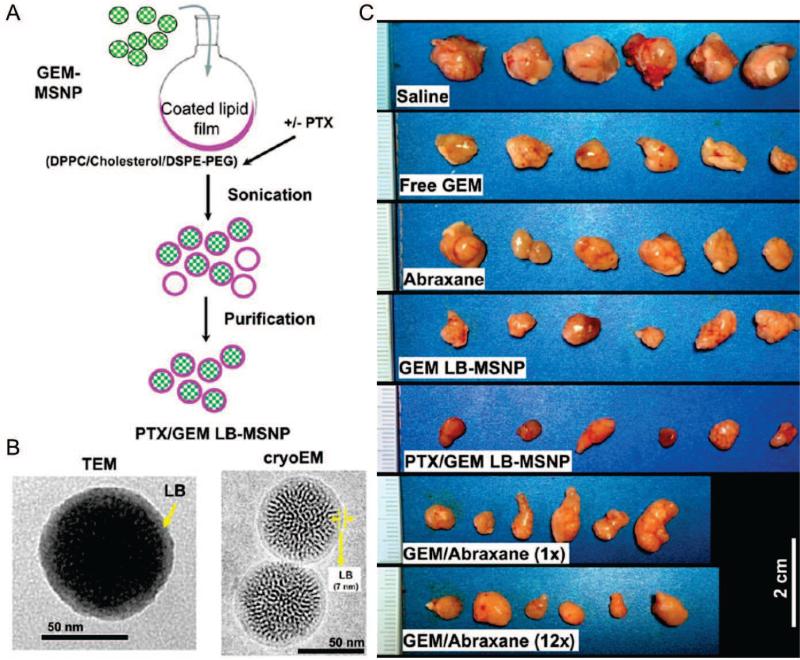
Gemcitabine (GEM), which is phosphorylated by deoxycytidine kinase to interfere DNA synthesis after endocytosis[144, 145], is frequently used as the first-line therapy in clinical treatment for pancreatic cancer. However, the rapid emergence of drug resistance significantly limited the application of GEM. It was found that PTX could improve the sensitivity of tumor cell when used in combination with GEM. In a phase 1-2 trial, GEM was co-administrated with albumin-bound PTX (nab-PTX) to patients with advanced pancreatic cancer. The results showed that the overall survival, progression-free survival, and response rate had been significantly improved in combination therapy. Furthermore, PTX and GEM combination therapy showed extensive potential when integrated with nanotechnology in preclinical studies. Meng et al. proposed a lipid-coated mesoporous silica nanoparticle (LB-MSNP) for co-delivering PTX and GEM to pancreatic cancer[146]. The LB-MSNP was comprised of a supported lipid bilayer (LB) and MSNP carrier. The attachment of LB provided the high loading capacity of GEM in MSNP as well as efficient co-entrapment of hydrophobic drug PTX (Fig. 4A). The resulting LB-MSNP displayed a uniform coating with an intact LB on the surface of MSNP, which was essential for encapsulation and controlled release of drugs (Fig. 4B). The LB-MSNP was demonstrated to show a sustained release profile with 22.9% cumulative release of GEM within 48 h. The administration of GEM-PTX-LB-MSNP was able to increase active GEM concentration at tumor site by 15-fold, resulting in effective inhibition of primary tumor growth (Fig. 4C), which was evidenced by increased the terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) positive cells in tumor tissue (36% for GEM-PTX-LB-MSNP, 16% for free GEM, 17% for GEM + 1 × dose of Abraxane and 23% for GEM-LB-MSNP).
Fig. 4.
A. Schematic illustration of the preparation of PTX and GEM co-encapsulated LB-MSNP. B. TEM and cryoTEM images of PTX-GEM-LB-MSNP at the ratio of 10:1 (PTX:GEM). C. In vivo antitumor efficacy evaluation after treatment with various drug formulations. Reprinted with permission from [146].
In addition to these commonly used chemotherapeutics, a variety of other drugs have also been paired. For instance, Huang et al. developed a nanoparticle self-assembled from an amphiphilic drug-drug conjugate with the co-encapsulation of the hydrophilic anticancer drug irinotecan (Ir) and the hydrophobic anticancer drug chlorambucil (Cb) using a hydrolyzable ester linkage[147]. Ir prevents the replication and transcription of DNA via the inhibition of topoisomerase 1[148], While Cb functions as alkylating agent to crosslink macromolecules[149]. The co-delivery nanoparticulate DDS exhibited longer blood circulation time, increased cellular uptake and enhanced accumulation at tumor site compared to the free drugs. In addition, the co-delivery system exhibited a stronger apoptosis inducing capability with the apoptosis rate of 76.78% when compared to the free drug combination and individual drugs. Additionally, tamoxifen (Tmx) and quercetin (QT) were paired in a PLGA nanoparticle with 67.16% ± 1.24% encapsulation efficiency for Tmx and 68.60 ± 1.58% for QT[150]. Tmx is the gold standard in the clinic for the endocrine treatment of the estrogen receptor positive breast cancer[151, 152]. QT acts as the antiproliferative agent to induce apoptosis via caspase activation and to inhibit the enzyme that is response for activating carcinogens[153]. It was found that the cytotoxicity of Tmx-QT-NP was 34.13-, 33.3-, and 24.74-fold stronger than that of free Tmx, free QT, and free drug combination, respectively. In vivo antitumor growth study showed that the tumor size decreased to 32.36% (compared to original size at day 0) with the treatment of Tmx-QT-NP, which was significantly smaller than that treated with free Tmx citrate + QT (56.62%) and saline (149.18%). Their findings demonstrated the superiority of combination chemotherapy in the nanoparticle delivery system. The involvement of these small-molecular drugs can further broaden the design flexibility and scope of applications by endowing the combination system with a vast drug library.
3.2. Additive combination effects
The additive combinations effect, different from synergistic effect, results from equivalent or overlapping actions, which involves the direct or indirect regulations or interactions with the targets at the same site, different sites at the same pathway or crosstalk pathway[101, 154]. For example, the retinoic acid and trichostatin A combination provides an additive effect to inhibit cancer cell proliferation by combining effects of upregulating retinoic acid receptor β and reactivating of the mRNA expression[155]. In addition, the independent actions at different sites of the same target or pathway can also be defined as additive combination effects. For instance, Dox and Pt produce an additive anticancer effect via equivalent action of DNA intercalation and distinct interference in DNA activity. Both drugs bind to DNA in a non-interfering manner[156]. Dox, which prefers GC regions, intercalates into DNA to inhibit the macromolecular biosysthesis and the bioactivity of topoisomerase II (TOP2A)[120], and Pt prefers binding to guanine and subsequently forms the crosslinking of DNA[157]. The better exploration of additive effects could also facilitate the development and design of synergistic drug combination.
Nucleus serves as the ideal target for drug combination with additive effects, since DNA provides abundant targets for drugs to generate the overlapping actions or equivalent actions at the same pathway or cross-talk pathway[158]. As the repository of the hereditary material of the cell, nucleus coordinates all sorts of cellular activities, which include growth, cellular metabolism, protein synthesis, and cell division[159, 160]. Thus, nucleus serves as the most important target for the additive combination therapy due to its vital role in the cancer cell proliferation and progression[161].
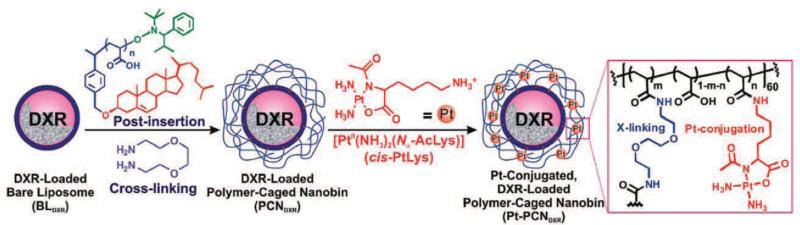
Dox is the most employed small-molecular model chemotherapeutics that is developed to target nucleus in combination of other drugs for the additive anticancer efficacy. Two strategies are often utilized to load Dox into the delivery system: physical encapsulation and chemical conjugation. Physical encapsulation of Dox results in quicker drug release compared to chemical conjugation of Dox to the polymer backbone; while the sustained and spatiotemporally controlled release behavior can be achieved by chemical conjugation of Dox, with the potential of responsiveness to various physiological signals. To date, researchers have developed various delivery systems to encapsulate Dox. For example, Lee et al. exploited a polymer-caged nanobin to co-deliver Pt and Dox (Fig. 5)[162]. In their system, Dox was loaded into a liposomal core, which was further protected by a pH-responsive Pt prodrug-loaded polymer shell. Besides, the polymer-caged nanobin held the potential to tune drug encapsulation ratio and surface charge potentials. In ovarian cancer cell, Pt/Dox-nanobin at a Pt/Dox molar ratio of 5.9 showed increased cytotoxicity with lower doses of Pt and Dox (IC50 Dox = 0.9 μM, IC50 Pt = 7.1 μM) compared to free Dox and Pt (IC50 Dox = 1.24 μM, IC50 Pt = 66.1 μM), which was contributed to an additive mechanism of combination therapy.
Fig. 5.
Preparation of platinum-conjugated, Dox-loaded polymer-caged nanobin. Reprinted with permission from [162].
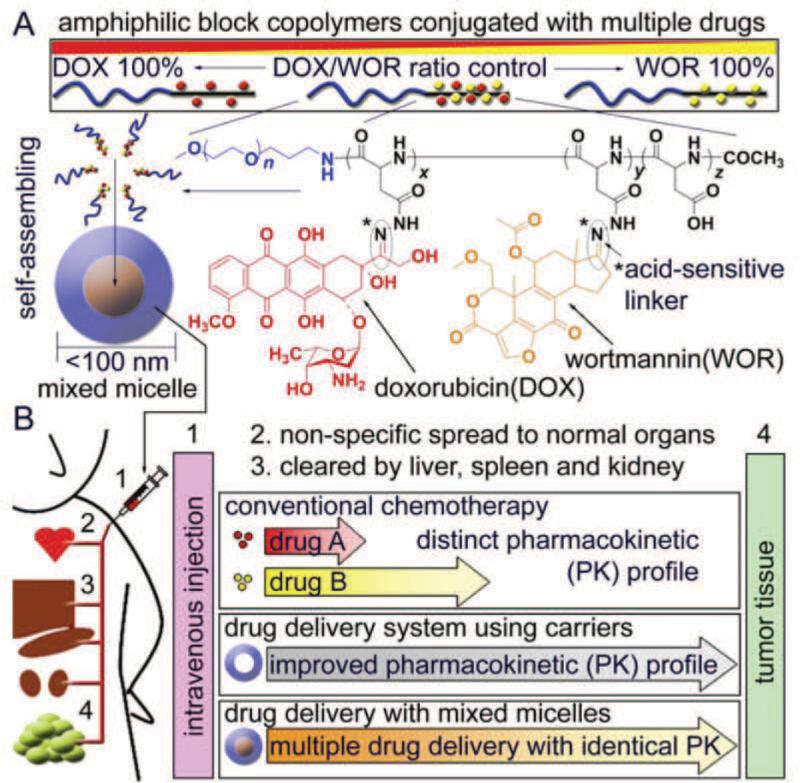
Bae et al. took a different approach to encapsulate Dox and wortmannin (WOR), which is phosphatidylinositol-3 kinase inhibitor involving in DNA repair. In the study, Dox and WOR were chemically conjugated to the poly(ethylene glycol)-poly(aspartate hydrazide) block copolymer(Fig. 6) [163]. This amphiphilic copolymer conjugated with drugs could self-assemble into micelle structure with precisely control of Dox/WOR ratio. Additionally, the facile control of Dox and WOR release was achieved via the acid-sensitive hydrazine linker. It was demonstrated that the proliferation of MCF-7 cells exposed to Dox/WOR co-encapsulated micelle was effectively inhibited. Of note, the partner drug concentration at the same treatment efficacy was significantly reduced by co-delivering Dox and WOR in the micelle when compared to the individual drug mixture. Zhang et al. encapsulated the small molecule hydrophobic drug—docetaxel (Dtxl) and the hydrophilic drug—Dox in a nanoparticle delivery system[56]. The novel DDS was comprised of 1) aptamers with the ability to promote the release of Dox and target cancer cell on the surface, and 2) polymeric nanoparticle core that served as the container for Dtxl. The aptamers provided the preferred binding site for Dox, which were further conjugated on the surface of Dtxl-encapsulated polymeric nanoparticles. The cumulative release ratios of Dtxl were about 50% and 80% at the first 6 and 25 h, respectively. In contrast, a fast release profile was observed for Dox loading into the aptamer, with 50% and 80% cumulative release within 4 and 6 h, respectively. The difference in the release behaviors of Dtxl and Dox could be explained by the distinct loading mechanisms. The release of Dox, which was loaded into aptamers via the intercalation into GC regions, was accelerated by exposure to outside aqueous solution. Additionally, the cell viability assay showed that Dtxl/Dox co-delivery nanoparticle displayed the enhanced cytotoxicity against LNCaP cells compared to Dtxl or Dox-loaded nanoparticle at the same dose of drugs. Furthermore, Chen et al. designed an inorganic mesoporous silica nanocapsules (IMNCs) to mimic organic nanoliposome for co-encapsulating and co-delivering hydrophobic drug (CPT) and hydrophilic drug (Dox) simultaneously[164]. The IMNCs were comprised of the hollow core part that acted as container for hydrophobic agents, and the hydrophilic mesoporous shell that functioned as the reservoirs for hydrophilic drugs and increased the stability of the nanocarriers. In comparison to drug-IMNCs and free drugs, the CPT-Dox-IMNCs effectively overcome the drug resistance of MCF-7 cells via additive combination effects. After incubation for 48 h, the anticancer efficiency was 62.8% for CPT-Dox-IMNCs, much higher than that of 21.7 % for free Dox and 47.3 % for Dox-IMNCs.
