Abstract
To date very few studies with small sample size have compared peroral esophageal myotomy (POEM) with the current surgical standard of care, laparoscopic Heller myotomy (LHM), in terms of efficacy and safety, and no recommendations have been proposed.
To investigate the efficacy and safety of POEM compared with LHM, for the treatment of achalasia.
The databases of Pubmed, Medline, Cochrane, and Ovid were systematically searched between January 1, 2005 and January 31, 2015, with the medical subject headings (MeSH) and keywords “achalasia,” “POEM,” “per oral endoscopic myotomy,” and “peroral endoscopic myotomy,” “laparoscopic Heller myotomy” (LHM), “Heller myotomy.”
All types of study designs including adult patients with diagnosis of achalasia were selected. Studies that did not report the comparison between endoscopic and surgical treatment, experimental studies in animal models, single case reports, technical reports, reviews, abstracts, and editorials were excluded.
The total number of included patients was 486 (196 in POEM group and 290 in LHM group).
There were no differences between POEM and LHM in reduction in Eckardt score (MD = −0.659, 95% CI: −1.70 to 0.38, P = 0.217), operative time (MD = −0.354, 95% CI: −1.12 to 0.41, P = 0.36), postoperative pain scores (MD = −1.86, 95% CI: −5.17 to 1.44, P = 0.268), analgesic requirements (MD = −0.74, 95% CI: −2.65 to 1.16, P = 0.445), and complications (OR = 1.11, 95% CI: 0.5–2.44, P = 0.796). Length of hospital stay was significantly lower for POEM (MD = −0.629, 95% CI: −1.256 to −0.002, P = 0.049). There was a trend toward significant reduction in symptomatic gastroesophageal reflux rate in favors of LHM compared to POEM group (OR = 1.81, 95% CI: 1.11–2.95, P = 0.017).
All included studied were not randomized. Furthermore all selected studies did not report the results of follow-up longer than 1 year and most of them included patients who were both treatment naive and underwent previous endoscopic or surgical interventions for achalasia.
POEM represents a safe and efficacy procedure comparable to the safety profile of LHM for achalasia at a short-term follow-up. Long-term clinical trials are urgently needed.
INTRODUCTION
Achalasia is a disorder of esophageal motility characterized by an incomplete or absent esophagogastric junction (EGJ) relaxation associated with loss of peristalsis or uncoordinated contractions of the esophageal body in response to swallowing. The subsequent functional EGJ outflow obstruction and ineffective food bolus transit result in progressively severe dysphagia for liquids and solids, and can additionally cause nonacid regurgitation, aspiration, chest pain, weight loss, and eventually an irreversible dilation of the esophageal body.1–3 All the current available therapeutic interventions have palliative intent and seek to abolish the EGJ pressures in order to facilitate passive transit of food boluses into the stomach improving the symptoms related to esophageal stasis.4–6 Although over the years pharmacotherapy (calcium channel antagonists, nitrates) and endoscopic injection of botulinum toxin have been favored as possible treatment modalities, the current standard of care include either endoscopic pneumatic dilation or surgical myotomy (laparoscopic Heller myotomy (LHM)) across the EGJ. A recent randomized trial found these 2 treatment options to have similar efficacy in terms of symptom relief at 2-year follow-up.5,7 Considerable evidence exists, however, that LHM provides the most durable symptoms improvement8,9 without the need for repeated and multiple interventions to maintain this effect, contrarily to what is often necessary with endoscopic pneumatic dilation.6–8
In 2010, Inoue et al10 introduced the peroral esophageal myotomy (POEM), a novel procedure for the treatment of achalasia that combined peculiarities of both endoscopic dilation (no skin incisions, decreased pain, and less blood loss) and LHM (durable surgical myotomy and single procedure). Since then, several single and multicenter institution POEM case series have demonstrated excellent results in terms of symptomatic relief and improvement in EGJ physiology at short-term follow-up, confirming the feasibility of this technique for the treatment of achalasia.11–13 Nevertheless, very few studies with small sample size have compared POEM with the current surgical standard of care, LHM, in terms of efficacy and safety, and no recommendations have been proposed. Therefore, a systematic review and meta-analysis was conducted to investigate if there is a significant difference in efficacy and safety between POEM and LHM for the treatment of esophageal achalasia in the adult patients.
METHODS
Searches
We planned and performed this systematic review and meta-analysis in accordance with Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement14 and Cochrane Handbook for Systematic Reviews of Intervention.15 We critically assessed the reporting quality of the study according to the PRISMA 2009 checklists.16 A literature search in Pubmed, Medline, Cochrane, and Ovid databases of all articles published, between January 1, 2005 and January 31, 2015 with the medical subject headings (MeSH) and keywords “achalasia,” “POEM,” “per oral endoscopic myotomy,” and “peroral endoscopic myotomy,” “laparoscopic Heller myotomy,” “Heller myotomy” was independently carried out by two investigators. The key words were used in all possible combinations to obtain the maximal number of articles.
