Abstract
Objectives
Some patients with deliberate drug poisoning subsequently have an adverse clinical course. The present study aimed to examine whether the type of drugs ingested and psychiatric diagnoses were related to an adverse clinical course.
Methods
We conducted a cohort study of patients with deliberate drug poisoning admitted to the intensive care unit of a university hospital located in Tokyo, Japan, between September 2006 and June 2013. Intensive care unit (ICU) stay of ≥4 days was used as a primary outcome measure, while the incidence of aspiration pneumonitis was used as a secondary outcome measure. Ingested substances and psychiatric diagnoses were used as explanatory variables.
Results
Of the 676 patients with deliberate drug poisoning, 88% had a history of psychiatric treatment and 82% had ingested psychotropic drugs. Chlorpromazine-promethazine-phenobarbital combination drug (Vegetamin®) ranked fifth among the most frequently ingested substances in cases of deliberate drug poisoning and had the highest incidence of prolonged ICU stay (20%) and aspiration pneumonitis (29%). The top three major classes consisted of benzodiazepines (79%), new-generation antidepressants (25%), and barbiturates/non-barbiturates (23%). Barbiturate overdose was independently associated with increased odds of both prolonged ICU stay (8% vs. 17%; odds ratio [OR], 2.97; 95% confidence interval [CI], 1.60–5.55) and aspiration pneumonitis (8% vs. 24%; OR, 3.83; 95% CI, 2.18–6.79) relative to those associated with overdose of only other sedative-hypnotics (i.e., benzodiazepines).
Conclusion
These results suggest that judicious prescribing of barbiturates by psychiatrists could reduce the risk of an adverse clinical course when a patient attempts an overdose.
Introduction
Drug poisoning is a worldwide public health concern and places a serious burden on emergency medical service. In Western countries, the annual incidence of drug poisoning has been estimated at 142–232 per 100,000 inhabitants [1–3] and drug poisoning accounts for 0.3%–0.6% of all patients admitted to emergency departments [4, 5]. Deliberate drug poisoning is responsible for 60%–78% of all drug poisoning and is a more common cause of admission than accidental drug poisoning [6, 7].
A non-negligible subgroup of patients with deliberate drug poisoning may show an adverse clinical course such as aspiration pneumonia [8, 9], respiratory failure [10], hypothermia [9], and cardiovascular events [11], although almost all (99%) patients survive their hospital stay [12–14]. Aspiration pneumonia is the most common adverse event among patients with deliberate drug poisoning [8] and doubles the length of intensive care unit (ICU) stay owing to physical recovery from the overdose-related complications [10]. Indeed, 27%–28% of patients develop aspiration pneumonia [10, 15]. In addition, 35% of patients are hospitalized for more than 3 days in acute care hospitals [16], although these patients are generally discharged from the ICU within only 16–32 hours of admission [4, 10].
Several factors contribute to an adverse clinical course among patients with drug poisoning. For example, demographic characteristics (i.e., sex [17, 18] and age [18]), clinical characteristics (i.e., blood pressure [10, 19, 20], renal function [10], and level of consciousness [15, 19, 21]), and characteristics of the drugs ingested (dosage [20] and type [15]) are important contributing factors in adverse clinical courses among patients with drug poisoning. The dose and type of ingested drugs are particularly preventable factors associated with a severe adverse clinical course among patients with deliberate drug poisoning [22].
Although few studies have explored the associations between adverse clinical courses and ingested drugs in patients with deliberate drug overdose [15, 23–26], some specific drugs might increase the risk of an adverse clinical course. Tricyclic antidepressant poisoning leads to arrhythmia and an increased rate of mortality [23]. Barbiturate poisoning leads to respiratory depression and an increased rate of mortality [15, 24, 25]. However, these studies had several limitations. First, the specific types of drugs ingested were the focus in each of these studies and outcomes were not compared with those of other drugs. Second, some patients in these studies attempted both self-poisoning and self-cutting, which might have confounded the relationship between the type of drugs ingested and the subsequent adverse clinical course. Finally, participants were limited to patients referred to psychiatry departments [15, 23], indicating a probable selection bias. Few studies are available on the relationship between psychiatric diagnoses and adverse clinical courses, although psychiatric diagnoses may be related to the type and dose of the drugs ingested.
Therefore, in this study, we aimed to compare the incidences of aspiration pneumonia and prolonged ICU stay by the class of drugs ingested and the psychiatric diagnoses of the patients.
Materials and Methods
Design and setting
We conducted a cohort study of inpatients who presented with deliberate self-harm. Patients were consecutively recruited from the ICU of the Tokyo Medical and Dental University in Tokyo, Japan. The unit provides tertiary emergency service that treats 10,000 to 15,000 patients annually. Since 2006, both physicians and psychiatrists in the unit have routinely assessed clinical information for all patients who survived self-harm episodes by using a standard data extraction form. In the present study, we included patients who (1) were admitted to the unit between September 11, 2006 and June 21, 2013; (2) attempted overdose as a single method for deliberate self-harm; and (3) had complete information on the ingested substances. The present study was reviewed and approved by the institutional review board at the Tokyo Medical and Dental University (1604). Because patient data were routinely collected, the review board waived the requirement for informed consent.