Fig. 6.
A. Schematic illustration of micelle self-assembled from Dox and WOR conjugated poly(ethylene glycol)-poly(aspartate hydrazide) block copolymer. B. Advantages of the Dox and WOR co-encapsulated micelle DDS compared with free drugs mixture. Reprinted with permission from [163].
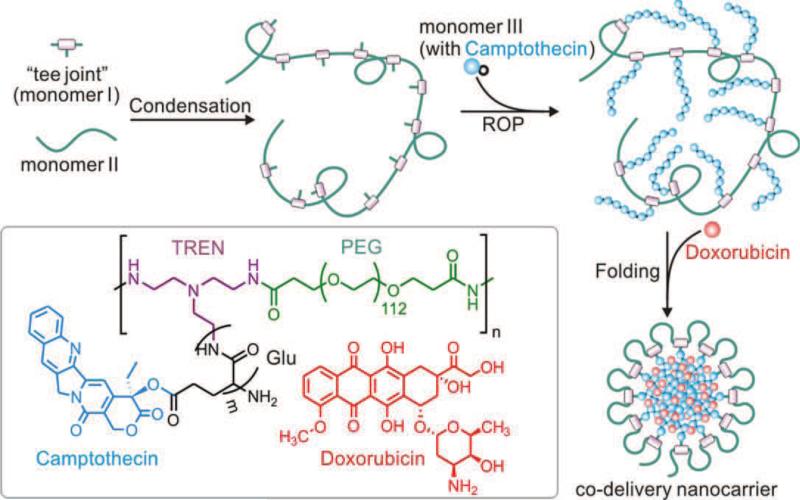
Our group has reported a co-delivery system in a bio-inspired manner [165]. For this formulation, CPT was conjugated into the glutamic acid N-carboxyanhydride and then grafted on the PEG backbone chain via ring opening polymerization, which maximized the drug loading efficiency and reduced the polymer heterogeneity with 100% CPT conjugation. Dox was directly encapsulated in the core of nanocarrier during the self-folding process as a result of the amphiphilic nature of the copolymer (Fig. 7). More than 20% of CPT (percentage of CPT weight compared to polymer) and as much as 30% of Dox could be encapsulated into the nanocarrier. In vitro drug release study showed the PEG shell could effectively prevent premature drug release, as evidenced by less than 10% of CPT released from nanocarrier in the presence of the mouse serum within 6 days. However, the release of Dox was triggered and accelerated by the acidic environment, which was beneficial for cytotoxicity. The controlled release behavior with coordinated doses of CPT and Dox resulted in potent in vitro cytotoxicity against a panel of 9 cancer cell lines. Moreover, CPT/Dox co-delivery nanocarrier presented 1.5- to 60-fold enhancement in cytotoxicity when compared to single drug-loaded formulations, which suggested improved therapeutic efficiency and additive effects. In vivo study showed the co-delivery of CPT and Dox in the graft-folded polymeric nanocarriers displayed higher tumor growth inhibition than single drug based monotherapy.
Fig. 7.
Schematic of synthesis of graft copolymer and formation of stealth nanocarriers. The nanocarriers encapsulated with Dox was self-assembled from graft copolymer with pendant CPT segments. Reprinted with permission from [165].
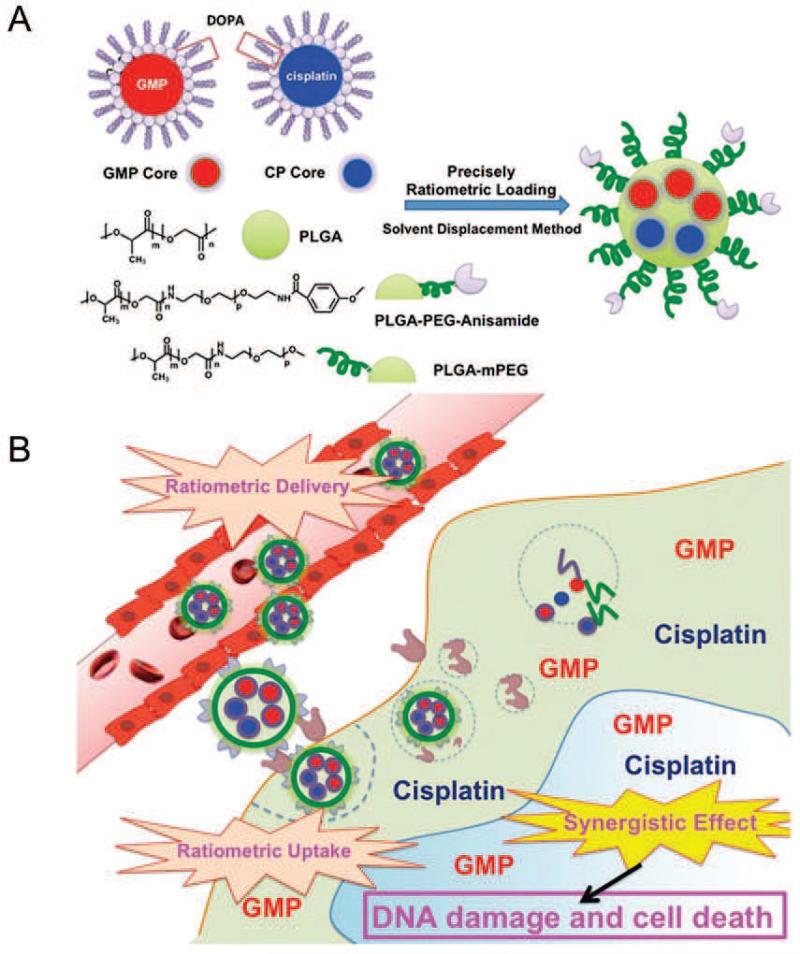
Other small molecular chemotherapeutics that function at nucleus site have also been exploited for additive combination therapy. For example, Miao et al. applied a nanoparticle delivery system to co-encapsulate GEM monophosphate and Pt for the treatment of bladder cancer (Fig. 8)[166]. GEM is widely used as chemotherapeutic in combination with Pt for the treatment of bladder cancer. A solvent displacement method was utilized to proportionally load gemcitabine monophosphate and 3, 4-dihydroxyphenylalanine (DOPA) coated Pt-precipitated nanocore into the same PLGA nanoparticles. In vitro results showed that GEM-NP resulted in a much lower IC50 of 17.8 μM compared to GEM free drug (IC50 of 34.8 μM). Using the isobologram equation of Chou–Talalay[167], the overall combination index (CI) was < 1 at drugs molar ratio of 5.3:1 (GEM : Pt). After administration, this single NP with well-controlled optimal drugs ratio exhibited more significant additive antitumor efficacy compared with individual drug-loaded NP in vivo. In another study, Kolishetti et al. engineered self-assembled nanoparticle for co-delivery of Pt(IV) prodrug and Dtxl[73]. To prepare the nanoparticle, Pt(IV) prodrug was first conjugated onto the pendant hydroxyl group of the polylactide (PLA) backbone. Thereafter, the PLA-Pt(IV) was mixed with poly(D,L-lactic-co-glycolic acid)-block-poly(ethylene glycol) copolymer and Dtxl. After extruding through microfluidic channels, the nanoparticulate co-delivery system with size of 100 nm was prepared. The controlled release profile of both drugs over a period of 48-72 h was achieved by co-delivery system. After decoration of A10 aptamer, nanoparticles were internalized by LNCaP cells via endocytosis and generated the cytotoxicity via intercalating into nuclear DNA. Comparison of IC50 values, it was found that a 2-fold increase in cytotoxicity of Pt-Dtxl-NP was achieved in LNCaP cells when compared to Pt-NP and Dtxl-NP, suggesting an additive effect.
Fig. 8.
A. Preparation of GMP and Pt co-encapsulated PLGA nanoparticles. B. Ratiometrical delivery of GMP and Pt to tumor site and strong additive anti-tumor efficacy. Reprinted with permission from [166].
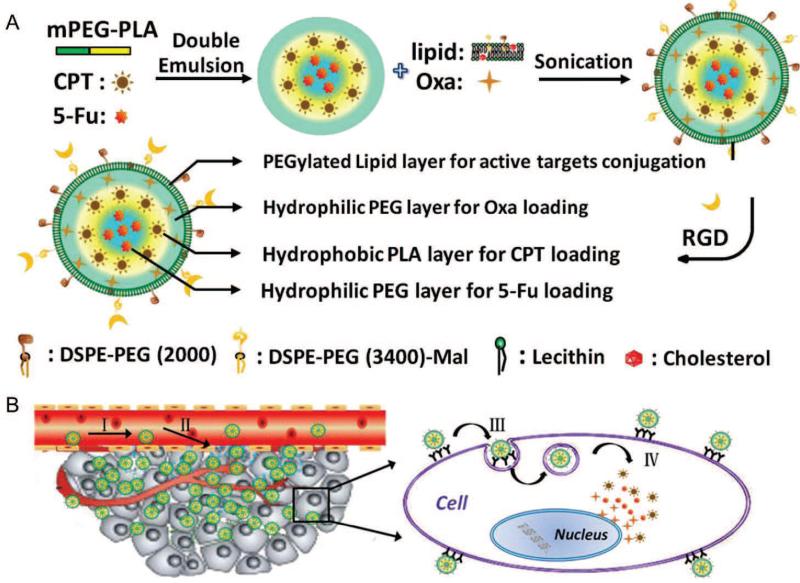
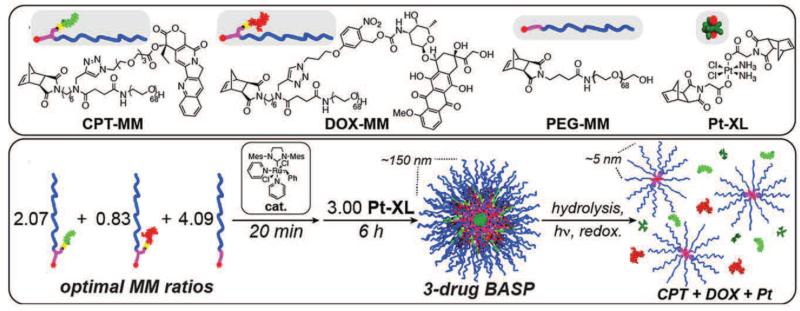
In exploring the maximum additive combination effects in cancer chemotherapy, multiple drugs were often packaged together in one nanocarrier for combination therapy. For instance, Ashley et al. developed a nanoporous particle-supported lipid bilayer to deliver multiple chemotherapeutic agents simultaneously, including Dox, 5-FU and Pt[168]. Furthermore, equipped with the targeting modality, the co-delivery system loaded with three drugs achieved 106-fold improvement in inhibition of cell proliferation compared to partner drug-loaded liposomes against the drug-resistant human hepatocellular carcinoma cell. In another example, Li et al. synthesized a multiple layer-by-layer lipid-polymer hybrid nanoparticle for co-delivery of two hydrophilic drugs 5-Fu and Oxa, and one hydrophobic drug CPT (Fig. 9A, B)[169]. In the hybrid nanoparticles system, 5-Fu was loaded into the hydrophilic core of the nanoparticles, while CPT was inserted into the hydrophobic layer. Additionally, Oxa was encapsulated in the interlayer of polymeric core and lipid bilayer. The results demonstrated that the encapsulation of the three antitumor drugs together could enormously increase therapeutic efficacy by co-delivering the chemotherapeutics to their most active destinations. Furthermore, Liao et al. developed a convergent single nanoparticle platform for combination delivery of Pt, Dox, and CPT (Fig. 10)[170]. The “brush-first” ring-opening metathesis polymerization method was employed to synthesize the nanoscopic brush-arm star polymers (BASPs). Moreover, two macromonomers (MMs), CPT-MM and Dox-MM with the responsiveness to cell physiological condition and long-wavelength ultraviolet (UV) light, Pt-conjugated crosslinker were synthesized for the development of combination delivery system. The resulted co-encapsulated nanoparticle was evidenced to release each drug upon each distinct trigger, leading to enhanced cytotoxicity and additive antitumor effects in vitro.