Selection
The articles were then screened for the presence of the following inclusion criteria: adult patients with diagnosis of achalasia. All types of study designs were included. Studies that did not report the comparison between endoscopic (POEM) and surgical (LHM) treatment, experimental studies in animal models, single case reports, technical reports, reviews, abstracts, and editorials were excluded. There were no language restrictions in the selection. The bibliography of all selected articles was hand searched to identify additional articles that met our inclusion criteria. In cases where multiple publications were available with increasing number of patients or longer follow-up for the same group, only data from the most recent article were used for statistical analysis.
Data Extraction
Two of the authors (LM and AP) independently reviewed the formal published versions of all eligible studies for content and screened them according to the specified inclusion criteria using a data extraction form based on the Cochrane Consumers and Communication Review Group's data extraction template.15 Disagreements were resolved by discussion between the 2 review authors; if no agreement could be reached, it was planned a third author which would decide.
The following data were recorded: type of study design, mono- or multicentricity, country of origin, year of publication, number of patients, median/mean patient age, gender distribution, preoperative Eckardt score, procedural time (in minutes), intra- and postoperative complications, postoperative pain score, postoperative analgesic dose (mg of morphine equivalents), days of hospitalization, follow-up duration (in months), postoperative Eckardt score and postprocedure symptomatic gastroesophageal reflux (GER).
The ethical approval was not necessary for this type of article.
Summary Measures
The primary outcome measure was the mean difference in reducing Eckardt score comparing POEM to LHM. The mean difference in procedure time, length of hospital stay, postoperative pain score and analgesic requirement, as well as the odds ratio (OR) of complications and postprocedure symptomatic GER comparing POEM to LHM was investigated as a secondary analysis.
Risk of Bias Assessment
A Cochrane risk of bias assessment tool for nonrandomized studies of interventions (ACROBAT-NRSI) was individually applied to all selected studies. The risk of bias of each study was rated as “critical risk,” “serious risk,” “moderate risk,” “low risk” or “no information” according to the match level between information extracted and evaluation criteria.15
Statistical Analysis
Effect sizes for numerical variables were expressed as difference in means with 95% confidence interval (CI); while that of categorical data were expressed as OR with 95% CI. Whenever data in individual studies were expressed as a median and range, they were converted to estimated mean ± standard deviation (SD) before analysis using “Estimation of a sample's mean and variance from its median and range software” (VassarStats: Website for Statistical Computation, www.vassarstats.net, Richard Lowry, Poughkeepsie, NY) on the basis of the sample's reported median and range according to the method devised by Hozo et al.17 A pre–post design was used for evaluating the outcomes after POEM and LHM in the same groups. Due to the small numbers of studies, we tested for heterogeneity between-study with the I2 measure.15 Percentages of around 25% (I2 = 25), 50% (I2 = 50), and 75% (I2 = 75) were considered at low, moderate, and high heterogeneity, respectively. A χ2 based Q-test was also performed to check between-study heterogeneity. When an I value higher than 50 indicated moderate heterogeneity between the studies the effect size for each study was calculated by the random-effect model DerSimonian–Laird approach.15 Alternatively a fixed-effect model was run. Publication bias was evaluated and quantified by the Egger test. With regard to outcomes when significant heterogeneity existed across studies, sensitivity analysis was performed by sequentially omitting each study to test the influence of each individual study on pooled data. In case of overlapped patients between the studies we tried to contact the corresponding authors to obtain the raw data. Otherwise the patients were excluded from the ultimate analysis. We did not produce the Funnel plot to test the publication bias due to the limited number (below 10) of studies included in each analysis.16 All analyses were performed using Comprehensive Meta-analysis software (Version 3.3.070, November 21, 2014).
RESULTS
Study Selection and Characteristics
The initial search produced 283 studies, of which 192 were selected for eligibility assessment after exclusion of duplicates. After detailed evaluation, 11 studies fulfilled criteria for eligibility. One hundred eighty-one studies that were not related to the comparison between endoscopic (POEM) and surgical (LHM) treatment were excluded. Of the remaining 11 records, 7 fulfilled criteria for inclusion in the meta-analysis.18–24 Among the 4 excluded studies, 2 were reviews and 2 were studies performed in children with esophageal achalasia.
