Abstract
Pedicle screw constructs have become the mainstay for surgical correction in patients with spinal deformities. To reduce or avoid the risk of pedicle screw-based complications and to decrease the costs associated with pedicle screw instrumentation, some authors have introduced interval, skipped, and key-vertebral pedicle screw strategies for correction. However, there have been no comparisons of outcomes among these 3 pedicle screw-placement strategies.
The aim of this study was to compare the correlative clinical outcomes of posterior correction and fusion with pedicle screw fixation using these 3 surgical strategies.
Fifty-six consecutive patients with Lenke type 1 adolescent idiopathic scoliosis were included in this study. Twenty patients were treated with the interval pedicle screw strategy (IPSS), 20 with the skipped pedicle screw strategy (SPSS), and 16 with the key-vertebral pedicle screw strategy (KVPSS). Coronal and sagittal radiographs were analyzed before surgery, at 1 week after surgery, and at the last follow-up after surgery.
There were no significant differences among the 3 groups regarding preoperative radiographic parameters. No significant difference was found between the IPSS and SPSS groups in correction of the main thoracic curve (70.8% vs 70.0%; P = 0.524). However, there were statistically significant differences between the IPSS and KVPSS groups (70.8% vs 64.9%) and between the SPSS and KVPSS groups (70.0% vs 64.9%) in correction of the main thoracic curve (P < 0.001 for both). Additionally, there were no significant differences among the 3 strategies for sagittal parameters at the immediate postoperative and last postoperative follow-up periods, though there were significant differences in the Cobb angle between the preoperative and immediate postoperative periods among the 3 groups, but not between the immediate postoperative and last follow-up periods. The amount of hospital charges in the SPSS group was significantly higher than those in the IPSS (P < 0.001) and KVPSS groups (P < 0.001). There were also significant differences in operative time between the IPSS and KVPSS groups (P < 0.001) and between the SPSS and KVPSS groups (P < 0.001).
Each of the 3 types of pedicle screw strategies for correction in patients with Lenke type 1 adolescent idiopathic scoliosis are effective, with satisfactory coronal and acceptable sagittal plane results. Although the KVPSS does not provide superior operative correction compared with the IPSS and SPSS, it can achieve a satisfactory clinical outcome and is more cost-effective.
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is a type of complex 3-dimensional structural deformity of the spine characterized by vertebral rotation in the transverse plane, lateral curvature in the frontal plane, and abnormal alignment in the sagittal plane. The goal of surgical treatment in AIS is not only to correct the spinal deformity and maintain long-term spinal stability but also to prevent cardiopulmonary and neurologic decline and to obtain cosmetic improvement. Since the presentation of the Harrington instrumentation system in 1962, the correction techniques used in scoliosis surgery have changed, evolving from Harrington concave distraction to segmental instrumentation, using a variety of procedures, including segmental sublaminar fixation of each vertebra to rods using the Luque system or the rod rotation maneuver and segmental approximation via cantilever maneuvers with C-D instrumentation, in addition to direct vertebral rotation with segmental pedicle screws.1–5
Lenke type 1 AIS is characterized by a structural main thoracic (MT) curve with a compensatory proximal thoracic curve (PT) and thoracolumbar/lumbar (TL/L) curve. In recent decades, pedicle screw constructs have become increasingly popular in the correction of spinal deformity. Several studies have reported that thoracic pedicle screw fixation provides superior coronal and axial curve correction, maintenance of this correction in the 3-dimensional (coronal, sagittal, and axial) planes, and a decreased number of fusion levels compared with hook or hybrid instrumentation.6–9 In addition, pedicle screw fixation in thoracic curves can also decrease the operative time (OT), intraoperative blood loss (IBL), and revision rate.6,7,10,11 Most studies have reported that the use of pedicle screw constructs is safe and reliable for correcting the spinal deformity of idiopathic thoracic scoliosis.4,9,10,12–14 However, several studies have described some potential neurological and vascular complications, intraoperative pedicle fracture, and pseudarthrosis.13,15–17 In addition, the pedicle screw used in the thoracic curves has been reported to induce hypokyphosis,18,19 and the widespread adoption of pedicle screw-based constructs has increased hospital expenses related to AIS.19,20
To reduce or avoid the risk of pedicle screw-based complications and decrease the cost associated with pedicle screw instrumentation, some authors have introduced interval, skipped, and key-vertebral pedicle screw strategies.12,21,22 However, no comparative analyses of interval, skipped, and key-vertebral pedicle screw strategies for correction of spinal deformity have been performed. The purpose of this study was to compare the results of posterior correction and fusion with pedicle screw fixation using these 3 surgical strategies.
METHODS
Setting and Patient Population
From January 2011 to March 2014, 56 consecutive patients with Lenke type 1 AIS were treated using single-stage posterior thoracic curve instrumentation and fusion with pedicle screws. The inclusion criteria were as follows: diagnosis of AIS and age of 12 to 19 years; a major thoracic curve Cobb angle of more than 40 degrees; a minimum of 1-year follow-up; and a flexibility rate of over 50% for the major thoracic curve observed on supine side-bending radiographs. The exclusion criteria were as follows: any previous spine surgery; anterior release; neurological deficit; and posterior osteotomy. The fusion level was selected from the upper instrumentation vertebra (UIV: T4/T5) to the lower instrumentation vertebra (LIV: T12/L1).