Fig. 9.
A. Scheme of multiple layer-by-layer structured hybrid nanoparticles co-encapsulated with Oxa, CPT and 5-Fu. B. The accumulation of co-delivery system at the tumor site with a combination of passive and active targeting. I. prolonged circulation time. II. selectively target to tumor cells. III. Endocytosis of co-delivery system. IV. the release of loaded drug. Reprinted with permission from [169].
Fig. 10.
Synthesis of drug-conjugated monomers and preparation of three-drug-loaded co-delivery system. The release of individual drug release is responsive to three distinct triggers. Reprinted with permission from [170].
3.3. Potentiation combination effects
The potentiation drug combinations refer to the regulation of partner drug internalization, accumulation, distribution and metabolism. The potentiation regulation of drug internalization can enhance intracellular drug concentration through bypassing, permeation, disruption of transport barrier, or inhibition of drug efflux. The potentiation regulation of drug distribution or accumulation increases drug concentration in specific site via active-targeting strategy or spatiotemporally controlled release of the drug. The potentiation modulation of drug metabolism can decrease undesirable drug-drug interaction and maximize the efficacy of partner drug[101].
The typical potentiation effects can be illustrated by two kinds of co-delivery strategies. One is delivering modulator of chemoresistance or drug transporters with chemotherapeutic agent to enhance the anticancer effects. For example, Barui et al. used liposome to co-deliver curcumin and Dox[171]. Curcumin, which holds potential to inhibit activation of transcription factor linked to drug resistance, is now being co-administered with various potent anticancer drugs for combination chemotherapy[172, 173]. The results showed that the curcumin and Dox co-encapsulated liposome exhibited potentiation effect in inhibiting proliferation, invasion and migration of both tumor and endothelial cells. The mechanism underlying this result might rely on the inhibition of proliferation and metastasis related genes both at mRNA and protein levels. Remarkable tumor growth inhibition was observed on mice treated with co-delivery system. A 2-3 folds increase in tumor growth inhibition was found in combination therapy compared to curcumin or Dox monotherapy. In another study, Duan et al. developed a pH-sensitive polymeric micelle for effective combination delivery of Dox and disulfiram (DSF)[174]. DSF is a P-glycoprotein (P-gp) inhibitor that can inactivate P-gp and inhibit the efflux of chemotherapeutic drug[175, 176]. P-gp is overexpressed in cancer cells in response to a number of chemotherapeutic agents[177]. Overexpressed P-gp can result in drug resistance and contribute to the formation of a drug efflux pump that inhibits the intracellular accumulation of chemotherapeutic agents[178]. The results showed that DSF could significantly enhance the cytotoxicity of Dox, induce cell apoptosis and change cell cycle. Importantly, the co-delivery system showed high tumor accumulation and superior antitumor effect in multi-drug resistance (MDR) tumors with low systemic toxicity.
Another strategy is to co-deliver nucleic acids and chemotherapeutics to tumor site for potentiation combination effect. For example, co-delivery of siRNA could achieve the restoration of drug sensitivity in cancer cells by knocking down genes involved in the resistance to one or more chemotherapeutic agents[15, 81, 179, 180]. Meng et al. developed mesoporous silica nanoparticle (MSNP) to deliver Dox and P-gp siRNA to overcome drug resistance[181]. The results demonstrated that the intracellular concentration of Dox was significantly increased in the presence of siRNA when compared to free Dox or Dox delivered by MSNP or PEI-MSNP without siRNA. Xiong et al. designed a traceable multifunctional micellar nanocarrier for co-delivering MDR-1 siRNA and Dox[182]. This multifunctional polymeric micellar system was shown to be capable of delivering Dox and siRNA to their intracellular targets, leading to the inhibition of P-gp-mediated Dox resistance in vitro and increased intracellular Dox concentration. Additionally, Xu et al. developed a versatile nanoparticle platform to deliver a DNA damaging Pt prodrug and REV1/REV3L-specific siRNA simultaneously to the same tumor cells for treating patients with malignancies[183]. The siRNA contained in nanoparticles could knock down target genes for error-prone DNA synthesis. The results revealed a remarkable enhancement on tumor inhibition in a human lymph node carcinoma than Pt monotherapy.
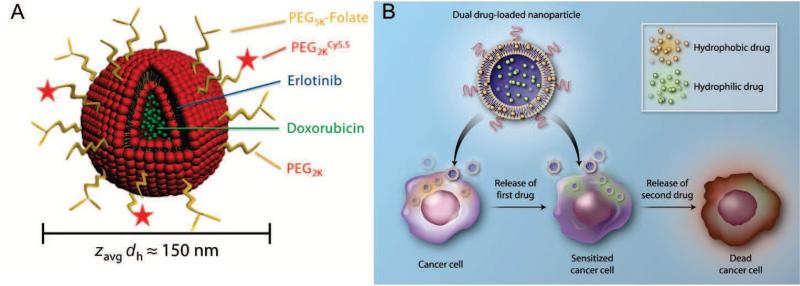
Recently, Morton et al. have inspired the advancement of potentiation drug combinations using the liposomal system with a unique time-staggered release of the encapsulated drugs (Fig. 11)[184, 185]. The implementation of new combination approach was built upon the hydrophobic and hydrophilic compartments of liposomes. Erlotinib (epidermal growth factor receptor inhibitor) was loaded in the hydrophobic layer and Dox was encapsulated in the hydrophilic core. Differential release profile was achieved for the combination DDS, due to the quicker release of erlotinib than Dox. The first release of erlotinib effectively rewired signaling networks through persistent EGFR inhibition and subsequently generated the sensitization and potentiation effect, which was beneficial for Dox. The sensitized cancer cell would unmask a caspase-8-dependent cell death pathway that was utilized by Dox to maximize the treatment efficacy.
Fig. 11.
A. Schematic of co-encapsulation of erlotinib and Dox in the liposomal delivery system. B. Rewiring of signaling network enabled by time-staggered release of combination drugs maximizes the potentiation effects of combination chemotherapy. Reprinted with permission from [184, 185].
4. Sequential delivery of multiple chemotherapeutics
Combination therapy has been validated to be more effective than monotherapy in cancer treatment[186, 187]. However, the traditional administration of drug “cocktails”-based combination therapy often suffers from distinct pharmacokinetic profiles of partner therapeutics, leading to an inconsistent in vivo pharmacokinetics and biodistribution and therefore an inefficient therapy[188]. Even though nanocarriers can transport the multiple chemotherapeutics to intracellular destination, how to differentiate different active targets of each chemotherapeutics still remains difficult. A co-delivery system capable of differentiating the extracellular and intracellular targets or differentiating subcellular targets will achieve stronger combination effect compared to conventional co-delivery system[83].
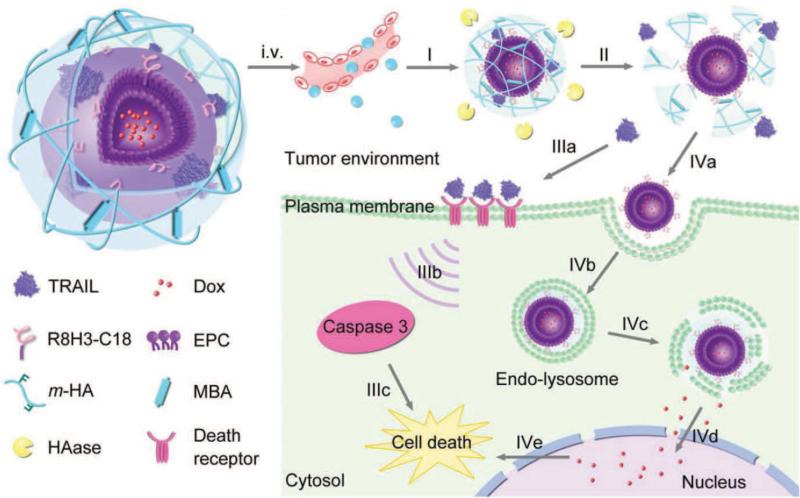
Our group has developed a sequential delivery system for site-specific delivery of tumor necrosis factor-related apoptosis inducing ligand (TRAIL) and Dox. A core–shell nanocarrier (Gel-liposome) comprised of a liposomal core and a crosslinked-gel shell was developed to co-encapsulate TRAIL and Dox (Fig. 12)[189]. The cell penetrating peptide—R8H3 was conjugated on the surface of Dox-loaded liposome. Subsequently, TRAIL was attached on the outside of negative charged liposome via electrostatic interaction. Finally, a layer of modified hyaluronic acid (HA) was crosslinked to form a shell to protect the TRAIL from denaturation. When the co-delivery DDS accumulated at the tumor microenvironment, HA-based shell was enzymatically degraded by hyaluronidase (HAase) overexpressed in the tumor microenvironment. The released TRAIL then bound to the death receptors on the cell membrane and triggered the caspase-3 signaling pathway to induce apoptosis of cancer cell. Simultaneously, the exposed cell penetrating peptide facilitated the endocytosis of Dox-loaded liposome, accompanied by the release of Dox from endosome and accumulation in the nuclei. In vitro cytotoxicity assay showed that the IC50 of TRAIL/Dox-Gelipo against human breast cancer (MDA-MB-231) cell lines was 83 ng/mL, which was significantly higher than that of Dox-Gelipo (569 ng/mL). The significant increase in cytotoxicity indicated remarkable synergistic combination effect. Furthermore, by taking advantage of the site-specific delivery manner, the TRAIL/Dox-Gelipo could effectively inhibit the tumor growth in the MDA-MB-231 xenograft tumor animal model.
Fig. 12.
Schematic design of TRAIL/Dox-Gelipo for sequential and site-specific drug delivery. The Gelipo is comprised of Dox-loaded liposome core and HA-based out shell. After intravenous injection, the Gelipo will accumulate at tumor site and the HA shell will be cleaved by overexpressed HAase readily. The exposed TRAIL will bind to the death receptor and trigger downstream apoptosis signal. The encapsulated Dox will be triggered to release by the vacidity of lysosome and accumulate at the nuclei. Reprinted with permission from [189].