The included retrospective case–control studies concerned different cohorts of patients published between 2013 and 2015, except for 2 studies21,24 in which the same group may overlap. The total number of included patients was 486 (196 in POEM group and 290 in LHM group) ranging from 8 to 180 patients per study. Mean (SD) age of the patients was 49.5 (11.8) years in POEM group and 47.8 (11.8) in LHM group. Among the 7 studies, 6 studies (306 patients, 63%) were performed in the United States populations, and the remaining 1 study (180 patients, 37%) was multicenter (Germany, Netherlands, Switzerland, and Canada). Perioperative symptom assessment was similar in 5 studies; in 3 studies20,21,24 high-resolution manometry were performed instead of stationary esophageal manometry and the data were evaluated according to the Chicago Classification of esophageal motility disorders.25 Previous interventions were reported for 61 cases that included: endoscopic pneumatic dilatation in 14 patients; botulinum injection in 9, combined botulinum injection with dilatation in 6, surgical myotomy in 6. Two studies did report the number of patients who underwent interventions (n = 26) but did not mention the details. Similarly, 2 studies reported the interventions but did not specify the number of patients. Only 1 study included patients without prior endoscopic or surgical treatment of achalasia. As regard the LHM operative technique, a partial anterior (Dor) or posterior (Toupet) fundoplication was performed after esophagogastric myotomy in all included patients. In all studies were registered no conversion to the other procedures or perioperative mortality. Mean (SD) follow-up resulted in 6.4 (4.6) months. The characteristics of each study included in the meta-analysis are shown in Table 1.
TABLE 1.
Characteristics of Included Studies
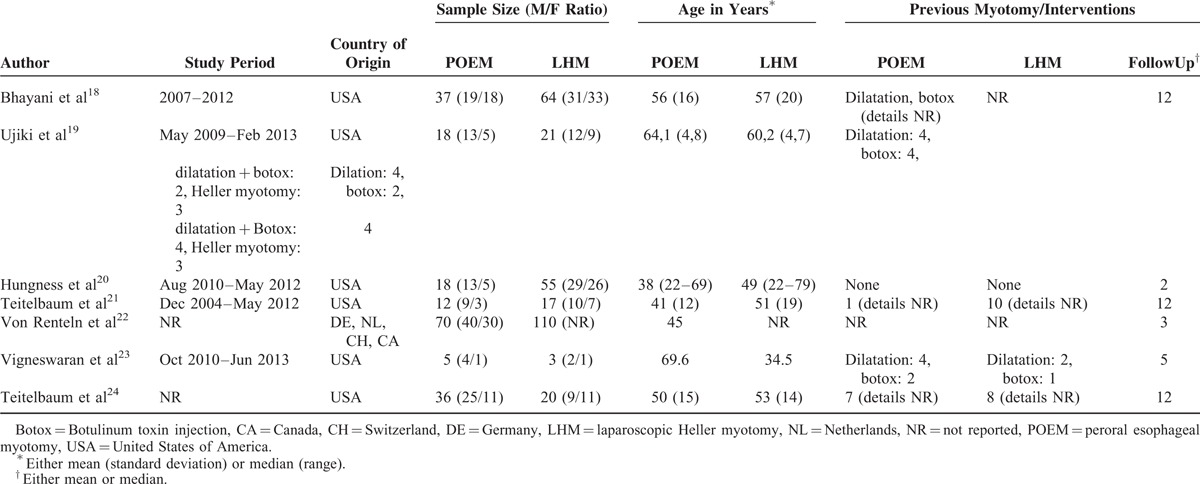
All 7 studies, 6 full-text articles and 1 brief report, were retrospective case–control studies due to limitation in surgical blinding or randomization. Nevertheless the evaluation of each study followed by the Cochrane risk of bias assessment tool for nonrandomized studies of interventions (ACROBAT-NRSI) resulted in “Moderate risk of bias” judgment for all studies.
Quantitative Data Synthesis
Eckardt Score Reduction
Five studies reported available data regarding the reduction in Eckardt score. The outcome showed no significant difference between POEM and LHM (MD = −0.659, 95% CI: −1.70 to 0.38, P = 0.217) (Figure 1). Significant heterogeneity existed among the included studies (I2 = 94.3%, P < 0.001), and a random-effect analysis model was used. Sensitivity analysis by sequentially omitting each study did not alter the primary outcome. Furthermore 2 studies were from the same groups,21,24 which led to a possibility of double reporting of cases. In order to negate this only data from the most recent article were used for statistical analysis.
FIGURE 1.
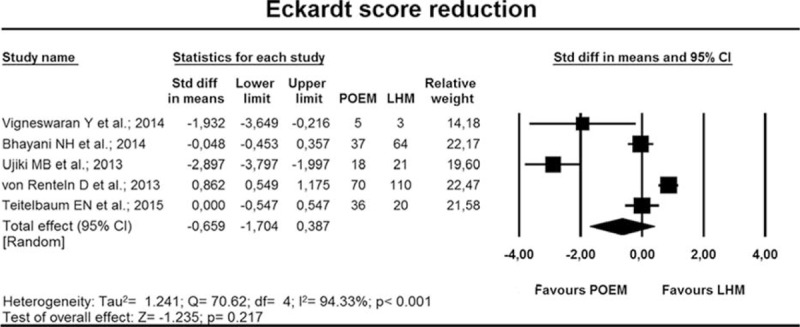
Forrest plot showing comparison of the efficacy of POEM with LHM in reducing Eckardt score.
