Abstract
Background and Purpose
Although the relationship between depression and stroke risk has been investigated, findings in previous reports were conflicting. The aim of this study was to prospectively examine the effect of major depressive episodes (MDE) on stroke incidence and further assess the potential dose-response relationship between numbers of depression symptoms and subsequent stroke risk in Chinese population.
Methods
A total of 199 294 men and 288 083 women aged 30 to 79 years without a prior history of stroke, heart disease and cancer in the China Kadoorie Biobank cohort were followed from 2004 to 2013. A World Health Organization Composite International Diagnostic Interview-Short Form was used to access MDE according to Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV criteria. Stroke events were ascertained through death certificates, medical records and health insurance data.
Results
Past year MDE was marginally associated with a 15% increased risk of stroke (adjusted hazard ratio = 1.15, 95% confidence interval = 0.99-1.33) in the fully-adjusted model, and the association was steeper and statistically significant in individuals aged <50 years, smokers, drinkers, those with higher education degree, BMI <24.0 kg/m2 and no history of diabetes. Moreover, there was a positive dose-response relationship between the number of depression symptoms and increased stroke risk (Ptrend = 0.011). Additionally, smoking status significantly interacted with MDE on stroke onset (P for multiplicative interaction = 0.025).
Conclusions
Findings from this large prospective study suggest that the presence of MDE is a risk factor for stroke, especially in smokers.
Keywords: depression, prospective study, stroke
Subject Terms: Mental Health, Cerebrovascular Disease/Stroke
Introduction
Stroke is the second most common cause of mortality worldwide and the first leading cause of death and disability in China.1, 2 According to the World Health Organization report, the incidence of stroke in China is growing at an annual rate of 8.7 % and this trend will most likely continue over the next three decades.3, 4 It is well known that early identification of risk factors for stroke would allow for effective preventive strategies and reduced economic burden. Some well-established stroke risk factors including hypertension, diabetes, coronary artery disease, smoking, physical inactivity and obesity have been identified;5 however, it is also necessary to investigate more potential risk factors.
Major depression, a serious psychiatric disorder affecting ~16% of the general population,6 is a known risk factor for vascular diseases such as coronary heart disease and myocardial infarction.7, 8 It's worth noting that a number of researches including prospective studies have investigated the associations between depressive disorder and the occurrence of stroke, but they have yielded mixed results. For example, a recent large cohort study with 80 574 participants showed an increased stroke risk in women with a previous diagnosis of depression,9 but other several studies found no evidence of depression being a significant risk factor for cerebrovascular diseases10, 11 or showed an increased stroke risk only in persons younger than 65 years old.12 These conflicting findings from the existing studies may be due to a limited sample size, a short follow-up duration or the use of self-reported symptom scales rather than diagnostic instruments to assess depressive disorder.11–13 Moreover, the relationship between depression and stroke may differ in different countries and races, because of divergent medical, behavioral, or social responses to depressive disorder or differential prevalence of other cardiovascular risk factors.
Thus, we conducted a prospective study with a relatively rigorous design to investigate the relationship between major depressive episodes (MDE) and incidences of stroke and further examine the potential dose-response effect of depression symptoms on stroke risk in a large cohort-the China Kadoorie Biobank of 0.5 million people enrolled from 10 geographically defined regions of China.
Methods
Study population
Detailed information about the China Kadoorie Biobank cohort design, methods, participants and follow-up have been described previously.14 Briefly, a total of 512 891 adults aged 30-79 years were enrolled into the cohort during 2004-08 from 10 diverse urban and rural areas in China and followed up ever since for cause-specific mortality as well as any episode of hospitalization, using routine mortality and health insurance data. In 10 study areas, the baseline survey was carried out by a Regional Coordinating Centre (RCC) and survey team, consisting of about 15 full-time staff with medical qualifications and fieldwork experience. Before the start of survey, all the staff underwent training including questioning technique, uniform methods of physical examination, standardized survey process, etc. At baseline, all the participants were face-to-face interviewed by trained staff using a standardized laptop-based questionnaire to collect detailed information, including demographic characteristics, socioeconomic status, medical history, personal behavior (e.g., smoking, alcohol and tea drinking), diet, physical activity and for women only, reproductive history. After the interview, a range of physical measurements were undertaken for each participant and a 10-ml blood sample was collected. All individuals provided written informed consent before the participation.