Outcomes
The incidence of prolonged ICU stay (≥4 days) was used as the primary outcome. We selected this threshold value because 90% of patients were discharged from the ICU within 3 days in our data. In addition, patients are more likely to be discharged from the ICU within 3 days rather than within 4 days because the per-day fee for admission among patients with an ICU stay of 4–7 days is 10% lower than that for a stay of 1–3 days. Indeed, the difference in the cumulative proportion of ICU stay peaked at 44% between day 1 (30%) to day 2 (77%), followed by 13% between day 2 (77%) and day 3 (90%), dropped to 4% between day 3 (90%) and day 4 (94%), and remained at 3% between day 4 (94%) and day 5 (97%).
The incidence of aspiration pneumonitis during the ICU stay was used as the secondary outcome. Patients presenting with clinical signs of pneumonia (e.g., fever ≥37.5°C, leukocytosis, and elevated C-reactive protein level) routinely undergo chest radiography and, if necessary, undergo chest computed tomography scan. Physicians in the ICU generally suspect the presence of aspiration pneumonitis on the basis of an episode of aspiration, the presence of predisposing conditions (e.g., neurological disorders, coma, and gastroesophageal reflux disease), chest radiography findings, and results of sputum culture. In this study, no distinction was made between aspiration pneumonitis and aspiration pneumonia [27].
Primary explanatory variables
Substances that led to ICU admissions and psychiatric diagnoses were used as primary explanatory variables. Each substance was assessed by the physicians based on information from the ambulance crews. Psychiatric diagnoses were assessed according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria by experienced psychiatrists.
Data analysis
First, we conducted univariate analyses to summarize the characteristics of the participants. Next, we selected the 20 most frequently ingested substances and major drug classes that lead to ICU admissions for overdose. Third, we identified major psychiatric diagnoses among patients with deliberate drug poisoning. Fourth, we estimated the odds ratios (ORs) and their 95% confidence intervals (CIs) for prolonged ICU stay and aspiration pneumonitis using logistic regression models. We sequentially introduced groups of variables into the model: first each primary explanatory variable, second age and sex, third psychiatric diagnoses, fourth drug classes ingested, and fifth alcohol intake during overdose. The primary explanatory variables were major drug classes and psychiatric diagnoses. The reference categories for sedative-hypnotics, antidepressants, and antipsychotics were as follows: only benzodiazepine receptor agonists or other sedative-hypnotics, only new-generation antidepressants or other antidepressants, and only second-generation antipsychotics, respectively. The reference group for mutually exclusive psychiatric diagnoses (adjustment disorders, bipolar disorders, major depressive disorders, and schizophrenia) was adjustment disorders. Finally, we performed a sensitivity analysis in which we used the prolonged length of stay as count data (i.e., days in the ICU) instead of binary data (i.e., ≥4 days or <4 days in the ICU). We estimated the incidence rate ratios (IRRs) and their 95% CIs for prolonged ICU stay using a quasi-Poisson model [28]. Significance levels were set at 5%. All data were analyzed using R version 3.2.2.
Results
Characteristics of the study participants
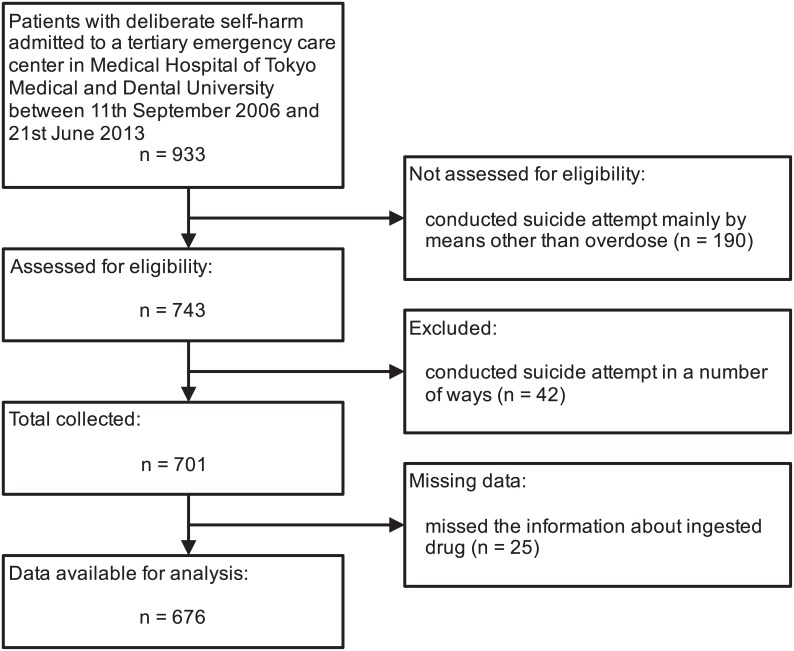
Of all the 933 patients who presented with self-harm, 676 patients that presented only with overdose were included in the analysis (see Fig 1). Characteristics of the study participants are listed in Table 1. Over 80% of patients with overdose were 20–49 years of age. The gender ratio (women: men) was 3.3:1. Among patients with overdose, 86% had a history of psychiatric treatment, 88% impulsively attempted overdose, and 60% attempted overdose with suicidal ideation.