Operative Time and Hospital Stay
No significant difference between POEM and LHM was found regarding the operative time (MD = −0.354, 95% CI: −1.12 to 0.41, P = 0.36) (Figure 2). A random-effect analysis model was run due to significant heterogeneity between studies (I2 = 82.1%, P = 0.001). The same studies were pooled in the analysis as regard the length of hospital stay, resulting in a lower hospital time of POEM compared with LHM (MD = −0.629, 95% CI: −1.256 to −0.002, P = 0.049) (Figure 3). Significant heterogeneity was found among the included studies (I2 = 71.8%, P = 0.014), and a random-effect analysis model was used. Sensitivity analysis was repeated sequentially omitting each study without primary outcome alteration.
FIGURE 2.
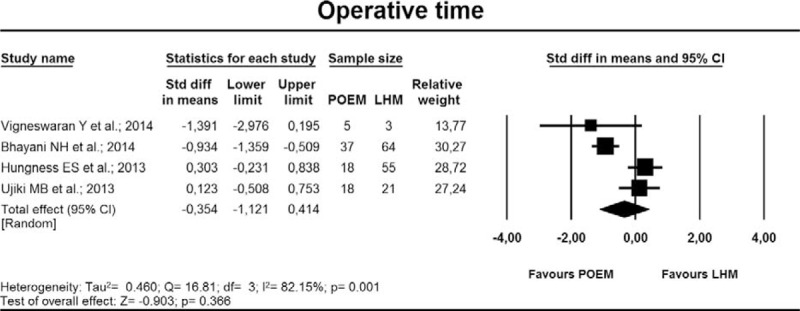
Forrest plot showing comparison of operative time required for POEM with that for LHM.
FIGURE 3.
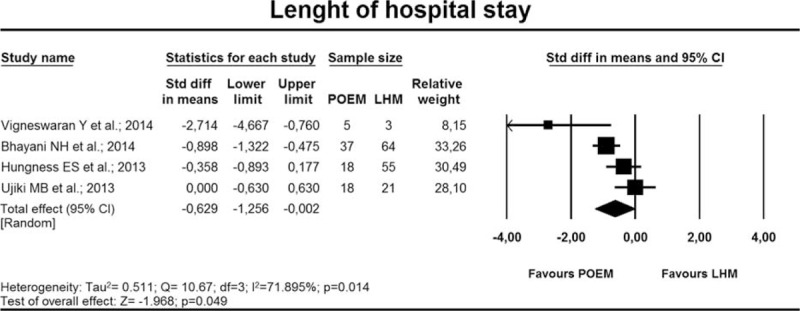
Forrest plot showing comparison of the length of hospital stay after POEM with that after LHM.
Postoperative Pain Score and Analgesic Requirement
There was no statistically significant difference in the reduction of postoperative pain score (MD = −1.86, 95% CI: −5.17 to 1.44, P = 0.268) (Figure 4) and analgesic medication (mg of morphine equivalent) dose (MD = −0.74, 95% CI: −2.65 to 1.16, P = 0.445) (Figure 5) resulting from the analysis of data of 2 studies. Significant heterogeneity was found among the included studies regarding the investigated outcomes (I2 = 97%, P < 0.001) and (I2 = 94.3%, P < 0.001), respectively.
FIGURE 4.
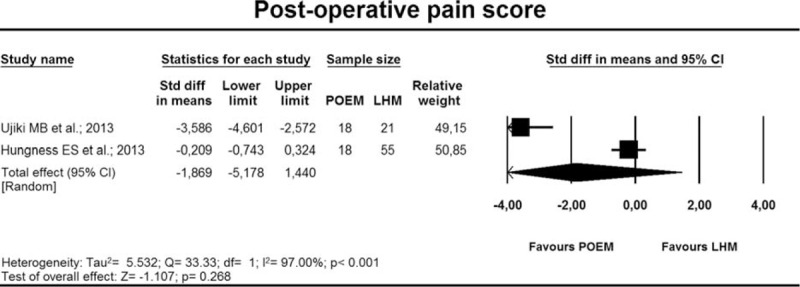
Forrest plot showing comparison of postoperative pain score after POEM with that after LHM.
FIGURE 5.
