Abstract
Few studies involving human participants have been conducted to investigate the effect of orthodontic treatment on alveolar bone density around the teeth. Our previous study revealed that patients who received 6 months of active orthodontic treatment exhibited an ∼24% decrease in alveolar bone density around the teeth. However, after an extensive retention period following orthodontic treatment, whether the bone density around the teeth can recover to its original state from before the treatment remains unclear, thus warranting further investigation.
The purpose of this study was to assess the bone density changes around the teeth before, during, and after orthodontic treatment.
Dental cone-beam computed tomography (CBCT) was used to measure the changes in bone density around 6 teeth in the anterior maxilla (maxilla central incisors, lateral incisors, and canines) of 8 patients before and after orthodontic treatment. Each patient underwent 3 dental CBCT scans: before treatment (T0); at the end of 7 months of active orthodontic treatment (T1); after several months (20–22 months) of retention (T2). The Friedman test was applied to evaluate the changes in the alveolar bone density around the teeth according to the 3 dental CBCT scans.
From T0 to T1, a significant reduction in bone density was observed around the teeth (23.36 ± 10.33%); by contrast, a significant increase was observed from T1 to T2 (31.81 ± 23.80%). From the perspective of the overall orthodontic treatment, comparing the T0 and T2 scans revealed that the bone density around the teeth was relatively constant (a reduction of only 0.75 ± 19.85%). The results of the statistical test also confirmed that the difference in bone density between T0 and T2 was nonsignificant.
During orthodontic tooth movement, the alveolar bone density around the teeth was reduced. However, after a period of bone recovery, the reduced bone density recovered to its previous state from before the orthodontic treatment. However, the bone density around ∼10% of the teeth in this region could not recover to 80% of its state from before the orthodontic treatment.
INTRODUCTION
Orthodontic treatment enables straightening the teeth of patients with malocclusion. In addition to enhancing teeth appearance, such treatment can also improve an undesirable occlusal scheme.1–3 However, observing the internal conditions of the alveolar bone (e.g., changes in root resorption and bone density around the teeth) during orthodontic treatment is difficult. Previous studies have indicated that orthodontic treatment can induce permanent root resorption; this causes root shortening, which increases the crown–root ratio and results in loose teeth.4 Thus, understanding orthodontic treatment-induced changes in alveolar bone density around the teeth is a critical research topic.
Among current methods for determining alveolar bone density, computed tomography (CT)5–10 and dental cone-beam computed tomography (CBCT)10–14 are the most applicable approaches because these 2 methods are noninvasive and provide information on the 3-dimensional (3D) structure of the bone. Moreover, CT and CBCT enable measuring the Hounsfield units (HU) or grayscale value (GV) of bone tissue; hence, they are also used in assessing radiographic bone density11,15,16 and are thus applicable to evaluating changes in bone density.11,17,18 In recent years, CT and dental CBCT have predominantly been used to assess alveolar bone density before dental implant surgery.10–14 However, undergoing multiple CT scans during orthodontic treatment exposes patients to high radiation dosages. By contrast, dental CBCT systems emit low doses of radiation and thus can be used for continually monitoring a patient's condition during orthodontic treatment.1,19,20
Some previous studies on the effect of orthodontic treatment on changes in alveolar bone density have indicated that orthodontic tooth movement can decrease bone density around the teeth,19,21–23 whereas others have reported the opposite.21,24,25 Campos et al26 indicated that bone density around the teeth following orthodontic treatment is similar to that from before treatment. Thus, research results regarding the effect of orthodontic treatment on bone density around the teeth have been inconsistent. Our previous study verified that after 7 months of active orthodontic treatment, alveolar bone density around the teeth was reduced by ∼24%,23 but whether this decrease is temporary (recoverable after a retention period) or permanent (similar to tooth resorption) requires further investigations. Therefore, in the present study, dental CBCT was applied to evaluate the changes in bone density around the teeth before, during, and after orthodontic treatment. Specifically, we hypothesized that despite alveolar bone density around the teeth being reduced after 7 months of active orthodontic treatment, it eventually recovers to its original state after the retention period has passed.
MATERIALS AND METHODS
Patient Selection, Dental CBCT Scanning Setup, and Time
Patient selection and the dental CBCT scanning setup and time were as reported in our previous study,23 which is briefly described as follows. Eight patients (age: 20–25 years) were selected for this study. A stainless steel bracket (Microarch, Roth type, Tomy International, Tokyo, Japan) and an improved superelastic NiTi-alloy archwire (LH wire, Tomy International) were used in this study. All patients underwent 3 CBCT (Imaging Sciences International, Hatfield) scans: before the orthodontic treatment (T0); at the end of 7 months of active orthodontic treatment (T1); and after several months (20–24 months) of retention (T2). Dental CBCT images were taken with the following parameters: 120 kVp, 47 mA, 250-μm voxel resolution, and 16-cm field-of-view. The research protocol used in this study was approved by the institutional research board of China Medical University and Medical Center (DMR96-IRB-160) and all patients have signed informed consent prior their participation in accordance with the Declaration of Helsinki.
Measurement of Bone Density Around the Teeth
The 6 teeth (the left and right canines, lateral incisors, and central incisors) in the anterior maxilla were selected as the target teeth. Dental CBCT images of each patient were imported into medical imaging software (Mimics 15.0, Materialise, Leuven, Belgium). Before measuring the bone densities around the teeth, the whole CBCT images were resliced to obtain new slices that were perpendicular to the longitudinal axes of the teeth by using the “reslice” function in the Mimics. The bone density around the tooth was assessed at 3 levels: cervical (3 mm above the cementoenamel junction), intermediate (between the cervical and apical levels), and apical (1 mm below the root tip) levels (Figure 1). To more accurately measure the alveolar bone density around the teeth, the measurement approach was modified slightly from our previous study.23
FIGURE 1.