Fig 1. Flow diagram for inclusion in the study.
Table 1. Characteristics of the study participants.
| Total (N = 676) | ||
|---|---|---|
| Characteristic | n | % |
| Age | ||
| ≤19 years | 38 | 5.6 |
| 20–34 years | 328 | 48.5 |
| 35–49 years | 227 | 33.6 |
| 50–64 years | 47 | 6.9 |
| ≥65 years | 36 | 5.3 |
| Gender | ||
| Men | 156 | 23.1 |
| Women | 520 | 76.9 |
| Living arrangement | ||
| Alone | 179 | 26.5 |
| With family | 494 | 73.1 |
| Unknown | 3 | 0.4 |
| History of psychiatric treatment | 581 | 87.6 |
| Reason for self-harm | ||
| Impulsive | 592 | 87.6 |
| Planned | 52 | 7.7 |
| Hallucination/delusion | 15 | 2.2 |
| Others | 7 | 1.0 |
| Unknown | 10 | 1.5 |
| Suicidal ideation | ||
| With | 403 | 59.9 |
| Without | 188 | 27.9 |
| Unknown | 82 | 12.2 |
| Drugs ingested | ||
| Psychotropic drug | 557 | 82.4 |
| Over-the-counter drug | 103 | 15.2 |
| Other drugs | 16 | 2.4 |
| Alcohol intake with overdose | 468 | 69.2 |
Major substance and drug classes for overdose
The top 20 substances that led to an overdose-related admission to the ICU are listed in Table 2. The top four substances were flunitrazepam, etizolam, brotizolam, and zolpidem, which are classified as benzodiazepine receptor agonists. Chlorpromazine-promethazine-phenobarbital combination drug (Vegetamin®) ranked as the fifth most common substance and had the highest incidence of prolonged ICU stay (20%) and aspiration pneumonitis (29%).
Table 2. The top 20 substances that led to ICU admission for overdose.
| Total (n = 676) | Incidence (%)a | |||
|---|---|---|---|---|
| Substance | n | % | Prolonged ICU stay | Aspiration pneumonitis |
| Total | 676 | 100.0 | 10.2 | 10.7 |
| 1. Flunitrazepam | 178 | 26.3 | 10.1 | 15.7 |
| 2. Etizolam | 121 | 17.9 | 8.3 | 10.7 |
| 3. Brotizolam | 113 | 16.7 | 9.7 | 12.4 |
| 4. Zolpidem | 105 | 15.5 | 8.6 | 11.4 |
| 5. Chlorpromazine-promethazine-phenobarbital | 104 | 15.4 | 20.2 | 28.8 |
| 6. Triazolam | 103 | 15.2 | 10.7 | 13.6 |
| 7. Bromazepam | 91 | 13.5 | 12.1 | 16.5 |
| 8. Alprazolam | 89 | 13.2 | 7.9 | 10.1 |
| 9. Valproate | 82 | 12.1 | 7.3 | 8.5 |
| 10. Nitrazepam | 71 | 10.5 | 9.9 | 16.9 |
| 11. Levomepromazine | 63 | 9.3 | 4.8 | 15.9 |
| 12. Acetaminophen | 61 | 9.0 | 11.5 | 0.0 |
| 13. Paroxetine | 59 | 8.7 | 13.6 | 15.3 |
| 14. Fluvoxamine | 58 | 8.6 | 12.1 | 17.2 |
| 15. Lorazepam | 48 | 7.1 | 8.3 | 16.7 |
| 16. Risperidone | 48 | 7.1 | 4.2 | 4.2 |
| 17. Diazepam | 43 | 6.4 | 7.0 | 11.6 |
| 18. Estazolam | 43 | 6.4 | 14.0 | 18.6 |
| 19. Chlorpromazine | 41 | 6.1 | 14.6 | 17.1 |
| 20. Clonazepam | 41 | 6.1 | 7.3 | 7.3 |
a The denominator was the number of patients who ingested a substance and the numerator was the number of incident cases among the patients.
ICU = intensive care unit
The major drug classes that led to ICU admission for overdose are listed in Table 3. The top three major classes consisted of benzodiazepines (79%), new-generation antidepressants (25%), and barbiturates/non-barbiturates (23%). Among these major drug classes, barbiturates/non-barbiturates had the highest incidence of prolonged ICU stay (17%) and aspiration pneumonitis (24%).