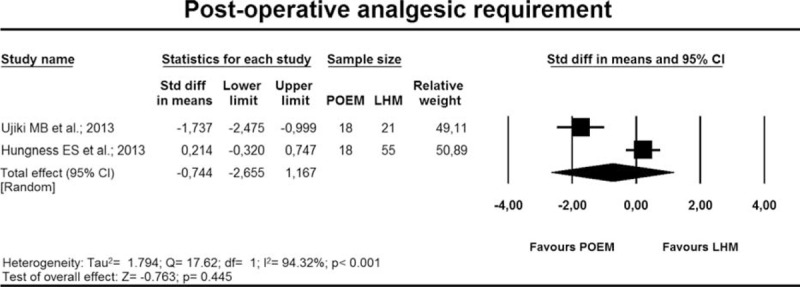
Forrest plot showing comparison of postoperative analgesic requirement after POEM with that after LHM.
Complications
Four studies reported available data regarding the complication rate. Bleeding and perioperative perforation were indexed as major complications, while urinary retention, splenic capsular injury, atrial fibrillation, vagal nerve injury, and subcutaneous emphysema were listed as minor complications according to Clavien–Dindo classification of surgical complications.26 The results of meta-analysis of overall complications did not differ between POEM and LHM (OR = 1.11, 95% CI: 0.5–2.44, P = 0.796) (Figure 6). Similarly, there was no statistically significant difference in the major complication rate as well as minor complication rate between endoscopic and laparoscopic technique: (OR = 1.33, 95% CI: 0.24–7.35, P = 0.74) and (OR = 1.82, 95% CI: 0.48–6.9, P = 0.375), respectively (data not shown). The test for heterogeneity was not significant (I2 = 0%, P = 0.482).
FIGURE 6.
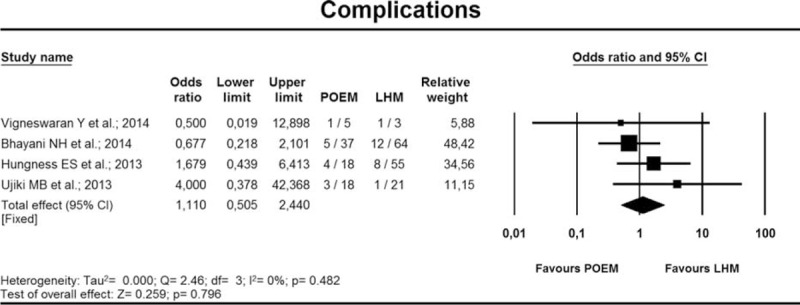
Forrest plot showing comparison of complications after POEM with that after LHM.
Postprocedure Symptomatic Gastroesophageal Reflux
Five studies reported the incidence of postprocedure symptomatic gastroesophageal reflux, which was estimated by a Gastroesophageal Reflux Disease Questionnaire (GerdQ) score ≥727 or a DeMeester score of ≥14.7% at pH testing. In the report by Bhayani et al18 the 24-hour testing of esophageal acid exposure was obtained only in 23 (76%) POEM and 31 (48%) LHM patients. The fixed effect analysis model was used because of low heterogeneity (I2 = 0%, P = 0.651). There was a trend toward significant reduction in symptomatic gastroesophageal reflux rate in favor of LHM compared to POEM group (OR = 1.81, 95% CI: 1.11–2.95, P = 0.017) (Figure 7). Furthermore sensitivity analysis was rerun sequentially omitting each study without primary outcome alteration.
FIGURE 7.
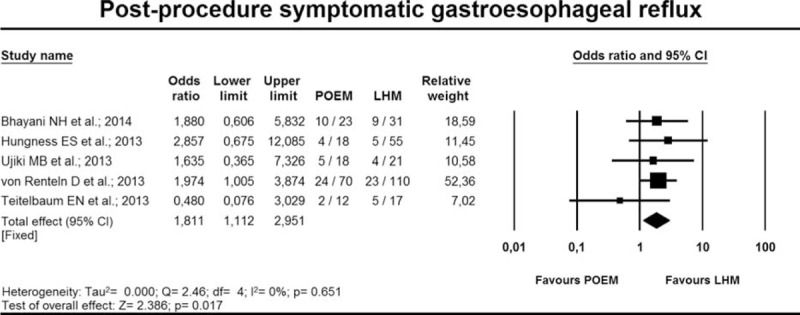
Forrest plot showing comparison of symptomatic gastroesophageal reflux after POEM with that after LHM.
DISCUSSION
In the present systematic review and meta-analysis, we demonstrate that: POEM and LHM are similar in terms of Eckardt score reduction, complications, postoperative analgesic need, operative time and length of hospital stay; POEM shows worse short-term results compared to LHM as regard the postprocedure symptomatic GER development.