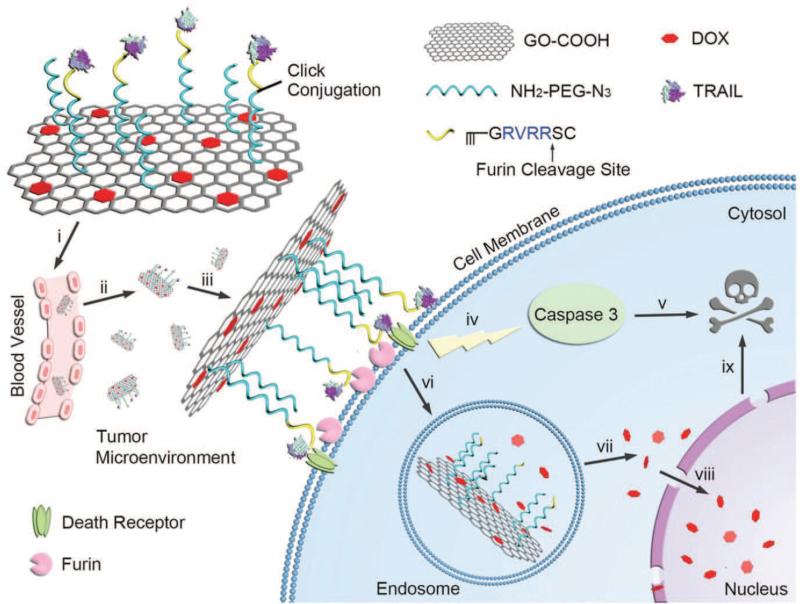
Further, a graphene-based system (TRAIL/Dox-fGO) has also been developed for the sequential and site-specific delivery of TRAIL and Dox in cancer cells (Fig. 13)[190]. The biofunctional amino- and azide-modified PEG linker was conjugated on the graphene oxide nanosheet. Subsequently, a furin-cleavable peptide was decorated on the PEG through a click reaction with the N3 terminus. TRAIL was then conjugated with the peptide via cysteine groups using an amine-to-sulfhydryl linker. Dox was loaded on the graphene oxide through the π–π stacking interaction between graphene oxide and Dox with high loading capacity. At the tumor site, the peptide linker was cleaved by the overexpressed furin, promoting the release and the interaction of TRAIL toward cell membrane to trigger downstream apoptosis signals. After the digestion, the Dox-loaded graphene oxide nanosheet underwent endocytosis with the subsequent release of Dox inside the cell triggered by the acidity of endosome and accumulation in the nuclei. A 8.5- and 3.6-fold increase in cytotoxicity against A549 cells was achieved by TRAIL/Dox-fGO when compared to TRAIL-fGO and Dox-fGO, respectively. In vivo antitumor efficacy was investigated on the A549 tumor-bearing nude mice, which showed stronger tumor inhibition capability of TRAIL/Dox-fGO when compared to TRAIL-fGO and Dox-fGO. Collectively, both in vitro and in vivo results showed the synergistic anticancer effects of the co-encapsulated chemotherapeutics delivered in a site-specific manner. Most recently, we have proposed a platelet-mimicking nanovehicle (PM-NV) platform with capability of sequentially and site-specifically delivering TRAIL and Dox into tumor cells. In this biomimetic delivery system, the natural platelet membrane was wrapped onto the synthetic nanovehicle to load TRAIL on the surface and Dox within the nanovehicle core[191]. By taking advantage of highly selective affinity between platelet and cancer cells, the PM-NV could aggregate on the surface of cancer cells to promote the interaction of TRAIL and death receptors, triggering programmed cell death. Moreover, equipped with pH-responsive modality, the PM-NV could release Dox in lysosome upon the cleavage of degradable matrix. The synergistic effect of the site-specific delivery of drugs in the PM-NV was established in mice models by the significant inhibition of primary tumor growth as well as efficient elimination of circulating tumor cells.
Fig. 13.
Schematic design of enzyme-responsive graphene oxide-based sequential delivery system. The TRAIL is conjugated on the graphene oxide through a furin-cleavable peptide linker and Dox was loaded on the graphene via π–π stacking interaction. After accumulation at tumor site, the overexpressed furin will cleave the peptide linker and promote the exposition of TRAIL toward death receptors. The Dox-loaded graphene oxide nanosheet will be internalized and Dox will release and accumulate at nuclei with the assistance of acidity of lysosome. Reprinted with permission from [190].
5. Conclusion and Outlook
Combination chemotherapy has long been adopted as the standard for cancer treatment. It is acknowledged that the proper drug combinations can promote combinatorial actions, improve target selectivity, and inhibit the development of cancer drug resistance. In particular, the emergence and rapid development of nanotechnology have offered unprecedented opportunities for combination chemotherapy. The various pharmacokinetics among different drugs in cocktail chemotherapy, which lead to distinctive physiological fates and non-uniform distribution, are the main cause of the poor outcome of clinical cancer treatment; while the nanocarrier-assisted combination chemotherapy can unify the in vivo pharmacokinetics of various chemotherapeutics through co-encapsulating multiple drugs inside.
Although nanotechnology has accelerated the development of combination chemotherapy, there exist multiple challenges in design of effective combination chemotherapy system for anticancer treatment. First, it is necessary to perform thorough biological evaluation, which must be supported by a well understanding of the molecular and cellular mechanisms involved. Understanding the mechanisms underlying combination effects of drug combinations could facilitate the discovery of novel efficacious combination chemotherapy and avoid potential unwanted side effects. Second, the optimal mass ratio of each chemotherapeutic within the combination drug delivery system needs to be precisely tuned, according to individual's pharmacokinetics and efficacy. The ratio of the combinatorial chemotherapeutics has been validated to play a vital role in the efficacy of combination treatment[192]. Additionally, the ratio of each individual drug holds high potential to determine the possibility of synergism and antagonism of a combination set. Moreover, the sequential and site-specific delivery system could be further extended into combination chemotherapy for achieving maximum treatment efficacy. Finally, side effects or toxicity of nanoparticles in nanocarrier-mediated combination chemotherapy need to be fully elucidated. In addition to general evaluation of the toxicity on major organs, the interaction between nanocarrier and endothelial cells of blood vessels should be taken into account due to intravenous injection is the most popular route of drug administration[193]. To minimize the systemic toxicity as well as preservation of treatment efficacy of nancarrier-based combination delivery system, several design principles need to be complied, such as rational design of the size and surface physicochemical property, carefully selecting and tailoring the composition materials. Finally, functionalize the nanocarrier with the targeting ligands to increase the drug accumulation at the interested disease site offers a promising strategy to reduce the side effect and enhance the treatment efficacy[51]. The ability to actively target specific cells/tissues makes ligand-conjugated nanocarrier-based combination delivery system outperform conventional drug delivery system. For cancer treatment, the presence of targeting ligand can enhance the intracellular drug concentration at tumor site via receptor-mediated endocytosis and decrease the systemic distribution to reduce the unwanted side effects.
Furthermore, as discussed, nanotechnology-assisted combination chemotherapy offers the superiority of using chemotherapeutics at lower dose, reducing systemic toxicity and enhancing therapeutic efficacy. However, translation of nanocarrier-based combination therapy into the clinic remains challenging[194]. Significant efforts are needed to be undertaken to elucidate the synergistic effect achieved by the combination therapy, which is attributed to the advanced drug delivery strategies rather than the simply summed effect of partner drugs. It is important to validate that the combination of multiple therapeutic agents in a single delivery system provides advantages over simple administration of combined free drugs. Importantly, side effects, especially long-term toxicity, should be carefully and thoroughly evaluated. Although, different chemotherapeutic agents with various modes of actions can be combined in a single delivery system to maximize the therapeutic efficacy, the systemic toxicity of combination chemotherapy might be significantly enhanced due to the sum of side effects of separated drugs, which will enormously limit the effectiveness of combination therapy in clinic. Additionally, in order to fulfill the translation of nanocarrier-based combination chemotherapy, the pharmacokinetics and biodistribution of delivery systems must be carefully studied to guarantee the sufficient drug concentration at tumor site and subsequently enhance treatment efficacy.
Acknowledgements
This work was supported by the grants from NC TraCS, NIH's Clinical and Translational Science Awards (CTSA, NIH grant 1UL1TR001111) at UNC-CH and the startup package from the Joint Biomedical Engineering Department of the UNC-CH and NC State University.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference
- 1.Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007;2:751–760. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 2.Stewart BW, Kleihues P. World cancer report. IARC press; Lyon: 2003. I.A.f.R.o. Cancer. [Google Scholar]
- 3.World cancer report 2014. WHO; Geneva: 2014. I.A.f.R.o. Cancer. [Google Scholar]
- 4.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014, CA. Cancer J. Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 5.DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A. Cancer treatment and survivorship statistics, 2014, CA. Cancer J. Clin. 2014;64:252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 6.Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014, CA. Cancer J. Clin. 2014;64:83–103. doi: 10.3322/caac.21219. [DOI] [PubMed] [Google Scholar]
- 7.Sporn MB. The war on cancer. The lancet. 1996;347:1377–1381. doi: 10.1016/s0140-6736(96)91015-6. [DOI] [PubMed] [Google Scholar]
- 8.DePinho RA. The age of cancer. Nature. 2000;408:248–254. doi: 10.1038/35041694. [DOI] [PubMed] [Google Scholar]
- 9.Chabner BA, Roberts TG. Chemotherapy and the war on cancer. Nat. Rev. Cancer. 2005;5:65–72. doi: 10.1038/nrc1529. [DOI] [PubMed] [Google Scholar]
- 10.Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat. Rev. Cancer. 2007;7:192–201. doi: 10.1038/nrc2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonadonna G, Brusamolino E, Valagussa P, Rossi A, Brugnatelli L, Brambilla C, De Lena M, Tancini G, Bajetta E, Musumeci R. Combination chemotherapy as an adjuvant treatment in operable breast cancer. N. Engl. J. Med. 1976;294:405–410. doi: 10.1056/NEJM197602192940801. [DOI] [PubMed] [Google Scholar]
- 12.Kelland L. The resurgence of platinum-based cancer chemotherapy. Nat. Rev. Cancer. 2007;7:573–584. doi: 10.1038/nrc2167. [DOI] [PubMed] [Google Scholar]
- 13.Coffey JC, Wang J, Smith M, Bouchier-Hayes D, Cotter T, Redmond H. Excisional surgery for cancer cure: therapy at a cost. The lancet oncology. 2003;4:760–768. doi: 10.1016/s1470-2045(03)01282-8. [DOI] [PubMed] [Google Scholar]
- 14.Pardoll D, Allison J. Cancer immunotherapy: breaking the barriers to harvest the crop. Nat. Med. 2004;10:887–892. doi: 10.1038/nm0904-887. [DOI] [PubMed] [Google Scholar]