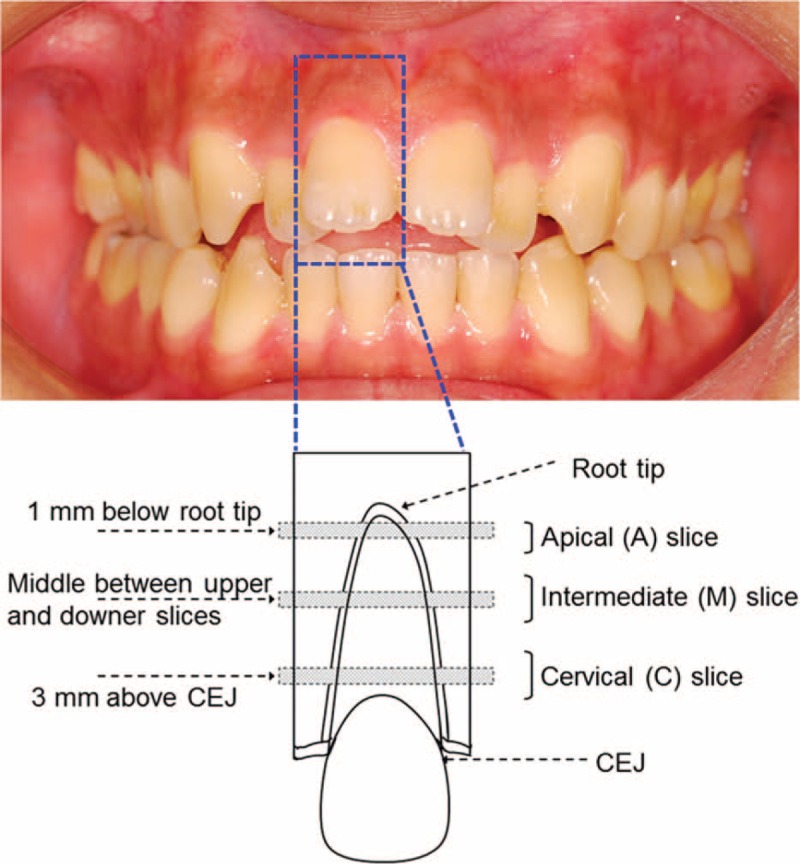
Schematic of the 3 levels at which the root of the upper right lateral incisor and surrounding bone were cross sectioned. CEJ = cementoenamel junction (the figure was adapted from our previous study).23
Figure 2 shows the procedure for measuring the bone density in the middle portion of the intermediate slice of the upper right lateral incisor (Patient 5). First, the area of the tooth in the slice was selected on the basis of the GV of the cementum (Figure 2A). The area of interest was expanded by 1 voxel (250 μm) to include the thickness of the periodontal ligament (PDL) (Figure 2B), and then by a further 3 voxels (750 μm) to include the surrounding bone (Figure 2C). Finally, the combined area of the tooth plus the PDL was subtracted from the entire area (i.e., the tooth plus the PDL) by using a Boolean operation to obtain the bone density around the tooth (Figure 2D).
FIGURE 2.
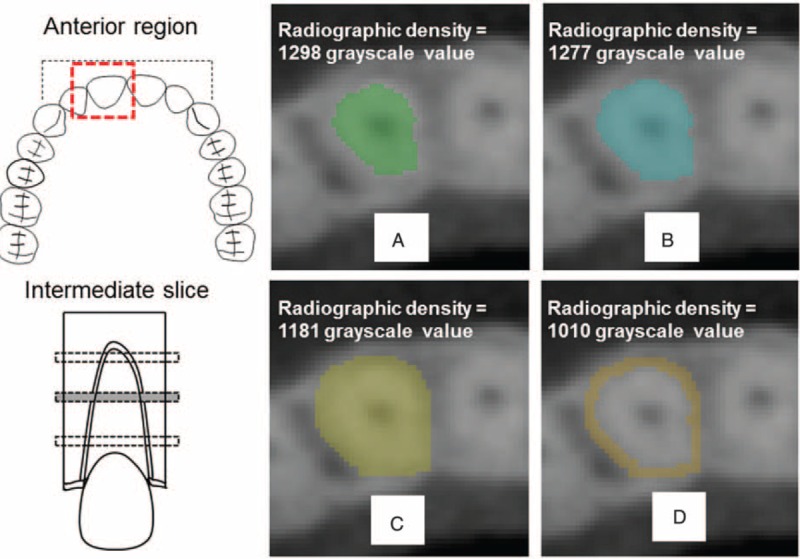
Bone-density measurement around the upper right incisor in the intermediate slice of Patient 5: (upper left) schematic occlusal view of the maxilla; (lower left) schematic of the middle slice of the intermediate portion of the upper right incisor; (A) segment the area of the tooth from the CBCT image according to the threshold value of the cementum; (B) expand the area by 1 voxel to include the PDL; (C) expand the area by a further 3 voxels to include the surrounding bone; (D) subtract the tooth and PDL from the combined tooth, PDL, and surrounding bone. The volumes of the areas of interest (mm3) and their densities (GV in the CBCT image) are also indicated (the figure was adapted from our previous study).23 CBCT = cone-beam computed tomography, GV = grayscale value, PDL = periodontal ligament.
Statistical Analysis
Before the bone density changes during orthodontic treatment were analyzed, the accuracy of the dental CBCT machine was validated. Furthermore, the intrarater and interrater measurement errors could be neglected in this study. For further detail on the approaches used in the present study, please refer to.23
The bone density around the teeth at T0, T1, and T2 were contrasted using the Friedman test. In addition, the bone density changes in different teeth and levels were analyzed using the Kruskal–Wallis test. All statistical analyses were performed using SPSS Version 19 (IBM Corporation, Armonk, NY). The level of the statistical significance was set as P < 0.05.