For the present study, participants who had a recorded implausible censoring date for loss to follow-up (n=1), or reported a prior history of stroke (n=8884), heart disease (n=15 472) and cancer (n=2577) at baseline were excluded, remaining a population of 487 377 individuals (men=199 294; women=288 083) eligible for analysis of the association between MDE and risk of stroke.
Our study was approved by the Ethics Review Committee of the Chinese Center for Disease Control and Prevention, Beijing, China, and the Oxford Tropical Research Ethics Committee, University of Oxford, Oxford, UK.
Assessment of major depressive episodes
Past year MDE at baseline was defined using the Chinese version of computerized Composite International Diagnostic Inventory -Short form,15 which produces similar population estimates of major depression to the Structured Clinical Interview for DSM (SCID).16, 17 Compared with the full Composite International Diagnostic Interview, the MDE diagnoses using short form have shown sensitivity of 89.6%, specificity of 93.9% and overall classification accuracy of 93.2%.15 Subjects were defined as having past year MDE if they had felt sad, blue, or depressed for 2 weeks or more during the past 12 months, and if they had at least three of seven additional symptoms including loss of interest and pleasure, loss of energy or fatigue, weight change, sleep problems, concentration problems, feelings of worthlessness, and thoughts of suicide.18
Ascertainment of stroke
Each participant’s vital status was ascertained through China’s Disease Surveillance Point death registries19 and residential records. Causes of death from official death certificates were supplemented, if necessary, by a review of medical records. Linkage to national and local health insurance (HI) databases also helped to improve the accuracy of diagnosis and classification of reported conditions, outcome adjudication, and further data collection. Additionally, participants who were not included in the HI system were followed annually by dedicated staff members to ascertain their status including disease development, hospital admission, death and migration.
Stroke was defined as a focal neurological deficit of sudden or rapid onset lasting ≥24 hours or until death, confirmed by computed tomography (CT) or magnetic resonance imaging (MRI). According to the International Classification of Diseases, 10th edition (ICD-10), strokes were coded as I60 (subarachnoid stroke), I61 (haemorrhagic stroke), I63 (ischaemic stroke) and I64 (other or unknown stroke type) by trained staff blinded to the baseline information. Stroke cases were further confirmed by a professional team consisting of 23 neurologists who received strict training including the recognition of CT/MRI imaging, application of uniform diagnostic criteria and standardized verification process.
Assessment of variables
Demographic and socioeconomic characteristics including age, sex, region (rural or urban), marital status (married, widowed, separated/divorced, or never married), education level (no formal school, primary school, middle school, high school, college, or university and above) and annual household income (<20 000 Yuan or ≥20 000 Yuan) were collected at the baseline interview. Lifestyle factors included self-reported smoking status (never smoker, occasional smoker, ex-smoker, or current regular smoker), alcohol use (non-drinker, occasional drinker, ex-drinker, or current regular drinker) and total physical activity calculated as metabolic equivalent task hours (MET-hours/day) spent on work, transportation, housework, non-sedentary recreation and sedentary leisure. In addition, all participants were asked to report personal medical history, including hypertension, diabetes, chronic hepatitis or cirrhosis, peptic ulcer, etc.
At baseline, weight, height and blood pressure were measured using standard instruments and protocols by trained staff. Body mass index (BMI) was calculated as weight in kilograms divided by the height in meters squared. Prevalent hypertension was defined as measured systolic blood pressure ≥140 mmHg, measured diastolic blood pressure ≥90 mmHg, self-reported diagnosis of hypertension, or self-reported use of antihypertensive medication at baseline. Prevalent diabetes was defined as measured fasting blood glucose ≥7.0 mmol/L, measured random blood glucose ≥11.1 mmol/L, or self-reported diagnosis of diabetes.