- 15.Whitehead KA, Langer R, Anderson DG. Knocking down barriers: advances in siRNA delivery. Nat. Rev. Drug Discovery. 2009;8:129–138. doi: 10.1038/nrd2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferrari M. Cancer nanotechnology: opportunities and challenges. Nat. Rev. Cancer. 2005;5:161–171. doi: 10.1038/nrc1566. [DOI] [PubMed] [Google Scholar]
- 17.Heldin C-H, Rubin K, Pietras K, Östman A. High interstitial fluid pressure—an obstacle in cancer therapy. Nat. Rev. Cancer. 2004;4:806–813. doi: 10.1038/nrc1456. [DOI] [PubMed] [Google Scholar]
- 18.Finkel T, Serrano M, Blasco MA. The common biology of cancer and ageing. Nature. 2007;448:767–774. doi: 10.1038/nature05985. [DOI] [PubMed] [Google Scholar]
- 19.Imai K, Takaoka A. Comparing antibody and small-molecule therapies for cancer. Nat. Rev. Cancer. 2006;6:714–727. doi: 10.1038/nrc1913. [DOI] [PubMed] [Google Scholar]
- 20.Chen HX, Cleck JN. Adverse effects of anticancer agents that target the VEGF pathway. Nat. Rev. Clin. Oncol. 2009;6:465–477. doi: 10.1038/nrclinonc.2009.94. [DOI] [PubMed] [Google Scholar]
- 21.Lotfi-Jam K, Carey M, Jefford M, Schofield P, Charleson C, Aranda S. Nonpharmacologic strategies for managing common chemotherapy adverse effects: a systematic review. J. Clin. Oncol. 2008;26:5618–5629. doi: 10.1200/JCO.2007.15.9053. [DOI] [PubMed] [Google Scholar]
- 22.Igney FH, Krammer PH. Death and anti-death: tumour resistance to apoptosis. Nat. Rev. Cancer. 2002;2:277–288. doi: 10.1038/nrc776. [DOI] [PubMed] [Google Scholar]
- 23.Falleti MG, Sanfilippo A, Maruff P, Weih L, Phillips K-A. The nature and severity of cognitive impairment associated with adjuvant chemotherapy in women with breast cancer: a meta-analysis of the current literature. Brain Cogn. 2005;59:60–70. doi: 10.1016/j.bandc.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Kamb A, Wee S, Lengauer C. Why is cancer drug discovery so difficult? Nat. Rev. Drug Discovery. 2007;6:115–120. doi: 10.1038/nrd2155. [DOI] [PubMed] [Google Scholar]
- 25.Klastersky J. Adverse effects of the humanized antibodies used as cancer therapeutics. Curr. Opin. Oncol. 2006;18:316–320. doi: 10.1097/01.cco.0000228734.32261.62. [DOI] [PubMed] [Google Scholar]
- 26.Rabinow BE. Nanosuspensions in drug delivery. Nat. Rev. Drug Discovery. 2004;3:785–796. doi: 10.1038/nrd1494. [DOI] [PubMed] [Google Scholar]
- 27.Lavan DA, McGuire T, Langer R. Small-scale systems for in vivo drug delivery. Nat. Biotechnol. 2003;21:1184–1191. doi: 10.1038/nbt876. [DOI] [PubMed] [Google Scholar]
- 28.Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3:16–20. doi: 10.1021/nn900002m. [DOI] [PubMed] [Google Scholar]
- 29.Saltzman WM, Olbricht WL. Building drug delivery into tissue engineering design. Nat. Rev. Drug Discovery. 2002;1:177–186. doi: 10.1038/nrd744. [DOI] [PubMed] [Google Scholar]
- 30.Langer R. Drug delivery and targeting. Nature. 1998;392:5–10. [PubMed] [Google Scholar]
- 31.Soppimath KS, Aminabhavi TM, Kulkarni AR, Rudzinski WE. Biodegradable polymeric nanoparticles as drug delivery devices. J. Control. Release. 2001;70:1–20. doi: 10.1016/s0168-3659(00)00339-4. [DOI] [PubMed] [Google Scholar]
- 32.Goldberg M, Langer R, Jia X. Nanostructured materials for applications in drug delivery and tissue engineering. J. Biomater. Sci. Polym. Ed. 2007;18:241–268. doi: 10.1163/156856207779996931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pillai O, Panchagnula R. Polymers in drug delivery. Curr. Opin. Chem. Biol. 2001;5:447–451. doi: 10.1016/s1367-5931(00)00227-1. [DOI] [PubMed] [Google Scholar]
- 34.Shim MS, Kwon YJ. Stimuli-responsive polymers and nanomaterials for gene delivery and imaging applications. Adv. Drug Deliv. Rev. 2012;64:1046–1059. doi: 10.1016/j.addr.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 35.Wissing S, Kayser O, Müller R. Solid lipid nanoparticles for parenteral drug delivery. Adv. Drug Deliv. Rev. 2004;56:1257–1272. doi: 10.1016/j.addr.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 36.Lian T, Ho RJ. Trends and developments in liposome drug delivery systems. J. Pharm. Sci. 2001;90:667–680. doi: 10.1002/jps.1023. [DOI] [PubMed] [Google Scholar]
- 37.Samad A, Sultana Y, Aqil M. Liposomal drug delivery systems: an update review. Curr. Drug Deliv. 2007;4:297–305. doi: 10.2174/156720107782151269. [DOI] [PubMed] [Google Scholar]
- 38.Mo R, Jiang T, Gu Z. Recent progress in multidrug delivery to cancer cells by liposomes. Nanomed. 2014;9:1117–1120. doi: 10.2217/nnm.14.62. [DOI] [PubMed] [Google Scholar]
- 39.Dong Y, Eltoukhy AA, Alabi CA, Khan OF, Veiseh O, Dorkin JR, Sirirungruang S, Yin H, Tang BC, Pelet JM. Lipid-Like Nanomaterials for Simultaneous Gene Expression and Silencing In Vivo. Adv. Healthc. Mater. 2014;3:1392–1397. doi: 10.1002/adhm.201400054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liong M, Lu J, Kovochich M, Xia T, Ruehm SG, Nel AE, Tamanoi F, Zink JI. Multifunctional inorganic nanoparticles for imaging, targeting, and drug delivery. ACS Nano. 2008;2:889–896. doi: 10.1021/nn800072t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arruebo M, Fernández-Pacheco R, Ibarra MR, Santamaría J. Magnetic nanoparticles for drug delivery. Nano today. 2007;2:22–32. [Google Scholar]
- 42.Arruebo M. Drug delivery from structured porous inorganic materials. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2012;4:16–30. doi: 10.1002/wnan.132. [DOI] [PubMed] [Google Scholar]
- 43.Sun C, Lee JS, Zhang M. Magnetic nanoparticles in MR imaging and drug delivery. Adv. Drug Deliv. Rev. 2008;60:1252–1265. doi: 10.1016/j.addr.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun W, Jiang T, Lu Y, Reiff M, Mo R, Gu Z. Cocoon-Like Self-Degradable DNA Nanoclew for Anticancer Drug Delivery. J. Am. Chem. Soc. 2014;136:14722–14725. doi: 10.1021/ja5088024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Andersen ES, Dong M, Nielsen MM, Jahn K, Subramani R, Mamdouh W, Golas MM, Sander B, Stark H, Oliveira CL. Self-assembly of a nanoscale DNA box with a controllable lid. Nature. 2009;459:73–76. doi: 10.1038/nature07971. [DOI] [PubMed] [Google Scholar]
- 46.Lee H, Lytton-Jean AK, Chen Y, Love KT, Park AI, Karagiannis ED, Sehgal A, Querbes W, Zurenko CS, Jayaraman M. Molecularly self-assembled nucleic acid nanoparticles for targeted in vivo siRNA delivery. Nat. Nanotechnol. 2012;7:389–393. doi: 10.1038/nnano.2012.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rothemund PW. Folding DNA to create nanoscale shapes and patterns. Nature. 2006;440:297–302. doi: 10.1038/nature04586. [DOI] [PubMed] [Google Scholar]
- 48.Sun W, Gu Z. Engineering DNA scaffolds for delivery of anticancer therapeutics. Biomater. Sci. 2015;3:1018–1024. doi: 10.1039/c4bm00459k. [DOI] [PubMed] [Google Scholar]
- 49.Sun W, Lu Y, Gu Z. Advances in Anticancer Protein Delivery using Micro-/Nanoparticles. Particle & Particle Systems Characterization. 2014;31:1204–1222. doi: 10.1002/ppsc.201400140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303:1818–1822. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 51.Shi J, Votruba AR, Farokhzad OC, Langer R. Nanotechnology in drug delivery and tissue engineering: from discovery to applications. Nano Lett. 2010;10:3223–3230. doi: 10.1021/nl102184c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sarikaya M, Tamerler C, Jen AK-Y, Schulten K, Baneyx F. Molecular biomimetics: nanotechnology through biology. Nat. Mater. 2003;2:577–585. doi: 10.1038/nmat964. [DOI] [PubMed] [Google Scholar]
- 53.Wagner V, Dullaart A, Bock A-K, Zweck A. The emerging nanomedicine landscape. Nat. Biotechnol. 2006;24:1211–1217. doi: 10.1038/nbt1006-1211. [DOI] [PubMed] [Google Scholar]
- 54.Smith DM, Simon JK, Baker JR., Jr Applications of nanotechnology for immunology. Nat. Rev. Immunol. 2013;13:592–605. doi: 10.1038/nri3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu D, Bimbo LM, Mäkilä E, Villanova F, Kaasalainen M, Herranz-Blanco B, Caramella CM, Lehto V-P, Salonen J, Herzig K-H. Co-delivery of a hydrophobic small molecule and a hydrophilic peptide by porous silicon nanoparticles. J. Control. Release. 2013;170:268–278. doi: 10.1016/j.jconrel.2013.05.036. [DOI] [PubMed] [Google Scholar]
- 56.Zhang L, Radovic-Moreno AF, Alexis F, Gu FX, Basto PA, Bagalkot V, Jon S, Langer RS, Farokhzad OC. Co - delivery of hydrophobic and hydrophilic drugs from nanoparticle – aptamer bioconjugates. Chemmedchem. 2007;2:1268–1271. doi: 10.1002/cmdc.200700121. [DOI] [PubMed] [Google Scholar]
- 57.Guo S, Huang L. Nanoparticles containing insoluble drug for cancer therapy. Biotechnol. Adv. 2014;32:778–788. doi: 10.1016/j.biotechadv.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moghimi SM, Hunter AC, Murray JC. Long-circulating and target-specific nanoparticles: theory to practice. Pharmacol. Rev. 2001;53:283–318. [PubMed] [Google Scholar]
- 59.Yoo J-W, Chambers E, Mitragotri S. Factors that control the circulation time of nanoparticles in blood: challenges, solutions and future prospects. Curr. Pharm. Des. 2010;16:2298–2307. doi: 10.2174/138161210791920496. [DOI] [PubMed] [Google Scholar]
- 60.Owens DE, Peppas NA. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int. J. Pharm. 2006;307:93–102. doi: 10.1016/j.ijpharm.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 61.Alexis F, Pridgen E, Molnar LK, Farokhzad OC. Factors affecting the clearance and biodistribution of polymeric nanoparticles. Mol. Pharm. 2008;5:505–515. doi: 10.1021/mp800051m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li S-D, Huang L. Stealth nanoparticles: high density but sheddable PEG is a key for tumor targeting. J. Control. Release. 2010;145:178–181. doi: 10.1016/j.jconrel.2010.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li S-D, Huang L. Pharmacokinetics and biodistribution of nanoparticles. Mol. Pharm. 2008;5:496–504. doi: 10.1021/mp800049w. [DOI] [PubMed] [Google Scholar]
- 64.Medina C, Santos - Martinez M, Radomski A, Corrigan O, Radomski M. Nanoparticles: pharmacological and toxicological significance. Br. J. Pharmacol. 2007;150:552–558. doi: 10.1038/sj.bjp.0707130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hu Q, Katti PS, Gu Z. Enzyme-responsive nanomaterials for controlled drug delivery. Nanoscale. 2014;6:12273–12286. doi: 10.1039/c4nr04249b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lu Y, Sun W, Gu Z. Stimuli-responsive nanomaterials for therapeutic protein delivery. J. Control. Release. 2014;194:1–19. doi: 10.1016/j.jconrel.2014.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davis ME, Shin DM. Nanoparticle therapeutics: an emerging treatment modality for cancer. Nat. Rev. Drug Discovery. 2008;7:771–782. doi: 10.1038/nrd2614. [DOI] [PubMed] [Google Scholar]