RESULTS
Alveolar Bone Density Changes Around the Teeth at T1 and T0
From T0 to T1, the 8 patients underwent 7 months of active orthodontic treatment to straighten their teeth. The method for measuring the bone density around the teeth was modified slightly from that used in our previous study.23 The measurement values, particularly those at the intermediate level, differed slightly yet were relatively similar to those acquired in our previous study,23 except for the apical level of the upper left lateral incisor and the cervical level of the upper left canine of Patient 3, whose maxillary anterior bone density around the teeth was significantly reduced by 23.36 ± 10.33% (range of reduction = − 44.13% to 9.40 %) at T1 (Figure 3 , left column).
FIGURE 3.
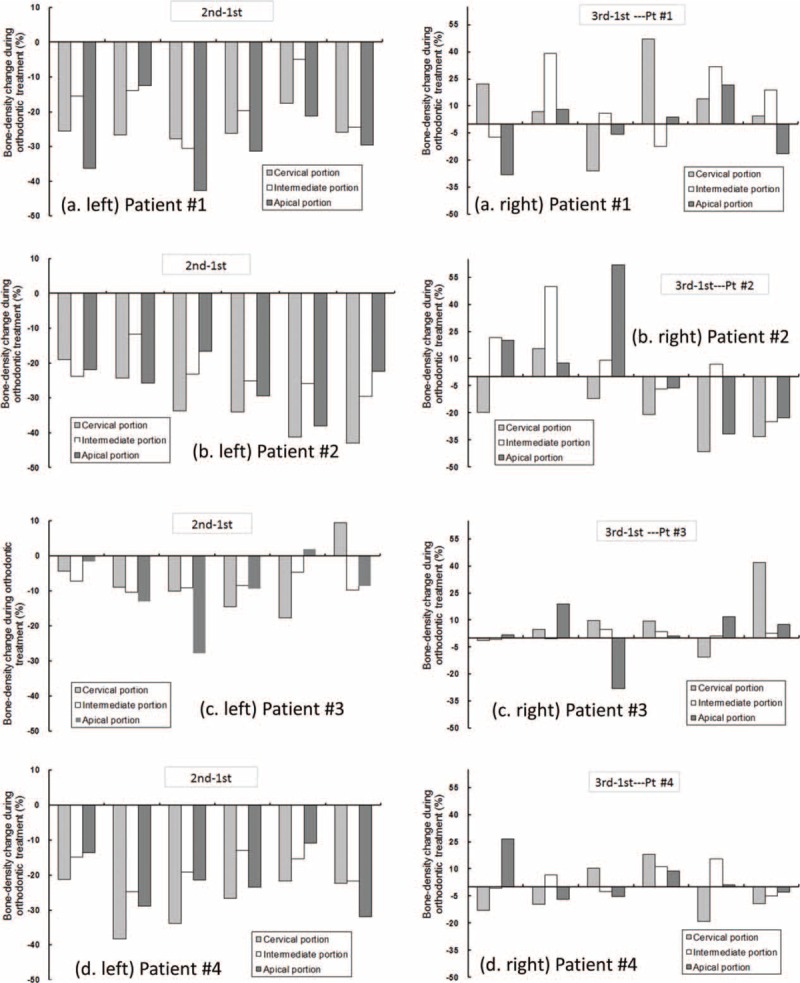
Bone density changes around the 3 levels of each patient's teeth during orthodontic treatment (UL1 = upper left central incisor, UL2 = upper left lateral incisor, UL3 = upper left canine, UR1 = upper right central incisor, UR2 = upper right lateral incisor, UR3 = upper right canine). Left column: changes between T1 and T0, right column: changes between T2 and T0. (A) Patient 1; (B) Patient 2; (C) Patient 3; (D) Patient 4; (E) Patient 5; (F) Patient 6; (G) Patient 7; (H) Patient 8.
FIGURE 3 (Continued).
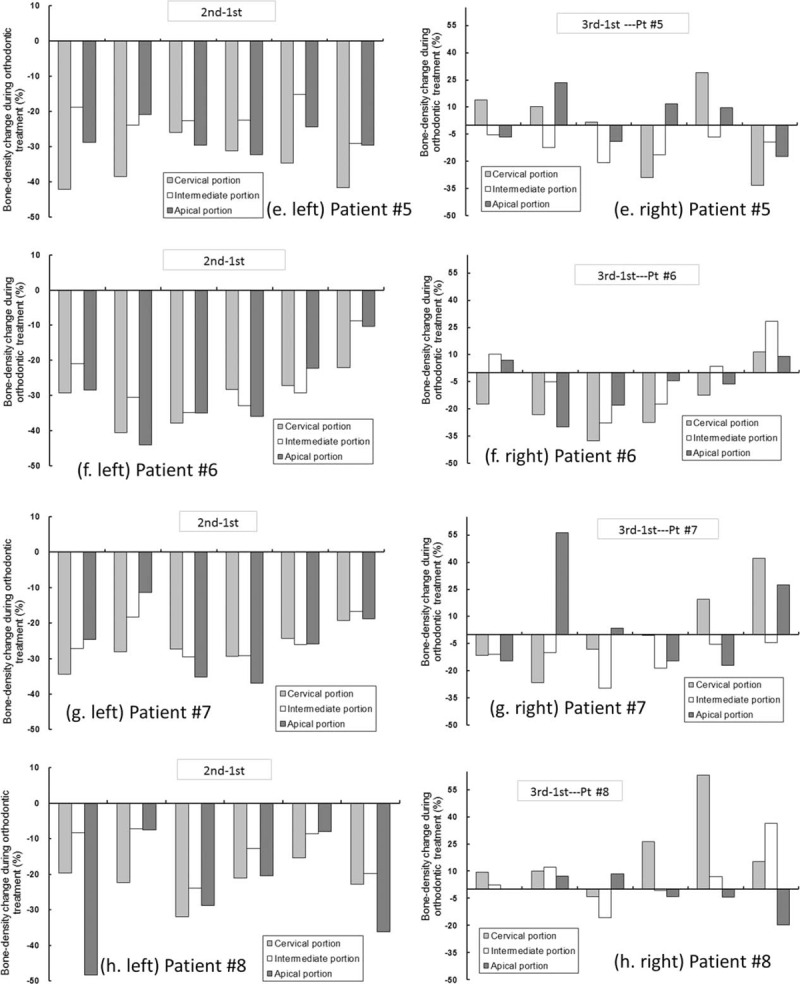
Bone density changes around the 3 levels of each patient's teeth during orthodontic treatment (UL1 = upper left central incisor, UL2 = upper left lateral incisor, UL3 = upper left canine, UR1 = upper right central incisor, UR2 = upper right lateral incisor, UR3 = upper right canine). Left column: changes between T1 and T0, right column: changes between T2 and T0. (A) Patient 1; (B) Patient 2; (C) Patient 3; (D) Patient 4; (E) Patient 5; (F) Patient 6; (G) Patient 7; (H) Patient 8.