The patients were divided into 3 groups according to the type of thoracic pedicle screw instrumentation. In the interval pedicle screw strategy (IPSS) group, pedicle screws were placed at intervals on both the concave and convex sides.12 In the skipped pedicle screw strategy (SPSS) group, each level had fixation on the concave side, with the skipping of levels on the convex side.21 In the key-vertebral pedicle screw strategy (KVPSS) group, 2 levels at the upper and lower ends of the fusion block were fixed bilaterally, and then 1 screw was placed at the apical vertebra on the convex side, whereas 1 screw each was placed on the adjacent upper and lower vertebrae on the concave side.22 The instrumentation system utilized was Expedium (uniaxial pedicle screw, Depuy Synthes) in all 56 cases. All surgical procedures were performed by 1 senior surgeon. The study was approved by the clinical research ethics committee of our hospital.
Radiographic and Clinical Assessments
Preoperative, immediate postoperative (ie, the 1st week), and final follow-up radiographs were obtained on long cassettes by certified radiology technicians in the standardized fashion. Supine side-bending radiographs were performed preoperatively for all patients. The parameters measured on the coronal radiographs were as follows: Cobb angles of the PT, MT, and TL/L curves; coronal balance (CB); and radiographic shoulder height (RSH). CB was defined as the horizontal distance between the center of the S1 vertebra and the vertical line drawn from the center of C7. RSH is the perpendicular distance in the soft tissue shadow directly superior to the acromioclavicular joint. The following 4 sagittal radiographic parameters were measured: thoracic kyphosis (TK); thoracolumbar junction (TLJ); lumbar lordosis (LL); and sagittal vertical axis (SVA). TK is the angle between perpendicular lines drawn from the T5 superior end plate and the T12 inferior end plate. The TLJ is the angle between perpendicular lines drawn from the T10 superior end plate and the L2 inferior end plate. LL is the angle between perpendicular lines drawn from the L1 superior end plate and the L5 inferior end plate. The SVA is the distance between the posterosuperior point of the sacral plate and the plumb line drawn from C7.
The OT, IBL, total transfusion volume (TTV), number of pedicle screws (NPS), and amount of hospital charges (HCs) were noted. The radiographs were analyzed by 2 authors of this study, who independently performed the measurements. An experienced spine surgeon reviewed the medical records and plain radiographs of all patients.
The correction rate and flexibility rate were calculated as follows:
Formula 1
correction rate (%) = (preoperative angle − postoperative angle)/preoperative angle × 100%
Formula 2
flexibility rate (%) = (preoperative standing angle − preoperative bending angle)/preoperative Cobb angle × 100%
CB >2.0 cm was considered to indicate coronal decompensation, CB ≤2.0 cm was considered satisfactory, and CB ≤1.0 cm was considered excellent.
Radiographic shoulder height was graded as significant imbalance (>3 cm), moderate imbalance (2–3 cm), minimal imbalance (1–2 cm), or balanced (<1 cm).
Statistical Analyses
Statistical analyses were performed using SPSS statistical software v. 17.0 (IBM, Chicago, IL). Preoperative and postoperative radiographic parameters were compared using paired t tests within group samples. Single-factor analysis of variance was employed to compare between groups. Statistical significance was defined as P < 0.05.
RESULTS
Patient Demographics
The IPSS group included 20 patients with AIS who completed an average of 19.0 ± 9.1 months follow-up. Eighteen patients (90%) were female, and 2 (10%) were male. The average age at surgery was 14.9 ± 1.7 years. There were 14 patients with a lumbar modifier A, 4 with a lumbar modifier B, and 2 with a lumbar modifier C. Nineteen patients were normokyphotic, and 1 was hypokyphotic in the sagittal plane. The UIV was T4 in 8 patients and T5 in 12 patients. In addition, the LIV was T12 in 8 patients and L1 in 12 patients (Table 1).
TABLE 1.
Demographic, Clinical, and Radiographical Data
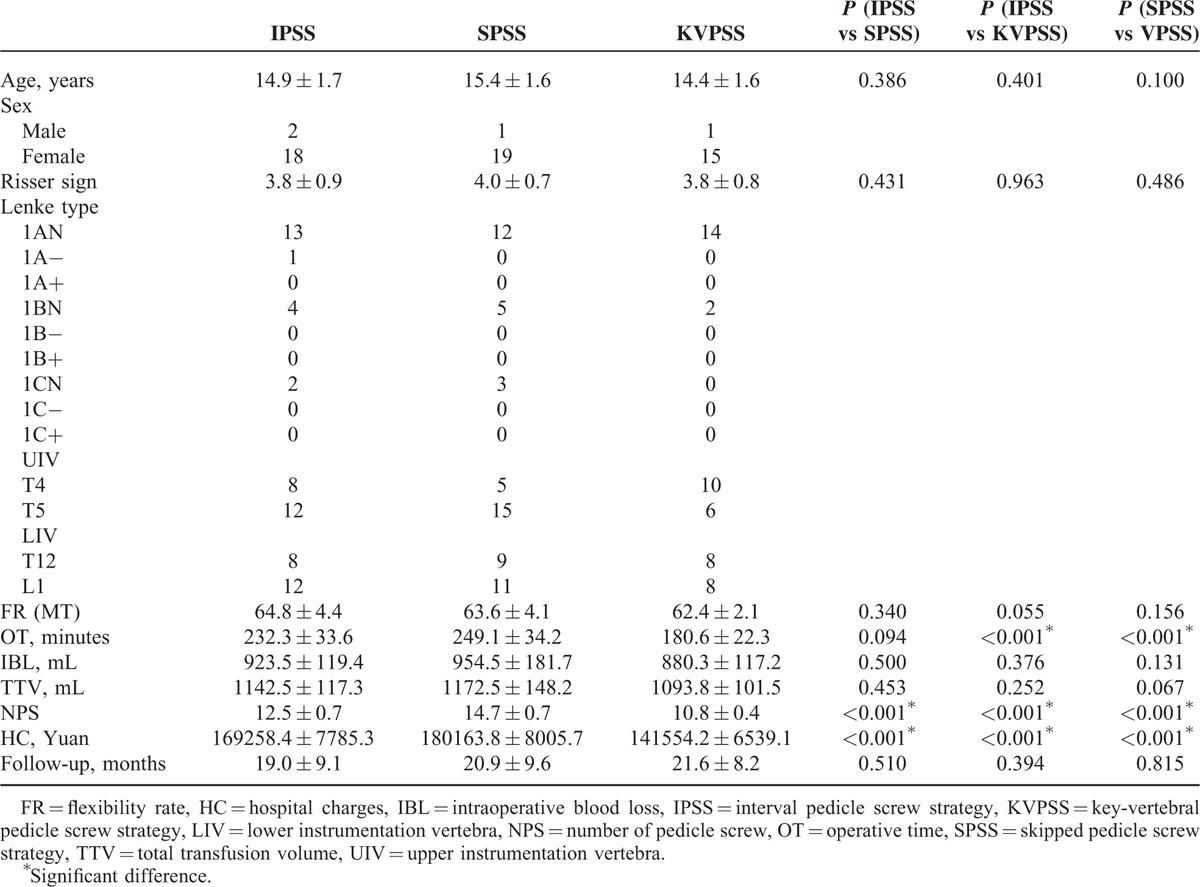
The SPSS group included 20 patients with AIS who completed an average of 20.9 ± 9.6 months follow-up. Nineteen patients (95%) were female 1 one (5%) was male. The average age at surgery was 15.4 ± 1.6 years. There were 12 patients with a lumbar modifier A, 5 with a lumbar modifier B, and 3 with a lumbar modifier C. All patients were normokyphotic. The UIV was T4 in 5 patients and T5 in 15 patients; the LIV was T12 in 9 patients and L1 in 11 patients.