- 68.Petros RA, DeSimone JM. Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discovery. 2010;9:615–627. doi: 10.1038/nrd2591. [DOI] [PubMed] [Google Scholar]
- 69.Minchin R. Nanomedicine: sizing up targets with nanoparticles. Nat. Nanotechnol. 2008;3:12–13. doi: 10.1038/nnano.2007.433. [DOI] [PubMed] [Google Scholar]
- 70.Sanhai WR, Sakamoto JH, Canady R, Ferrari M. Seven challenges for nanomedicine. Nat. Nanotechnol. 2008;3:242–244. doi: 10.1038/nnano.2008.114. [DOI] [PubMed] [Google Scholar]
- 71.Albanese A, Tang PS, Chan WC. The effect of nanoparticle size, shape, and surface chemistry on biological systems. Annu. Rev. Biomed. Eng. 2012;14:1–16. doi: 10.1146/annurev-bioeng-071811-150124. [DOI] [PubMed] [Google Scholar]
- 72.Song XR, Cai Z, Zheng Y, He G, Cui FY, Gong DQ, Hou SX, Xiong SJ, Lei XJ, Wei YQ. Reversion of multidrug resistance by co-encapsulation of vincristine and verapamil in PLGA nanoparticles. Eur. J. Pharm. Sci. 2009;37:300–305. doi: 10.1016/j.ejps.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 73.Kolishetti N, Dhar S, Valencia PM, Lin LQ, Karnik R, Lippard SJ, Langer R, Farokhzad OC. Engineering of self-assembled nanoparticle platform for precisely controlled combination drug therapy. Proc. Natl. Acad. Sci. U. S. A. 2010;107:17939–17944. doi: 10.1073/pnas.1011368107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Batist G, Gelmon KA, Chi KN, Miller WH, Chia SK, Mayer LD, Swenson CE, Janoff AS, Louie AC. Safety, pharmacokinetics, and efficacy of CPX-1 liposome injection in patients with advanced solid tumors. Clin. Cancer Res. 2009;15:692–700. doi: 10.1158/1078-0432.CCR-08-0515. [DOI] [PubMed] [Google Scholar]
- 75.Feldman EJ, Lancet JE, Kolitz JE, Ritchie EK, Roboz GJ, List AF, Allen SL, Asatiani E, Mayer LD, Swenson C. First-in-man study of CPX-351: a liposomal carrier containing cytarabine and daunorubicin in a fixed 5: 1 molar ratio for the treatment of relapsed and refractory acute myeloid leukemia. J. Clin. Oncol. 2011;29:979–985. doi: 10.1200/JCO.2010.30.5961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dilnawaz F, Singh A, Mohanty C, Sahoo SK. Dual drug loaded superparamagnetic iron oxide nanoparticles for targeted cancer therapy. Biomaterials. 2010;31:3694–3706. doi: 10.1016/j.biomaterials.2010.01.057. [DOI] [PubMed] [Google Scholar]
- 77.Jia L, Li Z, Shen J, Zheng D, Tian X, Guo H, Chang P. Multifunctional mesoporous silica nanoparticles mediated co-delivery of paclitaxel and tetrandrine for overcoming multidrug resistance. Int. J. Pharm. 2015;489:318–330. doi: 10.1016/j.ijpharm.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 78.Gerber H-P, Ferrara N. Pharmacology and pharmacodynamics of bevacizumab as monotherapy or in combination with cytotoxic therapy in preclinical studies. Cancer Res. 2005;65:671–680. [PubMed] [Google Scholar]
- 79.Ibrahim N, Yu Y, Walsh WR, Yang J-L. Molecular targeted therapies for cancer: Sorafenib monotherapy and its combination with other therapies (Review) Oncol. Rep. 2012;27:1303–1311. doi: 10.3892/or.2012.1675. [DOI] [PubMed] [Google Scholar]
- 80.Greco F, Vicent MJ. Combination therapy: opportunities and challenges for polymer–drug conjugates as anticancer nanomedicines. Adv. Drug Deliv. Rev. 2009;61:1203–1213. doi: 10.1016/j.addr.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 81.Dai X, Tan C. Combination of microRNA therapeutics with small-molecule anticancer drugs: Mechanism of action and co-delivery nanocarriers. Adv. Drug Deliv. Rev. 2015;81:184–197. doi: 10.1016/j.addr.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 82.Xu X, Ho W, Zhang X, Bertrand N, Farokhzad O. Cancer nanomedicine: from targeted delivery to combination therapy. Trends Mol. Med. 2015;21:223–232. doi: 10.1016/j.molmed.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pacardo DB, Ligler FS, Gu Z. Programmable nanomedicine: synergistic and sequential drug delivery systems. Nanoscale. 2015;7:3381–3391. doi: 10.1039/c4nr07677j. [DOI] [PubMed] [Google Scholar]
- 84.Bang Y-J, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. The Lancet. 2010;376:687–697. doi: 10.1016/S0140-6736(10)61121-X. [DOI] [PubMed] [Google Scholar]
- 85.Bozic I, Reiter JG, Allen B, Antal T, Chatterjee K, Shah P, Moon YS, Yaqubie A, Kelly N, Le DT. Evolutionary dynamics of cancer in response to targeted combination therapy. Elife. 2013;2:e00747. doi: 10.7554/eLife.00747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carrick S, Parker S, Thornton CE, Ghersi D, Simes J, Wilcken N. Single agent versus combination chemotherapy for metastatic breast cancer. Cochrane Database Syst. Rev. 2009:CD003372. doi: 10.1002/14651858.CD003372.pub2. [DOI] [PubMed] [Google Scholar]
- 87.Hu C-MJ, Aryal S, Zhang L. Nanoparticle-assisted combination therapies for effective cancer treatment. Ther. Deliv. 2010;1:323–334. doi: 10.4155/tde.10.13. [DOI] [PubMed] [Google Scholar]
- 88.Hu C-MJ, Zhang L. Nanoparticle-based combination therapy toward overcoming drug resistance in cancer. Biochem. Pharmacol. 2012;83:1104–1111. doi: 10.1016/j.bcp.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 89.Mann J. Natural products in cancer chemotherapy: past, present and future. Nat. Rev. Cancer. 2002;2:143–148. doi: 10.1038/nrc723. [DOI] [PubMed] [Google Scholar]
- 90.Papac RJ. Origins of cancer therapy. The Yale journal of biology and medicine. 2001;74:391. [PMC free article] [PubMed] [Google Scholar]
- 91.Farber S, Diamond LK, Mercer RD, Sylvester RF, Jr, Wolff JA. Temporary remissions in acute leukemia in children produced by folic acid antagonist, 4-aminopteroyl-glutamic acid (aminopterin) N. Engl. J. Med. 1948;238:787–793. doi: 10.1056/NEJM194806032382301. [DOI] [PubMed] [Google Scholar]
- 92.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/s0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 93.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 94.Egeblad M, Werb Z. New functions for the matrix metalloproteinases in cancer progression. Nat. Rev. Cancer. 2002;2:161–174. doi: 10.1038/nrc745. [DOI] [PubMed] [Google Scholar]
- 95.Miao L, Huang L. Nanotechnology-Based Precision Tools for the Detection and Treatment of Cancer. Springer; 2015. Exploring the Tumor Microenvironment with Nanoparticles; pp. 193–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pilpel Y, Sudarsanam P, Church GM. Identifying regulatory networks by combinatorial analysis of promoter elements. Nat. Genet. 2001;29:153–159. doi: 10.1038/ng724. [DOI] [PubMed] [Google Scholar]
- 97.Müller R. Crosstalk of oncogenic and prostanoid signaling pathways. J. Cancer Res. Clin. Oncol. 2004;130:429–444. doi: 10.1007/s00432-004-0570-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sergina NV, Rausch M, Wang D, Blair J, Hann B, Shokat KM, Moasser MM. Escape from HER-family tyrosine kinase inhibitor therapy by the kinase-inactive HER3. Nature. 2007;445:437–441. doi: 10.1038/nature05474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kassouf W, Dinney CP, Brown G, McConkey DJ, Diehl AJ, Bar-Eli M, Adam L. Uncoupling between epidermal growth factor receptor and downstream signals defines resistance to the antiproliferative effect of Gefitinib in bladder cancer cells. Cancer Res. 2005;65:10524–10535. doi: 10.1158/0008-5472.CAN-05-1536. [DOI] [PubMed] [Google Scholar]
- 100.Mayer LD, Janoff AS. Optimizing combination chemotherapy by controlling drug ratios. Mol. Interv. 2007;7:216. doi: 10.1124/mi.7.4.8. [DOI] [PubMed] [Google Scholar]
- 101.Jia J, Zhu F, Ma X, Cao ZW, Li YX, Chen YZ. Mechanisms of drug combinations: interaction and network perspectives. Nat. Rev. Drug Discovery. 2009;8:111–128. doi: 10.1038/nrd2683. [DOI] [PubMed] [Google Scholar]
- 102.MacDonald D, Perry M. The chemotherapy source book. The chemotherapy source book. 1992 [Google Scholar]
- 103.Tanabe M, Ito Y, Tokudome N, Sugihara T, Miura H, Takahashi S, Seto Y, Iwase T, Hatake K. Possible use of combination chemotherapy with mitomycin C and methotrexate for metastatic breast cancer pretreated with anthracycline and taxanes. Breast Cancer. 2009;16:301–306. doi: 10.1007/s12282-009-0093-0. [DOI] [PubMed] [Google Scholar]
- 104.Maciejczyk A, Lacko A, Ekiert M, Jagoda E, Wysocka T, Matkowski R, Halon A, Gyorffy B, Lage H, Surowiak P. Elevated nuclear S100P expression is associated with poor survival in early breast cancer patients. Histol. Histopathol. 2013;28:513–524. doi: 10.14670/HH-28.513. [DOI] [PubMed] [Google Scholar]
- 105.Stillwell TJ, Benson RC. Cyclophosphamide-induced hemorrhagic cystitis: a review of 100 patients. Cancer. 1988;61:451–457. doi: 10.1002/1097-0142(19880201)61:3<451::aid-cncr2820610308>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 106.Goette DK. Topical chemotherapy with 5-fluorouracil: A review. J. Am. Acad. Dermatol. 1981;4:633–649. doi: 10.1016/s0190-9622(81)80196-x. [DOI] [PubMed] [Google Scholar]
- 107.Socinski MA, Bondarenko I, Karaseva NA, Makhson AM, Vynnychenko I, Okamoto I, Hon JK, Hirsh V, Bhar P, Zhang H. Weekly nab-paclitaxel in combination with carboplatin versus solvent-based paclitaxel plus carboplatin as first-line therapy in patients with advanced non–small-cell lung cancer: final results of a phase III trial. J. Clin. Oncol. 2012;30:2055–2062. doi: 10.1200/JCO.2011.39.5848. [DOI] [PubMed] [Google Scholar]
- 108.Belani CP, Ramalingam S, Perry MC, LaRocca RV, Rinaldi D, Gable PS, Tester WJ. Randomized, phase III study of weekly paclitaxel in combination with carboplatin versus standard every-3-weeks administration of carboplatin and paclitaxel for patients with previously untreated advanced non–small-cell lung cancer. J. Clin. Oncol. 2008;26:468–473. doi: 10.1200/JCO.2007.13.1912. [DOI] [PubMed] [Google Scholar]
- 109.Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, Mannel RS, DeGeest K, Hartenbach EM, Baergen R. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J. Clin. Oncol. 2003;21:3194–3200. doi: 10.1200/JCO.2003.02.153. [DOI] [PubMed] [Google Scholar]