Alveolar Bone Density Changes Around the Teeth at T2 and T1
From T1 to T2, the bone density around the teeth of the 8 patients (8 patients × 6 teeth × 3 levels = 144 samples) was significantly increased by an average of 31.81 ± 23.80% (range of increase = 0.93–99.59%). Additionally, the results revealed a trend in which a high bone density decrease from T0 to T1 results in a high bone density increase from T1 to T2.
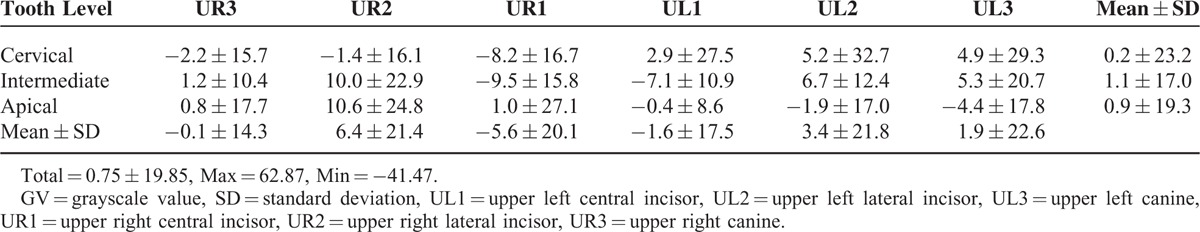
Alveolar Bone Density Changes Around the Teeth at T2 and T0.
The difference in bone density around the teeth between T0 and T2 was 0.75 ± 19.85% (Figure 3 , right column). Despite the average difference in bone density approximating 0 (and the densities before and after the treatment were also similar), the variance among the 144 samples ranged between −41.47% and 62.87%, and 16 samples exhibited a reduction of >20%. In other words, the bone density of 11% (16/144 samples) of the teeth in this region failed to recover to 80% of its original state.
Alveolar Bone Density Changes Around the Teeth in Different Teeth and Levels
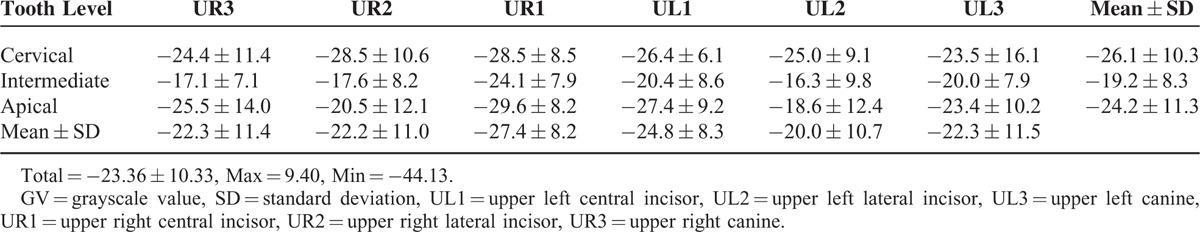
From T0 to T1, the declining trend in bone density around each tooth region was similar to that in our previous study.23 The largest mean bone-density reduction was observed around the central incisors, followed by the canines, and then the lateral incisors. However, comparing the extent of bone density reduction among the 3 root levels revealed distinctive results. Specifically, in contrast to our previous study,23 in which the mean bone-density reductions at the cervical (25.9%), intermediate (21.9%), and apical (23.9%) levels were nonsignificant, the mean bone-density reduction at the intermediate level (19.2%) was lower than those at the cervical (26.1%) and apical (24.2%) levels (Table 1).
TABLE 1.
Percentage Bone Density (GV) Changes (Mean ± SD) Around the Teeth in the 3 Levels of the 8 Patients Between T0 and T1
From T1 to T2 and from T0 to T2, the change in bone density around the tooth regions exhibited distinctive trends (Tables 2 and 3). Moreover, comparing the change in bone-density reductions at the 3 root levels revealed that from T1 to T2, the mean bone density change at the intermediate level (25.4 ± 18.4%) was less than that at the cervical (35.9 ± 28.2%) and apical (34.1 ± 23.0%) levels (Table 2). In addition, the differences in the mean bone density change at the cervical (0.2 ± 23.2%), intermediate (1.1 ± 17.0%), and apical (0.9 ± 19.3%) levels were nonsignificant from T0 to T2 (Table 3).
TABLE 2.
Percentage Bone Density (GV) Changes (Mean ± SD) Around the Teeth in the 3 Levels of the 8 Patients Between T1 and T2
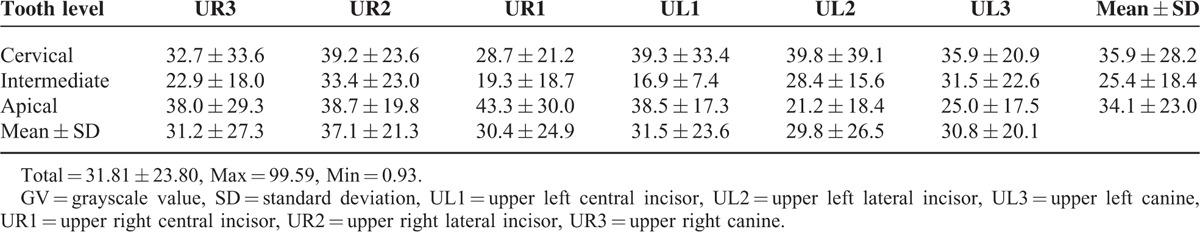
TABLE 3.