Table 3. Major classes of overdose.
| Total (n = 676) | Incidence (%)a | |||
|---|---|---|---|---|
| Class | n | % | Prolonged ICU stay | Aspiration pneumonitis |
| Total | 676 | 10.2 | 10.7 | |
| 1. Benzodiazepine receptor agonists | 537 | 79.4 | 9.7 | 11.5 |
| 2. New-generation antidepressants | 169 | 25.0 | 9.5 | 11.8 |
| 3. Barbiturates/non-barbiturates | 155 | 22.9 | 17.4 | 23.9 |
| 4. First-generation antipsychotics | 148 | 21.9 | 10.1 | 13.5 |
| 5. Pain killers | 135 | 20.0 | 7.4 | 3.7 |
| 6. Second-generation antipsychotics | 131 | 19.4 | 9.2 | 13.0 |
| 7. Mood stabilizers | 117 | 17.3 | 7.7 | 9.4 |
| 8. Other classes | 116 | 17.2 | 5.2 | 3.4 |
| 9. Drugs affecting the gut | 77 | 11.4 | 7.8 | 11.7 |
| 10. Tricyclic antidepressants | 72 | 10.7 | 9.7 | 18.1 |
| 11. Antiparkinson drugs | 71 | 10.5 | 14.1 | 22.5 |
| 12. Other antidepressants | 63 | 9.3 | 12.7 | 11.1 |
| 13. Antiallergic drugs | 31 | 4.6 | 16.1 | 3.2 |
| 14. Other sedatives and hypnotics | 32 | 4.7 | 15.6 | 6.3 |
| 15. Cardiovascular drugs | 19 | 2.8 | 15.8 | 5.3 |
| 16. Anticonvulsants | 4 | 0.6 | 25.0 | 0.0 |
a The denominator was the number of patients who ingested a substance and the numerator was the number of incident cases among the patients.
ICU = intensive care unit
Major psychiatric diagnoses
The major psychiatric diagnoses are listed in Table 4. The top three major diagnoses were major depressive disorders (26%), adjustment disorders (23%), and borderline personality disorder (21%). Amongst the major psychiatric diagnoses, borderline personality disorder had the highest incidence of prolonged ICU stay (28%) while alcohol use disorders had highest incidence of aspiration pneumonitis (31%).
Table 4. Psychiatric diagnoses.
| Total (n = 676) | Incidence (%)a | |||
|---|---|---|---|---|
| Diagnosis | n | % | Prolonged ICU stay | Aspiration pneumonitis |
| Total | 676 | 10.2 | 10.7 | |
| 1. Major depressive disorders | 174 | 25.7 | 13.8 | 10.3 |
| 2. Adjustment disorders | 157 | 23.2 | 7.0 | 7.0 |
| 3. Borderline personality disorders | 148 | 21.9 | 8.8 | 12.2 |
| 4. Schizophrenia | 72 | 10.7 | 16.7 | 18.1 |
| 5. Bipolar disorders | 59 | 8.7 | 6.8 | 13.6 |
| 6. Anxiety disorders | 56 | 8.3 | 5.4 | 10.7 |
| 7. Other personality disorders | 29 | 4.3 | 27.6 | 6.9 |
| 8. No psychiatric diagnoses | 17 | 2.5 | 11.8 | 0.0 |
| 9. Substance use disorders | 15 | 2.2 | 13.3 | 13.3 |
| 10. Alcohol use disorders | 13 | 1.9 | 15.4 | 30.8 |
| 11. Eating disorders | 9 | 1.3 | 0.0 | 11.1 |
| 12. Dementia | 6 | 0.9 | 16.7 | 16.7 |
a The denominator was the number of patients who have a psychiatric diagnosis and the numerator was the number of incident cases among the patients.
ICU = intensive care unit
Risk factors for adverse clinical courses
The adjusted ORs for prolonged ICU stay and aspiration pneumonitis are shown in Table 5. Barbiturate/non-barbiturate overdose was independently associated with increased odds for a prolonged ICU stay (OR: 2.97; 95% CI: 1.60, 5.55) and aspiration pneumonitis (OR: 3.83; 95% CI: 2.18, 6.79) relative to overdose with only other sedative-hypnotics (i.e., benzodiazepine overdose). These associations were not attenuated after adjustment for other risk factors (S1 and S2 Tables).