The KVPSS group included 16 patients with AIS who completed an average of 21.6 ± 8.2 months follow-up. Fifteen patients (94%) were female and 1 (6%) was male. The average age at surgery was 14.4 ± 1.6 years. There were 14 patients with a lumbar modifier A, 2 with a lumbar modifier B, and 1 patient with a lumbar modifier C. All patients were normokyphotic. The UIV was T4 in 10 patients and T5 in 6 patients; the LIV was T12 in 8 patients and L1 in 8 patients.
The groups did not significantly differ in terms of age, flexibility rate, IBL, TTV, or follow-up time. The average OT in the KVPSS group was significantly shorter than those in the IPSS (P < 0.001) and SPSS groups (P < 0.001); however, there was no significant difference between the IPSS and SPSS groups (P = 0.094). The NPS and amount of HCs were significantly higher in the SPSS group than in the IPSS (P < 0.001) and KVPSS groups (P < 0.001).
Radiographic Analysis
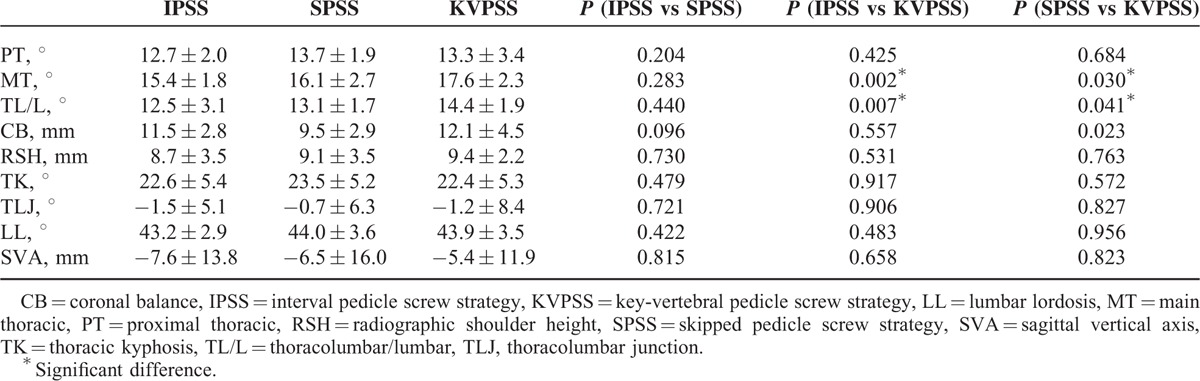
Preoperatively, there were no significant differences among the 3 groups in the Cobb angle of the PT curve, MT curve, or TL/L curve, or the CB, RSH, TK, TLJ, LL, or SVA value. During the immediate postoperative period, there were no significant differences among the 3 groups in the Cobb angle of the PT curve or TL/L curve, or the RSH, TK, TLJ, LL, or SVA value. There were significant differences in both the Cobb angle of the MT curve and CB between the KVPSS and IPSS groups and also between the KVPSS and SPSS groups. At the last follow-up, there were no significant differences among the 3 groups in the Cobb angle of the PT curve, or the CB, RSH, TK, TLJ, LL, or SVA value. There were significant differences in the Cobb angles of both the MT and TL/L curves between the KVPSS and IPSS groups and also between the KVPSS and SPSS groups (Table 2–4,,).
TABLE 2.
Comparing Preoperative Parameters among Three Groups
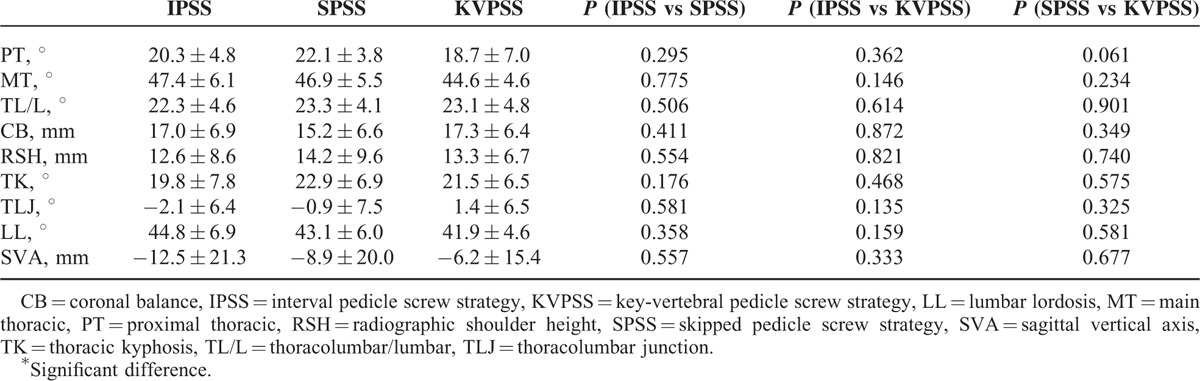
TABLE 3.
Comparing Immediate Postoperative Parameters Among 3 Groups
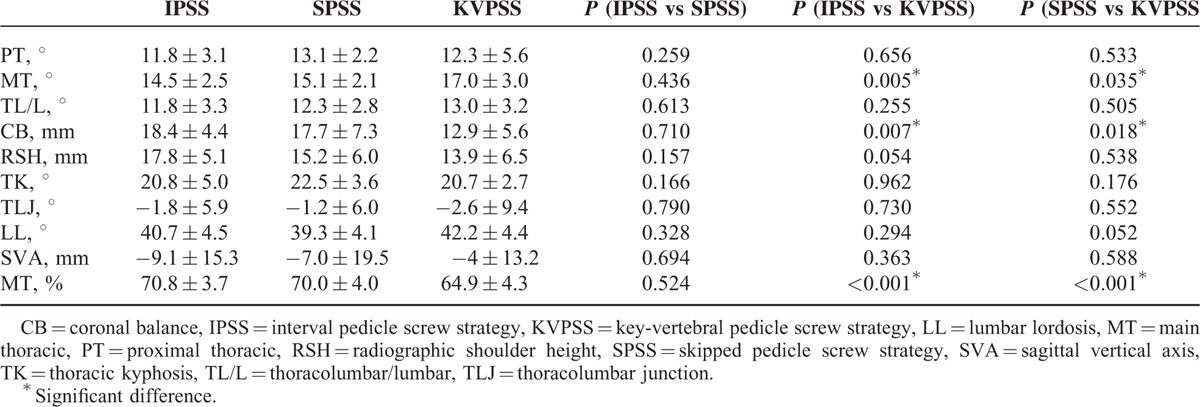
TABLE 4.
Comparing Last Follow-up Postoperative Parameters Among 3 Groups
In the IPSS group, the Cobb angles of the PT, MT, and TL/L curves were significantly different between the preoperative and immediate postoperative periods (P < 0.001, P < 0.001, P < 0.001, respectively), and no significant change was observed between the immediate postoperative and last follow-up postoperative periods (P = 0.125, P = 0.054, P = 0.163). The CB did not significantly differ between the preoperative and immediate postoperative periods (P = 0.49), but it did show a significant change between the immediate postoperative and last postoperative follow-up periods (P < 0.001). The RSH and LL showed significant differences between the preoperative and immediate postoperative periods (P = 0.023 and P = 0.037, respectively), and also between the immediate postoperative and last postoperative follow-up periods (P < 0.001 and P = 0.002, respectively), but no significant difference between the preoperative and final postoperative follow-up periods (P = 0.1 and P = 0.323, respectively). The TK, TLJ, and SVA values were not significantly different among the preoperative, immediate postoperative, and last postoperative follow-up periods (Table 5, Figure 1).
TABLE 5.
Comparing Preoperative, Immediate Postoperative, and Last Follow-up Parameters in IPSS Group
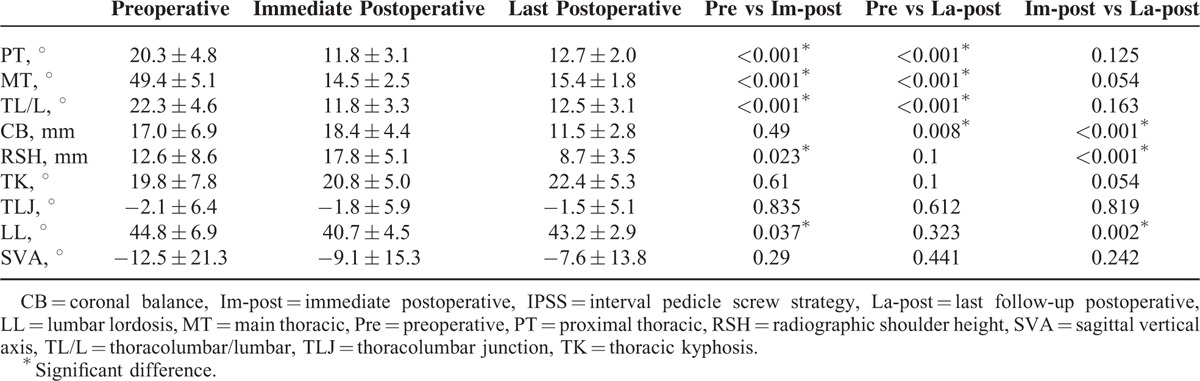
FIGURE 1.
Illustrative example of interval instrumentation. A, Preoperative standing coronal radiograph of a 15-year-old female patient with AIS and a main thoracic (MT) curve of 45° from T5 to T12. The sagittal Cobb angle of thoracic kyphosis (T5 to T12) was 25°. B, Immediate postoperative standing coronal radiograph obtained after application of the interval pedicle screw strategy for correction from T5 to T12 shows a 15° MT curve. The sagittal Cobb angle of thoracic kyphosis was 23°. After 24 months, a follow-up radiograph (C) shows a 16° MT curve and a 25° thoracic kyphosis. AIS = adolescent idiopathic scoliosis.
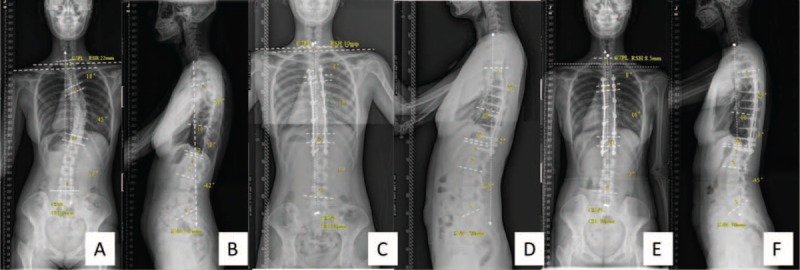
In the SPSS group, the Cobb angles of the PT, MT, and TL/L curves were significantly different between the preoperative and immediate postoperative periods (P < 0.001, P < 0.001, P < 0.001), but not between the immediate postoperative and last postoperative follow-up periods (P = 0.439, P = 0.056, P = 0.237, respectively). The CB and RSH values did not significantly differ between the preoperative and immediate postoperative periods (P = 0.317, P = 0.657, respectively), but they did significantly differ between the immediate and last postoperative follow-up periods (P < 0.001, P < 0.001). The LL showed a significant difference between the preoperative and immediate postoperative periods (P = 0.034) and also between the immediate postoperative and last postoperative follow-up periods (P < 0.001), but not between the preoperative and last postoperative follow-up periods (P = 0.493). The TK, TLJ, and SVA values were not significantly different among the preoperative, immediate postoperative, and last postoperative periods (Table 6, Figure 2).
TABLE 6.
Comparing Preoperative, Immediate Postoperative, and Last Follow-up Parameters in SPSS Group
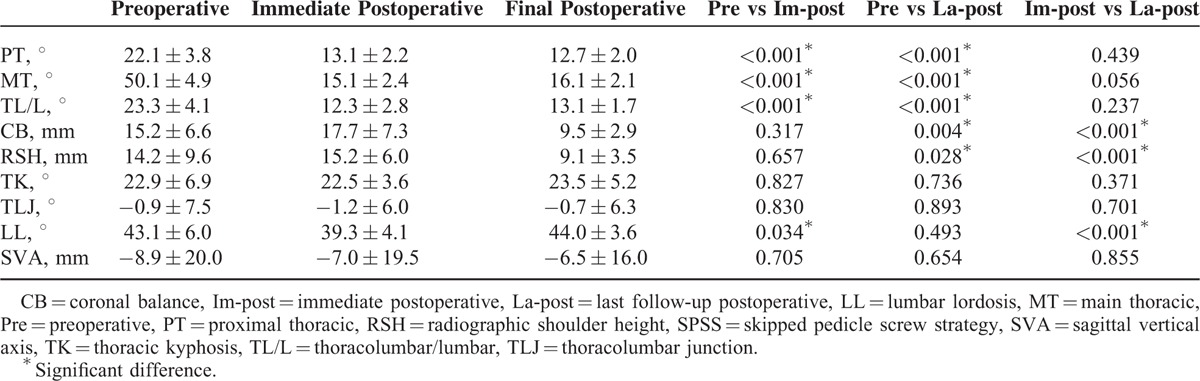
FIGURE 2.
Illustrative example of skipping instrumentation. A, Preoperative standing coronal radiograph of a 14-year-old female patient with AIS and a main thoracic (MT) curve of 50° from T5 to T12. The sagittal Cobb angle of thoracic kyphosis (T5 to T12) was 20°. B, Immediate postoperative standing coronal radiograph obtained after application of the skipped pedicle screw strategy for correction from T5 to T12 shows a 20° (MT) curve. The sagittal Cobb angle of thoracic kyphosis was 12°. After 18 months, a follow-up radiograph (C) shows a 20° MT curve and a 20° thoracic kyphosis.
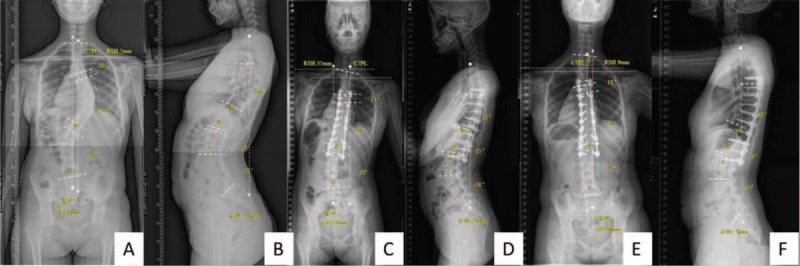
In the KVPSS group, the Cobb angles of the PT, MT, and TL/L curves significantly differed between the preoperative and immediate postoperative periods (P < 0.001, P < 0.001, P < 0.001, respectively), but not between the immediate postoperative and last postoperative follow-up periods (P = 0.213, P = 0.307, P = 0.064, respectively). The CB did not significantly differ between the preoperative and immediate postoperative periods (P = 0.085) or between the immediate and last postoperative follow-up periods (P = 0.705), but it did significantly differ between the preoperative and last postoperative follow-up periods (P = 0.028). The RSH did not significantly differ between the preoperative and immediate postoperative periods (P = 0.801), but it did significantly differ between the immediate and last postoperative follow-up periods (P = 0.006), and also between the preoperative and last postoperative follow-up periods (P = 0.049). The TK, TLJ, LL, and SVA values did not significantly differ among the preoperative, immediate postoperative, and last postoperative periods (Table 7, Figure 3).
TABLE 7.
Comparing Preoperative, Immediate Postoperative, and Last Follow-up Parameters in KVPSS Group
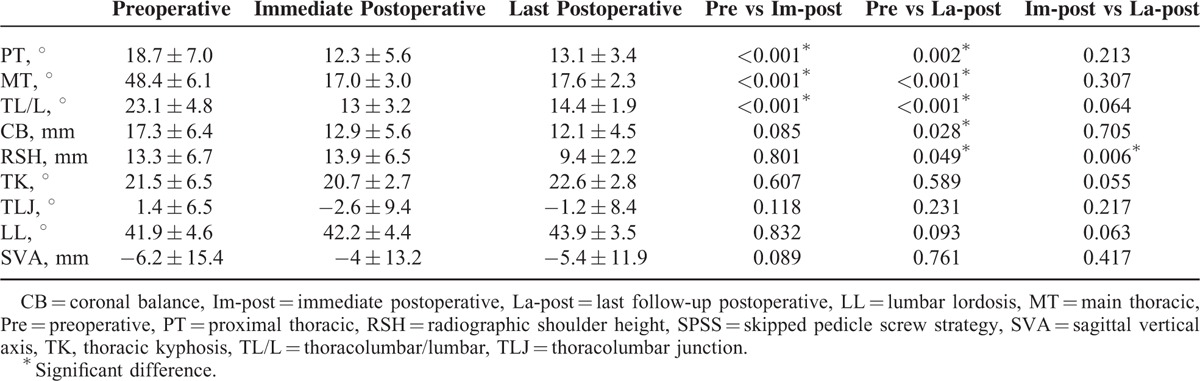
FIGURE 3.
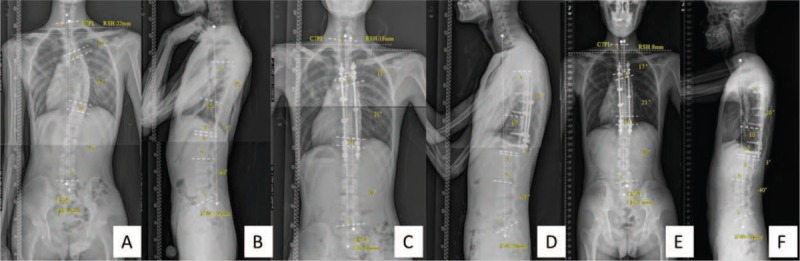
Illustrative example of key-vertebral instrumentation. A, Preoperative standing coronal radiograph of a 17-year-old male patient with AIS and a main thoracic (MT) curve of 42° from T5 to T11. The sagittal Cobb angle of thoracic kyphosis (T5 to T12) was 13°. B, Immediate postoperative standing coronal radiograph obtained after application of the key-vertebral pedicle screw strategy for correction from T5 to T12 shows a 21° (MT) curve. The sagittal Cobb angle of thoracic kyphosis was 15°. After 20 months, a follow-up radiograph (C) shows a 23° MT curve and a 20° thoracic kyphosis.
At 1 week after surgery, 1 patient in the SPSS group experienced wound infection that was resolved by antibiotic therapy and regular dressings. There were no neurologic complications or implant-associated complications among the 3 groups.
DISCUSSION
Over the past 30 years, the use of thoracic pedicle screws for the correction of AIS has become a popular method of fixation. Currently, pedicle screws have been shown to be safe and effective in the posterior correction of AIS. Furthermore, they provide superior spinal deformity correction in the coronal, sagittal, and axial planes compared with hook and hybrid instrumentation and maintain the corrective parameters during follow-up.10,23,24 Many biomechanical studies on cadaveric thoracic vertebrae have demonstrated that pedicle screw fixation provides powerful pullout strength for the spine.25,26 With the development of instrumentation and surgical techniques, surgeons are now able to insert segmental pedicle screws at every possible level. Furthermore, Kuklo et al27 have reported that pedicle screw insertion techniques are not associated with an increased occurrence of major neurologic complications. However, many surgeons have questioned whether it is worthwhile to insert screws into all segments. Therefore, various pedicle screw instrumentation strategies have been suggested as alternatives to the consecutive pedicle screw strategy. It is well known that the most important factor is how many pedicle screw instrumentations can be saved that do not affect spinal correction.
Li et al12 compared the IPSS and consecutive pedicle screw strategy (CPSS) for the correction of Lenke 1 AIS, and found that there was no significant difference between the IPSS and CPSS groups in the correction of the MT (74.7% vs 74.5%) curve. This group also found significant Cobb angle correction in pre versus postoperative radiographic outcomes, with no significant difference between groups. Morr et al21 retrospectively reviewed the use of the SPSS and CPSS for the correction of Lenke 1 curves, with both methods resulting in acceptable correction of the MT curve (66.9% vs 66.6% for the CPSS and SPSS groups, respectively) and spontaneous correction of the PT (41.5% vs 41.1%) and TL/L curves (54.8% vs 54.3%). Both methods also resulted in excellent coronal correction and sagittal balance, with no significant differences in radiographic findings or clinical outcomes. However, we believe that the CPSS of Li et al's study is similar to the SPSS of Morr et al's study. The CPSS of Li et al's study was defined as instrumentation at every level on the concave side of the curve and at 1 to 3 level intervals on the convex side of the curve.12 The SPSS of Morr et al's study was defined as instrumentation at every level on the concave side and the skipping of levels on the convex side.21 However, the CPSS of Morr et al's study was defined as bilateral consecutive pedicle screw instrumentation.21 Therefore, we consider that Li et al's study is essentially a comparison of IPSS and SPSS groups. Our study found that there was no significant difference between the IPSS and SPSS groups in correction of the MT curve (70.8% vs 70.0%, respectively). The correction rate of the MT curve in our study is similar to that of Li et al's study, but is higher than that of Morr et al's study. The correction rate was related to the curve flexibility. The inclusion criteria for curve flexibility (> 50%) in our study were similar to those in Li et al's study for the IPSS and SPSS groups. However, there was no clear cut-off value for preoperative curve flexibility n Morr et al's study.
Li et al22 were the first to introduce the KVPSS method for the treatment of AIS of the MT curve, and his group found that the KVPSS was a safe and cost-effective method for surgical treatment of the MT curve in patients with AIS. The immediate postoperative curve correction rate was 71.2%, and the flexibility rate was 62.2%, as determined using a fulcrum bending radiograph. There was no significant difference in the Cobb angle of the MT curve between the immediate and final postoperative follow-up periods. In our study, the immediate postoperative correction rate of the MT curve was 64.9% in the KVPSS group. The curve flexibility rate was 62.4%, as determined using a supine side-bending radiograph. No significant change was observed in the Cobb angle of the MT between the immediate postoperative and final postoperative follow-up periods. Although both studies used similar pedicle screw strategies, the correction rates of the MT curve differed. This discrepancy occurred due to the following 3 reasons: first, although the 2 flexibility rates were similar, their evaluation methods were not the same. Therefore, the curve flexibilities were actually different. Second, different inclusion criteria were used between the 2 studies. Third, both the pedicle screws and surgical techniques were different, which could also have led to the differences in the outcomes between the 2 studies. To enhance the stability of pedicle screw fixation, we added 1 level bilaterally at the upper and lower ends of the fusion block. The improvement of the correction rate alone cannot be used to evaluate the efficacy of the operation. The optimal operative goals of surgery in AIS are not only to obtain maximum correction of the curves but also to achieve a well-balanced spine. Among the 3 groups assessed in our study, no significant difference was found in the correction rate of the MT curve between the IPSS and SPSS groups. However, significant differences were observed between the IPSS and KVPSS groups and between the SPSS and KVPSS groups. Based on the similar Cobb angles and preoperative flexibilities of the MT curve, we believe that the IPSS and SPSS groups might achieve superior corrective outcomes compared with the KVPSS group. We found that all 3 construct types provided excellent coronal and sagittal balance postoperatively. However, there were significant differences in the NPS and HC among the 3 groups. The KVPSS was associated with the fewest pedicle screws and lowest cost for correction in patients with Lenke type 1 AIS. This finding is very important for developing countries, in which many patients with AIS lack medical insurance. We believe that the KVPSS not only achieves satisfactory correction but also saves operating expenses.
Several scholars have found that high-density thoracic pedicle screw constructs do not improve coronal and sagittal curve correction compared with low-density screw fixation.28,29 Clements et al30 have demonstrated a significant correlation between implant density and structural coronal curve correction. Chen et al31 have reported that implant density is positively correlated with TL/L coronal curve correction and that it is not related to sagittal correction. However, Yang et al32 have determined that increasing implant density only mildly improves the correction of the MT curve and that it does not affect the sagittal profile. In our study, we found that the KVPSS group had a lower pedicle screw density than the IPSS and SPSS groups. The correction rate of the MT curve in the KVPSS group (64.9%) was smaller than those in the IPSS (70.8%) and SPSS (70.0%) groups. However, there were no significant differences in the sagittal parameters among the 3 groups during the immediate postoperative period. We believe that these effects might influence the correction of the coronal curve by the KVPSS, but not the sagittal curve. However, further verification is necessary using biomechanics.
There are some potential limitations to this study. First, this was a retrospective study, and the patients were not randomized to the 3 types of pedicle screw fixation for their surgical procedures. Second, the number of included patients was relatively small, particularly in the KVPSS group. Third, we did not assess the degree of apical derotation. Fourth, the follow-up periods were relatively short, and a study with a longer follow-up duration is required for more optimal observations. However, the major strength of this study is that its pedicle screws were the only method of fixation in every case, and all surgical procedures were performed by 1 senior surgeon. Nonetheless, a larger, longer follow-up study is needed to validate our findings.
CONCLUSIONS
The three pedicle screw strategies for the correction of spinal deformities in patients with Lenke type 1 AIS are effective, achieving satisfactory coronal and acceptable sagittal plane results. Although the KVPSS does not provide superior operative correction compared with the IPSS and SPSS, it can achieve a satisfactory clinical outcome and is more cost-effective.
Footnotes
Abbreviations: AISa = dolescent idiopathic scoliosis, CB = coronal balance, HCs = hospital charges, IBL = intraoperative blood loss, IPSS = interval pedicle screw strategy, KVPSS = key-vertebral pedicle screw strategy, LIV = lower instrumentation vertebra, LL = lumbar lordosis, MT = main thoracic curve, NPS = number of pedicle screws, OT = operative time, PT = proximal thoracic curve, RSH = radiographic shoulder height, SPSS = skipped pedicle screw strategy, SVA = sagittal vertical axis, TK = thoracic kyphosis, TL/L = thoracolumbar/lumbar, TLJ = thoracolumbar junction, TTV = total transfusion volume, UIV = upper instrumentation vertebra
FW, XMX and YHL contributed equally to this study.
Disclaimer: The authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
The authors report no conflicts of interest.
REFERENCES
- 1.Harrington PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. June 1962. J Bone Joint Surg Am 2002; 84:316.-A. [PubMed] [Google Scholar]
- 2.Luque ER. The anatomic basis and development of segmental spinal instrumentation. Spine (Phila Pa 1976) 1982; 7:256–259. [DOI] [PubMed] [Google Scholar]
- 3.Cotrel Y, Dubousset J. A new technic for segmental spinal osteosynthesis using the posterior approach. Orthop Traumatol Surg Res 2014; 100:37–41. [DOI] [PubMed] [Google Scholar]
- 4.Suk SI, Lee CK, Kim WJ, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1995; 20:1399–1405. [PubMed] [Google Scholar]
- 5.Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004; 29:343–349. [DOI] [PubMed] [Google Scholar]
- 6.Liljenqvist U, Lepsien U, Hackenberg L, et al. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J 2002; 11:336–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2006; 31:291–298. [DOI] [PubMed] [Google Scholar]
- 8.Yilmaz G, Borkhuu B, Dhawale AA, et al. Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop 2012; 32:490–499. [DOI] [PubMed] [Google Scholar]
- 9.Crawford AH, Lykissas MG, Gao X, et al. All-pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery: a comparative radiographical study with a minimum 2-year follow-up. Spine (Phila Pa 1976) 2013; 38:1199–1208. [DOI] [PubMed] [Google Scholar]
- 10.Di Silvestre M, Bakaloudis G, Lolli F, et al. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Eur Spine J 2008; 17:1336–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuklo TR, Potter BK, Lenke LG, et al. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2007; 32:2258–2264. [DOI] [PubMed] [Google Scholar]
- 12.Li M, Shen Y, Fang X, et al. Coronal and sagittal plane correction in patients with Lenke 1 adolescent idiopathic scoliosis: a comparison of consecutive versus interval pedicle screw placement. J Spinal Disord Tech 2009; 22:251–256. [DOI] [PubMed] [Google Scholar]
- 13.Lehman RA, Jr, Lenke LG, Keeler KA, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976) 2008; 33:1598–1604. [DOI] [PubMed] [Google Scholar]
- 14.Fujimori T, Yaszay B, Bartley CE, et al. Safety of pedicle screws and spinal instrumentation for pediatric patients: comparative analysis between 0- and 5-year-old, 5- and 10-year-old, and 10- and 15-year-old patients. Spine (Phila Pa 1976) 2014; 39:541–549. [DOI] [PubMed] [Google Scholar]
- 15.Suk SI, Kim WJ, Lee SM, et al. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine (Phila Pa 1976) 2001; 26:2049–2057. [DOI] [PubMed] [Google Scholar]
- 16.Sarwahi V, Suggs W, Wollowick AL, et al. Pedicle screws adjacent to the great vessels or viscera: a study of 2132 pedicle screws in pediatric spine deformity. J Spinal Disord Tech 2014; 27:64–69. [DOI] [PubMed] [Google Scholar]
- 17.Hicks JM, Singla A, Shen FH, et al. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 2010; 35:E465–E470. [DOI] [PubMed] [Google Scholar]
- 18.Hwang SW, Samdani AF, Gressot LV, et al. Effect of direct vertebral body derotation on the sagittal profile in adolescent idiopathic scoliosis. Eur Spine J 2012; 21:31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCormick J, Aebi M, Toby D, et al. Pedicle screw instrumentation and spinal deformities: have we gone too far? Eur Spine J 2013; 22 (Suppl 2):S216–S224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin CT, Pugely AJ, Gao Y, et al. Increasing hospital charges for adolescent idiopathic scoliosis in the United States. Spine (Phila Pa 1976) 2014; 39:1676–1682. [DOI] [PubMed] [Google Scholar]
- 21.Morr S, Carrer A, Alvarez-García de Quesada LI, et al. Skipped versus consecutive pedicle screw constructs for correction of Lenke 1 curves. Eur Spine J 2015. [DOI] [PubMed] [Google Scholar]
- 22.Li J, Cheung KM, Samartzis D, et al. Key-vertebral screws strategy for main thoracic curve correction in patients with adolescent idiopathic scoliosis. J Spinal Disord Tech 2014; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1997; 22:1369–1379. [DOI] [PubMed] [Google Scholar]
- 24.Cheng I, Kim Y, Gupta MC, et al. Apical sublaminar wires versus pedicle screws: which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 2005; 30:2104–2112. [DOI] [PubMed] [Google Scholar]
- 25.Lehman RA, Jr, Kuklo TR. Use of the anatomic trajectory for thoracic pedicle screw salvage after failure/violation using the straight-forward technique: a biomechanical analysis. Spine (Phila Pa 1976) 2003; 28:2072–2077. [DOI] [PubMed] [Google Scholar]
- 26.Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br 2010; 92:1061–1065. [DOI] [PubMed] [Google Scholar]
- 27.Kuklo TR, Lenke LG, O’Brien MF, et al. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine (Phila Pa 1976) 2005; 30:222–226. [DOI] [PubMed] [Google Scholar]
- 28.Bharucha NJ, Lonner BS, Auerbach JD, et al. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome? Spine J 2013; 13:375–381. [DOI] [PubMed] [Google Scholar]
- 29.Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine (Phila Pa 1976) 2010; 35:562–567. [DOI] [PubMed] [Google Scholar]
- 30.Clements DH, Betz RR, Newton PO, et al. Correlation of scoliosis curve correction with the number and type of fixation anchors. Spine (Phila Pa 1976) 2009; 34:2147–2150. [DOI] [PubMed] [Google Scholar]
- 31.Chen J, Yang C, Ran B, et al. Correction of Lenke 5 adolescent idiopathic scoliosis using pedicle screw instrumentation: does implant density influence the correction? Spine (Phila Pa 1976) 2013; 38:E946–E951. [DOI] [PubMed] [Google Scholar]
- 32.Yang S, Jones-Quaidoo SM, Eager M, et al. Right adolescent idiopathic thoracic curve (Lenke 1 A and B): does cost of instrumentation and implant density improve radiographic and cosmetic parameters? Eur Spine J 2011; 20:1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]