Although the etiology of esophageal achalasia is scarcely understood, there is common consensus on its treatment, directed to reducing lower esophageal sphincter (LES) pressure in order to obtain symptoms relief, improve the esophageal emptying and prevent the development of megaesophagus.28 Among the various treatment modalities like pharmacotherapy (calcium channel antagonists, nitrates),28,29 endoscopic pneumatic dilatation30,31 and injection of botulinum toxin,32,33 the surgical esophagogastric extramucosal myotomy with partial fundoplication fulfilled the best short- and long-term clinical outcomes, especially with minimally invasive approach, and now is considered the treatment of choice for achalasic patients.5,7,8 Furthermore, in the last few years, there has been an impetus in the direction of a more minimal approach to achalasia and in 2010 Inoue et al10 introduced the Per-Oral Esophageal Myotomy as a promising endoscopic minimally invasive technique with overall initial good patient satisfaction and relief of dysphagia. Since then, many institutions started to investigate the feasibility, safety, and efficacy of this innovative endoscopic procedure with encouraging results.11–13 More recently, Inoue et al34 published the largest single center cohort study on 500 consecutive achalasic patients treated with POEM, reporting the longest follow-up of POEM patients registered to date (3 years). Based on this large series, POEM resulted in significant improvements in Eckardt scores and LES pressures at postoperative short- as well long-term follow up with no mortality rate and rare adverse events (3.2%), highlighting the safety and effectiveness of this treatment as first- or second-line therapy for achalasia.33
Nevertheless, very few studies with small sample size have compared POEM with the current surgical standard of care, LHM, and no recommendations have been proposed.
The current meta-analysis involved 7 studies compared POEM with Heller myotomy in a nonrandomized manner with 486 included patients (196 in POEM group and 290 in LHM group) ranging from 8 to 180 patients per study. Seven studies were all judged as “moderate risk of bias” according to Cochrane risk of bias assessment tool for nonrandomized studies of interventions (ACROBAT-NRSI).
The efficacy in reduction of Eckardt score was the primary outcome measure of this study. In terms of symptomatic efficacy, the Eckardt score (maximum score, 12) is the sum of the symptom scores for dysphagia, regurgitation, chest pain (0, absent; 1, occasional; 2, daily; and 3, each meal), and weight loss (0, no weight loss; 1, <5 kg; 2, 5–10 kg; and 3, >10 kg), representing a validated and comprehensive assessment of disease severity.34 Even though the limitations of small numbers and short-term follow-up, POEM resulted in a success rate of 90%, similar to initial treatment success of LHM.8,11 Furthermore in this present meta-analysis, we found a comparable decrease in Eckardt score between groups.
There was no significant difference between POEM and LHM as regard the time of interventions, postoperative pain score, and analgesic requirement. Indeed, length of hospital stay was significantly less in POEM compared to LHM.
Previous studies were also investigated as regard postoperative complications.
Swanstrom et al11 reported a 16.7% esophageal perforation during POEM in their preliminary experience, and Von Renteln et al22 described an high intraoperative complication rate (69% full-thickness dissection in the mediastinum and 57% perforation into the peritoneal cavity). On the other hand some case series of small sample size determined no serious POEM-related complications13,35 and, more recently, Inoue et al34 reported an adverse event rate of 3.2% in a large case series on 500 patients. Even if the total number of adverse events appeared to be higher than what would usually be seen with other treatments, most of these were inherent to POEM and were self-limiting. Majority of the symptomatic adverse events could be managed conservatively and no perioperative mortality or conversion to the other procedure was found in any study. Furthermore the frequency of perforation and bleeding was not high and the results of meta-analysis of overall complications as well as major and minor adverse events did not differ between POEM and LHM, emerging POEM as a safe procedure that was comparable to the safety profile of LHM. Of course, POEM represents a challenging procedure that should be performed only in specialized centers by experts in interventional endoscopy or surgeons with advanced skills in endoscopy, to guarantee the highest outcomes for the patients. POEM operators must be expert in esophageal pathology, particularly as regard the EGJ peculiarities, the submucosal dissection technique and the management of the most frequent complications.36 To this address a learning curve of approximately 20 cases has been proposed to achieve the learning curve plateau in POEM for an experienced endoscopist.37
Nevertheless, gastroesophageal reflux is a common dilemma after a transoral approach for myotomy since no antireflux procedure is involved differently from surgical myotomy. To this address, many authors showed very good outcomes with the application of an antireflux procedure to laparoscopic or laparotomic myotomy, reporting an incidence of pathological gastroesophageal reflux of 5.7% to 10%.38–42 Furthermore, a prospective randomized trial performed by Richards et al43 evidenced pathological GER rate of 47.6% in the group with Heller myotomy without antireflux procedure compared with a 9.1% in the group with Heller myotomy followed by anterior fundoplication, with no statistical significant differences between the 2 groups as regard postoperative dysphagia score. Indeed, last retrospective studies evaluating the long-term outcomes of LHM demonstrated a pathological GER rate of 11.3% to 80%,44–46 while a more recent meta-analysis showed that an antireflux procedure following myotomy is associated with a lower pathologic acid exposure and GER, and that the dysphagia relief is not affected by the type of fundoplication.8,42,43
On the other hand, endoscopic myotomy through the luminal side accounts for an incidence between 0% and 37% of symptomatic GER after POEM during short-term follow-up.13,47–51 Interestingly, Inoue et al34 reported endoscopic findings of reflux esophagitis in 64.7% and GERD symptoms, such as heartburn or regurgitation, in 16.8% of patients at 2 months post-POEM follow-up; at 1 to 2 years after POEM, GERD symptoms were registered in 19.4% of patients and endoscopic evidence of esophagitis was noted in 59.2% of patients. Similarly, at 3 years follow-up, similar results were found, accounting the GERD symptoms for 21.3% of patients and endoscopic evidence of esophagitis for 56.3% of patients. However, in all cases reflux symptoms were completely controlled by proton pump inhibitors therapy.34 Although this large single center cohort study is the first to report 3 years outcomes regarding gastroesophageal reflux, some limitations, such as inclusion of relatively small number of greater curvature POEMs as well as significant long-term missing data rate, make challenging to deduce any solid conclusions about this debated issue.