Percentage Bone Density (GV) Changes (Mean ± SD) Around the Teeth in the 3 Levels of the 8 Patients Between T0 and T2
DISCUSSION
Despite the success of orthodontic treatment in realigning the teeth, this type of treatment can also affect the appearance and density of the alveolar bone. Changes in appearance of the alveolar bone can be observed easily, whereas tissue reactions in the bone are difficult to observe. Previous studies on the effect of orthodontic tooth movement on bone density around the teeth have mainly involved animal models22,24 or computer simulations.25 By contrast, our previous study was the first to apply dental CBCT to explore the effect of orthodontic treatment on bone density changes around the teeth. The results of our previous study revealed that after 7 months of active orthodontic treatment, the bone density around the 6 teeth in the anterior maxilla was reduced by 24%.23 However, we were unsure of whether the bone density would recover to its original state after all orthodontic treatment stages were completed. Therefore, the present study extends our previous study by monitoring bone density changes around the teeth of patients who previously received orthodontic treatment. Additionally, the method applied in the previous study was modified slightly for the present study. The results indicate that although active orthodontic treatment can reduce bone density around the teeth, the associated bone can recover to its original density after 2 years of retention.
Currently, various noninvasive clinical methods can be used to measure bone density, including digital image analysis of microradiographs,27 dual-energy x-ray absorptiometry,28 and ultrasound measurement.29 However, these methods cannot accurately emulate 3D bone-tissue structures and were thus considered unsuitable for the present study. Additionally, CT and peripheral quantitative CT are prevalent clinical methods for measuring bone density. In particular, CT involves exploring the linear correlation between the bone HU and bone density.5–9 However, CT exposes patients to high dosages of radiation and it is thus unsafe for conducting multiple scans on orthodontic patients within a short period (2–3 years). Compared with CT scanners, for which the fan-beam imaging approach has been applied for many decades, dental CBCT scanners, which utilize a cone-beam imaging method, were pioneered independently by Mozzo et al30 and Arai et al31 in the late 1990s. Since 2004, dental CBCT has become prevalent in dentistry clinical treatments and in vitro experiments.32–35
The prevalence of dental CBCT is attributable to its numerous advantages.17,32–34 it involves lower dosages of radiation, incurs less cost, and requires less space compared with CT. However, several studies have indicated that the bone GV determined through dental CBCT is not equivalent to the bone HU. Moreover, GV is an unreliable indicator for measuring bone mineral density (BMD)36 because it can be affected by various factors including dental CBCT instrument specifications, scanning parameter configurations (current, voltage, and scan time), scanning location, and field of scan.18,36,37 Nevertheless, numerous studies have confirmed a strong direct correlation between dental CBCT bone GV and CT bone HU.18,38–42 Furthermore, previous studies have indicated that dental CBCT is applicable for assessing bone density.11,17,18,43,44 Similar to the aforementioned studies, we also applied dental CBCT to examine changes in the alveolar bone density around the teeth of patients who had received orthodontic treatment. Moreover, the dental CBCT scanning parameter configurations, including the angle at which the patient tilts his or her head during the scanning process, were consistent throughout this study, and the bone density comparisons involved the same patients and tooth regions but at different treatment periods. Therefore, the results of our study are unlikely to be affected by the intrinsic defects of dental CBCT. Several other recent studies have also adopted dental CBCT to examine changes in alveolar bone density around the teeth of orthodontic patients.1,19
Our previous study23 revealed that from T0 to T1, changes in alveolar bone density around the teeth were on average –24.3 ± 9.5%. In the present study, the average difference of alveolar bone density from T0 to T1 was –23.4 ± 10.3%. This slight difference between the 2 results was attributed to how, in the present study, the intermediate level was defined as the region between the cervical level and apical level, whereas in the previous study, the intermediate level was defined as the region 8 mm below the apical level. According to the length of each tooth, the definition used in the previous study could result in an experimental error when the intermediate level is not located between the cervical and apical levels. In other words, for shorter teeth, the region 8 mm below the apical level might be closely adjacent to the cervical level. Moreover, the extent of bone density reduction (21.9 ± 8.9%) at the intermediate level (T0–T1) in the previous study was larger than that observed in the present study (19.2 ± 8.3%). This finding indicates that the modified definition in the present study enabled accurately pinpointing the intermediate level of a tooth root because during tip and upright tooth movement, the alveolar bone around the intermediate level is subject to less tension and pressure compared with that around the cervical or apical level; hence, the reduction in bone density was smaller. This finding also accords with that of Verna et al (1999), which examined a mouse model and confirmed that, during tooth movement, the bone density change at the intermdiate level was less than that at the cervical and apical levels.