Table 5. Risk factors for adverse clinical course.
| Incidence (%)a | Odds ratio (95% confidence interval)b | ||||
|---|---|---|---|---|---|
| Characteristic | n | Prolonged ICU stay | Aspiration pneumonitis | Prolonged ICU stay | Aspiration pneumonitis |
| Sedative-hypnotics | |||||
| Only benzodiazepine receptor agonists/others | 426 | 8.2 | 7.7 | ref | ref |
| Barbiturates/non-barbiturates | 155 | 17.4 | 23.9 | 2.97 (1.60, 5.55)* | 3.83 (2.18, 6.79)* |
| No sedative-hypnotics | 95 | 7.4 | 2.1 | 1.03 (0.36, 2.62) | 0.35 (0.05, 1.30) |
| Antidepressants | |||||
| Only new-generation antidepressants/others | 168 | 8.3 | 10.7 | ref | ref |
| Tricyclic antidepressants | 72 | 9.7 | 18.1 | 0.85 (0.27, 2.42) | 2.25 (0.93, 5.38) |
| No antidepressants | 436 | 11.0 | 9.4 | 1.18 (0.58, 2.53) | 0.85 (0.44, 1.71) |
| Antipsychotics | |||||
| Only second-generation antipsychotics | 92 | 9.8 | 12.0 | ref | ref |
| First-generation antipsychotics | 148 | 10.1 | 13.5 | 0.78 (0.30, 2.08) | 1.02 (0.43, 2.53) |
| No antipsychotics | 436 | 10.3 | 9.4 | 0.98 (0.43, 2.46) | 1.12 (0.50, 2.66) |
| Other classes (ref = without each drug class) | |||||
| Mood stabilizers | 117 | 7.7 | 9.4 | 0.75 (0.30, 1.69) | 0.56 (0.24, 1.21) |
| Antiparkinson drugs | 71 | 14.1 | 22.5 | 1.76 (0.70, 4.17) | 2.77 (1.26, 5.96)* |
| Pain killers | 135 | 7.4 | 3.7 | 1.27 (0.54, 2.83) | 0.59 (0.19, 1.53) |
| Antiallergy drugs | 31 | 16.1 | 3.2 | 2.67 (0.78, 7.85) | 0.28 (0.01, 1.61) |
| Cardiovascular drugs | 19 | 15.8 | 5.3 | 0.97 (0.19, 3.74) | 0.14 (0.01, 0.91)* |
| Drugs affecting the gut | 77 | 7.8 | 11.7 | 0.59 (0.20, 1.49) | 1.10 (0.44, 2.53) |
| Other | 120 | 5.8 | 3.3 | 0.59 (0.22, 1.34) | 0.23 (0.06, 0.64)* |
| Major diagnosis | |||||
| Adjustment disorders | 156 | 7.1 | 7.1 | ref | ref |
| Bipolar disorders | 59 | 6.8 | 13.6 | 1.37 (0.33, 4.83) | 2.07 (0.65, 6.39) |
| Major depressive disorders | 174 | 13.8 | 10.3 | 1.82 (0.77, 4.51) | 0.87 (0.36, 2.18) |
| Schizophrenia | 72 | 16.7 | 18.1 | 2.65 (0.95, 7.54) | 1.81 (0.68, 4.86) |
| Other | 215 | 8.4 | 10.2 | 0.73 (0.27, 1.99) | 0.70 (0.25, 1.96) |
| Other diagnoses | |||||
| Borderline personality disorders | 148 | 8.8 | 12.2 | 2.87 (1.13, 7.14)* | 1.86 (0.79, 4.27) |
| Other personality disorders | 29 | 27.6 | 6.9 | 6.50 (2.15, 19.12)* | 0.90 (0.13, 3.79) |
| Anxiety disorders | 56 | 5.4 | 10.7 | 1.18 (0.25, 4.21) | 1.54 (0.46, 4.65) |
| Substance use disorders | 15 | 13.3 | 13.3 | 1.63 (0.21, 7.91) | 0.85 (0.11, 4.26) |
| Alcohol use disorders | 13 | 15.4 | 30.8 | 1.49 (0.17, 8.07) | 5.40 (1.13, 23.01)* |
a The denominator was the number of patients who ingested a substance or who have a psychiatric diagnosis and the numerator was the number of incident cases among the patients.
b Adjusted for sex, age, psychiatric diagnoses, drug classes ingested, and alcohol intake.
ICU = intensive care unit; ref = reference group.
* p < 0.05.
The incidence of prolonged ICU stay was 27.6% (8 of 29) in patients with other personality disorders and 9.4% (61 of 647) in those without (OR: 6.50; 95% CI: 2.15, 19.12). In addition, the incidence of prolonged ICU stay was 8.8% (13 of 148) in patients with borderline personality disorder and 10.6% (56 of 528) in those without (OR: 2.87; 95% CI: 1.13, 7.14). In the analysis of aspiration pneumonitis, there were no statistically significant differences between patients with and without personality disorders. The proportion of inter-hospital transfers was similar among patients with and without borderline personality disorder (4.1% vs. 4.7%) and was higher among patients with other personality disorders than among those without (10.3% vs. 4.3%).
The association between barbiturate overdose and prolonged length of stay was robust in the sensitivity analysis (S3 Table). Although the directions of the associations between personality disorders and prolonged length of stay were maintained, the associations did not reach statistical significance in the sensitivity analysis (S3 Table).