- 110.Sun S, Tang L, Zhang J, Lv F, Wang Z, Wang L, Zhang Q, Zheng C, Qiu L, Jia Z. Cisplatin improves antitumor activity of weekly nab-paclitaxel in patients with metastatic breast cancer. Int. J. Nanomedicine. 2014;9:1443. doi: 10.2147/IJN.S58275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Honecker F, Kollmannsberger C, Quietzsch D, Haag C, Schroeder M, Spott C, Hartmann J, Baronius W, Hempel V, Kanz L. Phase II study of weekly paclitaxel plus 24-h continuous infusion 5-fluorouracil, folinic acid and 3-weekly cisplatin for the treatment of patients with advanced gastric cancer. Anti-Cancer Drugs. 2002;13:497–503. doi: 10.1097/00001813-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 112.Gatzemeier U, Pluzanska A, Szczesna A, Kaukel E, Roubec J, De Rosa F, Milanowski J, Karnicka-Mlodkowski H, Pesek M, Serwatowski P. Phase III study of erlotinib in combination with cisplatin and gemcitabine in advanced non–small-cell lung cancer: The Tarceva Lung Cancer Investigation Trial. J. Clin. Oncol. 2007;25:1545–1552. doi: 10.1200/JCO.2005.05.1474. [DOI] [PubMed] [Google Scholar]
- 113.Wendel H-G, de Stanchina E, Fridman JS, Malina A, Ray S, Kogan S, Cordon-Cardo C, Pelletier J, Lowe SW. Survival signalling by Akt and eIF4E in oncogenesis and cancer therapy. Nature. 2004;428:332–337. doi: 10.1038/nature02369. [DOI] [PubMed] [Google Scholar]
- 114.Aryal S, Hu C-MJ, Zhang L. Polymeric nanoparticles with precise ratiometric control over drug loading for combination therapy. Mol. Pharm. 2011;8:1401–1407. doi: 10.1021/mp200243k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lammers T, Subr V, Ulbrich K, Peschke P, Huber PE, Hennink WE, Storm G. Simultaneous delivery of doxorubicin and gemcitabine to tumors in vivo using prototypic polymeric drug carriers. Biomaterials. 2009;30:3466–3475. doi: 10.1016/j.biomaterials.2009.02.040. [DOI] [PubMed] [Google Scholar]
- 116.Kitano H. A robustness-based approach to systems-oriented drug design. Nat. Rev. Drug Discovery. 2007;5:202–210. doi: 10.1038/nrd2195. [DOI] [PubMed] [Google Scholar]
- 117.Bell A. Antimalarial drug synergism and antagonism: mechanistic and clinical significance. FEMS Microbiol. Lett. 2005;253:171–184. doi: 10.1016/j.femsle.2005.09.035. [DOI] [PubMed] [Google Scholar]
- 118.Chou T-C. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol. Rev. 2006;58:621–681. doi: 10.1124/pr.58.3.10. [DOI] [PubMed] [Google Scholar]
- 119.Berenbaum M. Synergy, additivism and antagonism in immunosuppression. A critical review. Clin. Exp. Immunol. 1977;28:1. [PMC free article] [PubMed] [Google Scholar]
- 120.Tacar O, Sriamornsak P, Dass CR. Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems. J. Pharm. Pharmacol. 2013;65:157–170. doi: 10.1111/j.2042-7158.2012.01567.x. [DOI] [PubMed] [Google Scholar]
- 121.Gabizon A, Shmeeda H, Grenader T. Pharmacological basis of pegylated liposomal doxorubicin: impact on cancer therapy. Eur. J. Pharm. Sci. 2012;45:388–398. doi: 10.1016/j.ejps.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 122.Ganz W, Sridhar K, Ganz S, Gonzalez R, Chakko S, Serafini A. Review of tests for monitoring doxorubicin-lnduced cardiomyopathy. Oncology. 1996;53:461–470. doi: 10.1159/000227621. [DOI] [PubMed] [Google Scholar]
- 123.Saltiel E, McGuire W. Doxorubicin (adriamycin) cardiomyopathy—a critical review. West. J. Med. 1983;139:332. [PMC free article] [PubMed] [Google Scholar]
- 124.Lv S, Tang Z, Li M, Lin J, Song W, Liu H, Huang Y, Zhang Y, Chen X. Co-delivery of doxorubicin and paclitaxel by PEG-polypeptide nanovehicle for the treatment of non-small cell lung cancer. Biomaterials. 2014;35:6118–6129. doi: 10.1016/j.biomaterials.2014.04.034. [DOI] [PubMed] [Google Scholar]
- 125.Wang H, Zhao Y, Wu Y, Hu Y.-l., Nan K, Nie G, Chen H. Enhanced anti-tumor efficacy by co-delivery of doxorubicin and paclitaxel with amphiphilic methoxy PEG-PLGA copolymer nanoparticles. Biomaterials. 2011;32:8281–8290. doi: 10.1016/j.biomaterials.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 126.Sun R, Liu Y, Li S-Y, Shen S, Du X-J, Xu C-F, Cao Z-T, Bao Y, Zhu Y-H, Li Y-P. Co-delivery of all-trans-retinoic acid and doxorubicin for cancer therapy with synergistic inhibition of cancer stem cells. Biomaterials. 2015;37:405–414. doi: 10.1016/j.biomaterials.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 127.Sengupta S, Eavarone D, Capila I, Zhao G, Watson N, Kiziltepe T, Sasisekharan R. Temporal targeting of tumour cells and neovasculature with a nanoscale delivery system. Nature. 2005;436:568–572. doi: 10.1038/nature03794. [DOI] [PubMed] [Google Scholar]
- 128.Marupudi NI, Han JE, Li KW, Renard VM, Tyler BM, Brem H. Paclitaxel: a review of adverse toxicities and novel delivery strategies. Expert Opin. Drug Saf. 2007;6:609–621. doi: 10.1517/14740338.6.5.609. [DOI] [PubMed] [Google Scholar]
- 129.Ma P, Mumper RJ. Paclitaxel nano-delivery systems: a comprehensive review. J. Nanomed. Nanotechnol. 2013;4:1000164. doi: 10.4172/2157-7439.1000164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Blagosklonny MV, Fojo T. Molecular effects of paclitaxel: myths and reality (a critical review) Int. J. Cancer. 1999;83:151–156. doi: 10.1002/(sici)1097-0215(19991008)83:2<151::aid-ijc1>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 131.Fan W. Possible mechanisms of paclitaxel-induced apoptosis. Biochem. Pharmacol. 1999;57:1215–1221. doi: 10.1016/s0006-2952(99)00006-4. [DOI] [PubMed] [Google Scholar]
- 132.Wood AJ, Rowinsky EK, Donehower RC. Paclitaxel (taxol) N. Engl. J. Med. 1995;332:1004–1014. doi: 10.1056/NEJM199504133321507. [DOI] [PubMed] [Google Scholar]
- 133.Horwitz S. Taxol (paclitaxel): mechanisms of action. Ann. Oncol. 1993;5:S3–6. [PubMed] [Google Scholar]
- 134.Cragg GM. Paclitaxel (Taxol®): a success story with valuable lessons for natural product drug discovery and development. Med. Res. Rev. 1998;18:315–331. doi: 10.1002/(sici)1098-1128(199809)18:5<315::aid-med3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 135.Rowinsky E, Chaudhry V, Cornblath D, Donehower R. Neurotoxicity of taxol. J. Natl. Cancer Inst. Monogr. 1992:107–115. [PubMed] [Google Scholar]
- 136.Guchelaar H-J, Ten Napel C, De Vries E, Mulder N. Clinical, toxicological and pharmaceutical aspects of the antineoplastic drug taxol: a review. Clin. Oncol. 1994;6:40–48. doi: 10.1016/s0936-6555(05)80367-x. [DOI] [PubMed] [Google Scholar]
- 137.Aryal S, Hu CMJ, Zhang L. Combinatorial Drug Conjugation Enables Nanoparticle Dual-Drug Delivery. Small. 2010;6:1442–1448. doi: 10.1002/smll.201000631. [DOI] [PubMed] [Google Scholar]
- 138.Wang W, Song H, Zhang J, Li P, Li C, Wang C, Kong D, Zhao Q. An injectable, thermosensitive and multicompartment hydrogel for simultaneous encapsulation and independent release of a drug cocktail as an effective combination therapy platform. J. Control. Release. 2015;203:57–66. doi: 10.1016/j.jconrel.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 139.Siddik ZH. Cisplatin: mode of cytotoxic action and molecular basis of resistance. Oncogene. 2003;22:7265–7279. doi: 10.1038/sj.onc.1206933. [DOI] [PubMed] [Google Scholar]
- 140.Barabas K, Milner R, Lurie D, Adin C. Cisplatin: a review of toxicities and therapeutic applications. Vet. Comp. Oncol. 2008;6:1–18. doi: 10.1111/j.1476-5829.2007.00142.x. [DOI] [PubMed] [Google Scholar]
- 141.Desale SS, Cohen SM, Zhao Y, Kabanov AV, Bronich TK. Biodegradable hybrid polymer micelles for combination drug therapy in ovarian cancer. J. Control. Release. 2013;171:339–348. doi: 10.1016/j.jconrel.2013.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Xiao H, Song H, Yang Q, Cai H, Qi R, Yan L, Liu S, Zheng Y, Huang Y, Liu T. A prodrug strategy to deliver cisplatin (IV) and paclitaxel in nanomicelles to improve efficacy and tolerance. Biomaterials. 2012;33:6507–6519. doi: 10.1016/j.biomaterials.2012.05.049. [DOI] [PubMed] [Google Scholar]
- 143.Cai L, Xu G, Shi C, Guo D, Wang X, Luo J. Telodendrimer nanocarrier for co-delivery of paclitaxel and cisplatin: A synergistic combination nanotherapy for ovarian cancer treatment. Biomaterials. 2015;37:456–468. doi: 10.1016/j.biomaterials.2014.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dingle BH, Rumble RB, Brouwers MC. The role of gemcitabine in the treatment of cholangiocarcinoma and gallbladder cancer: a systematic review. Can. J. Gastroenterol. 2005;19:711–716. doi: 10.1155/2005/565479. [DOI] [PubMed] [Google Scholar]
- 145.Aapro MS, Martin C, Hatty S. Gemcitabine-a safety review. Anti-Cancer Drugs. 1998;9:191–202. doi: 10.1097/00001813-199803000-00001. [DOI] [PubMed] [Google Scholar]
- 146.Meng H, Wang M, Liu H, Liu X, Situ A, Wu B, Ji Z, Chang CH, Nel AE. Use of a Lipid-Coated Mesoporous Silica Nanoparticle Platform for Synergistic Gemcitabine and Paclitaxel Delivery to Human Pancreatic Cancer in Mice. ACS Nano. 2015;9:3540–3557. doi: 10.1021/acsnano.5b00510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Huang P, Wang D, Su Y, Huang W, Zhou Y, Cui D, Zhu X, Yan D. Combination of Small Molecule Prodrug and Nanodrug Delivery: Amphiphilic Drug–Drug Conjugate for Cancer Therapy. J. Am. Chem. Soc. 2014;136:11748–11756. doi: 10.1021/ja505212y. [DOI] [PubMed] [Google Scholar]
- 148.Ramesh M, Ahlawat P, Srinivas NR. Irinotecan and its active metabolite, SN-38: review of bioanalytical methods and recent update from clinical pharmacology perspectives. Biomed. Chromatogr. 2010;24:104–123. doi: 10.1002/bmc.1345. [DOI] [PubMed] [Google Scholar]
- 149.Steinberg AD. Chlorambucil in the treatment of patients with immune-mediated rheumatic diseases. Arthritis. Rheum. 1993;36:325–328. doi: 10.1002/art.1780360306. [DOI] [PubMed] [Google Scholar]
- 150.Jain AK, Thanki K, Jain S. Co-encapsulation of tamoxifen and quercetin in polymeric nanoparticles: implications on oral bioavailability, antitumor efficacy, and drug-induced toxicity. Mol. Pharm. 2013;10:3459–3474. doi: 10.1021/mp400311j. [DOI] [PubMed] [Google Scholar]
- 151.Jordan VC. Tamoxifen: a most unlikely pioneering medicine. Nat. Rev. Drug Discovery. 2003;2:205–213. doi: 10.1038/nrd1031. [DOI] [PubMed] [Google Scholar]
- 152.Cho SK, Pedram A, Levin ER, Kwon YJ. Acid-degradable core–shell nanoparticles for reversed tamoxifen-resistance in breast cancer by silencing manganese superoxide dismutase (MnSOD) Biomaterials. 2013;34:10228–10237. doi: 10.1016/j.biomaterials.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Granado-Serrano AB, Martín MA, Bravo L, Goya L, Ramos S. Quercetin induces apoptosis via caspase activation, regulation of Bcl-2, and inhibition of PI-3-kinase/Akt and ERK pathways in a human hepatoma cell line (HepG2) The Journal of nutrition. 2006;136:2715–2721. doi: 10.1093/jn/136.11.2715. [DOI] [PubMed] [Google Scholar]