Zhuang et al24 explored the upper right first molars of Sprague–Dawley rats exposed to orthodontic force for 14 days and investigated the associated structural parameters of the trabecular alveolar bone around the upper right first molars. The results revealed that the bone volume fraction of the trabecular alveolar bone around the teeth was significantly increased. This finding is in contrast to that of our previous study during the T0 to T1 period (the alveolar bone density around the teeth was reduced by 23.36% during the T0–T1 period in our study). Zhuang et al24 attributed this contradiction to how micro-CT was applied to acquire the 3D microstructure of the alveolar bone (whereas a 2-dimensional histomorphometric analysis was conducted in our study). However, dental CBCT was used instead of histomorphometric analysis in our study; hence, we disagree with their assertion. We believe that the contradiction between our research results and those of Zhuang et al24 is mainly caused by how they measured the bone volume fraction of the 300 × 300 × 300 μm bone cube on the distal side of the upper right first molars. The bone located in this region is highly susceptible to being affected by a tension force. According to pressure–tension theory, bone density on the tension side should increase. By contrast, we measured the alveolar bone density (thickness = 0.5 mm) around the tooth root, where both the compression and tension sides exert pressure on the alveolar bone; hence, the average bone density in this region was lower than that solely affected by the tension side. The aforementioned inference was verified by another study,21 in which the upper left first molars of Sprague–Dawley rats subjected to 14 days of orthodontic force were investigated (specifically, they investigated the trabecular bone structure parameters on the compression side and tension side on the days 0, 3, 7, and 14). Their results revealed that the bone volume fraction on the compression side was reduced from 69.1% to 31.2%, whereas that on the tension side was increased from 68.22% to 78.20%.21 Therefore, after the alveolar bone was subjected to orthodontic force for 14 days, the extent of reduction in the bone volume fraction on the compression side was greater than that on the tension side.
In addition to conducting mouse model experiments, several scholars have also used dental CBCT to measure the alveolar bone densities of orthodontic patients. Campos et al26 compared the bone mineral densities (BMDs) and root mineral densities (RMDs) of 30 untreated persons and 15 patients who had completed their orthodontic treatment. The results revealed that the RMDs of the 15 patients were reduced, but their BMDs were similar. This finding is in contrast to our findings in our previous study, and this inconsistency was attributed to how our sampling period differed to that of Campos et al.26 Specifically, we measured the difference in bone density between T0 and T1—a period of 7 months of orthodontic treatment—whereas the 15 patients in their study underwent dental CBCT scans for 6 years following completion of their orthodontic treatment, during which their BMDs may have recovered to the original states before the treatment. Moreover, Campos et al26 mainly conducted their study to compare the BMDs and RMDs of treated and untreated individuals and did not use dental CBCT to examine the changes in alveolar bone density before and after orthodontic treatment.
Regarding previous studies that have used dental CBCT to monitor changes in the alveolar bones of orthodontic patients (conducted 2 dental CBCT scans), Jiang et al44 used this instrument to explore changes in the alveolar bone density around the apical, middle, and coronal levels of 18 orthodontic patients who had their premolars removed and received canine retraction. Specifically, they divided the alveolar bone around the teeth into 36 areas and examined the correlation between the direction of tooth movement and changes in bone density. Their results revealed that the alveolar bone density around the teeth was reduced by 4.2% to 11.0%, which is considerably <24% reduction observed in our previous study.23 Jiang et al44 indicated that the difference between the results of their study and our own might be attributed to the interval between the 2 dental CBCT scans in their study (4.9 months) being shorter than that in our study (7 months). Additionally, we believe that this difference might be attributable to several other factors including the type of orthodontic treatment (tooth retraction versus no tooth retraction), type of occlusion, and specifications of the brackets and archwires. Nevertheless, the findings of Jiang et al44 are agreement with our own, in that the newly generated bone tissue following orthodontic treatment was less mineralized.
Recently, Ma et al19 administered othodontic treatment to 41 people with healthy periodontal tissue and 40 patients with chronic periodontitis. All participants received dental CBCT scanning before and after the treatment to enable an analysis of the changes in their alveolar bone height and density. The results confirmed that the alveolar bone height remained constant, but their alveolar bone density was significantly reduced. In particular, the extent of the reduction was clearly noticeable in the patients with chronic periodontitis. Ma et al19 mentioned that bone resorption in areas of pressure and bone deposition in areas of tension are not synchronous, and they classified the new bone tissue as “less-mineralized bones.” Furthermore, their results are similar to those in our previous study,23 confirming that orthodontic treatment can induce the reduction of alveolar bone density. However, their study did not address the timing of the second dental CBCT scans; hence, whether the alveolar bone densities of the participants in their study recovered to their original state before the treatment remains unclear.
The results of the present study confirmed that the changes in alveolar bone density from T0 to T1, from T1 to T2, and from T0 to T2 were –23.36 ± 10.33%, 31.81 ± 23.80%, and 0.75 ± 19.85%, respectively. In particular, the extent of the reduction from T0 to T1 was less prominent than the increase from T1 to T2 because the former value (T0–T1) was calculated using T0 as the denominator, whereas the later value (T1–T2) was calculated using T1 as the denominator. Because the T1 observed values were mostly less than that of T0 values, the average value from T1 to T2 increased. Changes in alveolar bone density before and after the complete orthodontic treatment (T0–T2) revealed that the difference between T0 and T2 was negligible, indicating that alveolar bone-density reduction resulting from orthodontic tooth movement can recover to its original state provided that the recovery period is sufficient to allow complete bone mineralization. Previous studies involving animal model experiments24 and computer simulations25 have revealed that alveolar bone density either increases or remains constant following orthodontic treatment, and this finding is in contrast to that of our previous study.23 This contradiction is mainly caused by how our previous study assessed changes in bone density only from T0 to T1. By contrast, the differences between T0 and T2 in the present study are consistent with those reported by the aforementioned studies. Therefore, after an active orthodontic treatment has been administered to straighten the teeth of a patient, the patient must wear an orthodontic retainer for a certain period, whereas the low-density woven bone mineralizes into the tough lamellar bone.45
Comparing the bone densities around various tooth positions revealed that from T0 to T1, changes in bone density around the central incisors were the highest, followed by those around the canines and lateral incisors. However, no correlation was observed between tooth position and bone density changes from T1 to T2 or from T0 to T1. Changes in bone density around the teeth before and after orthodontic treatment (T0–T2) exhibited a small difference in mean value (0.75%) but a large SD (19.85%), indicating high variance in the bone density changes (from–41.47% to 62.87%). Among the 144 samples in the present study, 16 samples exhibited a bone-density reduction exceeding 20%. In other words, following orthodontic treatment, bone density around ∼11% of the teeth in this region failed to recover to 80% of its previous state. In particular, these 16 samples were mainly collected from 2 patients (each provided 5 samples). Therefore, we suggested that these 2 patients wear an orthodontic retainer for an extended period to allow their bones to fully mineralize. Nevertheless, their recovery should be monitored.
The limitations of this study are described as follows. First, despite many previous studies having verified that dental CBCT is suitable for assessing bone density, several studies have indicated that the bone GV obtained through this method do not represent BMD. However, because this method involves low radiation dosages and enables us to use the same CBCT instrument and scan settings used in our previous study, we believe that this method is the most applicable one for monitoring changes in alveolar bone density around the teeth of orthodontic patients. Second, this study measured only the alveolar bone density around the teeth in the anterior maxilla, but the bone density around the mandibular teeth or multirooted teeth in the posterior region also merits further investigation. Third, to obtain the 3D measurement of the alveolar bone density around the teeth by using low radiation dosages, only the CBCT instrument was used. Other methods that may be formulated in the future could provide relevant information. Finally, because of the difficulty involved in long-term follow-up research, the present study investigated only 8 patients undergoing orthodontic treatment over a 3-year period. Future studies are suggested to monitor a larger sample of patients to obtain more definitive research outcomes.
CONCLUSION
Based on the experimental setup and given the research limitations, particularly that the research sample comprised only 8 patients, the following conclusions were derived:
Under identical dental CBCT scan settings; this method can be used to analyze changes in bone density around a tooth position (e.g., the alveolar bone around a tooth) of patients before, during, and after orthodontic treatment.
Comparing the difference between T0 and T1—a 7-month period of active orthodontic treatment—revealed 23.36% reduction in bone density around the teeth, whereas the difference between T1 and T2 (after the retention period) showed a 31.81% increase in bone density.
Comparing the difference between T0 and T2 (before and after orthodontic treatment) confirmed that the bone density around the teeth remained mostly constant (0.75% mean reduction). However, the bone density around ∼11% of the teeth in this region failed to recover to only 80% of its original state.
Footnotes
Abbreviations: BMDs = bone mineral densities, CBCT = cone-beam computed tomography, CT = computed tomography, GV = grayscale value, HU = Hounsfield units, PDL = periodontal ligament, RMDs = root mineral densities
Funding: this study was supported by the Ministry of Science and Technology, Taiwan (MOST 103-2815-C-039-077-B and MOST 103-2221-E-039-002).
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Chang HW, Huang HL, Yu JH, et al. Effects of orthodontic tooth movement on alveolar bone density. Clin Oral Investig 2012; 16:679–688. [DOI] [PubMed] [Google Scholar]
- 2.Sunnak R, Johal A, Fleming P. Is orthodontics prior to 11 years of age evidence-based? A systematic review and meta-analysis. J Dent 2015; 43:477–486. [DOI] [PubMed] [Google Scholar]
- 3.Rischen RJ, Breuning KH, Bronkhorst EM, et al. Records needed for orthodontic diagnosis and treatment planning: a systematic review. PLoS One 2013; 8:e74186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu JH, Shu KW, Tsai MT, et al. A cone-beam computed tomography study of orthodontic apical root resorption. J Dent Sci 2013; 8:74–79. [Google Scholar]
- 5.Banse X, Devogelaer JP. Does peripheral quantitative computed tomography ignore tissue density of cancellous bone? J Clin Densitom 2002; 5:403–410. [DOI] [PubMed] [Google Scholar]
- 6.Li X, Viceconti M, Cohen MC, et al. Developing CT based computational models of pediatric femurs. J Biomech 2015; 48:2034–2040. [DOI] [PubMed] [Google Scholar]
- 7.Dragomir-Daescu D, Salas C, Uthamaraj S, et al. Quantitative computed tomography-based finite element analysis predictions of femoral strength and stiffness depend on computed tomography settings. J Biomech 2015; 48:153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Link TM, Lang TF. Axial QCT: clinical applications and new developments. J Clin Densitom 2014; 17:438–448. [DOI] [PubMed] [Google Scholar]
- 9.Fonseca A, Gordon CL, Barr RD. Peripheral quantitative computed tomography (pQCT) to assess bone health in children, adolescents, and young adults: a review of normative data. J Pediatr Hematol Oncol 2013; 35:581–589. [DOI] [PubMed] [Google Scholar]
- 10.Fuh LJ, Huang HL, Chen CS, et al. Variations in bone density at dental implant sites in different regions of the jawbone. J Oral Rehabil 2010; 37:346–351. [DOI] [PubMed] [Google Scholar]
- 11.Aranyarachkul P, Caruso J, Gantes B, et al. Bone density assessments of dental implant sites: 2. Quantitative cone-beam computerized tomography. Int J Oral Maxillofac Implants 2005; 20:416–424. [PubMed] [Google Scholar]
- 12.Benavides E, Rios HF, Ganz SD, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent 2012; 21:78–86. [DOI] [PubMed] [Google Scholar]
- 13.Song YD, Jun SH, Kwon JJ. Correlation between bone quality evaluated by cone-beam computerized tomography and implant primary stability. Int J Oral Maxillofac Implants 2009; 24:59–64. [PubMed] [Google Scholar]
- 14.Guerrero ME, Jacobs R, Loubele M, et al. State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin Oral Investig 2006; 10:1–7. [DOI] [PubMed] [Google Scholar]
- 15.González-García R, Monje F. The reliability of cone-beam computed tomography to assess bone density at dental implant recipient sites: a histomorphometric analysis by micro-CT. Clin Oral Implants Res 2013; 24:871–879. [DOI] [PubMed] [Google Scholar]
- 16.Giro G, Gonçalves D, Sakakura CE, et al. Influence of estrogen deficiency and its treatment with alendronate and estrogen on bone density around osseointegrated implants: radiographic study in female rats. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105:162–167. [DOI] [PubMed] [Google Scholar]
- 17.Naitoh M, Hirukawa A, Katsumata A, et al. Evaluation of voxel values in mandibular cancellous bone: relationship between cone-beam computed tomography and multislice helical computed tomography. Clin Oral Implants Res 2009; 20:503–506. [DOI] [PubMed] [Google Scholar]
- 18.Kim DG. Can dental cone beam computed tomography assess bone mineral density? J Bone Metab 2014; 21:117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma ZG, Yang C, Fang B, et al. Three-D imaging of dental alveolar bone change after fixed orthodontic treatment in patients with periodontitis. Int J Clin Exp Med 2015; 8:2385–2391. [PMC free article] [PubMed] [Google Scholar]
- 20.Huang H, Richards M, Bedair T, et al. Effects of orthodontic treatment on human alveolar bone density distribution. Clin Oral Investig 2013; 17:2033–2040. [DOI] [PubMed] [Google Scholar]
- 21.Ru N, Liu SSY, Zhuang L, et al. In vivo microcomputed tomography evaluation of rat alveolar bone and root resorption during orthodontic tooth movement. Angle Orthod 2013; 83:402–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verna C, Zaffe D, Siciliani G. Histomorphometric study of bone reactions during orthodontic tooth movement in rats. Bone 1999; 24:371–379. [DOI] [PubMed] [Google Scholar]
- 23.Hsu JT, Chang HW, Huang HL, et al. Bone density changes around teeth during orthodontic treatment. Clin Oral Investig 2011; 15:511–519. [DOI] [PubMed] [Google Scholar]
- 24.Zhuang L, Bai Y, Meng X. Three-dimensional morphology of root and alveolar trabecular bone during tooth movement using micro-computed tomography. Angle Orthod 2011; 81:420–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C, Han J, Li Q, et al. Simulation of bone remodelling in orthodontic treatment. Comput Methods Biomech Biomed Engin 2014; 17:1042–1050. [DOI] [PubMed] [Google Scholar]
- 26.Campos MJ, de Albuquerque EG, Pinto BCH, et al. The role of orthodontic tooth movement in bone and root mineral density: a study of patients submitted and not submitted to orthodontic treatment. Med Sci Monit 2012; 18:CR752–CR757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jager A, Radlanski RJ, Taufall D, et al. Quantitative determination of alveolar bone density using digital image analysis of microradiographs. Anat Anz 1990; 170:171–179. [PubMed] [Google Scholar]
- 28.Drage NA, Palmer RM, Blake G, et al. A comparison of bone mineral density in the spine, hip and jaws of edentulous subjects. Clin Oral Implants Res 2007; 18:496–500. [DOI] [PubMed] [Google Scholar]
- 29.Al Haffar I, Padilla F, Nefussi R, et al. Experimental evaluation of bone quality measuring speed of sound in cadaver mandibles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102:782–791. [DOI] [PubMed] [Google Scholar]
- 30.Mozzo P, Procacci C, Tacconi A, et al. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 1998; 8:1558–1564. [DOI] [PubMed] [Google Scholar]
- 31.Arai Y, Tammisalo E, Iwai K, et al. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 1999; 28:245–248. [DOI] [PubMed] [Google Scholar]
- 32.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg 2009; 38:609–625. [DOI] [PubMed] [Google Scholar]
- 33.Scarfe WC, Farman AG, Levin MD, et al. Essentials of maxillofacial cone beam computed tomography. Alpha Omegan 2010; 103:62–67. [DOI] [PubMed] [Google Scholar]
- 34.Vandenberghe B, Jacobs R, Bosmans H. Modern dental imaging: a review of the current technology and clinical applications in dental practice. Eur Radiol 2010; 20:2637–2655. [DOI] [PubMed] [Google Scholar]
- 35.Hsu JT, Wang SP, Huang HL, et al. The assessment of trabecular bone parameters and cortical bone strength: a comparison of micro-CT and dental cone-beam CT. J Biomech 2013; 46:2611–2618. [DOI] [PubMed] [Google Scholar]
- 36.da Silva Campos MJ, de Souza TS, Júnior SLM, et al. Bone mineral density in cone beam computed tomography: only a few shades of gray. World J Radiol 2014; 6:607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nackaerts O, Maes F, Yan H, et al. Analysis of intensity variability in multislice and cone beam computed tomography. Clin Oral Implants Res 2011; 22:873–879. [DOI] [PubMed] [Google Scholar]
- 38.Valiyaparambil JV, Yamany I, Ortiz D, et al. Bone quality evaluation: comparison of cone beam computed tomography and subjective surgical assessment. Int J Oral Maxillofac Implants 2011; 27:1271–1277. [PubMed] [Google Scholar]
- 39.Pittman JW, Navalgund A, Byun SH, et al. Primary migration of a mini-implant under a functional orthodontic loading. Clin Oral Investig 2014; 18:721–728. [DOI] [PubMed] [Google Scholar]
- 40.Nomura Y, Watanabe H, Honda E, et al. Reliability of voxel values from cone-beam computed tomography for dental use in evaluating bone mineral density. Clin Oral Implants Res 2010; 21:558–562. [DOI] [PubMed] [Google Scholar]
- 41.Parsa A, Ibrahim N, Hassan B, et al. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin Oral Implants Res 2015; 26:e1–e7. [DOI] [PubMed] [Google Scholar]
- 42.Mah P, Reeves T, McDavid W. Deriving Hounsfield units using grey levels in cone beam computed tomography. Dentomaxillofac Radiol 2012; 41:500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hsu JT, Chen YJ, Ho JT, et al. A comparison of micro-CT and dental CT in assessing cortical bone morphology and trabecular bone microarchitecture. PLoS One 2014; 9:e107545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jiang F, Liu SSY, Xia Z, et al. Hounsfield unit change in root and alveolar bone during canine retraction. Am J Orthod Dentofacial Orthop 2015; 147:445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meghji S. Bone remodelling. Br Dent J 1992; 172:235–242. [DOI] [PubMed] [Google Scholar]