Discussion
Our study yielded three major findings. First, we observed that an overwhelming majority (79%) of the patients ingested benzodiazepines that were four of the top 5 substances involved in an overdose-related admission to the ICU. Our findings differ from those of previous studies conducted in other countries [2, 7]. For example, paracetamol and ibuprofen were the two most frequently ingested substances involved in overdose-related visits to an emergency department in a teaching hospital in the United Kingdom [7]. In addition, opiates and benzodiazepines were the top 2 major drug classes involved in overdose-related visits to emergency departments in the United States [2]. One potential explanation for this discrepancy is that the availability of drugs and prescribing practice may vary from country to country.
Second, we observed that barbiturate overdose increased the odds of aspiration pneumonitis compared to other sedative-hypnotic overdose (i.e., benzodiazepine overdose). One potential explanation for the adverse effects is that barbiturates have respiratory depressant effects [15, 24]. To our knowledge, this study is the first to quantify the comparative risk of aspiration pneumonitis between a barbiturate and benzodiazepine overdose, even though the results are similar to those of previous studies that showed the comparative risk between poisoning by barbiturates and that by any other drug [15, 29]. In addition, a previous study showed that ingestion of opioids increased the risk of aspiration pneumonitis compared to non-ingestion [21]; however, this association was not replicated in our study. One potential explanation for this discrepancy is that opioids are much less consumed in Japan than in other countries [30]. Furthermore, a previous study showed that ingestion of tricyclic antidepressants increased the risk of aspiration pneumonitis compared to non-ingestion [18]. Our results did not confirm this significant association between tricyclic antidepressants and aspiration pneumonitis, although the association remained in the same direction.
Our study also adds to the literature demonstrating that barbiturate overdose increased the odds of prolonged ICU stay. Patients with barbiturate poisoning sometimes require treatment for aspiration pneumonitis and consequently have an increased risk of prolonged ICU stay. In addition, our study showed that 23% of patients presented poisoning by barbiturates. The non-negligible share of poisoning by barbiturates among overdose patients can be explained by the fact that 3% of psychiatric outpatients still receive a prescription for barbiturates in Japan [31]. Since barbiturates have been replaced by benzodiazepines as the most commonly prescribed sedatives, there has been a marked reduction in overdose-related deaths by barbiturates in the United Kingdom and India [32]. These results suggest that judicious prescription of barbiturates by psychiatrists could reduce the risk of an adverse clinical course when a patient attempts overdose.
Third, our study shows that personality disorders are associated with increased odds of prolonged ICU stay but not aspiration pneumonitis. Similar results for aspiration pneumonitis have been reported by a previous study that demonstrated no significant differences in overdose-related treatments between personality disorders and mood disorders [33]. However, our results extend this by showing that personality disorders are associated with an increased risk of prolonged ICU stay. One potential explanation for the relationship between other personality disorders and prolonged ICU stay is the coordination of inter-hospital transfer, although the mechanisms through which borderline personality contributed to a prolonged ICU stay remains unknown. This hypothesis is partly supported by the fact that patients with other personality disorders represent a higher proportion of those who require inter-hospital transfer. These patients are likely to demonstrate a greater severity of mental disorders that require acute intensive psychiatric care in a crisis stabilization unit.
Our study has three major limitations. First, the accuracy of information on the ingested drugs and psychiatric diagnoses was unknown. The data on the ingested drugs were based on reports by the ambulance crew. Psychiatric diagnoses were made only during the ICU stay. Second, a selection bias might be present because this was a single-center study. Our study population was recruited from a tertiary emergency medical facility in Japan and may have a higher frequency of patients with a severe clinical course. Third, this study lacks information on clinical, physiological, and procedural characteristics (e.g., coma at admission, acute severity scores, duration of mechanical ventilation) that might affect the risk of an adverse clinical course. Therefore, we cannot identify whether aspiration pneumonitis is associated with level of consciousness alteration or with a specific effect of the barbiturate used.
Conclusions
Our cohort study shows increased odds for adverse clinical courses in cases of barbiturate overdose. Our results suggest that judicious prescription of barbiturates by psychiatrists could reduce the risk of an adverse clinical course when a patient attempts overdose.
Supporting Information
(PDF)
(PDF)
(PDF)
Data Availability
The ethical restrictions prohibit the authors from making the minimal dataset publicly available. Data sharing will be considered for researchers upon request and upon institutional review board approval from the research sites. Requests should be submitted to yokumura@blue.zero.jp.