Overall, our pooled outcomes on postprocedure symptomatic gastroesophageal reflux showed a trend toward significant reduction in favor of LHM compared to POEM group (OR = 1.81, 95% CI: 1.11–2.95, P = 0.017). Nevertheless, future studies are needed to investigate the long-term effects of POEM on acid reflux.
Our study was affected by some limitations. High heterogeneity rate, no randomization of patients and significant publication bias certainly constituted the weak points of the seven included studies. Furthermore all selected studies did not report the results of follow-up longer than 1 year and most of them included patients who were both treatment naive and underwent previous endoscopic or surgical interventions for achalasia.
This meta-analysis points to the urgent need of high quality clinical trials with long-term evaluation comparing POEM with other standard procedures, including surgical myotomy, in a randomized manner.
Footnotes
Abbreviations: ACROBAT-NRSI = A Cochrane risk of bias assessment tool for nonrandomized studies of interventions, CI = confidence interval, EGJ = esophagogastric junction, GER = gastroesophageal reflux, GERD = Gastroesophageal Reflux Disease, GerdQ = Gastroesophageal Reflux Disease Questionnaire, LES = lower esophageal sphincter, LHM = laparoscopic Heller myotomy, MeSH = medical subject headings, OR = odds ratio, POEM = peroral esophageal myotomy, PRISMA = Preferred Reporting Items for Systematic Review and Meta-analysis, SD = standard deviation
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Triadafilopoulos G, Boeckxstaens GE, Gullo R, et al. The Kagoshima consensus on esophageal achalasia. Dis Esophagus 2012; 25:337–348. [DOI] [PubMed] [Google Scholar]
- 2.Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology 2010; 139:369–374. [DOI] [PubMed] [Google Scholar]
- 3.Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut 2001; 49:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patti MG, Diener U, Molena D. Esophageal achalasia: preoperative assessment and postoperative follow-up. J Gastrointest Surg 2001; 5:11–12. [DOI] [PubMed] [Google Scholar]
- 5.Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med 2011; 364:1807–1816. [DOI] [PubMed] [Google Scholar]
- 6.Patti MG, Pellegrini CA. Esophageal achalasia 2011: pneumatic dilatation or laparoscopic myotomy? J Gastrointest Surg 2012; 16:870–873. [DOI] [PubMed] [Google Scholar]
- 7.Kostic S, Kjellin A, Ruth M, et al. Pneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trial. World J Surg 2007; 31:470–478. [DOI] [PubMed] [Google Scholar]
- 8.Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 2009; 249:45–57. [DOI] [PubMed] [Google Scholar]
- 9.Yaghoobi M, Mayrand S, Martel M, et al. Laparoscopic Heller's myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a metaanalysis of randomized, controlled trials. Gastrointest Endosc 2013; 78:468–475. [DOI] [PubMed] [Google Scholar]
- 10.Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42:265–271. [DOI] [PubMed] [Google Scholar]
- 11.Swanstrom LL, Kurian A, Dunst CM, et al. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 2012; 256:659–667. [DOI] [PubMed] [Google Scholar]
- 12.Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia. Surg Endosc 2012; 26:3267–3272. [DOI] [PubMed] [Google Scholar]
- 13.Costamagna G, Marchese M, Familiari P, et al. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis 2012; 44:827–832. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions 5.1.0. 2008; Oxford:Wiley Online Library, www.cochrane-handbook.org [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005; 5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2014; 259:1098–1103. [DOI] [PubMed] [Google Scholar]
- 19.Ujiki MB, Yetasook AK, Zapf M, et al. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surgery 2013; 154:893–897. [DOI] [PubMed] [Google Scholar]
- 20.Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 2013; 17:228–235. [DOI] [PubMed] [Google Scholar]
- 21.Teitelbaum EN, Rajeswaran S, Zhang R, et al. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery 2013; 154:885–891. [DOI] [PubMed] [Google Scholar]
- 22.Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 2013; 145:309.e1-3–311.e1-3. [DOI] [PubMed] [Google Scholar]
- 23.Vigneswaran Y, Yetasook AK, Zhao JC, et al. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 2014; 18:1071–1076. [DOI] [PubMed] [Google Scholar]