- 154.Mills EJ, Thorlund K, Ioannidis JP. Calculating additive treatment effects from multiple randomized trials provides useful estimates of combination therapies. J. Clin. Epidemiol. 2012;65:1282–1288. doi: 10.1016/j.jclinepi.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 155.Touma SE, Goldberg JS, Moench P, Guo X, Tickoo SK, Gudas LJ, Nanus DM. Retinoic acid and the histone deacetylase inhibitor trichostatin a inhibit the proliferation of human renal cell carcinoma in a xenograft tumor model. Clin. Cancer Res. 2005;11:3558–3566. doi: 10.1158/1078-0432.CCR-04-1155. [DOI] [PubMed] [Google Scholar]
- 156.Li M, Tang Z, Lv S, Song W, Hong H, Jing X, Zhang Y, Chen X. Cisplatin crosslinked pH-sensitive nanoparticles for efficient delivery of doxorubicin. Biomaterials. 2014;35:3851–3864. doi: 10.1016/j.biomaterials.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 157.Gately D, Howell S. Cellular accumulation of the anticancer agent cisplatin: a review. Br. J. Cancer. 1993;67:1171. doi: 10.1038/bjc.1993.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hurley LH. DNA and its associated processes as targets for cancer therapy. Nat. Rev. Cancer. 2002;2:188–200. doi: 10.1038/nrc749. [DOI] [PubMed] [Google Scholar]
- 159.Görlich D. Transport into and out of the cell nucleus. The EMBO journal. 1998;17:2721–2727. doi: 10.1093/emboj/17.10.2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Robertson JD, Orrenius S, Zhivotovsky B. Review: nuclear events in apoptosis. J. Struct. Biol. 2000;129:346–358. doi: 10.1006/jsbi.2000.4254. [DOI] [PubMed] [Google Scholar]
- 161.Zhong J, Li L, Zhu X, Guan S, Yang Q, Zhou Z, Zhang Z, Huang Y. A smart polymeric platform for multistage nucleus-targeted anticancer drug delivery. Biomaterials. 2015;65:43–55. doi: 10.1016/j.biomaterials.2015.06.042. [DOI] [PubMed] [Google Scholar]
- 162.Lee S-M, O'Halloran TV, Nguyen ST. Polymer-caged nanobins for synergistic cisplatin–doxorubicin combination chemotherapy. J. Am. Chem. Soc. 2010;132:17130–17138. doi: 10.1021/ja107333g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bae Y, Diezi TA, Zhao A, Kwon GS. Mixed polymeric micelles for combination cancer chemotherapy through the concurrent delivery of multiple chemotherapeutic agents. J. Control. Release. 2007;122:324–330. doi: 10.1016/j.jconrel.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 164.Chen Y, Gao Y, Chen H, Zeng D, Li Y, Zheng Y, Li F, Ji X, Wang X, Chen F. Engineering Inorganic Nanoemulsions/Nanoliposomes by Fluoride - Silica Chemistry for Efficient Delivery/Co-Delivery of Hydrophobic Agents. Adv. Funct. Mater. 2012;22:1586–1597. [Google Scholar]
- 165.Tai W, Mo R, Lu Y, Jiang T, Gu Z. Folding graft copolymer with pendant drug segments for co-delivery of anticancer drugs. Biomaterials. 2014;35:7194–7203. doi: 10.1016/j.biomaterials.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Miao L, Guo S, Zhang J, Kim WY, Huang L. Nanoparticles with Precise Ratiometric Co-Loading and Co-Delivery of Gemcitabine Monophosphate and Cisplatin for Treatment of Bladder Cancer. Adv. Funct. Mater. 2014;24:6601–6611. doi: 10.1002/adfm.201401076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Chou T-C, Talalay P. Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 1984;22:27–55. doi: 10.1016/0065-2571(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 168.Ashley CE, Carnes EC, Phillips GK, Padilla D, Durfee PN, Brown PA, Hanna TN, Liu J, Phillips B, Carter MB. The targeted delivery of multicomponent cargos to cancer cells by nanoporous particle-supported lipid bilayers. Nat. Mater. 2011;10:389–397. doi: 10.1038/nmat2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Li F, Zhao X, Wang H, Zhao R, Ji T, Ren H, Anderson GJ, Nie G, Hao J. Multiple Layer- by - Layer Lipid - Polymer Hybrid Nanoparticles for Improved FOLFIRINOX Chemotherapy in Pancreatic Tumor Models. Adv. Funct. Mater. 2015;25:788–798. [Google Scholar]
- 170.Liao L, Liu J, Dreaden EC, Morton SW, Shopsowitz KE, Hammond PT, Johnson JA. A convergent synthetic platform for single-nanoparticle combination cancer therapy: ratiometric loading and controlled release of cisplatin, doxorubicin, and camptothecin. J. Am. Chem. Soc. 2014;136:5896–5899. doi: 10.1021/ja502011g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Barui S, Saha S, Mondal G, Haseena S, Chaudhuri A. Simultaneous delivery of doxorubicin and curcumin encapsulated in liposomes of pegylated RGDK-lipopeptide to tumor vasculature. Biomaterials. 2014;35:1643–1656. doi: 10.1016/j.biomaterials.2013.10.074. [DOI] [PubMed] [Google Scholar]
- 172.Bar-Sela G, Epelbaum R, Schaffer M. Curcumin as an anti-cancer agent: review of the gap between basic and clinical applications. Curr. Med. Chem. 2010;17:190–197. doi: 10.2174/092986710790149738. [DOI] [PubMed] [Google Scholar]
- 173.Wilken R, Veena MS, Wang MB, Srivatsan ES. Curcumin: A review of anti-cancer properties and therapeutic activity in head and neck squamous cell carcinoma. Mol. Cancer. 2011;10:1–19. doi: 10.1186/1476-4598-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Duan X, Xiao J, Yin Q, Zhang Z, Yu H, Mao S, Li Y. Smart pH-sensitive and temporal-controlled polymeric micelles for effective combination therapy of doxorubicin and disulfiram. ACS Nano. 2013;7:5858–5869. doi: 10.1021/nn4010796. [DOI] [PubMed] [Google Scholar]
- 175.Loo TW, Clarke DM. Blockage of drug resistance in vitro by disulfiram, a drug used to treat alcoholism. J. Natl. Cancer Inst. 2000;92:898–902. doi: 10.1093/jnci/92.11.898. [DOI] [PubMed] [Google Scholar]
- 176.Loo TW, Bartlett MC, Clarke DM. Disulfiram metabolites permanently inactivate the human multidrug resistance P-glycoprotein. Mol. Pharm. 2004;1:426–433. doi: 10.1021/mp049917l. [DOI] [PubMed] [Google Scholar]
- 177.Gottesman MM. Mechanisms of cancer drug resistance. Annu. Rev. Med. 2002;53:615–627. doi: 10.1146/annurev.med.53.082901.103929. [DOI] [PubMed] [Google Scholar]
- 178.Nielsen D, Skovsgaard T. P-glycoprotein as multidrug transporter: a critical review of current multidrug resistant cell lines. Biochim. Biophys. Acta. 1992;1139:169–183. doi: 10.1016/0925-4439(92)90131-6. [DOI] [PubMed] [Google Scholar]
- 179.Dorsett Y, Tuschl T. siRNAs: applications in functional genomics and potential as therapeutics. Nat. Rev. Drug Discovery. 2004;3:318–329. doi: 10.1038/nrd1345. [DOI] [PubMed] [Google Scholar]
- 180.Li J, Wang Y, Zhu Y, Oupický D. Recent advances in delivery of drug–nucleic acid combinations for cancer treatment. J. Control. Release. 2013;172:589–600. doi: 10.1016/j.jconrel.2013.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Meng H, Mai WX, Zhang H, Xue M, Xia T, Lin S, Wang X, Zhao Y, Ji Z, Zink JI. Codelivery of an optimal drug/siRNA combination using mesoporous silica nanoparticles to overcome drug resistance in breast cancer in vitro and in vivo. ACS Nano. 2013;7:994–1005. doi: 10.1021/nn3044066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Xiong X-B, Lavasanifar A. Traceable multifunctional micellar nanocarriers for cancer-targeted co-delivery of MDR-1 siRNA and doxorubicin. ACS Nano. 2011;5:5202–5213. doi: 10.1021/nn2013707. [DOI] [PubMed] [Google Scholar]
- 183.Xu X, Xie K, Zhang X-Q, Pridgen EM, Park GY, Cui DS, Shi J, Wu J, Kantoff PW, Lippard SJ. Enhancing tumor cell response to chemotherapy through nanoparticle-mediated codelivery of siRNA and cisplatin prodrug. Proc. Natl. Acad. Sci. U. S. A. 2013;110:18638–18643. doi: 10.1073/pnas.1303958110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Morton SW, Lee MJ, Deng ZJ, Dreaden EC, Siouve E, Shopsowitz KE, Shah NJ, Yaffe MB, Hammond PT. A nanoparticle-based combination chemotherapy delivery system for enhanced tumor killing by dynamic rewiring of signaling pathways. Sci. Signal. 2014;7:ra44. doi: 10.1126/scisignal.2005261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Fang RH, Zhang L. Combinatorial Nanotherapeutics: Rewiring, Then Killing. Cancer Cells, Sci. Signal. 2014;7:pe13–pe13. doi: 10.1126/scisignal.2005386. [DOI] [PubMed] [Google Scholar]
- 186.Bergh J, Bondarenko IM, Lichinitser MR, Liljegren A, Greil R, Voytko NL, Makhson AN, Cortes J, Lortholary A, Bischoff J. First-line treatment of advanced breast cancer with sunitinib in combination with docetaxel versus docetaxel alone: results of a prospective, randomized phase III study. J. Clin. Oncol. 2012;30:921–929. doi: 10.1200/JCO.2011.35.7376. [DOI] [PubMed] [Google Scholar]
- 187.Gradishar WJ, Meza LA, Amin B, Samid D, Hill T, Chen Y-M, Lower EE, Marcom PK. Capecitabine plus paclitaxel as front-line combination therapy for metastatic breast cancer: a multicenter phase II study. J. Clin. Oncol. 2004;22:2321–2327. doi: 10.1200/JCO.2004.12.128. [DOI] [PubMed] [Google Scholar]
- 188.Lehár J, Krueger AS, Avery W, Heilbut AM, Johansen LM, Price ER, Rickles RJ, Short GF, Iii, Staunton JE, Jin X. Synergistic drug combinations tend to improve therapeutically relevant selectivity. Nat. Biotechnol. 2009;27:659–666. doi: 10.1038/nbt.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Jiang T, Mo R, Bellotti A, Zhou J, Gu Z. Gel–Liposome-Mediated Co-Delivery of Anticancer Membrane-Associated Proteins and Small-Molecule Drugs for Enhanced Therapeutic Efficacy. Adv. Funct. Mater. 2014;24:2295–2304. [Google Scholar]
- 190.Jiang T, Sun W, Zhu Q, Burns NA, Khan SA, Mo R, Gu Z. Furin-Mediated Sequential Delivery of Anticancer Cytokine and Small-Molecule Drug Shuttled by Graphene. Adv. Mater. 2015;27:1021–1028. doi: 10.1002/adma.201404498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hu Q, Sun W, Qian C, Wang C, Bomba HN, Gu Z. Anticancer Platelet-Mimicking Nanovehicles. Adv. Mater. 2015 doi: 10.1002/adma.201503323. DOI: 10.1002/adma.201503323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Noh J, Kwon B, Han E, Park M, Yang W, Cho W, Yoo W, Khang G, Lee D. Amplification of oxidative stress by a dual stimuli-responsive hybrid drug enhances cancer cell death. Nat. Commun. 2015;6 doi: 10.1038/ncomms7907. [DOI] [PubMed] [Google Scholar]
- 193.Setyawati MI, Tay CY, Docter D, Stauber RH, Leong DT. Understanding and exploiting nanoparticles' intimacy with the blood vessel and blood. Chem. Soc. Rev. 2015 doi: 10.1039/c5cs00499c. DOI: 10.1039/C5CS00499C. [DOI] [PubMed] [Google Scholar]
- 194.Mitragotri S, Anderson DG, Chen X, Chow EK, Ho D, Kabanov AV, Karp JM, Kataoka K, Mirkin CA, Petrosko SH. Accelerating the translation of nanomaterials in biomedicine. ACS Nano. 2015;9:6644–6654. doi: 10.1021/acsnano.5b03569. [DOI] [PMC free article] [PubMed] [Google Scholar]