Funding Statement
Funding for this study was provided by a Grant-in-Aid for Young Scientists (B) (No. 26870914) by the Japan Society for the Promotion of Science. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wilkinson S, Taylor G, Templeton L, Mistral W, Salter E, Bennett P. Admissions to hospital for deliberate self-harm in England 1995–2000: an analysis of hospital episode statistics. Journal of public health medicine. 2002;24:179–83. . [DOI] [PubMed] [Google Scholar]
- 2.Xiang Y, Zhao W, Xiang H, Smith GA. ED visits for drug-related poisoning in the United States, 2007. The American journal of emergency medicine. 2012;30:293–301. 10.1016/j.ajem.2010.11.031 . [DOI] [PubMed] [Google Scholar]
- 3.Hovda KE, Bjornaas MA, Skog K, Opdahl A, Drottning P, Ekeberg O, et al. Acute poisonings treated in hospitals in Oslo: a one-year prospective study (I): pattern of poisoning. Clinical toxicology (Philadelphia, Pa). 2008;46:35–41. 10.1080/15563650601185969 . [DOI] [PubMed] [Google Scholar]
- 4.Hendrix L, Verelst S, Desruelles D, Gillet J-B. Deliberate self-poisoning: characteristics of patients and impact on the emergency department of a large university hospital. Emergency medicine journal: EMJ. 2013;30:e9 10.1136/emermed-2011-201033 . [DOI] [PubMed] [Google Scholar]
- 5.Albert M, McCaig LF, Uddin S. Emergency department visits for drug poisoning: United States, 2008–2011. NCHS data brief. 2015:1–8. . [PubMed] [Google Scholar]
- 6.Hirata K, Matsumoto Y, Tomioka J, Kurokawa A, Matsumoto M, Murata M. Acute drug poisoning at critical care departments in Japan. Japanese Journal of Hospital Pharmacy. 1998;24:340–8. 10.5649/jjphcs1975.24.340 [DOI] [Google Scholar]
- 7.Prescott K, Stratton R, Freyer A, Hall I, Le Jeune I. Detailed analyses of self-poisoning episodes presenting to a large regional teaching hospital in the UK. British Journal of Clinical Pharmacology. 2009;68:260–8. 10.1111/j.1365-2125.2009.03458.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouknight RR, Alguire PC, Lofgren RP, Hoppe RB. Self-poisoning: outcome and complications in the community hospital. The Journal of family practice. 1986;23:223–5. . [PubMed] [Google Scholar]
- 9.Kamijo Y. Acute drug poisoning. (In Japanese). Psychiatry. 2007;10:297–301. [Google Scholar]
- 10.Liisanantti J, Kaukoranta P, Martikainen M, Ala-Kokko T. Aspiration pneumonia following severe self-poisoning. Resuscitation. 2003;56:49–53. . [DOI] [PubMed] [Google Scholar]
- 11.Manini AF, Hoffman RS, Stimmel B, Vlahov D. Clinical risk factors for in-hospital adverse cardiovascular events after acute drug overdose. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 2015;22:499–507. 10.1111/acem.12658 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heyerdahl F, Bjornaas MA, Dahl R, Hovda KE, Nore AK, Ekeberg O, et al. Repetition of acute poisoning in Oslo: 1-year prospective study. The British journal of psychiatry: the journal of mental science. 2009;194:73–9. 10.1192/bjp.bp.107.048322 . [DOI] [PubMed] [Google Scholar]
- 13.Okumura Y, Shimizu S, Ishikawa KB, Matsuda S, Fushimi K, Ito H. Comparison of emergency hospital admissions for drug poisoning and major diseases: a retrospective observational study using a nationwide administrative discharge database. BMJ open. 2012;2:Online. 10.1136/bmjopen-2012-001857 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwake L, Wollenschläger I, Stremmel W, Encke J. Adverse drug reactions and deliberate self-poisoning as cause of admission to the intensive care unit: a 1-year prospective observational cohort study. Intensive Care Medicine. 2009;35:266–74. 10.1007/s00134-008-1250-1 . [DOI] [PubMed] [Google Scholar]
- 15.Wada K, Kishimoto M, Yamori T, Fukumoto T, Iwamoto T, Sasaki T. Aspiration pneumonia in patients with self-poisoning of psychotropics. (In Japanese). Japanese journal of general hospital psychiatry. 2009;21:258–63. [Google Scholar]
- 16.Okumura Y, Shimizu S, Ishikawa KB, Matsuda S, Fushimi K, Ito H. Characteristics, procedural differences, and costs of inpatients with drug poisoning in acute care hospitals in Japan. General hospital psychiatry. 2012;34:681–5. 10.1016/j.genhosppsych.2012.07.009 . [DOI] [PubMed] [Google Scholar]
- 17.Zyoud SeH, Awang R, Sulaiman SAS, Al-Jabi SW. A cross-sectional observation of the factors associated with deliberate self-poisoning with acetaminophen: impact of gender differences and psychiatric intervention. Human psychopharmacology. 2010;25:500–8. 10.1002/hup.1140 . [DOI] [PubMed] [Google Scholar]