- 24.Teitelbaum EN, Soper NJ, Pandolfino JE, et al. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 2015; 29:522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012; 24 (Suppl. 1):57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 2009; 30:1030–1038. [DOI] [PubMed] [Google Scholar]
- 28.Richter JE. Achalasia—an update. J Neurogastroenterol Motil 2010; 16:232–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beck WC, Sharp KW. Achalasia. Surg Clin North Am 2011; 91:1031–1037. [DOI] [PubMed] [Google Scholar]
- 30.Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 2013; 108:1238–1249.quiz 1250. [DOI] [PubMed] [Google Scholar]
- 31.Chuah SK, Hsu PI, Wu KL, et al. 2011 update on esophageal achalasia. World J Gastroenterol 2012; 18:1573–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Katzka DA, Castell DO. Review article: an analysis of the efficacy, perforation rates and methods used in pneumatic dilation for achalasia. Aliment Pharmacol Ther 2011; 34:832–839. [DOI] [PubMed] [Google Scholar]
- 33.Allaix ME, Patti MG. What is the best primary therapy for achalasia: medical or surgical treatment? Who owns achalasia? J Gastrointest Surg 2013; 17:1547–1549. [DOI] [PubMed] [Google Scholar]
- 34.Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 2015; 221:256–264. [DOI] [PubMed] [Google Scholar]
- 35.Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 2001; 11:281–292. [PubMed] [Google Scholar]
- 36.Zhou PH, Li QL, Yao LQ, et al. Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy 2013; 45:161–166. [DOI] [PubMed] [Google Scholar]
- 37.Tantau M, Crisan D. Peroral endoscopic myotomy: time to change our opinion regarding the treatment of achalasia? World J Gastrointest Endosc 2015; 7:237–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kurian AA, Dunst CM, Sharata A, et al. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 2013; 77:719–725. [DOI] [PubMed] [Google Scholar]
- 39.Bonavina L, Nosadini A, Bardini R, et al. Primary treatment of esophageal achalasia. Long-term results of myotomy and Dor fundoplication. Arch Surg 1992; 127:222–226. [DOI] [PubMed] [Google Scholar]
- 40.Ancona E, Peracchia A, Zaninotto G, et al. Heller laparoscopic cardiomyotomy with antireflux anterior fundoplication (Dor) in the treatment of esophageal achalasia. Surg Endosc 1993; 7:459–461. [DOI] [PubMed] [Google Scholar]
- 41.Patti MG, Molena D, Fisichella PM, et al. Laparoscopic Heller myotomy and Dor fundoplication for achalasia: analysis of successes and failures. Arch Surg 2001; 136:870–877. [DOI] [PubMed] [Google Scholar]
- 42.Anselmino M, Zaninotto G, Costantini M, et al. One-year follow-up after laparoscopic Heller-Dor operation for esophageal achalasia. Surg Endosc 1997; 11:3–7. [DOI] [PubMed] [Google Scholar]
- 43.Di Martino N, Brillantino A, Monaco L, et al. Laparoscopic calibrated total vs partial fundoplication following Heller myotomy for oesophageal achalasia. World J Gastroenterol 2011; 17:3431–3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Richards WO, Torquati A, Holzman MD, et al. Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 2004; 240:405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lindenmann J, Maier A, Eherer A, et al. The incidence of gastroesophageal reflux after transthoracic esophagocardio-myotomy without fundoplication: a long term follow-up. Eur J Cardiothorac Surg 2005; 27:357–360. [DOI] [PubMed] [Google Scholar]
- 46.Gupta R, Sample C, Bamehriz F, et al. Long-term outcomes of laparoscopic Heller cardiomyotomy without an anti-reflux procedure. Surg Laparosc Endosc Percutan Tech 2005; 15:129–132. [DOI] [PubMed] [Google Scholar]
- 47.Robert M, Poncet G, Mion F, et al. Results of laparoscopic Heller myotomy without anti-reflux procedure in achalasia. Monocentric prospective study of 106 cases. Surg Endosc 2008; 22:866–874. [DOI] [PubMed] [Google Scholar]
- 48.von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 2012; 107:411–417. [DOI] [PubMed] [Google Scholar]
- 49.Lee BH, Shim KY, Hong SJ, et al. Peroral endoscopic myotomy for treatment of achalasia: initial results of a Korean study. Clin Endosc 2013; 46:161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc 2014; 26:43–51. [DOI] [PubMed] [Google Scholar]
- 51.Sharata A, Kurian AA, Dunst CM, et al. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 2013; 17:1188–1192. [DOI] [PubMed] [Google Scholar]