Statistical analysis
Person-years were measured from baseline (2004-08) until the date of stroke diagnosis, death of any other cause, or December 31, 2013, whichever occurred first. Comparisons between respondents with different baseline depression status were conducted using Student’s T-test for continuous variables and Chi-squared test for categorical variables. Multivariate Cox proportional hazard regression analyses were then performed to estimate the relationship between MDE and stroke risk. Besides, stratification analysis was conducted to investigate the association in different subgroups and the Chi-square-based Q test was used to test the heterogeneity. Interaction analysis was further carried out between MDE and selected exposures collected in the study. Data analyses were carried out by R software (Version 3.0.2, 2013-09-25; R Foundation for Statistical Computing, http://www.cran.r-project.org/). The significance level was set at P < 0.05 and P values were given for two-sided tests.
Results
Baseline characteristics of the study population stratified by depression status are summarized in Table 1. Individuals with past year MDE were more likely to be younger, female, rural residents and solitary (widowed, separated/divorced, or never married), and have lower education, household income and BMI, but less likely to be physically active, current regular smokers and drinkers, compared with those without a history of depression. Besides, the prevalence of diabetes was higher in depressed people, whereas hypertension was more prevalent in those without MDE. In addition, the associations between baseline characteristics and stroke risk were displayed in supplementary file Table I in the (online-only Data Supplement, http://stroke.ahajournals.org).
Table 1. Baseline characteristics of the study population according to baseline depression status.
| Characteristic | All subjects | MDE |
P | |
|---|---|---|---|---|
| No | Yes | |||
| No. of participants (%) | 487 377 (100.0) | 484 389 (99.4) | 2988 (0.6) | |
| Mean age (yr) | 51.0 | 51.1 | 50.4 | <0.001 |
| Male, n (%) | 199 294 (40.9) | 198 456 (41.0) | 838 (28.1) | <0.001 |
| Rural area, n (%) | 277 236 (56.9) | 275 254 (56.8) | 1982 (66.3) | <0.001 |
| Currently married, n (%) | 442 943 (90.9) | 440 714 (91.0) | 2229 (74.6) | <0.001 |
| Middle school and above, n (%) | 239 676 (49.2) | 238 401 (49.2) | 1275 (42.7) | <0.001 |
| Household income ≥20 000 Yuan/year, n (%) | 208 490 (42.8) | 207 569 (42.9) | 921 (30.8) | <0.001 |
| Mean BMI (kg/m2) | 23.6 | 23.6 | 23.1 | <0.001 |
| Diabetes, n (%) | 26 162 (5.4) | 25 975 (5.4) | 187 (6.3) | 0.030 |
| Hypertension, n (%) | 240 201 (49.3) | 238 845 (49.3) | 1356 (45.4) | <0.001 |
| Current regular smoker, n (%) | 130 371 (26.8) | 129 731 (26.8) | 640 (21.4) | <0.001 |
| Current regular drinker, n (%) | 73 644 (15.1) | 73 344 (15.1) | 300 (10.0) | <0.001 |
| Mean physical activity (MET-hr/day) | 21.6 | 21.6 | 20.7 | 0.002 |
MDE indicates major depressive episodes; BMI, body mass index; and MET, metabolic equivalent of task.
During 3 429 808 person-years of follow-up between 2004 and 2013 (median, 7.2 years), a total of 27 623 (5.67%) first-ever strokes occurred [5255 hemorrhagic (subarachnoid or intracerebral), 21 427 ischemic and 941 unknown type of strokes]. As shown in Table 2, past year MDE was marginally associated with a 15% increased risk of stroke with adjustment of age, sex, marital status, household income, education, region, smoking status, alcohol consumption, physical activity, BMI, history of hypertension and history of diabetes [adjusted hazard ratio (HR) = 1.15, 95% confidence intervals (95% CI) = 0.99-1.33]. Furthermore, analysis was also conducted to evaluate the cumulative effect of the seven depression symptoms on stroke occurrence. Intriguingly, we found a significantly positive dose-response association between the number of symptoms and stroke risk (Ptrend = 0.011). Compared with individuals having “0-2” depression symptoms, those with more symptoms had higher risk of stroke, especially for the group with “6” and “7” symptoms [adjusted HRs of 1.33 (1.01-1.74) and 1.47 (1.04-2.08), respectively].
Table 2. Hazard ratio (95% confidence intervals) of incident stroke according to baseline depression status and numbers of depression symptoms.
| Variables | No. of subjects | PYs of follow-up | Incident strokes | Incidence rate (per 1000 PYs) | Model 1 | Model 2 |
|---|---|---|---|---|---|---|
| MDE | ||||||
| No | 484 389 | 3 407 861 | 27 440 | 8.05 | 1.00 | 1.00 |
| Yes | 2988 | 21 947 | 183 | 8.34 | 1.14 (0.98-1.31) | 1.15 (0.99-1.33) |
| No. of depression symptoms | ||||||
| 0-2 | 484 389 | 3 407 861 | 27 440 | 8.05 | 1.00 | 1.00 |
| 3 | 475 | 3471 | 25 | 7.20 | 0.92 (0.62-1.36) | 0.99 (0.67-1.47) |
| 4 | 603 | 4424 | 32 | 7.23 | 0.97 (0.69-1.38) | 1.01 (0.71-1.43) |
| 5 | 741 | 5490 | 41 | 7.47 | 1.01 (0.75-1.37) | 1.01 (0.74-1.37) |
| 6 | 719 | 5251 | 53 | 10.09 | 1.37 (1.05-1.79) | 1.33 (1.01-1.74) |
| 7 | 450 | 3311 | 32 | 9.66 | 1.47 (1.04-2.08) | 1.47 (1.04-2.08) |
| P for trend | 0.010 | 0.011 |
Model 1: Adjusted for age and sex.
Model 2: Model 1 plus adjustment for marital status, household income, education, region, smoking status, alcohol consumption, physical activity, BMI, history of hypertension and history of diabetes.
MDE indicates major depressive episodes; and PYs indicates person-years.
The stratification analysis for the association between MDE and incident stroke was then conducted by all aforementioned variables. In supplementary analyses (Table II in the online-only Data Supplement, http://stroke.ahajournals.org), steeper and statistically significant associations were observed in individuals aged <50 years (adjusted HR, 1.54; 95% CI, 1.16-2.03), smokers (adjusted HR, 1.51; 95% CI, 1.16-1.98), drinkers (adjusted HR, 1.62; 95% CI, 1.08-2.41), those with higher education degree (adjusted HR, 1.38; 95% CI, 1.10-1.73), BMI <24.0 kg/m2 (adjusted HR, 1.23; 95% CI, 1.02-1.49) and no history of diabetes (adjusted HR, 1.18; 95% CI, 1.02-1.38). However, heterogeneity in every two strata was significant only for age (P = 0.003), education (P = 0.047) and smoking status (P = 0.024). Furthermore, stratification analysis by different stroke subtypes was also performed, but the association with stroke incidence was not statistically significant for either hemorrhagic stroke or ischemic stroke.
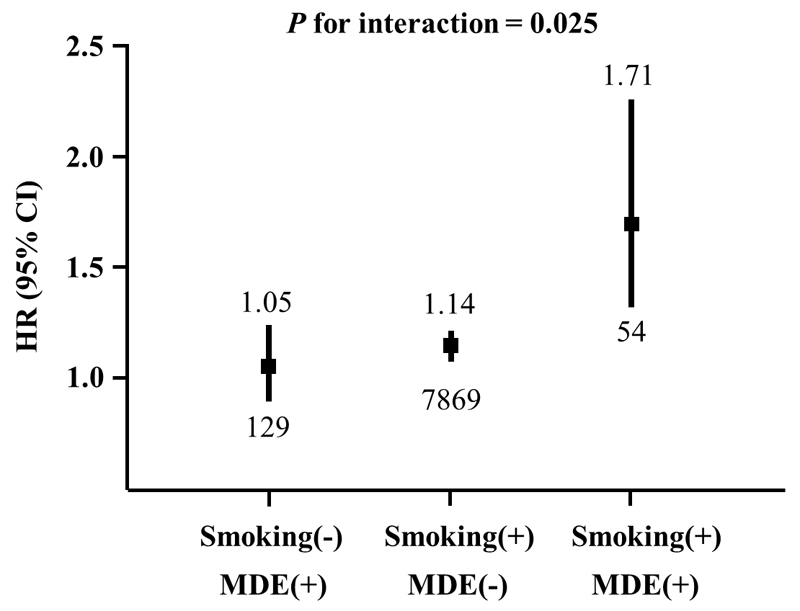
Then, a statistically significant multiplicative interaction between MDE and smoking status on stroke risk was identified (Figure 1, P for interaction = 0.025). Compared with nonsmokers with no prior depression, current smokers with MDE had a 1.71-fold increased risk of stroke (adjusted HR = 1.71, 95% CI = 1.31-2.24, P < 0.001) after adjusting for age, sex, marital status, household income, education, region, alcohol consumption, physical activity, BMI, history of hypertension and history of diabetes.
Figure 1. Interaction analysis between smoking status and baseline depression status.
Adjusted for age, sex, marital status, household income, education, region, alcohol consumption, physical activity, BMI, history of hypertension and history of diabetes. MDE, major depressive episodes. “Smoking(-) & MDE(-)” was used as the reference group. Squares represent the hazard ratios (HR) and vertical lines represent the corresponding 95% confidence intervals (95% CI). Numbers above the CIs are the HRs and numbers below the CIs represent participants with stroke events.
Discussion
In the present study, we found past year MDE was marginally associated with an increased risk of stroke, independently of potential confounders. A positive dose-response association was also observed between the number of depression symptoms and stroke risk. Additionally, smoking status significantly interacted with MDE on stroke occurrence.
A variety of prospective studies have assessed the association between depression and stroke incidence, suggesting that depression could be a modifiable risk factor for stroke;20 however, few researches have examined such relationship in Chinese population. Our finding showed a marginally positive association between MDE and stroke incidence and a positive dose-response relationship between the number of depression symptoms and increased stroke risk, which were consistent with results from several previous studies.9, 13, 20–22 For example, Larson et al.21 reported the prior depressive disorder was associated with a 2.6-fold increased risk of stroke during a 13-year follow-up and Jackson et al.22 found a 1.9 times elevated risk of incident stroke associated with depression during a 12-year follow-up. Additionally, some studies have already evaluated the effect of single specific symptom of depression on stroke occurrence.13, 23, 24 Liebetrau et al.13 found that both of depressed mood and loss of interest or pleasure were related to an increased incidence of stroke among 401 Swedes. Glymour et al.23 demonstrated that endorsement of any individual depressive symptom could predict subsequent stroke risk among 14 778 American whites. Since the number of symptoms is the reflection of the disease severity, it is reasonable that the risk of stroke could increase with the severity of depression in this study.
The association between depression and first-ever stroke may have several explanations. Firstly, depression has been found to be associated with cardiac arrhythmia,25 enhanced insulin resistance,26 more white matter lesions,27 and increased levels of platelet activation,28 fibrinogen29 and C-reactive protein,30 all of which might influence stroke risk. Secondly, depression could affect the occurrence of stroke by acting on risk factors related to health, including low physical activity,31 smoking,32, 33 heavy drinking,31 obesity,34 and certain comorbidities.35 Nevertheless, when adjusting for baseline measures of smoking status, alcohol consumption, physical activity, BMI, hypertension and diabetes, the effects of MDE on stroke incidence remained stable in the present study, indicating the effect of depression on stroke risk was independent of these factors. Finally, it is really hard for patients with depressive disorder to follow prescribed medical regimens,36 including antihypertensive drugs and lipid-lowering medications, which may be another explanation for the elevated stroke risk. Thus, specific mechanisms for the association between depression and incident stroke still need to be further explored.
Besides, it was worth mentioning that, in the stratification analysis, we found the significant association between MDE and stroke onset only existed in subjects younger than 50 years old but not in the elderly, similar with the findings in two previous studies.12, 37 The Framingham Study suggested the antecedent depression was associated with a 3-fold increased risk of stroke in participants aged <65 years but not in those aged ≥65 years.12 Likewise, another study showed an elevated stroke risk with depression in individuals aged 55 to 64 years but not in those 65 years old and above.37 Some reasons may explain this result. On one hand, older people with depression have a considerably higher mortality,38, 39 which could interfere with stroke occurrence through preventing its change into an observable event, thus altering the risk of stroke linked to depressive disorder. On the other hand, younger depressed individuals usually have greater life pressure and more daily hassles, which might increase stroke risk by aggravating the neuroendocrine effect of depression.40 Meanwhile, our results provided statistical evidence on multiplicative interactions between baseline MDE and smoking status in relation to stroke risk. Both depressive disorder and tobacco smoking have been identified to independently increase the risk of stroke in the literature41, 42 as well as in the present study. Additionally, increasing evidence has suggested that cigarette use may cause or worsen depressive symptoms,43, 44 whereas the presence of depression could also increase the risk of daily smoking in some earlier reports.32, 33 Taking together, these results suggested the effect of the two risk factors on stroke onset could be modified by each other, although the exact biological mechanism is unclear. Further studies with large samples and functional investigations may lead to important insights for such interactions.
The strengths of our study include its prospective design, markedly large sample size, long duration of follow-up, complete endpoint-data, and careful control of several confounding factors. However, some limitations should be considered. First of all, the relatively low prevalence of MDE at baseline could limit the capacity of the current study to detect associations between the depression and stroke risk. The potential bias arising from a 1-year period of retrospective recall for the MDE may provide an alternative explanation for the low prevalence. Another reason may be that the participants in this study usually have better mental health relative to general people. To more generally investigate the association between depression and stroke risk, we also compared the participants with negative emotions (feeling sad, blue or depressed, feeling useless, feeling exhausted or even numb, or losing interest in most things, n=13 601), instead of MDE (n=2988), with those who were not depressed at baseline, and a significantly positive association was observed between past year depression and stroke incidence (adjusted HR = 1.15, 95% CI = 1.07-1.24). Secondly, participants with minor stroke episodes may not be hospitalized and therefore not reported in the HI system, which could lead to the bias. Thirdly, some mental factors may potentially modify the real effect of depressive disorder on stroke risk in this study. However, further adjusting for prior history of psychiatric disorders or neurasthenia at baseline did not obviously change the hazard of incident stroke with adjusted HR of 1.14 (0.99-1.32). Finally, we assessed MDE only at the time of the baseline survey and did not track the progression of the disorder, which might also affect the association of MDE with stroke risk.
Conclusions
In summary, our study showed a marginally positive association between past year MDE and stroke incidence, which could be modified by smoking status. Besides, there was a significant dose-response relationship between the number of depression symptoms and increased stroke risk. Further prospective studies in diverse populations are warranted to validate the results and enhance the generalizability of these findings.
Supplementary Material
Acknowledgments
We gratefully thank the participants, project staff, and China National Center for Disease Control and Prevention (CDC) and its regional offices for access to death and disease registries. The Chinese National Health Insurance scheme provides electronic linkage to all hospital treatment.
Sources of Funding
This work was supported by grant from the National Natural Science Foundation of China (81390543 and 81202266). The CKB baseline survey and the first re-survey were supported by a grant from the Kadoorie Charitable Foundation in Hong Kong. The long-term follow-up is supported by grants from the UK Wellcome Trust (088158/Z/09/Z and 104085/Z/14/Z) and a grant from the Chinese Ministry of Science and Technology (2011BAI09B01). The funders had no role in the study design, data collection, data analysis and interpretation, writing of the report, or the decision to submit the article for publication.
Footnotes
Disclosures
None.
References
- 1.Donnan GA, Fisher M, Macleod M, Davis SM. Stroke. Lancet. 2008;371:1612–1623. doi: 10.1016/S0140-6736(08)60694-7. [DOI] [PubMed] [Google Scholar]
- 2.Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao D, Liu J, Wang W, Zeng Z, Cheng J, Sun J, et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONICA-Beijing Project. Stroke. 2008;39:1668–1674. doi: 10.1161/STROKEAHA.107.502807. [DOI] [PubMed] [Google Scholar]
- 4.Liu M, Wu B, Wang WZ, Lee LM, Zhang SH, Kong LZ. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6:456–464. doi: 10.1016/S1474-4422(07)70004-2. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 7.Rugulies R. Depression as a predictor for coronary heart disease. a review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 8.Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22:613–626. doi: 10.1002/gps.1723. [DOI] [PubMed] [Google Scholar]
- 9.Pan A, Okereke OI, Sun Q, Logroscino G, Manson JE, Willett WC, et al. Depression and incident stroke in women. Stroke. 2011;42:2770–2775. doi: 10.1161/STROKEAHA.111.617043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nabi H, Kivimaki M, Suominen S, Koskenvuo M, Singh-Manoux A, Vahtera J. Does depression predict coronary heart disease and cerebrovascular disease equally well? The Health and Social Support Prospective Cohort Study. Int J Epidemiol. 2010;39:1016–1024. doi: 10.1093/ije/dyq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Surtees PG, Wainwright NW, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Psychological distress, major depressive disorder, and risk of stroke. Neurology. 2008;70:788–794. doi: 10.1212/01.wnl.0000304109.18563.81. [DOI] [PubMed] [Google Scholar]
- 12.Salaycik KJ, Kelly-Hayes M, Beiser A, Nguyen AH, Brady SM, Kase CS, et al. Depressive symptoms and risk of stroke: the Framingham Study. Stroke. 2007;38:16–21. doi: 10.1161/01.STR.0000251695.39877.ca. [DOI] [PubMed] [Google Scholar]
- 13.Liebetrau M, Steen B, Skoog I. Depression as a risk factor for the incidence of first-ever stroke in 85-year-olds. Stroke. 2008;39:1960–1965. doi: 10.1161/STROKEAHA.107.490797. [DOI] [PubMed] [Google Scholar]
- 14.Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40:1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Andrews G, Mroczek DK, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview short-form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7:171–185. [Google Scholar]
- 16.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13:122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mezuk B, Chen Y, Yu C, Guo Y, Bian Z, Collins R, et al. Depression, anxiety, and prevalent diabetes in the Chinese population: findings from the China Kadoorie Biobank of 0.5 million people. J Psychosom Res. 2013;75:511–517. doi: 10.1016/j.jpsychores.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang GH, Stroup DF, Thacker SB. National public health surveillance in China: implications for public health in China and the United States. Biomed Environ Sci. 1997;10:1–13. [PubMed] [Google Scholar]
- 20.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306:1241–1249. doi: 10.1001/jama.2011.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larson SL, Owens PL, Ford D, Eaton W. Depressive disorder, dysthymia, and risk of stroke: thirteen-year follow-up from the Baltimore epidemiologic catchment area study. Stroke. 2001;32:1979–1983. doi: 10.1161/hs0901.094623. [DOI] [PubMed] [Google Scholar]
- 22.Jackson CA, Mishra GD. Depression and risk of stroke in midaged women: a prospective longitudinal study. Stroke. 2013;44:1555–1560. doi: 10.1161/STROKEAHA.113.001147. [DOI] [PubMed] [Google Scholar]
- 23.Glymour MM, Yen JJ, Kosheleva A, Moon JR, Capistrant BD, Patton KK. Elevated depressive symptoms and incident stroke in Hispanic, African-American, and White older Americans. J Behav Med. 2012;35:211–220. doi: 10.1007/s10865-011-9356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Glymour MM, Maselko J, Gilman SE, Patton KK, Avendano M. Depressive symptoms predict incident stroke independently of memory impairments. Neurology. 2010;75:2063–2070. doi: 10.1212/WNL.0b013e318200d70e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 26.Okamura F, Tashiro A, Utumi A, Imai T, Suchi T, Tamura D, et al. Insulin resistance in patients with depression and its changes during the clinical course of depression: minimal model analysis. Metabolism. 2000;49:1255–1260. doi: 10.1053/meta.2000.9515. [DOI] [PubMed] [Google Scholar]
- 27.Vermeer SE, Hollander M, van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MM. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke. 2003;34:1126–1129. doi: 10.1161/01.STR.0000068408.82115.D2. [DOI] [PubMed] [Google Scholar]
- 28.Musselman DL, Tomer A, Manatunga AK, Knight BT, Porter MR, Kasey S, et al. Exaggerated platelet reactivity in major depression. Am J Psychiatry. 1996;153:1313–1317. doi: 10.1176/ajp.153.10.1313. [DOI] [PubMed] [Google Scholar]
- 29.Kop WJ, Gottdiener JS, Tangen CM, Fried LP, McBurnie MA, Walston J, et al. Inflammation and coagulation factors in persons > 65 years of age with symptoms of depression but without evidence of myocardial ischemia. Am J Cardiol. 2002;89:419–424. doi: 10.1016/s0002-9149(01)02264-0. [DOI] [PubMed] [Google Scholar]
- 30.Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 31.Strine TW, Mokdad AH, Dube SR, Balluz LS, Gonzalez O, Berry JT, et al. The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen Hosp Psychiatry. 2008;30:127–137. doi: 10.1016/j.genhosppsych.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 32.Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P. Major depression and stages of smoking. A longitudinal investigation. Arch Gen Psychiatry. 1998;55:161–166. doi: 10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- 33.Diwan A, Castine M, Pomerleau CS, Meador-Woodruff JH, Dalack GW. Differential prevalence of cigarette smoking in patients with schizophrenic vs mood disorders. Schizophr Res. 1998;33:113–118. doi: 10.1016/s0920-9964(98)00045-0. [DOI] [PubMed] [Google Scholar]
- 34.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 35.Huang CQ, Zhang XM, Dong BR, Lu ZC, Yue JR, Liu QX. Health status and risk for depression among the elderly: a meta-analysis of published literature. Age Ageing. 2010;39:23–30. doi: 10.1093/ageing/afp187. [DOI] [PubMed] [Google Scholar]
- 36.Grenard JL, Munjas BA, Adams JL, Suttorp M, Maglione M, McGlynn EA, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med. 2011;26:1175–1182. doi: 10.1007/s11606-011-1704-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seifert CL, Poppert H, Sander D, Feurer R, Etgen T, Ander KH, et al. Depressive symptoms and the risk of ischemic stroke in the elderly--influence of age and sex. PLoS One. 2012;7:e50803. doi: 10.1371/journal.pone.0050803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baxter AJ, Page A, Whiteford HA. Factors influencing risk of premature mortality in community cases of depression: a meta-analytic review. Epidemiology Research International. 2011;2011:1–12. [Google Scholar]
- 39.Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Biol Psychiatry. 2002;52:205–225. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- 40.Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55:580–592. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- 41.Albertsen IE, Overvad TF, Lip GY, Larsen TB. Smoking, atrial fibrillation, and ischemic stroke: a confluence of epidemics. Curr Opin Cardiol. 2015;30:512–517. doi: 10.1097/HCO.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 42.Pikija S, Trkulja V, Malojcic B, Mutzenbach JS, Sellner J. A high burden of ischemic stroke in regions of Eastern/Central Europe is largely due to modifiable risk factors. Curr Neurovasc Res. 2015;12:341–352. doi: 10.2174/1567202612666150731105554. [DOI] [PubMed] [Google Scholar]
- 43.Edwards AC, Kendler KS. A twin study of depression and nicotine dependence: shared liability or causal relationship? J Affect Disord. 2012;142:90–97. doi: 10.1016/j.jad.2012.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Menezes AM, Murray J, Laszlo M, Wehrmeister FC, Hallal PC, Goncalves H, et al. Happiness and depression in adolescence after maternal smoking during pregnancy: birth cohort study. PLoS One. 2013;8:e80370. doi: 10.1371/journal.pone.0080370. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.