- 18.Isbister GK, Downes F, Sibbritt D, Dawson AH, Whyte IM. Aspiration pneumonitis in an overdose population: frequency, predictors, and outcomes. Critical care medicine. 2004;32:88–93. 10.1097/01.CCM.0000104207.42729.E4 . [DOI] [PubMed] [Google Scholar]
- 19.Novack V, Jotkowitz A, Delgado J, Novack L, Elbaz G, Shleyfer E, et al. General characteristics of hospitalized patients after deliberate self-poisoning and risk factors for intensive care admission. European Journal of Internal Medicine. 2006;17:485–9. 10.1016/j.ejim.2006.02.029 . [DOI] [PubMed] [Google Scholar]
- 20.Maignan M, Pommier P, Clot S, Saviuc P, Debaty G, Briot R, et al. Deliberate drug poisoning with slight symptoms on admission: are there predictive factors for intensive care unit referral? A three-year retrospective study. Basic & clinical pharmacology & toxicology. 2014;114:281–7. 10.1111/bcpt.12132 . [DOI] [PubMed] [Google Scholar]
- 21.Christ A, Arranto CA, Schindler C, Klima T, Hunziker PR, Siegemund M, et al. Incidence, risk factors, and outcome of aspiration pneumonitis in ICU overdose patients. Intensive care medicine. 2006;32:1423–7. 10.1007/s00134-006-0277-4 . [DOI] [PubMed] [Google Scholar]
- 22.Värnik A, Sisask M, Värnik P, Wu J, Kõlves K, Arensman E, et al. Drug suicide: a sex-equal cause of death in 16 European countries. BMC public health. 2011;11:Online. 10.1186/1471-2458-11-61 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eyer F, Stenzel J, Schuster T, Felgenhauer N, Pfab R, von Bary C, et al. Risk assessment of severe tricyclic antidepressant overdose. Human & experimental toxicology. 2009;28:511–9. 10.1177/0960327109106970 . [DOI] [PubMed] [Google Scholar]
- 24.Mactier R, Laliberté M, Mardini J, Ghannoum M, Lavergne V, Gosselin S, et al. Extracorporeal treatment for barbiturate poisoning: recommendations from the EXTRIP Workgroup. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2014;64:347–58. 10.1053/j.ajkd.2014.04.031 . [DOI] [PubMed] [Google Scholar]
- 25.Mowry JB, Spyker DA, Cantilena LR, Bailey JE, Ford M. 2012 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 30th Annual Report. Clinical toxicology (Philadelphia, Pa). 2013;51:949–1229. 10.3109/15563650.2013.863906 . [DOI] [PubMed] [Google Scholar]
- 26.Tournier M, Grolleau A, Cougnard A, Verdoux H, Molimard M. The prognostic impact of psychotropic drugs in intentional drug overdose. Pharmacopsychiatry. 2009;42:51–6. 10.1055/s-0028-1100426 . [DOI] [PubMed] [Google Scholar]
- 27.Marik PE. Aspiration pneumonitis and aspiration pneumonia. The New England journal of medicine. 2001;344(9):665–71. 10.1056/NEJM200103013440908 . [DOI] [PubMed] [Google Scholar]
- 28.Dobson AJ, Barnett G. An Introduction to Generalized Linear Models Chapman and Hall; 2008. [Google Scholar]
- 29.Ando S, Yasugi D, Matsumoto T, Kanata S, Kasai K. Serious outcomes associated with overdose of medicines containing barbiturates for treatment of insomnia. Psychiatry and clinical neurosciences. 2014;68:721 10.1111/pcn.12198 . [DOI] [PubMed] [Google Scholar]
- 30.Foundation for Promotion of Cancer Research. Cancer statistics in Japan 2014 2014 [cited 2015 June 22]. Available from: http://ganjoho.jp/data/professional/statistics/backnumber/2014/cancer_statistics_2014.pdf.
- 31.Okumura Y, Inada K, Matsumoto T, Shimizu S. Changes in high-dose and combined anxiolytic-hypnotic prescription in outpatient psychiatric practice after regulatory action. (In Japanese). Japanese journal of clinical psychopharmacology. 2015;18:1173–88. [Google Scholar]
- 32.Eddleston M, Karalliedde L, Buckley N, Fernando R, Hutchinson G, Isbister G, et al. Pesticide poisoning in the developing world—a minimum pesticides list. Lancet. 2002;360:1163–7. . [DOI] [PubMed] [Google Scholar]
- 33.Ando S, Matsumoto T, Omoya R, Hojo A, Shimada T, Nakanotani T, et al. Clinical differences in the extent of suicide intent, depression and dissociation between self-poisoning patients with mood disorder and those with personality disorder. (In Japanese). Clinical psychiatry. 2009;51:749–59. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
Data Availability Statement
The ethical restrictions prohibit the authors from making the minimal dataset publicly available. Data sharing will be considered for researchers upon request and upon institutional review board approval from the research sites. Requests should be submitted to yokumura@blue.zero.jp.