Abstract
Objective. To evaluate acceptability and clinical outcomes of acupuncture on patient-reported pain and anxiety in an emergency department (ED).
Design. Observational, retrospective pilot study.
Setting. Abbott Northwestern Hospital ED, Minneapolis, MN.
Methods. Retrospective data was used to identify patients receiving acupuncture in addition to standard medical care in the ED between 11/1/13 and 12/31/14. Feasibility was measured by quantifying the utilization of acupuncture in a novel setting and performing limited tests of its efficacy. Patient-reported pain and anxiety scores were collected by the acupuncturist using an 11-point (0–10) numeric rating scale before (pre) and immediately after (post) acupuncture. Efficacy outcomes were change in pain and anxiety scores.
Results. During the study period, 436 patients were referred for acupuncture, 279 of whom were approached by the acupuncturist during their ED visit. Consent for acupuncture was obtained from 89% (248/279). A total of 182 patients, who had a pre-pain score >0 and non-missing anxiety scores, were included in analyses. Of the 52% (94/182) who did not have analgesics before or during the acupuncture session, the average decrease of 2.37 points (95% CI: 1.92, 2.83) was not different (p > 0.05) than the mean decrease of 2.68 points for those receiving analgesics (95% CI 2.21, 3.15). The average pre-anxiety score was 4.73 points (SD = 3.43) and the mean decrease was 2.27 points (95% CI: 1.89, 2.66).
Conclusions. Results from this observational trial indicate that acupuncture was acceptable and effective for pain and anxiety reduction, in conjunction with standard medical care. These results will inform future randomized trials.
Keywords: Acupuncture, Emergency Department, Complementary Integrative Health, Acute Pain, Anxiety
Background
In this paper, we describe a study of acupuncture as a complementary approach to treating pain in the emergency department (ED) of a tertiary care hospital. Pain management is a central challenge in the ED setting, where pain is identified as one of the most common complaints of ED patients and accounts for at least 75% of visits [1]. Opioid medications remain the primary method providers in the ED have to treat acute pain [2,3]. ED physicians are among the most frequent prescribers of opioid pain relievers [4], with approximately 48.9% of ED patients either receiving opioids in the ED or at discharge—an increase of 21.5% over the past decade [5]. Although pharmacotherapy including opioid analgesics is common practice in the ED, opioid use is not without risk of adverse effects, tolerance, addiction, and abuse [3].
Pain management, and the conventional course of treatment with pain medications including opioids, is of concern to patients. The authors of a study composed of interviews with recently discharged ED patients about pain management reported that patients worry about potential opioid addiction [6]. Patients also felt that ED physicians did not talk with them about the dangers of opioid dependence or about potential alternative approaches to pain relief [6]. A descriptive study that included interviews with recent ED patients who had received prescriptions for opioids found that patients tended to underestimate the risks of opioid addiction or feared addiction to the point of under-treating their pain [7]. Studies of patient satisfaction with pain management in the ED have found that pain management is largely suboptimal in emergency departments [8].
Complementary and integrative health (CIH) therapies are a popular approach to pain management [9–14], generally as a choice made by patients as consumers of health care. CIH offerings in hospitals are less common, particularly in EDs. Acupuncture is a CIH modality used by millions of patients every year for a variety of reasons, and has been shown to be efficacious and effective in treating pain and anxiety among a variety of patient populations [15–20].
To date, five studies have explored either the efficacy or effectiveness of acupuncture treatments delivered in the ED setting [21–25]. The limited scope and size of the previous studies prompted a recent systematic review of acupuncture in ED settings, which concluded that there is insufficient evidence to make recommendations regarding acupuncture use in the ED [26]. The article suggests that safety, feasibility, and effectiveness of acupuncture in the ED should be tested in future RCTs [26].
In the investigation described here, we sought to examine the adaptation of acupuncture to standard medical care at Abbott Northwestern Hospital, a large, urban ED. We were primarily interested in determining whether providing acupuncture in the ED setting was feasible and acceptable. Additionally, we gathered data to describe which ED patients were referred for and received acupuncture as well as changes in pain and anxiety among patients who received acupuncture in the ED.
Methods
Study Setting and Design
This pilot study and retrospective electronic health record (EHR) review of acupuncture in the emergency department were conducted at Abbott Northwestern Hospital (ANW), a 631-bed teaching and specialty hospital in Minneapolis, MN. The ANW ED is a 35-bed facility that annually treats more than 45,000 patients. The ED is open 24 hours a day, seven days a week, and treats patients age 12 and older. Staff includes physicians, physician assistants, nurse practitioners, nurses, and emergency medical technicians.
The idea for providing acupuncture in the ED emerged from discussions between the ED medical director and the research director for the Penny George Institute for Health and Healing (PGIHH) at ANW. Since 2003, PGIHH has delivered CIH services to inpatients throughout the hospital and has grown into one of the largest inpatient integrative health care programs in the country [27]. After successful integration of complementary therapies into patient care across service lines at ANW [27,28], it seemed like a viable next step to adapt the PGIHH program to address the needs of the ED. Acupuncture was selected as the modality to implement due to its potential for treating a wide variety of conditions, such as pain, anxiety, and nausea [28].
The study acupuncturist was scheduled in the ED approximately 15–30 hours per week, usually during normal business hours. Before administering any treatments, the acupuncturist first shadowed providers in the ED to get a better sense of the patient population and flow of patients through the department. The shadowing period also allowed the ED staff to get to know the acupuncturist, ask questions, and even receive treatments themselves. This onboarding was later acknowledged by the ED director and the study acupuncturist as a vital step that helped successfully integrate acupuncture into the ED. Acupuncture treatments for patients in the ED began in November 2013, paid for through funds from a philanthropic donor to PGIHH as well as an administrative supplement to a National Institutes of Health grant. The integration of acupuncture into the ED is described further in the “Adaptation” section of the results.
Study Participants
Participants in this study included all ED patients age 18 years or older at Abbott Northwestern Hospital between November 1, 2013 and December 31, 2014 who received acupuncture in the ED. The EHR (Epic; Verona, WI) was used to retrospectively identify all eligible patients and extract data necessary for the analysis. All patients whose data were obtained had provided written permission upon admission to the ED for their medical records to be used for general research purposes by Allina Health. The Quorum Review IRB approved this specific study with a waiver of informed consent.
Acupuncture Referral and Therapy Protocol
Potential acupuncture patients were identified in the ED either by providers, nurses, or the licensed acupuncturist. Clinical providers were required to complete an acupuncture referral in the EHR. Once identified and referred, the acupuncturist would approach the patient to determine their interest in receiving an acupuncture treatment. It was possible that during the study period the acupuncturist would be unavailable due to scheduling or workflow issues and would not be able to act on the referral placed by the ED providers. If individuals were interested, the acupuncturist would explain the procedure and possible risks before obtaining written consent for the acupuncture treatment as required by state law and hospital policy. After obtaining consent, the acupuncturist discussed with the patient their chief complaints and medical history.
An individualized acupuncture treatment was then delivered based on the patient's presentation and the acupuncturist’s assessment. Acupuncture was delivered by a single acupuncturist who was licensed by the Minnesota Board of Medical Practice. Traditional Chinese Medicine (TCM) acupuncture, auricular acupuncture, Balance Method acupuncture, and Master Tung style acupuncture were used on patients in the study, as deemed appropriate by the acupuncturist. In his experience, distal treatments were effective for symptom management and flexible enough in terms of point selection to accommodate virtually any patient in the ED. Patients were treated based on their presenting symptoms and conditions at the discretion of the acupuncturist. No predetermined acupuncture point protocol was used. The acupuncturist was free to vary the number of needles inserted, acupuncture points, depth of needles, and needle stimulation for each patient. Acupuncture treatments were delivered using sterile, single use, Seirin J Type acupuncture needles which were 30 mm in length and either .16 mm, .18 mm, or .20 mm in diameter.
Using a customized documentation flowsheet in the EHR, the acupuncturist recorded the time that the acupuncture was initiated and completed, the location of needles, and the primary clinical reason for the provision of acupuncture. The acupuncturist also recorded any instances of bleeding in the EHR, noting quantity and from which acupuncture point it had occurred.
Measurements
Data Extraction
Data extracted from the EHR included demographic information such as patients’ age at time of admission, sex, race (White, African American, Asian, or other), ethnicity (Hispanic or Latino, not Hispanic/Latino, or declined), and marital status (married, widowed, divorced, or single).
All referrals for acupuncture services were documented in the EHR and included time and location of each referral. Treatment details, including focus of visit, pain and anxiety assessments for each acupuncture session, and duration of acupuncture were routinely documented in a customized flowsheet. Retrospective medical chart reviews were also conducted to determine the area of the body for which the acupuncture session was delivered.
Trained health information specialists extracted specified data from the EHR using Microsoft SQL. All extracted data was checked for integrity and cleaned by the study biostatistician. Missing data was assumed to be missing at random and, therefore, ignored.
Feasibility Measures
To assess the feasibility of utilizing acupuncture in the ED to treat pain, we focused on three measures: acceptability by providers and patients, adaptability of pre-existing acupuncture procedures, and limited-efficacy. Acceptability was measured by determining the proportion of ED providers who referred patients for treatment as well as the proportion of referred patients who agreed to receive acupuncture. Adaptation, as a feasibility measure, is defined as the modification of established treatment procedures to better accommodate a new situation [29]. We described adaptation by detailing the ways in which standard acupuncture procedures changed in order to be adapted to a novel environment, the ED. This study was also designed to test the effects of acupuncture in reducing pain and anxiety for patients in the ED. This efficacy testing was done with limited statistical power and is described in more detail in the following sections.
Pain and Anxiety Scores
For patients who received acupuncture services, the acupuncturist collected patients’ self-reported pain and anxiety scores directly prior to and after each session. The acupuncturist asked patients to provide a number to indicate the level of pain they were currently experiencing on an 11-point numeric rating scale where 0 was defined as ‘no pain’ and 10 was defined as ‘worst pain imaginable’ [30,31]. Similarly, the acupuncturist obtained anxiety scores, where 0 was ‘no anxiety’ and 10 was ‘worst anxiety imaginable.’ The study measures of interest were change in pain and anxiety scores, calculated by subtracting the pre-score from the post-score. As part of previous NIH-funded studies of CIH at ANW, a comprehensive training manual for documenting in the EHR was developed. This was done to ensure consistent data collection and recording by all CIH providers within ANW and the entire Allina Health system. The study acupuncturist utilized these procedures in the present investigation.
Analgesic Use Measures
Analgesic use was determined by examining the Medical Administration Record (MAR), as documented by the nurse or provider. This record includes the pharmaceutical class, specific type of medication, time of administration, dosage, and route of delivery. Subjects were identified has having received an analgesic if there was at least one record of receipt of a drug categorized in the analgesic pharmaceutical class before the end of the acupuncture session. Drugs in the analgesic class consisted of both opioids and non-opioids. Dosing was not considered for this study.
Analytic Data Set
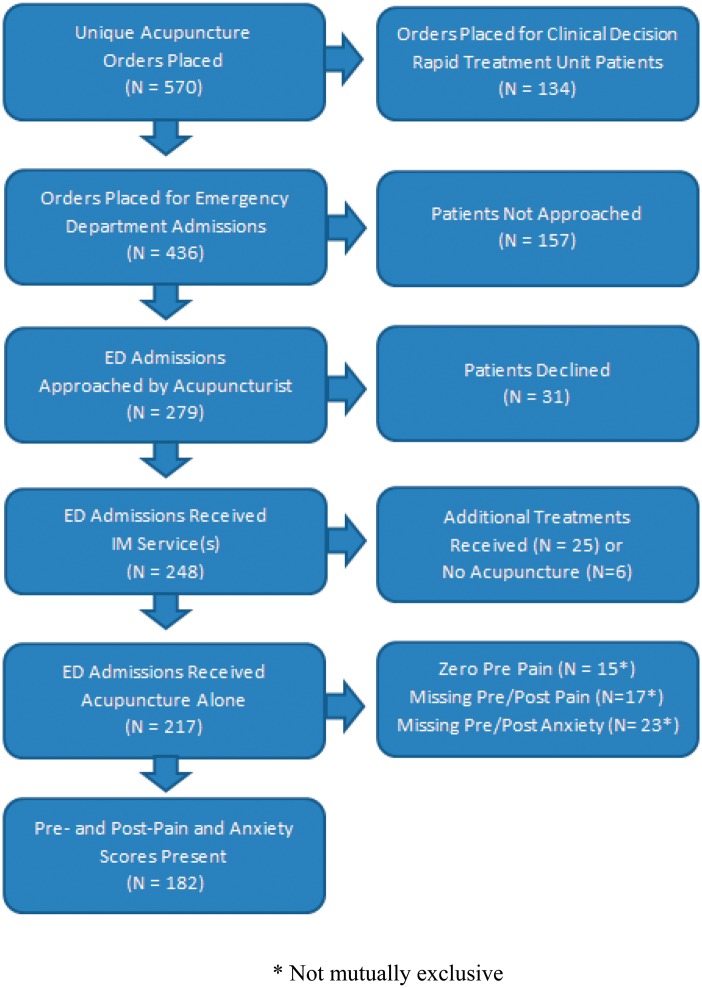
A total of 597 orders for acupuncture were placed between November 1, 2013 and December 31, 2014. Some patients who present at the ED require further observation before the physicians determine whether they should be discharged. For these patients, ANW has a Clinical Decision and Rapid Treatment (CDART) unit located next to the ED. Since the acuity of CDART patients varies from that of ED patients, patients under observation in CDART (N = 134) were not included in this analysis. Duplicate orders within the same hospital stay (N = 27) were also excluded from the data set. Due to scheduling and workflow issues, the acupuncturist was unable to approach some of the patients referred for acupuncture (N = 157).
The study acupuncturist approached 279 patients in the ED, 248 of whom (88.9%) agreed to receive therapy. A total of 31 sessions were dropped because other CIH therapies (e.g., aromatherapy, Korean hand therapy, acupressure) were given in addition to or in place of acupuncture. In some cases, the acupuncturist was unable to collect pre- or post-acupuncture pain and anxiety scores. Of these sessions, 200 had both pre- and post-pain scores and 194 had pre- and post-anxiety scores. Because the efficacy outcome of interest was pain change, 15 subjects who presented with no pain were excluded from analysis, creating a final sample size of 182 acupuncture sessions from 180 unique patients (see Figure 1). Two patients in the analytic data set received acupuncture twice, one time at each of their two ED visits. Both encounters were included in the final data set.
Figure 1.
CONSORT Diagram.
Statistical Analysis
As this was a retrospective feasibility study intended to inform the design of future randomized trials, an a priori power calculation was considered but was deemed unnecessary. Instead, the sample was designed such that it was representative of the overall ED population and based on the same inclusion/exclusion criteria to be used in future research of this nature. A value of p ≤ 0.05 was considered statistically significant. All analyses were conducted using SAS Version 9.3 (SAS Institute Inc.; Cary, NC).
No formal statistical tests were used to analyze the acceptability of acupuncture in the ED. We simply observed the number of ED providers who referred subjects for treatment as well as the proportion of referred patients who agreed to receive acupuncture. Similarly, adaptation was analyzed by describing the exact modifications made to the acupuncture procedures in order to make it better suited for the urgent setting in the ED.
We compared pre-and post-intervention scores to establish point estimates and variability around the chosen measures of acupuncture effectiveness: pain and anxiety reduction. Paired t-tests were used to determine if absolute changes in outcomes were statistically different from zero.
To explore the relationship between pain and anxiety, we computed a Pearson’s product-moment correlation coefficient. Influential points were identified using Cook’s distance statistics and a sensitivity analysis was conducted by computing the correlation coefficient with and without these observations. A subgroup analysis was also conducted to test whether this relationship was influenced by the usage of analgesics before or during acupuncture therapy. We also conducted a multivariate regression with pain change as the outcome variable and adjusted for group and analgesic use before or during treatment.
Since analgesia use was not consistent across all patients, we used a paired t-test to compare the percentage decrease in pain scores in patients receiving analgesics before or during the acupuncture session with those patients who did not receive analgesic medications.
Results
Acceptability
Acupuncture was found to be widely accepted by both practitioners and patients as an adjunctive treatment for pain in the ED. Fifty-five of the 75 credentialed physicians, physician assistants, and nurse practitioners in the ANW ED referred a total of 436 patients for acupuncture. Of these, 279 subjects were approached by the study acupuncturist, and 248 (88.9%) accepted the acupuncture treatment (Figure 1). There are several reasons why the remaining 157 patients were not approached, including the referral was placed at a time when the acupuncturist was not working in the department, there were multiple referrals at the same time, and some patients may have discharged prior to the acupuncturist being able to approach them. Tests to compare baseline characteristics of patients not approached and those who declined to the final study population were conducted and it was found that patients who declined only differed in regards to marital status (p = 0.045). The populations were similar in all other aspects (data not shown). Baseline characteristics of the 182 study participants are shown in Table 1.
Table 1.
Baseline characteristics of 182 study participants
| Characteristic | Study Population (N = 182) |
|---|---|
| Age1 | 45.3 (16.7) |
| Age Category | |
| 11–202 | 6 (3.3%) |
| 21–30 | 34 (18.7%) |
| 31–40 | 36 (19.8%) |
| 41–50 | 40 (22.0%) |
| 51–60 | 30 (16.5%) |
| 61–70 | 17 (9.3%) |
| >70 | 19 (10.4%) |
| Sex | |
| Female | 123 (67.6%) |
| Male | 59 (32.4%) |
| Race | |
| American Indian/Alaska Native | 10 (5.5%) |
| Asian | 4 (2.2%) |
| Native Hawaiian or Other Pacific Islander | 1 (0.5%) |
| Black or African American | 50 (27.5%) |
| White | 111 (61.0%) |
| Patient Declined | 6 (3.3%) |
| Ethnicity | |
| Hispanic or Latino | 8 (4.4%) |
| Not Hispanic/Not Latino | 170 (93.4%) |
| Patient Declined | 4 (2.2%) |
| Marital Status | |
| Life Partner, Married, Significant Other | 59 (32.4%) |
| Seperated, Divorced | 24 (13.2%) |
| Widowed | 6 (3.3%) |
| Single | 92 (50.5%) |
| Unknown, Other | 1 (0.5%) |
| Analgesics Taken Before or During Therapy1 | |
| No | 94 (51.6%) |
| Yes | 88 (48.4%) |
Values are mean (SD) or no. (%) of subjects.
1Mean age and analgesic use is not available for the total emergency department population.
2Youngest subject in analysis data set was 18, as required by IRB.
Adaptation
We began planning an acupuncture program for the ED by basing it on the already established system used within the hospital for delivering acupuncture to inpatients [27]. After observing the workflow in the ED, it became clear that the inpatient referral and integrative delivery model would need to be adapted to better suit the needs of the ED. The first change that was implemented was to embed the acupuncturist directly into the ED, rather than basing him out of a separate office. In the original inpatient system, clinical providers sent electronic referrals to the acupuncturists via the EPIC-based EHR. These referrals were triaged and divided up amongst the team every morning. With inpatient acupuncture there was a significant time lag between the order being placed and the services being delivered. Obviously, this delay in services would not work in the ED where patient visits are measured in hours, not days. By having the acupuncturist work closely with the ED providers, we created a system that could deliver treatments in a timely manner to the patients most in need. Referrals for acupuncture were still ordered through the EHR, but most of the communication about who should be seen took place verbally.
For acupuncture in the ED, the overall length of treatments was shortened from about 30 to 20 minutes. This change was due to ED patients having a shorter length of stay and the desire to accommodate the flow of patients through the ED. The goal was for the acupuncturist to blend into the ED and not create a bottleneck which could adversely affect the patient throughput of the department.
Almost exclusively, acupuncture points used on ED patients were distal to the area of concern. Given the focus on patient safety and the constraints of treating in the small ED rooms with limited access to all areas of the patients’ body, the acupuncturist employed acupuncture techniques that were both simple and effective. Treatments were typically limited to fewer acupuncture points. The acupuncturist also avoided using treatments that involved repositioning the patients or removing shoes, socks, or other articles of clothing.
By incorporating all of these changes, it was possible to adapt the ANW inpatient acupuncture program to suit the needs of the patients and providers in the fast-paced ED.
The study acupuncturist was scheduled in the ED approximately 15–30 hours per week, usually during normal business hours. Although ED providers were instructed to refer patients at any time—that is, whether or not the acupuncturist was present in the ED at that moment—referrals were made more frequently when he was present.
Acupuncture Intervention
Acupuncture sessions lasted, on average, 23 minutes (SD = 8.9) and ranged from 6 to 78 minutes. Patients presented with pain in a variety of locations, with the highest percentage (34.2%) experiencing discomfort in their backs (Table 2). The second most common location reported was the head (21.1%), which included headaches, migraines, facial, and throat pain.
Table 2.
Pain location treated with acupuncture (N = 182)
| Location | Frequency | Percent |
|---|---|---|
| Back | 57 | 31.3% |
| Head | 41 | 22.5% |
| Limb | 37 | 20.3% |
| Abdomen | 27 | 14.8% |
| Chest | 17 | 9.3% |
| Groin | 3 | 1.7% |
Limited-Efficacy: Pain and Anxiety Change
A total of 182 patients presented in the ED with pain (pre-pain>0) with over half reporting that their pain was an 8 or above. These subjects had a mean pre-pain of 6.80 (SD = 2.58) and reported an average decrease of 2.52 points (95% CI: 2.20, 2,85; p-value<0.001) after acupuncture therapy (Table 3). Of those patients, 43% reported at least a 50% pain reduction and 57% reported at least a 30% pain reduction. Furthermore, 160 patients with high pain (pre-pain ≥ 4) had a mean pre-pain of 7.47 (SD = 1.93) and reported an average decrease of 2.71 points (95% CI: 2.36, 3.07). Of those patients, 39% reported at least a 50% pain reduction and 54% reported at least a 30% pain reduction.
Table 3.
Summary of pain and anxiety scores (N = 182)
| Statistic | Pre- Pain | Pain Change1 | Pre- Anxiety | Anxiety Change1 |
|---|---|---|---|---|
| Mean | 6.80 | −2.52 | 4.72 | −2.27 |
| Standard Deviation | 2.58 | 2.23 | 3.43 | 2.66 |
| Minimum | 1 | −9 | 0 | −10 |
| Median | 8 | −2 | 5 | −2 |
| Maximum | 10 | 2 | 10 | 6 |
1Negative values are desirable as it indicates a shift toward lower pain or anxiety.
Analgesic use was not uniform among the 182 participants with 52% (94/182) not receiving analgesics before or during the acupuncture session, whereas 48% (88/182) did receive analgesics in the same time frame. The average decrease for the former group was 2.37 points on the 11-point scale (95% CI: 1.92, 2.83), whereas the mean decrease for those receiving analgesics was 2.68 points (95% CI 2.21, 3.15). Results from a paired t-test indicate that there was no significant difference in these changes across the groups (p > 0.05).Putting these changes into clinical context, detecting a 1.3-point difference in NRS pain scores is reported as being clinically significant [31]. Importantly, both the acupuncture + analgesics group and the acupuncture only group reported NRS decreases exceeding the 2-point threshold that is considered clinically significant [31].
Of the 182 subjects with non-missing pre- and post- anxiety scores, 23% reported a pre-anxiety score of 0. The mean pre-anxiety score was 4.73 (SD = 3.43) and, on average, decreased by 2.27 points (95% CI: 1.89, 2.66; p-value < 0.001) after acupuncture. A total of 101 reported high anxiety levels (pre-anxiety ≥ 5) with a mean pre-anxiety of 7.37 (SD = 1.85) and an average decrease of 3.47 points (95% CI: 2.92, 4.01).
Relationship Between Pain and Anxiety Change
As seen in Table 4, there was a positive correlation between pain change and anxiety change (r = 0.186, N = 182, p = 0.0117). That is, subjects with a larger reduction in anxiety after treatment with acupuncture also experienced a larger reduction in pain. This relationship remained significant in a sensitivity analysis where four influential points with a Cook’s distance greater than 0.04 were removed (r = 0.216, N = 178, p = 0.004). Analgesia-use was suspected to influence this relationship, so a subgroup analysis was conducted and we discovered that the correlation was not significant among subjects who did not receive an analgesic before or during acupuncture therapy (r = 0.152, N = 94, p = 0.1436), but significant for those who did (r = 0.233, N = 88, p = 0.0289).
Table 4.
Pearson’s correlation between pain change and anxiety change
| N | r | P-value | |
|---|---|---|---|
| Overall | 182 | 0.186 | 0.0117 |
| Analgesic Use | 88 | 0.233 | 0.0289 |
| No Analgesic Use | 94 | 0.152 | 0.1436 |
Limitations
This study has some limitations inherent to its observational design. Because our first objective was to determine feasibility, and our data collection was not randomized, there was no comparison group to help us better understand the effects of the acupuncture intervention. It is also possible that selection bias may have resulted from how the providers and nurses referred patients for acupuncture and how the acupuncturist decided whom to treat if multiple referrals were placed at the same time. However, the study was reflective of how acupuncture was actually referred in clinical practice, which was our goal from a feasibility standpoint.
Our patient population was extremely heterogeneous with regard to clinical conditions. Since the intent of the pilot project was to determine whether or not acupuncture could reasonably be integrated into a busy ED, the approach was to treat all patients regardless of clinical condition. It is also possible that self-report of pain and anxiety by the patients could have been influenced by the therapeutic relationship, since the acupuncturist was the same individual who captured the patient-reported pain and anxiety scores. Nevertheless, self-reported scores are a recommended part of clinical practice for pain management [32].
All scores reported in this manuscript were collected by the acupuncturist before and after delivering the acupuncture treatments. We only considered the timing of the analgesics in a binary way; for analytical purposes, patients either received analgesics before or during the acupuncture treatment, or not at all. Therefore, it is quite possible that the analgesics had only just been administered. Any analgesics administered after the acupuncture treatment were not captured by our data collection nor considered in our analysis.
The absence of a standardized acupuncture protocol may be viewed as a limitation, but it was the most appropriate choice for the heterogeneous patient population and fast pace of the ED. Operationally, our provision of acupuncture in the ED may have been limited by having only one acupuncturist who worked for 15–30 hours per week during business hours. Since the acupuncturist worked this limited schedule, acupuncture treatments were only possible during the times when he was present. The tendency of ED providers to make referrals when the acupuncturist was present may suggest the importance of having an acupuncturist on staff in the ED in order to assist in the referral process. However, this limited provision of acupuncture via one practitioner was appropriate for the scope and scale of a preliminary feasibility study.
Discussion
This pilot study provides preliminary evidence for the feasibility and effectiveness of acupuncture as an adjunct to usual care for pain in the ED. We found that stationing an acupuncturist in the ED and streamlining his services into the workflow and referral processes of ED care providers was acceptable to ED providers and patients. Our outcome data, while limited by the study design, suggest that acupuncture plus usual pain treatment (e.g., analgesics) is associated with comparable pain relief to that provided by acupuncture alone among ED patients at ANW. However, the small sample sizes of the analgesic and non-analgesic groups suggest these results should be interpreted with caution and would be better explored within a large, randomized controlled trial. Finally, changes in pain and anxiety were correlated, consistent with previous evidence for a relationship between anxiety and acute pain among ED patients [33].
Of the previous studies that have investigated acupuncture in the ED, only two assessed feasibility. Our study found higher acceptance (88.9%) than Zhang (69%) [24] or Arnold (43%) [21]. Of note, however, these studies included only patients admitted with pain and/or nausea, while our population as measured for acceptability included any ED patients, even those without pain. Despite different designs, populations, and sample sizes, these studies, like ours, suggest that acupuncture in the ED is feasible. We also determined that a high percentage (73.3%) of ED providers placed referrals for acupuncture. Acceptability by providers was not reported in the other studies; however, they reported additional measures not included in our pilot. Zhang and colleagues measured patient satisfaction with and willingness to repeat acupuncture, with high scores for both. And Arnold et al. found that acupuncture did not extend patients’ time in the ED.
Our findings of reduced pain in ED patients treated with acupuncture are generally consistent with the small body of pilot investigations. In the large observational study of 400 ED patients conducted by Zhang et al., the authors found that those patients who received acupuncture reported significant pain decreases of about 2.3 points on the 11-point scale [24]. Arnold’s observational study of 20 ED patients presenting with minor acute trauma to the extremities found that median visual analogue scale scores significantly decreased by 20.5 mm compared to pre-acupuncture scores [21]. One randomized controlled trial of 100 participants found significantly higher pain reduction in the acupuncture plus standard care group compared to the standard care alone group when using auricular acupuncture [22], while a second randomized controlled trial of 45 patients reported no significant differences between the acupuncture and conventional treatment groups [23]. A pilot cohort study of acupuncture for low back pain in an ED in Taiwan compared acupuncture with sham acupuncture and found a significant pain reduction in the experimental but not the control (sham) group [25]. To our knowledge, no prior investigations have investigated the utilization of acupuncture to reduce anxiety in the ED or were able to compare pain reduction across patients receiving or not receiving analgesics.
Our study demonstrated that acupuncture, as an adjunct to usual care, is beneficial in managing pain and anxiety in ED patients. Using this integrative therapy, hospitals may be able to provide a more holistic approach to pain and anxiety management within a large and busy ED setting. In light of ED patient concerns and misconceptions regarding the use of opioid pain medications [6,7], introducing a nonpharmacologic option for pain management has the potential to offset some medication use, potentially reducing risks and side effects in patients for whom this complementary treatment works.
Scientific evidence suggests a close relationship between pain and anxiety, and some research suggests that this relationship may be particularly relevant in the ED [33]. The results from the current study show that changes in pain and anxiety are correlated within our ED patient population. It was beyond the scope of the present study to further investigate the depth of the relationship between anxiety and pain. It is well-documented that acupuncture effectively treats pain and anxiety among various patient populations [15–20]. In the ED, future research on acupuncture should further investigate the possible interaction between pain and anxiety, whether acupuncture could reduce pain without analgesics, and a future focus on understanding for which patients acupuncture within the ED setting may be most beneficial.
While we must be cautious about overstating the potential benefits of offering acupuncture in the ED, it is worth noting the widespread problem of prescription pain medication misuse and addiction, which can stem from initial exposure to these medications in health care settings such as primary and emergency care [34]. In the United States, prescriptions written for painkillers have skyrocketed from approximately 76 million in 1991 to nearly 207 million in 2013 [4]. According to the CDC, prescription drug abuse is the fastest growing drug problem in the United States, driven by increased use of prescribed opioids—which are responsible for more overdose deaths than heroin and cocaine combined [35]. While there are some existing efforts to limit opioid exposure, such as low pill counts in opioid prescriptions written at ED discharge [36], the serious adverse effect profile of opioids may be underappreciated given their common use in the ED. For example, there is evidence that for “opioid-naïve” patients who visit the ED, that is, those patients who have not had an opioid prescription within one year of the ED visit, filling a prescription puts them at significant risk of recurrent opioid use after discharge compared with opioid-naïve patients who do not fill their prescriptions [34].
Given the rapid increase in opioid prescriptions for pain and the corresponding increased risk of opioid abuse—as well as the risk of adverse effects—it seems evident that the existing treatments for acute pain do not address the problem fully [37]. Low-risk, effective approaches to relieve acute pain in the ED are needed to assist US health systems with mitigating this epidemic. Acupuncture has the potential to be a tool for hospitals to address pain in addition to the medication-based care already being delivered.
Conclusions
This pilot study provided a unique opportunity to describe and investigate the effectiveness of providing acupuncture therapy to patients in the ED. Our results suggest that acupuncture is well-accepted by both medical providers and patients and that acupuncture contributes to reducing both pain and anxiety in this setting.
Funding sources: This work was partially supported by the National Center for Complementary & Alternative Medicine of the National Institutes of Health (grant number R01 AT006518-01 to JD). The work was also supported by the Abbott Northwestern Hospital Foundation, the Rob and Kris Johnson Family Foundation and the Penny George Institute Foundation.
Conflicts of interest: The authors declare no conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Downey LV, Zun LS. Pain management in the emergency department and its relationship to patient satisfaction. J Emerg Trauma Shock 2010;3(4):326–30. DOI 10.4103/0974-2700.70749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang HY, Daubresse M, Kruszewski SP, Alexander GC. Prevalence and treatment of pain in EDs in the United States, 2000 to 2010. Am J Emerg Med 2014;32(5):421–31. [DOI] [PubMed] [Google Scholar]
- 3.Cantrill S, Brown M, Carlisle R, et al. Clinical policy: Critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med 2012;60(4):499–525. [DOI] [PubMed] [Google Scholar]
- 4.Volkow N. America's addiction to opioids: Heroin and prescription drug abuse. Paper presented at Senate Caucus on International Narcotics Control. Washington, DC; 2014.
- 5.Mazer-Amirshahi M, Mullins P, Rasooly I, van den Anker J, Pines J. Rising opioid prescribing in adult U.S. emergency department visits: 2001-2010. Acad Emerg Med 2014;21(3):236–43. [DOI] [PubMed] [Google Scholar]
- 6.Smith RJ, Rhodes K, Paciotti B, et al. Patient perspectives of acute pain management in the era of the opioid epidemic. Ann Emerg Med 2015;66(3):246–252.e1. [DOI] [PubMed] [Google Scholar]
- 7.Conrardy M, Lank P, Cameron KA, et al. Emergency department patient perspectives on the risk of addiction to prescription opioids. Pain Med 2015; DOI 10.1111/pme.12862. [DOI] [PubMed] [Google Scholar]
- 8.O'Connor AB, Zwemer FL, Hays DP, Feng C. Outcomes after intravenous opioids in emergency patients: A prospective cohort analysis. Acad Emerg Med 2009;16(6):477–87. [DOI] [PubMed] [Google Scholar]
- 9.Frass M, Strassl RP, Friehs H, et al. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: A systematic review. Ochsner J 2012;12(1):45–56. [PMC free article] [PubMed] [Google Scholar]
- 10.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 2008;(12):1–23. [PubMed] [Google Scholar]
- 11.Kong S, Zhang YH, Liu CF, et al. The complementary and alternative medicine for endometriosis: A review of utilization and mechanism. Evid Based Complement Alternat Med 2014;2014:146383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cowan RP. CAM in the real world: You may practice evidence-based medicine, but your patients don’t. Headache 2014;54(6):1097–102. [DOI] [PubMed] [Google Scholar]
- 13.Dossett ML, Davis RB, Lembo AJ, Yeh GY. Complementary and alternative medicine use by US adults with gastrointestinal conditions: Results from the 2012 National Health Interview Survey. Am J Gastroenterol 2014;109(11):1705–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahall M. Complementary and alternative medicine usage among cardiac patients: A descriptive study. BMC Complement Altern Med 2015;15:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao P, Gao XI, Fu T, Xu D, Wen Q. Acupuncture: Emerging evidence for its use as an analgesic (Review). Exp Ther Med 2015;9(5):1577–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sniezek DP, Siddiqui IJ. Acupuncture for treating anxiety and depression in women: A clinical systematic review. Med Acupunct 2013;25(3):164–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarris J, Moylan S, Camfield DA, et al. Complementary medicine, exercise, meditation, diet, and lifestyle modification for anxiety disorders: A review of current evidence. Evid Based Complement Alternat Med 2012;2012:809653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pilkington K. Acupuncture therapy for psychiatric illness. Int Rev Neurobiol 2013;111:197–216. [DOI] [PubMed] [Google Scholar]
- 19.Pilkington K, Kirkwood G, Rampes H, Cummings M, Richardson J. Acupuncture for anxiety and anxiety disorders–a systematic literature review. Acupunct Med 2007;25(1-2):1–10. [DOI] [PubMed] [Google Scholar]
- 20.Mendelson GE, et al. Is acupuncture effective for the treatment of chronic pain? A systematic review, PAIN 86(2000)217-225. Pain 2001;93(2):198–200. [DOI] [PubMed] [Google Scholar]
- 21.Arnold AA, Ross BE, Silka PA. Efficacy and feasibility of acupuncture for patients in the ED with acute, nonpenetrating musculoskeletal injury of the extremities. Am J Emerg Med 2009;27(3):280–4. [DOI] [PubMed] [Google Scholar]
- 22.Goertz C, Niemtzow R, Burns S, et al. Auricular acupuncture in the treatment of acute pain syndromes: A pilot study. Mil Med 2006;171(10):1010–4. [DOI] [PubMed] [Google Scholar]
- 23.Harkin C, Parker R. A prospective, randomised control trial of acupuncture for select common conditions within the emergency department. J Chinese Med 2007;85:45–52. [Google Scholar]
- 24.Zhang AL, Parker SJ, Smit de V, Taylor DM, Xue CC. Acupuncture and standard emergency department care for pain and/or nausea and its impact on emergency care delivery: A feasibility study. Acupunct Med 2014;32(3):250–6. [DOI] [PubMed] [Google Scholar]
- 25.Liu YT, Chiu CW, Chang CF, et al. Efficacy and safety of acupuncture for acute low back pain in emergency department: A pilot cohort study. Evid Based Complement Alternat Med 2015;2015: 179731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim K, Lee B, Ryu J, Choi T, Yang G. The role of acupuncture in emergency department settings: A systematic review. Complement Ther Med 2013;21(1):65–72. [DOI] [PubMed] [Google Scholar]
- 27.Knutson L, Johnson PJ, Sidebottom A, Fyfe-Johnson A. Development of a hospital-based integrative healthcare program. J Nurs Adm 2013;43(2):101–7. [DOI] [PubMed] [Google Scholar]
- 28.Dusek JA, Finch M, Plotnikoff G, Knutson L. The impact of integrative medicine on pain management in a tertiary care hospital. J Patient Saf 2010;6(1):48–51. [DOI] [PubMed] [Google Scholar]
- 29.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med 2009;36(5): 452–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gerbershagen HJ, Rothaug J, Kalkman CJ, Meissner W. Determination of moderate-to-severe postoperative pain on the numeric rating scale: A cut-off point analysis applying four different methods. Br J Anaesth 2011;107(4):619–26. [DOI] [PubMed] [Google Scholar]
- 31.Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med 2003;10(4):390–2. [DOI] [PubMed] [Google Scholar]
- 32.Acute Pain Management Guideline Panel. 2. Process of Pain Assessment and Reassessment (AHCPR Clinical Practice Guidelines, No. 1) Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: Agency for Health Care Policy and Research (AHCPR; ); 1992. [Google Scholar]
- 33.Craven P, Cinar O, Madsen T. Patient anxiety may influence the efficacy of ED pain management. Am J Emerg Med 2013;31(2):313–8. [DOI] [PubMed] [Google Scholar]
- 34.Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med 2015;65(5):493–9.e494. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Policy Impact: Prescription Painkiller Overdoses. Atlanta, GA: US Department of Health and Human Services; 2011. [Google Scholar]
- 36.Hoppe JA, Nelson LS, Perrone J, Weiner SG. Opioid prescribing in a cross section of US emergency departments. Ann Emerg Med 2015;66(3): 253–9.e251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosenblum A, Marsch L, Joseph H, Poetenoy R. Opioids and the treatment of chronic pain: Controversies, current status, and future directions. Exp Clin Psychopharmacol 2008;16(5):405–16. [DOI] [PMC free article] [PubMed] [Google Scholar]