Abstract
Background
Community survey data suggest high prevalence of substance use disorders among currently homeless individuals. There is less data regarding illicit drug and alcohol use problems of homeless-experienced persons engaged in primary care. They may have less severe use and require different care responses from primary care teams.
Methods
We surveyed currently and formerly homeless, i.e., homeless-experienced, persons engaged in primary care at 5 federally-funded programs in the U.S., administering the World Health Organization (WHO) Alcohol, Smoking and Substance Involvement Screening Test (ASSIST). We used the ASSIST definitions of lower, moderate, and high risk to assess a spectrum of lifetime and recent substance use, from any use to likely dependence, and to identify sociodemographic and health status characteristics associated with severity of use.
Results
Almost one-half of the sample (n = 601) had recently (within the past 3 months) used alcohol, and one-third had recently used an illicit drug. The most commonly used illicit drugs in the past 3 months were cannabis (19%), cocaine (16%), and opioids (7.5%). Over one-half (59%) of respondents had ASSIST-defined moderate or high risk substance use. A significant proportion (31%) of those identified as at moderate risk had no recent substance use, but did report past problematic use. Ten percent of the lower risk group had past problematic use of alcohol. Severity of use was associated with worse health status, but not with housing status or type of homelessness experienced.
Conclusions
Less severe (moderate risk) use and past problematic use, potentially indicative of remitted substance use disorders, were more common than high risk use in this primary care, homeless-experienced sample. Our findings highlight the urgency of identifying effective ways to reduce risky substance use and prevent relapse in homeless-experienced persons.
Keywords: Substance use, homeless, primary care
INTRODUCTION
There is growing recognition that homeless-experienced persons require primary care tailored to their complex health challenges, including substance use.1--4 Substance use disorders (SUDs) involving alcohol and illicit drugs are strongly associated with homelessness, with prevalence sometimes exceeding 50% in community homeless samples.5--10 Alcohol and drug use contributed to one-third of deaths among homeless adults in a primary care program.11,12 Given the prevalence of SUDs in this population, the two U.S. federal programs that fund primary care for homeless persons -- the Department of Health and Human Services (HHS) Health Care for Homeless programs13 and the Department of Veteran Affairs (VA) Homeless Patient-Aligned Care Teams14 -- have explicitly committed (and in the case of HHS, are legally mandated) to address substance abuse.15,16
The aforementioned community surveys could lead primary care teams to expect a high prevalence of severe SUDs among homeless-experienced patients.5--10 However, detailed data on SUD among homeless-experienced persons in primary care are lacking. One study of homeless patients at Federally Qualified Health Centers (FQHCs) reported dependence prevalence of 12-15% and binge drinking in 40%.17 Further characterization of risky use or prior history of disorder were not reported, but may be more common. In a medical records review of homeless and formerly homeless patients, 60% had “any substance use disorder,” but no distinction was made between active and remitted disorder.18 Neither study reported specific drugs used.
Much of the clinical guidance offered to primary care teams concerns currently homeless persons in need of addiction treatment.19 However, homeless-experienced patients often seek housing as they enter primary care; they could be more stable than persons in emergency shelters or on the street. Thus, dependence or “any SUD” does not provide the detail or breadth necessary to understand the spectrum of substance use and SUD among homeless-experienced persons accessing primary care, whose needs may extend beyond addiction treatment. Clarifying the severity, particular substances used, and extent of current versus remitted disorders is crucial because the expected treatment and triage response resources would differ depending on the severity of problems presented. Risky substance use exacerbates chronic medical and psychiatric conditions,20,21 which are associated with homelessness.6,22 Maintaining SUD remission may require social support,23,24 often lacking among homeless-experienced individuals.25 Recommendations for effective treatment vary according to substance.26,27 Finally, ongoing or remitted SUD is a contextual factor that may influence the care plan for conditions ranging from hypertension to chronic pain.28
To remedy this knowledge gap, we present data from a geographically-diverse sample of currently and previously homeless persons, all engaged in primary care. The study objective is to describe a spectrum of lifetime and recent substance use, from any use to likely dependence, and to identify sociodemographic and health status characteristics associated with severity of use.
METHODS
This is a secondary analysis of data from the Primary Care Quality-Homeless (PCQ-H) study.29 The objective of the PCQ-H study was to develop a survey to measure primary care experiences among homeless and formerly homeless patients (the PCQ-H-33).30 Study participants were recruited from five federally-funded primary care organizations: four VA sites in Alabama, Pennsylvania, and California, and one HCH program in Massachusetts.29
Participants
A random sample of currently or previously homeless persons engaged in primary care was recruited for participation (n = 601). Eligibility was based on having had at least two primary care visits at the participating sites in the preceding two years, and having experienced homelessness.29,30 Research associates administered a one-time, in-person standardized survey to participants between January, 2011 and March, 2012. The full sample is used here. This analysis was approved by the Birmingham VA Medical Center Institutional Review Board (IRB) and deemed IRB-exempt at Washington University.
Measures
Substance use was assessed using the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) Version 3.0 of the World Health Organization (WHO), a tool developed for primary care.31 It identifies hazardous use of alcohol, cannabis, cocaine, amphetamines, sedatives/benzodiazepines, hallucinogens, inhalants, and opioids.31 To describe substance use severity, we use the lower, moderate, and high levels of risk as defined by the WHO. At the lower and moderate levels, risk refers to “risk of health and other problems from [your] current pattern of substance use.” At the high level, risk refers to “risk of experiencing severe problems (health, social financial, legal, relationship) as a result of [your] current pattern of use.”32(p49) High risk indicates likely DSM-IV dependence.32,33 The ASSIST has discriminative and predictive validity for substance use disorder diagnoses.32,33 It has been used to measure substance dependence in homeless samples.17
The ASSIST items query lifetime and recent (past 3 months) use of each substance. For recently used substances, it assesses: frequency of use; urges to use; health, social, legal, or financial problems; and interference with role responsibilities. For each substance ever used, the ASSIST queries failed attempts to reduce use, and whether a friend, relative, or health care provider ever expressed concern about their use; a follow-up question determines if this occurred in the past 3 months or more than 3 months ago. These two questions are asked regardless of whether the respondent used the substance in the past 3 months. The ASSIST weights answers based on a 1047-person validation study.34
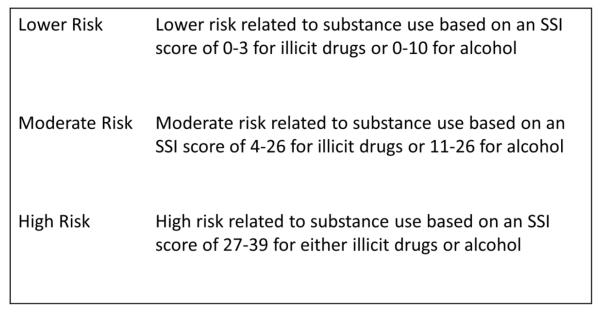
A Specific Substance Involvement (SSI) score is calculated for each substance (range: 0-39). Figure 1 indicates the ASSIST-defined risk levels based on SSI scores, as used for this analysis. We devised the term “past problematic use” to refer to having ever had failed attempts to quit and having others express concern about their use, with no use of that substance in 3 months. In addition to age, gender, race and ethnicity, we collected socioeconomic data regarding difficulties paying for basics (food, shelter, or utilities), insurance status, education, and recent work history.
Figure 1.
WHO risk categories as assessed by Specific Substance Involvement (SSI) scores on the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) Version 3.0.
Social support was measured with the “strong ties” scale (range: 3-15). The scale has demonstrated validity35 and is inversely associated with emotional distress in homeless persons.25 Respondents report how frequently they are bothered by not having a close companion, not having enough friendships, and not seeing enough of the people to whom they feel close. Higher scores indicate more social support.35
Current housing status and type of homelessness is based on federal definitions.36,37 Current housing status is either housed or homeless, where homelessness includes sleeping outdoors or other places not meant for sleeping, staying in temporary accommodations for homeless persons, or “doubling up” with relatives or friends with no assurance of being able to stay long-term.
Type of homelessness refers to having ever experienced chronic homelessness, defined as 4 or more episodes in the past 3 years, or a continuous episode of homelessness lasting at least one year. We combined these two variables to create four categories: currently chronically homeless; currently non-chronically homeless; currently housed, previously chronically homeless; and currently housed, never chronically homeless.
Health status was assessed by asking participants about lifetime diagnoses of 14 chronic medical conditions and diagnoses of 23 episodic health conditions in the past 6 months. These conditions are associated with mortality38 and health-related quality of life22 in homeless and substance-using adults. Mental health status was assessed with the Colorado Symptom Index (CSI), an instrument validated in homeless populations; higher scores indicate higher distress.39--41
Less than 4% of data were missing for each variable.
Analysis
Descriptive statistics were calculated as appropriate. To identify sociodemographic and health characteristics associated with WHO-designated risk categories, we placed respondents in mutually exclusive groups of lower, moderate, and high risk based on their highest SSI score, e.g., respondents with lower risk alcohol use and moderate risk cocaine use were classified as “moderate risk.” Bivariate tests of association with risk categorization were calculated using t-tests, ANOVAs, and Pearson’s chi-square. To identify characteristics independently associated with WHO-designated moderate or high risk, we analyzed a multivariable binomial logistic regression model, with the lower risk group as the referent. The moderate and high risk groups were combined because of the small number of high risk respondents, and because the ASSIST is better at distinguishing between low and moderate risk than between moderate and high risk.33 The final model retained all sociodemographic and health variables analyzed bivariately, with one exception; “difficulty paying for basics” was dropped due to missing data from 3.8% of respondents (n = 24) and because of construct overlap with housing status. To assist interpretation, continuous variables were modeled as the effect of a 1-standard deviation increase above the mean. Statistics were calculated using SAS© version 9.4.
The odds of being in the combined group of moderate or high risk differed significantly across the five recruitment sites (χ = 13.3, p = .01). A null multi-level model was assessed to estimate the variation explained by site; an intraclass correlation coefficient (ICC) was calculated using fixed variance for level-1 residuals as recommended for logistic models.42 The ICC was very low (0.023, or 2.3% of variance), indicating that the variation in risk cannot be accounted for at the site level. It would be misleading to retain recruitment site as an individual-level variable. Thus, while a multilevel interpretation would be inappropriate, we used a multilevel model that calculated the adjusted odds ratios based on correlated outcomes within sites, using the SAS© GLIMMIX procedure. Variation across site is addressed in the discussion.
RESULTS
Sample
The sample (n = 601) was mostly male (85%), with an average age of 53 [range: 22-78] and over one-half identifying as Black, non-Hispanic (Table 2). Two-thirds of the respondents were recruited at VA sites. Most respondents (69%) were currently housed; two-thirds had ever experienced chronic homelessness. Of those who were currently homeless (n = 185), 17% had not experienced chronic homelessness, representing just 5% of the sample. There were no differences on any of the variables between respondents who were currently non-chronically homeless and respondents who were currently chronically homeless, so we combined them into a “currently homeless” category for the analyses.
Table 2.
Characteristics of Homeless-Experienced Persons in Primary Care, by Highest Specific Substance Involvement Score (N = 601)
| All | Lower Risk N = 244 (41%) |
Moderate Risk N = 297 (49%) |
High Risk N = 60 (10%) |
p | |
|---|---|---|---|---|---|
| n (% of sample) |
n (% of risk group) |
n (% of risk group) |
n (% of risk group) |
||
| Demographics | |||||
| Male, % | 512 (86) |
208 (85) |
254 (86) | 50 (83) | 0.96 |
| Self-identified race and ethnicity, % | 0.05 | ||||
| White non-Hispanic | 183 (30) |
81 (33) | 83 (28) | 19 (32) | |
| Black non-Hispanic | 345 (57) |
135 (55) |
181 (61) | 29 (48) | |
| Hispanic | 30 (5) | 11 (5) | 17 (6) | 2 (3) | |
| Other race | 43 (7) | 17 (7) | 16 (5) | 10 (17) | |
| Age, Mean [SD] | 53.1 [8.3] |
55.4 [8.2] |
52.4 [7.6] |
47.3 [9.3] |
<0.0001 |
| Socioeconomic Status, % | |||||
| Difficulty paying for food, shelter, or utilities |
394 (66) |
141 (58) |
208 (70) | 45 (75) | 0.01 |
| Insurance for medical expenses | 544 (91) |
211 (86) |
275 (93) | 58 (97) | 0.01 |
| More than high school education | 268 (45) |
119 (49) |
128 (43) | 21 (35) | 0.05 |
| Full- or part-time work in past 3 months | 111 (18) |
45 (18) | 58 (20) | 8 (13) | 0.52 |
| Social Support, Mean [SD] | 10.1 [3.6] |
10.5 [3.6] |
10.1 [3.5] |
8.0 [3.3] | <0.0001 |
|
Current Housing Status and Type of
Homelessness, % |
0.08 | ||||
| Currently housed, never chronically homeless |
165 (27) |
77 (32) | 78 (26) | 10 (17) | |
| Currently housed, previously chronically homeless |
250 (42) |
100 (41) |
126 (43) | 24 (40) | |
| Currently homeless | 185 (31) |
67 (27) | 92 (31) | 23 (43) | |
| Health and Mental Health Status | |||||
| Chronic medical conditions (of 14), Mean [SD] |
2.7 [1.8] |
2.7 [1.7] |
2.7 [1.9] | 2.3 [1.9] | 0.27 |
| Episodic health conditions (of 23), Mean [SD] |
1.4 [1.7] |
1.2 [1.7] |
1.4 [2.0] | 2.2 [2.5] | 0.0001 |
| Psychological distress, Mean [SD] | 17.0 [11.5] |
14.6 [11.2] |
17.2 [10.7] |
25.4 [12.3] |
<0.0001 |
Lifetime and recent substance use
Nearly all respondents reported lifetime use of alcohol (95%) or illicit drugs (90%). However, almost one half (46%, n = 276) were recently (past 3 months) abstinent. One-half had recently used alcohol, and one-third had recently used illicit drugs. Lifetime and recent illicit drug use was most common for cannabis (84% lifetime, 19% recent) and cocaine (76% lifetime, 16% recent). A smaller percentage reported recent use of opioids (7.5%) and sedatives (6.5%).
Risk related to use of specific substances
Lower risk use (based on the WHO ASSIST), which includes abstinence, was the most common pattern for all substances. ASSIST-designated moderate risk for alcohol, cannabis, and cocaine use affected one-quarter to one-third of respondents (Table 1). Prevalence of moderate risk due to any illicit drug use was 52%; the prevalence of high risk illicit drug use was 6% (not shown in Table). The total prevalence of moderate risk substance use, including alcohol, was 57% (n = 340); the total prevalence of high risk substance use, indicating likely dependence, was 10%.
Table 1.
Prevalence of Lower, Moderate, and High Risk of Experiencing Health and Other Problems Due to Use of Specific Substances among Homeless-Experienced Persons in Primary Care (N = 601)
| Alcoh ol |
Cannab is |
Cocain e |
Amphetamin es |
Inhalan ts |
Sedativ es |
Hallucinoge ns |
Opioi ds |
|
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Lower Risk |
434 (72) |
423 (70) |
378 (63) |
557 (93) | 580 (97) |
537 (89) |
567 (94) | 504 (84) |
| Modera te Risk |
136 (23) |
171 (28) |
198 (33) |
43 (7) | 21 (3) | 59 (10) | 34 (6) | 85 (14) |
| High Risk |
31 (5) | 7(1) | 25 (4) | 1 (<1) | 0 (0) | 5 (1) | 0 (0) | 12 (2) |
Past problematic use
Past problematic drug use (defined as having ever failed to reduce use and having others express concern about use, with no use in the past 3 months) characterized 41% of the 289 respondents classified on the ASSIST as having “moderate risk” drug use. Past problematic alcohol use characterized 22% of the 434 respondents classified on the ASSIST as having “lower risk” alcohol use.
The extent to which respondents met the ASSIST’s moderate risk thresholds due to recent use, rather than past problematic use, varied by drug. Respondents with moderate risk sedative and cannabis use were more likely than not to have recently used these substances (53% for sedatives and 57% for cannabis). On the other hand, two-thirds of respondents classified as moderate risk for cocaine use had not recently used cocaine. This figure was similar for opioids (61%). For the remaining drugs, the vast majority of moderate risk was due to past problematic use rather than recent use: amphetamines (98%), inhalants (85%), and hallucinogens (94%).
Respondents with past problematic use of a substance were not necessarily abstinent, however; between 12% and 16% of respondents with past problematic use of cocaine and opioids had recent moderate risk use of cannabis or alcohol, and 14% of respondents with past problematic opioid use had recent moderate risk use of cocaine.
Patient risk groups based on highest specific substance involvement (SSI) score
When respondents were grouped based on their highest SSI score, over one-half (59%) met ASSIST criteria for moderate (49%) or high (10%) risk substance use, irrespective of how recently they had used (Table 2). There are two groups with past problematic use and no recent use. Nearly one-third of the moderate risk group (n = 92 of 297) had no recent illicit drug or alcohol use, but nonetheless met ASSIST criteria for moderate risk based on their report of past problematic drug use. Additionally, 10% of the ASSIST-designated lower risk group (n = 24 of 244) reported past problematic alcohol use. Summing these two, 116 persons (19% of the 601-person sample) had past problematic use of drugs or alcohol without recent use.
Characteristics of homeless-experienced persons in primary care, by highest SSI
As shown in Table 2, “high risk” respondents (their highest SSI score met ASSIST criteria for high risk use) were younger, least likely to have post-high school education, and more likely to have medical insurance. They were most likely to indicate difficulty paying for basic needs. A higher-than-expected proportion of people reporting “Other race” was high risk.
High risk respondents reported worse health and mental health status. They had the greatest psychological distress, scoring a standard deviation higher on the CSI compared to the lower risk group. They reported more episodic health conditions. The moderate and lower risk groups had a slightly higher average number of chronic medical conditions (2.7) than the high risk group (2.3), but this was nonsignificant (p = .27). The high risk group also reported the lowest social support. In general, differences were greatest between the high and lower risk groups, with the moderate risk group intermediate.
Current housing status and type of homelessness was not associated with ASSIST-designated substance use risk level (p = .08). Among those who were currently housed (n = 415), there were no statistically significant differences on risk status between those who had experienced chronic homelessness and those who had not (p = .25).
Respondents recruited from the four VA primary care sites were underrepresented in the high risk group. They constituted two-thirds of the overall study sample but 40% of the high risk group. At the VA study sites, between 4% and 7% of study participants qualified as high risk for at least one substance; at the HCH site, 18% did (p < .0001).
Characteristics associated with being at moderate or high risk, adjusting for covariates
The analytic sample size for the multivariable model was 574 (Table 3). ASSIST-defined moderate or high risk was independently associated with younger age, male gender, and Black, non-Hispanic race, but not socioeconomic status or social support. The moderate/high risk group also reported greater psychological distress and more episodic health conditions, but not more chronic medical conditions. Current housing status and type of homelessness was not associated with ASSIST-defined moderate or high risk.
Table 3.
Adjusted Odds Ratios of Being at ASSIST-Defined Moderate or High Risk Due to Substance Use, among Homeless-Experienced Persons in Primary Care (n = 574) (referent: Lower Risk)
| Adjusted Odds Ratio [95% CI] |
p-value | |
|---|---|---|
| Demographics | ||
| Gender | ||
| Female | --- | .04 |
| Male | 1.78 [1.02 -- 3.10] | |
| Self-identified race and ethnicity | ||
| White non-Hispanic | --- | |
| Black non-Hispanic | 1.66 [1.08 -- 2.53] | .02 |
| Hispanic | 1.08 [0.40 -- 2.90] | .88 |
| Other race | 1.02 [0.47 -- 2.18] | .97 |
| Age (+1 SD) | 0.63 [0.50 -- 0.78] | <.0001 |
| Socioeconomic Status | ||
| Insurance for medical expenses | 1.50 [0.78 -- 2.90] | .23 |
| More than high school education | 0.75 [0.52 -- 1.07] | .11 |
| Full- or part-time work in past 3 months | 1.11 [0.70 -- 1.77] | .66 |
| Social Support (+1 SD) | 0.91 [0.74 -- 1.11] | .35 |
| Current Housing Status and Type of Homelessness | ||
| Currently housed, never chronically homeless | --- | |
| Currently housed, previously chronically homeless | 1.06 [0.66 -- 1.72] | .81 |
| Currently homeless | 1.08 [0.69 -- 1.71] | .73 |
| Health and Mental Health Status | ||
| Each additional chronic medical condition (of 14) | 0.96 [.86 -- 1.08] | .51 |
| Each additional episodic health condition (of 23) | 1.15 [1.01 -- 1.30] | .04 |
| Psychological distress (+1 SD) | 1.30 [1.03 -- 1.63] | .02 |
DISCUSSION
The study objective was to describe a spectrum of lifetime and recent substance use in a primary care (PC)-engaged homeless-experienced sample, from any use to likely dependence, and to identify sociodemographic and health characteristics associated with severity of use. The most common pattern of use in our sample was not dependence, as might be expected given the high prevalence of SUD in community studies of homeless persons, but recent, moderate risk use of cannabis, alcohol, or cocaine. The total proportion at moderate or high risk (59%) broadly agrees with previous research.10,18 However, our study was among the first to describe a range of substance use, and not just dependence,17 among formerly and currently homeless primary care patients across the US. Our study also offered more precise examination of homelessness (past and current as well as chronicity) than previous studies of homeless primary care patients,17,18 however, we found that current housing status or chronic homelessness was not a significant predictor of risk.
Our study highlights a substantial number of respondents classified as moderate risk (49%). For one third of these, this was due to past problematic use of illicit drugs; this is in addition to the 10% of respondents with past problematic use of alcohol. Nearly one-half of the study sample reported abstinence from drugs and alcohol. However, 19% of the overall sample also reported past problematic use with recent abstinence. This may indicate remitted SUDs, a relevant clinical status not readily picked up by the ASSIST scoring criteria unless close attention is paid to questions about past attempts to quit and expressions of concern from others.
In multivariable analysis, WHO-designated moderate/high risk ASSIST score was associated with younger age, greater number of episodic health conditions, male gender, and psychological distress, consistent with general population studies.43--46 Self-identified Black race was also independently associated with WHO-designated moderate/high risk (Table 3). This finding has mixed support in the literature; Black race is associated with lower risk of substance use and SUDs, but also lower likelihood of remission45,47,48 and greater social consequences.49
The spectrum of drug and alcohol use in this sample entails some clinical risk, even when criteria for a formal diagnosis are not met. Less severe substance use is associated with cancer risk, poor hypertension control, and worse mental health.20,21 Less severe substance use is particularly significant for homeless persons, who are at greater risk of falls and injuries.50 Persons with past problematic use, especially with ongoing use of other substances, incur risk of relapse.51,52
Clinical guidance on how primary care teams can reduce risky substance use for any population, let alone homeless-experienced persons, is limited.53,54 The effectiveness of formal service packages such as Screening, Brief Intervention and Referral to Treatment to reduce alcohol and drug use have been mixed.55--59 Gordon and Haibach, recognizing time constraints in primary care, argue for global wellness programs for patients with multiple health problems, including unhealthy substance use.60 Friedmann et al. offer guidance on relapse prevention, which may be relevant for homeless-experienced patients with past problematic use.24 Many of their recommendations set the stage for a supportive primary care relationship in the event of a future relapse, including regular follow-up, mobilization of social support, medication-assisted therapy, and management of depression, anxiety and other comorbid conditions.
Successfully carrying out these recommendations requires attention to relevant contextual factors that may mean individualizing care.28,61,62 For example, SUD increases risk for overdose with prescription opioids, necessitating adjustments in chronic pain care.63 Similarly, socioeconomic status and extent of social support are contextual factors that could influence how primary care teams respond to substance use.28,61,62 In our sample, these contextual factors varied significantly across substance use risk groups. Importantly, attending to these aspects of life context may require a longitudinal care relationship.55,64,65
Our study has limitations. The ASSIST does not explicitly assess lifetime disorders. ASSIST only asks two questions regarding substance use prior to the past 3 months; for this reason, we do know how recently the “past problematic use” occurred, or its severity. The ASSIST imposes a higher “moderate risk” numeric threshold for alcohol use (≥11) than for drug use (≥4). This may underestimate alcohol-related risk, and misses past problematic use. This is of particular concern given the extent of alcohol-related problems among homeless-experienced persons.66--68
Despite the lack of prior validation of the ASSIST in homeless populations, it has been used in homeless patients.17 WHO’s validation among 1047 respondents from 7 countries suggests broad applicability.33,34 Additional reassurance can be drawn from our Table 2, which shows that progression across ASSIST risk groups is associated with increasing health, social, and financial problems. This argues for the ASSIST having criterion validity in homeless populations. Finally, self-report faces limitations of social desirability bias;69 under-reporting is expected. However, the magnitude of under-reporting is not worse for homeless populations.70 The ASSIST itself was validated against biologic measures of drug use,33,34 which are themselves imperfect.
The participating sites were purposively selected to represent a range of federally-funded approaches to primary care service delivery for homeless persons.29 This resulted in a sample that was two-thirds veterans, compared to 12% in the adult homeless population.71 This purposive site sampling, rather than veteran status per se, likely contributed to the overrepresentation of HCH patients in the high risk group, compared to the VA patients. The HCH program was selected in part because its model of care includes extensive outreach to homeless persons on the streets and in emergency shelters,1 which likely enriched the HCH sample with persons having more severe drug and alcohol use. A recent comparison between homeless veterans and non-veterans found no differences in housing or clinical characteristics, including addiction severity.72
Conclusion
Less severe use and past problematic use, which may be indicative of remitted SUDs, were especially common in this diverse sample of homeless-experienced persons using primary care. These findings highlight the urgency of identifying effective ways to reduce risky substance use and prevent relapse in homeless-experienced persons, and may sensitize care teams to the importance of past problematic use as a relevant contextual factor in making health care decisions.
Acknowledgments
FUNDING
The Department of Veterans Affairs, Health Services Research & Development Branch (Grant IAA-07-069-2) provided funding for the data collection on which this analysis is based.
The Social Work Training in Addictions Research Institutional Predoctoral Fellowship (T32 DA015035) through the National Institute on Drug Abuse (NIDA) provided funding for the writing of this manuscript.
Footnotes
AUTHOR CONTRIBUTIONS
Ms. Stringfellow and Drs. Kim, Pollio, Gordon, and Kertesz contributed to research conception and design, data collection, analysis, and interpretation of the results as well as writing and revision of the manuscript. Ms. Johnson contributed to data collection and initial review of the manuscript. Drs. Grucza and Austin contributed to analysis of the results and in revisions of the manuscript.
While the authorship team has no commercial conflict of interest, most authors have past or present employment relationships with the entities studied in this paper (4 VA health care centers and 1 Health Care for Homeless program). The Health Care for Homeless Program has employed authors Kertesz, Kim, and Stringfellow, the VA institutions have employed authors Austin, Gordon, Johnson, and Kertesz. Dr. Pollio received compensation for research services from the VA. Dr. Grucza has no affiliation with the institutions.
REFERENCES
- 1.O’Connell JJ, Oppenheimer SC, Judge CM, et al. The Boston health care for the homeless program: A public health framework. Am J Public Health. 2010;100(8):1400–8. doi: 10.2105/AJPH.2009.173609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Toole TP, Pirraglia PA, Dosa D, et al. Building care systems to improve access for high-risk and vulnerable veteran populations. J Gen Intern Med. 2011;26(Suppl 2):683–688. doi: 10.1007/s11606-011-1818-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsai J, Rosenheck RA, Culhane DP, Artiga S. Medicaid expansion: Chronically homeless adults will need targeted enrollment and access to a broad range of services. Health Aff. 2013;32(9):1552–1559. doi: 10.1377/hlthaff.2013.0228. [DOI] [PubMed] [Google Scholar]
- 4.O’Toole TP, Pape L, Kane V. Ending homelessness-then what? Am J Public Health. 2013;103(S2):S185–S187. doi: 10.2105/AJPH.2013.301730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palepu A, Gadermann A, Hubley AM, et al. Substance use and access to health care and addiction treatment among homeless and vulnerably housed persons in three Canadian cities. PLoS One. 2013;8(10):e75133. doi: 10.1371/journal.pone.0075133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caton CLM, Dominguez B, Schanzer B, et al. Risk factors for long-term homelessness: Findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005;95(10):1753–1759. doi: 10.2105/AJPH.2005.063321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Toole TP, Gibbon JL, Hanusa BH, Freyder PJ, Conde AM, Fine MJ. Self-reported changes in drug and alcohol use after becoming homeless. Am J Public Health. 2004;94(5):830–836. doi: 10.2105/ajph.94.5.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? Am J Public Health. 2004;94(1):103–8. doi: 10.2105/ajph.94.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breakey WR, Fischer P, Kramer M, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262(6):1352–1357. [PubMed] [Google Scholar]
- 10.Burt MR, Aron LY, Douglas T, Valente J, Lee E, Iwen B. Homelessness: Programs and the People They Serve. Technical Report of Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, D.C.: 1999. Available at: http://www.urban.org/publications/310291.html. [Google Scholar]
- 11.Baggett TP, Hwang SW, O’Connell JJ, et al. Mortality among homeless adults in Boston: Shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173(3):189–95. doi: 10.1001/jamainternmed.2013.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baggett TP, Chang Y, Singer DE, et al. Tobacco-, alcohol-, and drug-attributable deaths and their contribution to mortality disparities in a cohort of homeless adults in Boston. Am J Public Health. 2015;105(6):1189–97. doi: 10.2105/AJPH.2014.302248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Health Care for the Homeless Council [Accessed November 7, 2015];The health care for the homeless program fact sheet. 2013 Available at: http://www.nhchc.org/wp-content/uploads/2011/09/hch-fact-sheet-2013.pdf.
- 14.U.S. Department of Veterans Affairs Homeless patient aligned care teams (H-PACT) 2015 Available at: http://www.endveteranhomelessness.org/programs/homeless-pact.
- 15.Health Resources and Services Administration Bureau of Primary Health Care Program requirements.
- 16.42 U.S. Code § 254b - Health centers. United States; 2011. Available at: http://uscode.house.gov/view.xhtml?edition = prelim&req = 42+usc+254b&f = treesort&fq = true&num = 20&hl = true. [Google Scholar]
- 17.Lebrun-Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: Findings from the 2009 patient survey. Health Serv Res. 2013;48(3):992–1017. doi: 10.1111/1475-6773.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bharel M, Lin W-C, Zhang J, et al. Health care utilization patterns of homeless individuals in Boston: Preparing for Medicaid expansion under the Affordable Care Act. Am J Public Health. 2013;103(Suppl):S311–7. doi: 10.2105/AJPH.2013.301421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Health Care for the Homeless Council [Accessed November 15, 2015];Substance use disorder. Available at: https://www.nhchc.org/resources/clinical/diseases-and-conditions/substance-use-disorder/
- 20.Kertesz SG, Khodneva Y, Richman J, et al. Trajectories of drug use and mortality outcomes among adults followed over 18 years. J Gen Intern Med. 2012;27(7):808–16. doi: 10.1007/s11606-011-1975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mertens JR, Weisner C, Ray GT, Fireman B, Walsh K. Hazardous drinkers and drug users in HMO primary care: Prevalence, medical conditions, and costs. Alcohol Clin Exp Res. 2005;29(6):989–998. doi: 10.1097/01.ALC.0000167958.68586.3D. [DOI] [PubMed] [Google Scholar]
- 22.Kertesz SG, Larson MJ, Horton NJ, Winter M, Saitz R, Samet JH. Homeless chronicity and health-related quality of life trajectories among adults with addictions. Med Care. 2005;43(6):574–585. doi: 10.1097/01.mlr.0000163652.91463.b4. [DOI] [PubMed] [Google Scholar]
- 23.Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. Am Psychol. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- 24.Friedmann PD, Saitz R, Samet JH. Management of adults recovering from alcohol or other drug problems: Relapse prevention in primary care. JAMA. 1998;279(15):1227–1231. doi: 10.1001/jama.279.15.1227. [DOI] [PubMed] [Google Scholar]
- 25.Irwin J, LaGory M, Ritchey F, Fitzpatrick K. Social assets and mental distress among the homeless: Exploring the roles of social support and other forms of social capital on depression. Soc Sci Med. 2008;67(12):1935–1943. doi: 10.1016/j.socscimed.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- 27.Amato L, Davoli M, Vecchi S, et al. Cochrane systematic reviews in the field of addiction: What’s there and what should be. Drug Alcohol Depend. 2011;113(2-3):96–103. doi: 10.1016/j.drugalcdep.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Weiner SJ, Kelly B, Ashley N, et al. Content coding for contextualization of care: Evaluating physician performance at patient-centered decision making. Med Decis Mak. 2014;34(1):97–106. doi: 10.1177/0272989×13493146. [DOI] [PubMed] [Google Scholar]
- 29.Kertesz SG, Holt CL, Steward JL, et al. Comparing homeless persons’ care experiences in tailored versus nontailored primary care programs. Am J Public Health. 2013;103(S2):S331–S339. doi: 10.2105/AJPH.2013.301481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kertesz SG, Pollio DE, Jones RN, et al. Development of the primary care quality-homeless (PCQ-H) instrument: A practical survey of homeless patients’ experiences in primary care. Med Care. 2014;52(8):734–742. doi: 10.1097/MLR.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization [Accessed November 20, 2015];The ASSIST project: Alcohol, smoking and substance involvement screening test. 2014 Available at: http://www.who.int/substance_abuse/activities/assist/en/
- 32.Humeniuk RE, Henry-Edwards S, Ali RL, Poznyak V, Monteiro M. The alcohol, smoking and substance involvement screening test (ASSIST): Manual for use in primary care. