Abstract
As chronic illnesses and chronic pain are related to erectile dysfunction (ED), migraine as a prevalent chronic disorder affecting lots of people all over the world may negatively affect quality of life as well as sexual function. However, a large-scale population-based study of erectile dysfunction and other different comorbidities in patients with migraine is quite limited. This cohort longitudinal study aimed to estimate the association between migraine and ED using a nationwide population-based database in Taiwan.
The data used for this cohort study were retrieved from the Longitudinal Health Insurance Database 2000 in Taiwan. We identified 5015 patients with migraine and frequency matched 20,060 controls without migraine from 2000 to 2011. The occurrence of ED was followed up until the end of 2011. We used Cox proportional hazard regression models to analyze the risks of ED.
The overall incidence of ED was 1.78-fold greater in the migraine cohort than in the comparison cohort (23.3 vs 10.5 per 10,000 person-years; 95% confidence interval [CI] = 1.31–2.41). Furthermore, patients with migraine were 1.75-fold more likely to develop organic ED (95% CI = 1.27–2.41) than were the comparison cohort. The migraine patients with anxiety had a 3.6-fold higher HR of having been diagnosed with ED than the comparison cohort without anxiety (95% CI, 2.10–6.18).
The results support that patients with migraine have a higher incidence of being diagnosed with ED, particularly in the patient with the comorbidity of anxiety.
INTRODUCTION
Because chronic pain and disease are associated with sexual dysfunction, migraine is a common chronic disease involving many people in the world and related to different psychological problems and poor quality of life such as sexual function.1–3
The influences of the chronic disease on sexual function are several causes and impacts on different sexual processes.4 It is necessary to integrate normal neurological, psychological, and vascular responses for normal sexual function. Different sexual processes and responses could be changed due to chronic illness by disturbance of the integrity of hormonal, vascular, and neural for the genitalia, as well as the influences of different medications. Many neuropsychiatric disorders are strongly related to a lot of chronic or systemic diseases may induce sexual dysfunction.5–7 From another point of view, the impaired sexual function could also induce many social problems and poor life quality for the patient and his wife.8,9
There were some analyses to evaluate the association between migraine with sexual dysfunction. Bestepe et al reported the patients with migraine had significantly sexual dysfunction.10 Ifergane et al found that these students with migraine had higher frequent sexual intercourses but lower sexual pleasures.11 There findings were related to the other study that women with migraine treatments shown higher frequency of sexual dysfunction.12
According to the evidences from the above studies, we thought that patients with migraine are related to a higher risk of erectile dysfunction. However, a population-based study about the risk of sexual dysfunction for migraine patients is still limited. Therefore, we designed the population-based cohort study in order to (1) identify the comorbidity of migraine, (2) analyze the psychosocial impact, risk factors, and comorbidity of sexual dysfunction, and (3) verify the association between migraine with subsequent sexual dysfunction.
MATERIALS AND METHODS
Data Source
Present study conducted a nationwide cohort study from Taiwan's National Health Insurance Research Database (NHIRD). The NHIRD is a large computerized database that contains information of all insured persons including detailed health services such as medications, examinations, and operations, as well as background conditions and diagnoses. NHIRD was set up in March 1, 1995, by the Bureau of National Health Insurance (NHI) and maintains by the National Health Research Institute (NHRI) of Taiwan (http://www.nhi.gov.tw/english/index.aspx). We used Longitudinal Health Insurance Database 2000 (LHID 2000) which is a part of NHIRD for this study. LHID 2000 included all medical claims from 1996 to 2011 of 1 million beneficiaries who were randomly selected from the entire 23.74 million beneficiaries of NHI. Disease definition was based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) in NHIRD. According to personal Information Protection Act, identification of beneficiary was recoding by a computer. This study was approved by the Institutional Review Board at China Medical University and Hospital, Taiwan (CMUH104-REC2-115).
Sampled Participants
Figure 1 shows the process of selecting participants for study cohorts. We identified patients aged 20 years with diagnosed migraine (ICD-9 codes 364) from 2000 to 2011 as the migraine cohort. The date of migraine diagnosis served as the index date. We excluded patients with a baseline history of organic and psychogenic ED (ICD-9 codes 302.72 and 607.84) before the data of migraine diagnosis and those missing information on age and sex. Patients without a history of migraine and/or organic and psychogenic ED were randomly chosen to form the comparison cohort from LHID 2000. The comparison cohort was frequency-matched on age (every 5-year span), sex, and the index year of migraine diagnosis using inclusion criteria similar to the migraine cohort. The control-to-case ratio was set at 4:1 to enhance the power of statistical tests.
FIGURE 1.
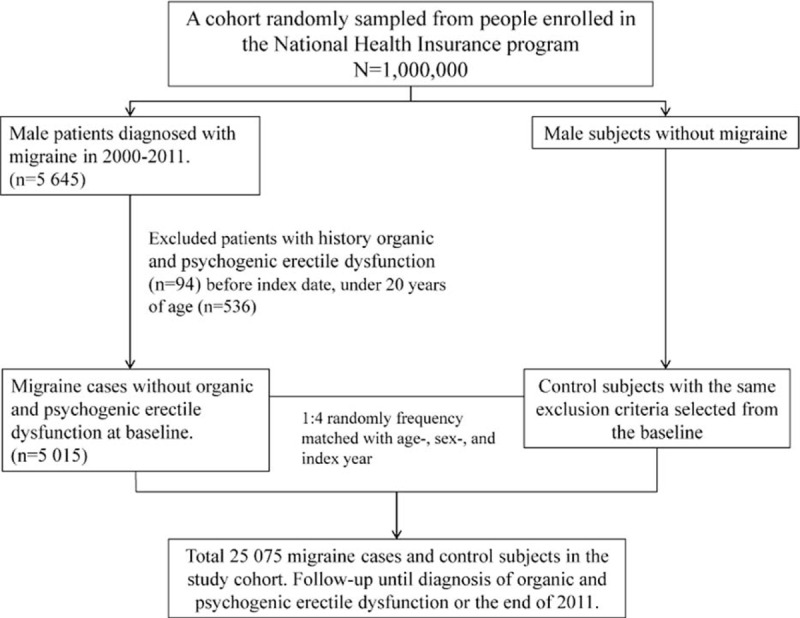
The process of selecting participants for study cohorts.
Outcome and Comorbidity
The follow-up person-years were measured for every participant until diagnosed organic or psychogenic ED, the participant withdrew from the insurance, or until the end in 2011. In this study, the considered baseline comorbidity include depression (ICD-9-CM: 296.2, 296.3, 300.4, 311), anxiety (ICD-9-CM: 300.00), hypertension (ICD-9-CM: 401 to 405), diabetes (ICD-9-CM: 250), hyperlipidemia (ICD-9-CM: 272), coronary artery disease (CAD) (ICD-9-CM: 410–414), chronic obstructive pulmonary disease (COPD) (ICD-9-CM 490–496), and chronic kidney disease (CKD) (ICD-9-CM: 580–589).
Statistical Analysis
We used the χ− test to determine the differences in the distribution of age and baseline comorbidities between the migraine cohort and comparison cohort. We used the t test to test the differences of mean age and mean follow-up time (years) between both cohorts. We calculated the incidences of organic and psychogenic erectile dysfunction in migraine and comparison cohorts based on demographic status and comorbidity. The Kaplan–Meier method depicted the curves of cumulative incidence rate for the 2 cohorts and the log-rank test examined the difference between the curves. We calculated the overall, age-specific, and comorbidity-specific incidence density rates of organic and psychogenic ED with person-years in each cohort. The migraine to comparison cohort relative hazard ratios (HRs) and the 95% confidence interval (CI) were estimated using univariable and multivariable Cox proportional hazards regression models. The multivariable model controlled the age, and comorbidity of CAD, COPD, CKD, hypertension, diabetes, hyperlipidemia, depression, and anxiety with a significant difference in univariable Cox proportion hazards regression. This study used the SAS statistical package, Version 9.3 (SAS Institute Inc, Cary, NC), with P = 0.05 set as the level of significance, and performed 2-tailed tests for all analyses.
RESULTS
We established a migraine cohort of 5015 patients with migraine and a comparison cohort of 20,060 people without migraine. The migraine and comparison cohorts had similar distributions of age and, with approximately mean age of 48 years (Table 1).
TABLE 1.
Demographic Characteristics and Comorbidity in Cohorts With and Without Migraine
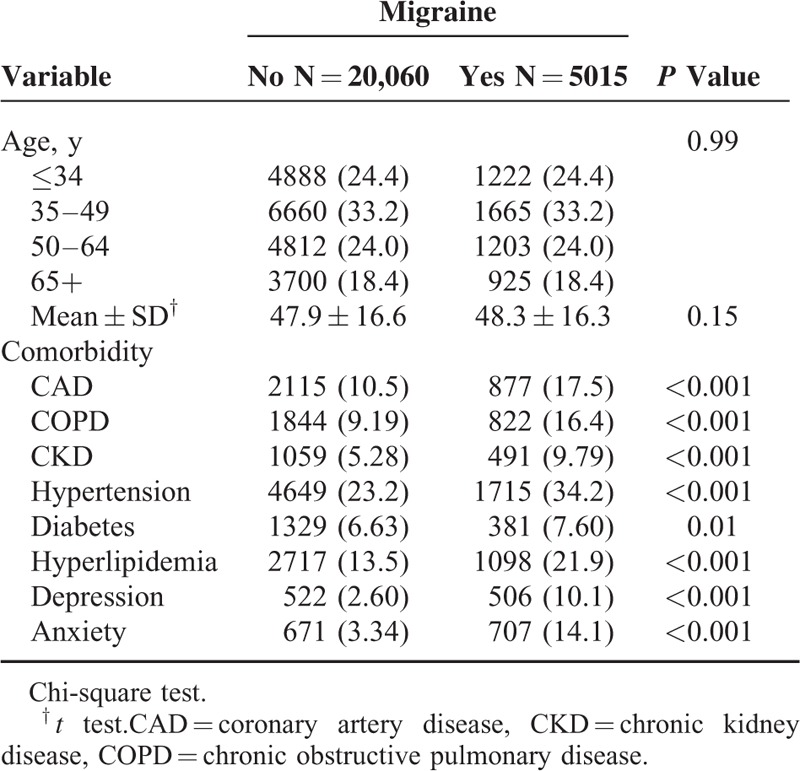
The migraine cohort exhibited higher prevalence than the comparison cohort in terms of CAD, COPD, CKD, hypertension, diabetes, hyperlipidemia, depression, and anxiety. The mean follow-up time in the migraine and comparison cohorts was 6.25 ± 3.42 years and 6.12 ± 3.43 years, respectively (data not shown). Figure 2 shows that the cumulative incidence of organic and psychogenic erectile dysfunction was higher in the migraine cohort than that in the comparison cohort by 1.04% (log-rank test P < 0.001) at the end of follow-up.
FIGURE 2.
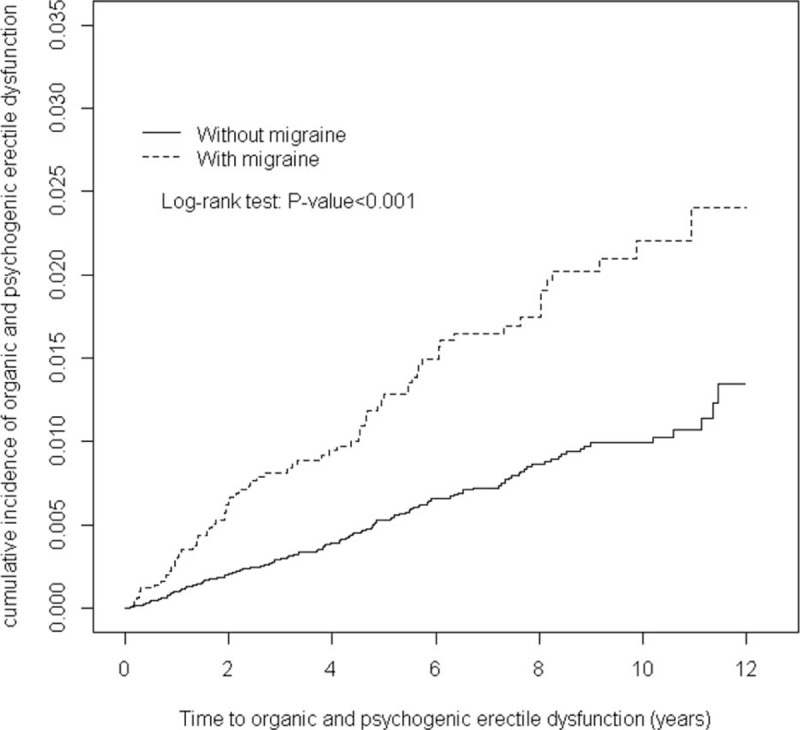
Cumulative incidence comparison of organic and psychogenic erectile dysfunction for patients with (dashed line) or without (solid line) migraine disease.
The incidence and hazards ratios (HRs) between the migraine and comparison cohorts are shown in Table 2. The crude HR of organic and psychogenic ED in the migraine cohort was 2.22 times greater than that in the comparison cohort (23.3 vs 10.5 per 10,000 person-years), with an adjusted HR of 1.78 (95% CI = 1.31–2.41).
TABLE 2.
Incidence of Organic and Psychogenic Erectile Dysfunction by Comorbidity and Cox Model Measured Hazards Ratio for Patients With Migraine Compared Those Without Migraine
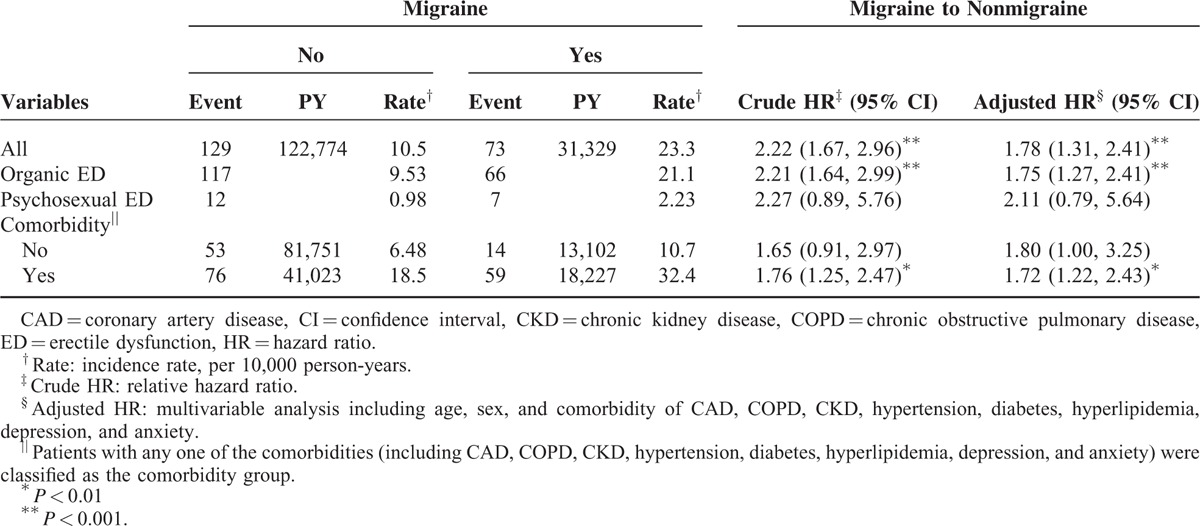
Furthermore, patients with migraine were 1.75-fold more likely to develop organic ED (95% CI = 1.27–2.41) than were the comparison cohort after adjusting for age and comorbidity. The overall incidence density of psychosexual ED was not significantly higher in the migraine patients than in the comparisons (2.23 vs 0.98 per 10,000 person-years), with an HR of 2.11 (95% CI: 0.79–5.64). The age-specific migraine subjects to compared subjects adjusted HR of organic and psychogenic ED was the highest for those 50 to 64 years of age (adjusted HR = 2.16, 95% CI = 1.32–3.54). The organic and psychogenic erectile ED increased with comorbidity in both cohorts.
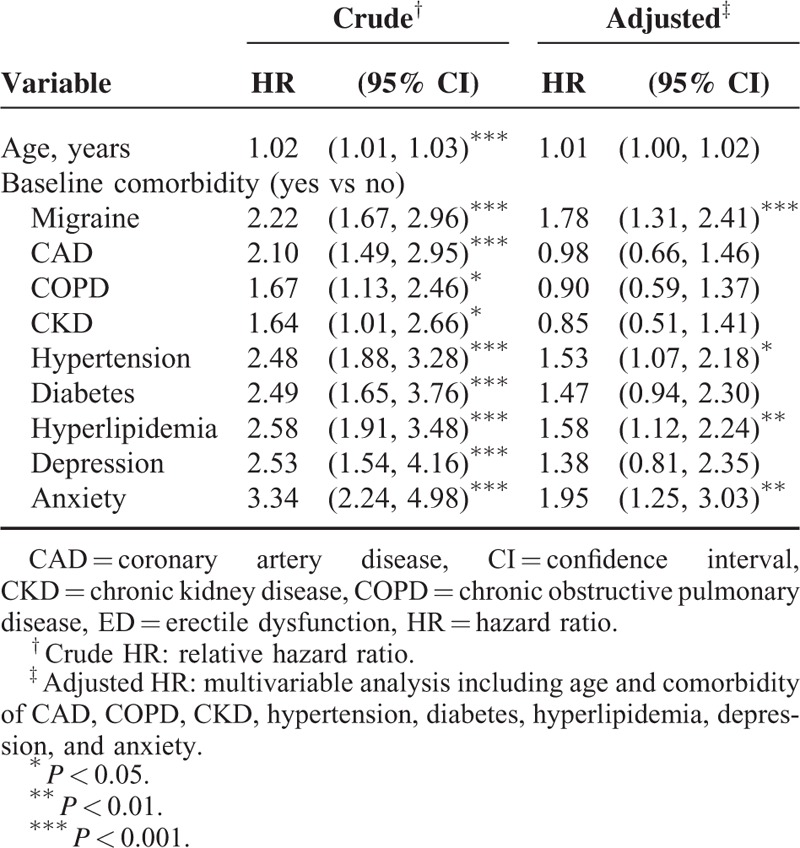
Table 3 shows migraine and other risk factors for organic and psychogenic ED. The multivariable Cox proportional hazards regression model found an increased risk of organic and psychogenic ED in migraine patients with one of the following characteristics: hypertension (adjusted HR = 1.53, 95% CI = 1.07–2.18), hyperlipidemia (adjusted HR = 1.58, 95% CI = 1.12–2.24), and anxiety (adjusted HR = 1.95, 95% CI = 1.25–3.03).
TABLE 3.
Hazard Ratios of Erectile Dysfunction in Association With Age and Comorbidities in Univariable and Multivariable Cox Regression Models
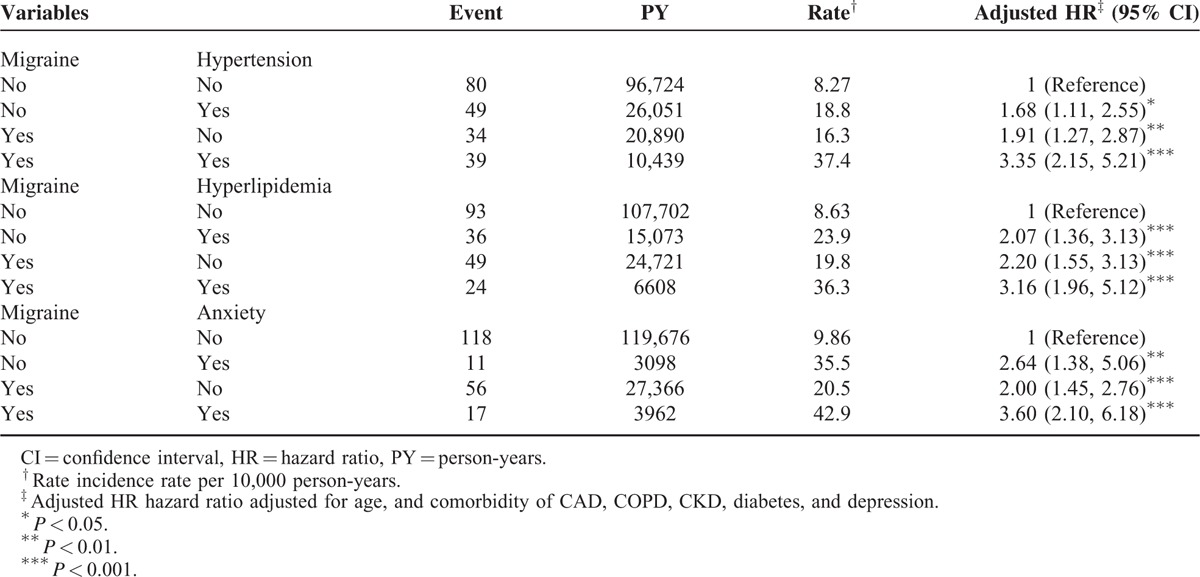
Furthermore, relative to the comparison cohort without anxiety, the migraine patients with anxiety were at a much higher risk of organic and psychogenic ED (adjusted HR = 3.60, 95% CI = 2.10–6.18) (Table 4). A significant higher risk of organic and psychogenic ED was observed for patients with both migraine and hypertension (adjusted HR = 3.35, 95% CI = 2.15–5.21) or both with migraine and hyperlipidemia (adjusted HR = 3.16, 95% CI = 1.96–5.12) than those without migraine, hypertension, and hyperlipidemia.
TABLE 4.
Cox Proportional Hazard Regression Analysis for the Risk of Erectile Dysfunction-Associated Migraine With Joint Effect of Comorbidity
DISCUSSION
To the best of our knowledge, there are only a few studies documenting the relationship between migraine and diagnosis of sexual dysfunction. As sexual dysfunction is an important health problem that increases in diagnostic rate nowadays, it negatively affects patients’ and their partners’ social lives and mental health. Thus, we emphasize on identifying the correlation between migraine and subsequent sexual dysfunction in this study.
The population-based longitudinal design and generalizability of findings is the strengths in this study. We used population-based data from NHIRD includes a big sample number and a low loss follow-up for study and control cohorts. Besides, NHIRD can accurately represent the sample for the general population in Taiwan because of the insurance system is only one and operated by the Taiwan government. All claims in the insurance system should be strictly surveyed by peer review of the medical specialists based on the standard clinical diagnosed criteria. The doctors or hospitals would be punished to pay a lot of penalties, if they make wrong diagnoses or coding to against these regulations. So, we have to believe the diagnoses of ED by ICD-9 codes are highly reliable in our study. Besides, a lot of papers related to ED used the same diagnosed criteria based on ICD-9 coding were published.13–16
We evaluated the migraine patient and the risk for sexual dysfunction in the Taiwanese cohort longitudinal study and enrolled 5015 patients diagnosed of migraine investigated for erectile dysfunction from the Taiwan LHID2000. Accordingly, the enrollment is from the nationwide database, which can enhance the statistical power to detect subtle differences and have fundamental data exploring the relationship between ED and the comorbidity among patients with migraine.
With accurate diagnosis of erectile dysfunction, there are increased possibilities of improvement or cure of the condition. Organic erectile dysfunction should be investigated and diagnosed first such as vascular, neurological, other urological, and endocrine causes which should be dealt initially and the diagnosis of purely psychogenic dysfunction should be the one of exclusion. We can take psychogenic erectile dysfunction into the definition as the persistent inability to achieve or maintain erection satisfactory for sexual performance owing predominantly or exclusively to psychologic or interpersonal factors. This definition recently was adopted by the International Society of Impotence Research and acknowledges 3 key components: (1) psychogenic erectile dysfunction is a positive diagnosis that should not be used when the etiology of the disorder is uncertain or unknown; (2) psychosocial factors should be identified as the predominant or exclusive cause of the patient's dysfunction, and patients with a combination of organic and psychogenic factors should be diagnosed as having mixed organic-psychogenic erectile dysfunction; and (3) other components of the definition are consistent with recent consensus definitions of erectile dysfunction.17–19
From this matched cohort study, the patient with migraine had ∼1.78 times the hazard of erectile dysfunction as compared to nonmigraine patients. These findings were robust with adjustment for multiple potential confounders and consistent using multiple strategies to address confounding by health status. This result was consistent with the study by Huang et al in 2012 estimate the association between ED and migraines.20 Also, the study of Sicuteri et al revealed sexual dysfunction was found more often in patients with migraine.21 As, neurogenic, organic, vascular, and endocrinologic etiologies can result in sexual dysfunction,22 we separated sexual dysfunction into 2 categories. After adjusting for sociodemographic characteristics and medical comorbidity, including CAD, COPD, chronic renal disease, hypertension, hyperlipidemia, depression and anxiety, patients with migraine compared with control group had statistically higher rate of organic erectile dysfunction (ED), but not with psychogenic ED. Nonetheless, migraine group had a trend to have more psychogenic erectile dysfunction.
Some possible mechanisms are related to sexual dysfunction by systemic or chronic diseases. Therefore, systemic or chronic diseases should the important comorbidity that could influence the vascular or neuron structures for sexual function. The related comorbidity found in Taiwan were very similar to these findings in Western countries,23 including cardiovascular diseases and endocrine system disorders. We found the increased incidences of organic and psychogenic erectile dysfunction with comorbidity in both cohorts. Among those comorbidities, the HRs for sexual dysfunction were 2.1, 2.48, 2.49, 2.58, 2.53, and 3.34 in CAD, hypertension, diabetes, hyperlipidemia, depression, and anxiety, respectively. All comorbidity factors were related with greater hazard of ED in the univariable Cox regression models. In the model simultaneously considering all comorbidity, subjects with anxiety showed approximately twice the risk of ED (adjusted HR = 1.95, 95% CI = 1.25–3.03); adjusted HR were 1.58 and 1.53, respectively, for hyperlipidemia (95% CI = 1.12–2.24), and hypertension (95% CI = 1.07–2.18). In the multivariable model simultaneously considering all comorbidity, subjects with depression was not significantly higher the risk of ED. Another reason, in the previous study, they did not consider the effect of migraine, maybe an important risk factor for ED.
The association between CAD and ED is possibly attributed to endothelial dysfunction and increased circulating levels of inflammatory markers which impaired the release of nitric oxide (NO).24,25 Common risk factors for atherosclerosis are considered 1 mechanism in the association between ED and CVD. Montorsi et al proposed that atherosclerosis affects all vascular beds equally, including penile and coronary arteries.26
Previous researches associate diabetes mellitus with the contribution of distressing complications to ED.27 The pathophysiologic changes behind ED associated with diabetes can broadly be classified as (1) vasculopathy, (2) peripheral and autonomic neuropathy, and (3) hypogonadism. All of which can affect the relaxation of the smooth muscle of the corpus cavernosum.27 The association between hyperlipidemia and ED can be postulated that hypercholesterolemia may be responsible for the impairment of endothelium-dependent relaxation of the corpus cavernosum.28
In our study, the other highly prevalent comorbidity includes depression and anxiety which are related to ED. There are many life pressures related to anxiety and induce secondary ED.29 Although we cannot exclude the possibility that depression and anxiety are consequences of ED, our findings are consistent with previous studies.30 Bonierbale et al studied 4557 patients with major depression to find that the prevalence of erectile dysfunction was 35% by spontaneous problems’ reports of these patients and 69% by identification of the physicians’ survey.
The relationship may be from the endothelial dysfunction which is common in both ED and vascular depression.31,32 Besides, a decreased serum level of plasma testosterone may be the other association between depression in older men with sexual dysfuncion.33 One population-based study found the relationship between depression or antidepressants and ED.34 The findings may suggest a bidirectional association between depression with ED.35
Taking migraine and comorbidity both into consideration, the migraine patients with anxiety had a 3.6-fold higher HR of having been diagnosed with ED than the control cohort without anxiety. Furthermore, the HRs for subsequent ED among migraine patients demonstrated an increasing effect with comorbidity, such as hypertension, hyperlipidemia, and anxiety. It can remind physicians when treating ED it is essential to consider a global approach and provide a overwhelm treatment to these related issues in addition to the ED.
Nevertheless, there are some limitations in the present study should be addressed. The study's first limitation is its use of ICD coding to diagnose ED. Discussing sexuality is culturally taboo in Taiwan, which may made less ED patient seeking medical assistance in Taiwan as compared to studies conducted in Western countries, so the relative correlation may be underestimated. Second, the causal association cannot determine by our observational study. The present study is primarily a hypothesis and secondarily an aid to clinical practitioners who may want to inquire their patients, who are suffering from comorbidity associated with migraine, about their patients’ sexual health. Further research is required to elucidate the tentative causal association with ED. Third, individual information such as laboratory data, imaging findings, and personal information such as partnership, smoking, alcohol consumption, and obesity, which may contribute to ED, was not available through the administrative dataset. We will not be able to clarify the relationship between these factors and comorbid disease development. Fourth, the severity of disease was not documented in this study; a possible confounding effect arising from this variable cannot be excluded. Fifth, chronic use of antihypertensive, digoxin, clofibrate, cimetidine, and various hormonal agents have been reported to be associated with ED.36 However, our study did not evaluate the effect of medication on the development of ED. Lastly, the vast majority of enrollees are ethnic Taiwanese people under the Taiwan NHI program. Therefore, the application of our findings to other ethnicities should be exercised with caution. Finally, the study's design cannot prevent the possibility of ascertainment bias—meaning patients with ED may be more likely to receive examination for clinically asymptomatic comorbidity than patients without ED. Likewise, those patients with comorbidity, by virtue of their greater exposure, are more likely to report ED than those who have less contact with physicians. Thus, the results of our study do not seem to have been compromised by ascertainment bias.
CONCLUSION
In this study, we want to estimate the association between migraine and ED using a nationwide population-based database and want to highlight the support that patients with migraine have a higher incidence of being diagnose with ED, particularly in the patient with the comorbidity of anxiety. When assessing patients for ED in clinical practice, we can take migraine and other comorbidity into consideration and treated as well. When assessing patients for ED in daily clinical practice and providing timely sexual counseling for such patients, migraine, and other comorbidity should be taken into consideration and may be warranted.
Footnotes
Abbreviations: aHR = adjusted hazard ratio, BNHI = Bureau of National Health Insurance, CI = confidence interval, ED = erectile dysfunction, LHID 2000 = Longitudinal Health Insurance Database 2000, NERD = nonerosive reflux disease, NHI = National Health Insurance, NHIA = National Health Insurance Administration, NHIRD = National Health Insurance Research Database, NHRI = National Health Research Institutes
Author contributions—all authors have contributed significantly, and that all authors are in agreement with the content of the manuscript. Conception/design: all authors; provision of study materials: C-HK; collection and/or assembly of data: all authors; data analysis and interpretation: all authors; manuscript writing: all authors; final approval of manuscript: all authors.
S-HW and M-CL contributed equally to this study.
Also, D-JY and C-HK contributed equally to this work.
Funding: this study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019), China Medical University Hospital, Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10501010037), NRPB Stroke Clinical Trial Consortium (MOST 104-2325-B-039-005), Tseng-Lien Lin Foundation, Taichung, Taiwan, Taiwan Brain Disease Foundation, Taipei, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan; and CMU under the Aim for Top University Plan of the Ministry of Education, Taiwan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding received for this study.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Lipton RB, Pan J. Is migraine a progressive brain disease? JAMA 2004; 291:493–494. [DOI] [PubMed] [Google Scholar]
- 2.Patel NV, Bigal ME, Kolodner KB, et al. Prevalence and impact of migraine and probable migraine in a health plan. Neurology 2004; 63:1432–1438. [DOI] [PubMed] [Google Scholar]
- 3.Kelman L, Rains JC. Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache 2005; 45:904–910. [DOI] [PubMed] [Google Scholar]
- 4.McInnes RA. Chronic illness and sexuality. Med J Aust 2003; 179:263–266. [DOI] [PubMed] [Google Scholar]
- 5.Kessler TM, Fowler CJ, Panicker JN. Sexual dysfunction in multiple sclerosis. Expert Rev Neurother 2009; 9:341–350. [DOI] [PubMed] [Google Scholar]
- 6.Shiri R, Koskimäki J, Hakama M, et al. Effect of chronic diseases on incidence of erectile dysfunction. Urology 2003; 62:1097–1102. [DOI] [PubMed] [Google Scholar]
- 7.Tamler R. Diabetes, obesity, and erectile dysfunction. Gend Med 2009; 6 (Suppl 1):4–16. [DOI] [PubMed] [Google Scholar]
- 8.Hashizume M, Yamada U, Sato A, et al. Stress and psychological factors before a migraine attack: a time-based analysis. Biopsychosoc Med 2008; 2:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Althof SE. Quality of life and erectile dysfunction. Urology 2002; 59:803–810. [DOI] [PubMed] [Google Scholar]
- 10.Bestepe E, Cabalar M, Kucukgoncu S, et al. Sexual dysfunction in women with migraine versus tension-type headaches: a comparative study. Int J Impot Res 2011; 23:122–127. [DOI] [PubMed] [Google Scholar]
- 11.Ifergane G, Ben-Zion IZ, Plakht Y, et al. Not only headache: higher degree of sexual pain symptoms among migraine sufferers. J Headache Pain 2008; 9:113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nappi RE, Terreno E, Tassorelli C, et al. Sexual function and distress in women treated for primary headaches in a tertiary university center. J Sex Med 2012; 9:761–769. [DOI] [PubMed] [Google Scholar]
- 13.Shen TC, Chen WC, Lin CL, et al. The risk of erectile dysfunction in chronic obstructive pulmonary disease: a population-based cohort study in Taiwan. Medicine (Baltimore) 2015; 94:e448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen YG, Lin TY, Lin CL, et al. Risk of erectile dysfunction in transfusion-naive thalassemia men: a nationwide population-based retrospective cohort study. Medicine (Baltimore) 2015; 94:e700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsu CY, Lin CL, Kao CH. Irritable bowel syndrome is associated not only with organic but also psychogenic erectile dysfunction. Int J Impot Res 2015; 27:233–238. [DOI] [PubMed] [Google Scholar]
- 16.Hsu CY, Lin CL, Kao CH. Gout is associated with organic and psychogenic erectile dysfunction. Eur J Intern Med 2015; 26:691–695. [DOI] [PubMed] [Google Scholar]
- 17.LoPiccolo J. Rosen RC, Leiblum SR. Postmodern sex therapy for erectile failure. Erectile Disorders: Assessment and Treatment.. New York:Guilford Press; 1992. 171–197. [Google Scholar]
- 18.The Process of Care Consensus Panel. The process of care model for evaluation and treatment of erectile dysfunction. Int J Impot Res 1999; 11:59–74. [DOI] [PubMed] [Google Scholar]
- 19.Jardin A, Wagner G, Khoury S, et al. Erectile Dysfunction. Plymouth:Health Publications; 2000. [Google Scholar]
- 20.Huang CY, Keller JJ, Sheu JJ, et al. Migraine and erectile dysfunction: evidence from a population-based case-control study. Cephalalgia 2012; 32:366–372. [DOI] [PubMed] [Google Scholar]
- 21.Sicuteri F, Del Bene E, Fonda C. Sex, migraine and serotonin interrelationships. Monogr Neural Sci 1976; 3:94–101. [DOI] [PubMed] [Google Scholar]
- 22.Lewis RW. Epidemiology of erectile dysfunction. Urol Clin North Am 2001; 28:209–216.vii. [DOI] [PubMed] [Google Scholar]
- 23.Montorsi F, Briganti A, Salonia A, et al. Erectile dysfunction prevalence, time of onset and association with risk factors in 300 consecutive patients with acute chest pain and angiographically documented coronary artery disease. Eur Urol 2003; 44:360–364.discussion 364–365. [DOI] [PubMed] [Google Scholar]
- 24.Yao F, Huang Y, Zhang Y, et al. Subclinical endothelial dysfunction and low-grade inflammation play roles in the development of erectile dysfunction in young men with low risk of coronary heart disease. Int J Androl 2012; 35:653–659. [DOI] [PubMed] [Google Scholar]
- 25.Vlachopoulos C, Rokkas K, Ioakeimidis N, et al. Inflammation, metabolic syndrome, erectile dysfunction, and coronary artery disease: common links. Eur Urol 2007; 52:1590–1600. [DOI] [PubMed] [Google Scholar]
- 26.Montorsi P, Ravagnani PM, Galli S, et al. The artery size hypothesis: a macrovascular link between erectile dysfunction and coronary artery disease. Am J Cardiol 2005; 96:19M–23M. [DOI] [PubMed] [Google Scholar]
- 27.Malavige LS, Levy JC. Erectile dysfunction in diabetes mellitus. J Sex Med 2009; 6:1232–1247. [DOI] [PubMed] [Google Scholar]
- 28.Azadzoi KM, Saenz de Tejada I. Hypercholesterolemia impairs endothelium-dependent relaxation of rabbit corpus cavernosum smooth muscle. J Urol 1991; 146:238–240. [DOI] [PubMed] [Google Scholar]
- 29.Hedon F. Anxiety and erectile dysfunction: a global approach to ED enhances results and quality of life. Int J Impot Res 2003; 15 (Suppl 2):S16–19. [DOI] [PubMed] [Google Scholar]
- 30.Van Thiel DH, Gavaler JS, Sanghvi A. Recovery of sexual function in abstinent alcoholic men. Gastroenterology 1983; 84:677–682. [PubMed] [Google Scholar]
- 31.Bonierbale M, Lançon C, Tignol J. The ELIXIR study: evaluation of sexual dysfunction in 4557 depressed patients in France. Curr Med Res Opin 2003; 19:114–124. [DOI] [PubMed] [Google Scholar]
- 32.Baldwin RC. Is vascular depression a distinct sub-type of depressive disorder? A review of causal evidence. Int J Geriatr Psychiatry 2005; 20:1–11. [DOI] [PubMed] [Google Scholar]
- 33.Barrett-Connor E, Von Mühlen DG, Kritz-Silverstein D. Bioavailable testosterone and depressed mood in older men: the Rancho Bernardo Study. J Clin Endocrinol Metab 1999; 84:573–577. [DOI] [PubMed] [Google Scholar]
- 34.Shiri R, Koskimäki J, Tammela TL, et al. Bidirectional relationship between depression and erectile dysfunction. J Urol 2007; 177:669–673. [DOI] [PubMed] [Google Scholar]
- 35.Araujo AB, Durante R, Feldman HA, et al. The relationship between depressive symptoms and male erectile dysfunction: cross-sectional results from the Massachusetts Male Aging Study. Psychosom Med 1998; 60:458–465. [DOI] [PubMed] [Google Scholar]
- 36.Brock GB, Lue TF. Drug-induced male sexual dysfunction. An update. Drug Saf 1993; 8:414–426. [DOI] [PubMed] [Google Scholar]


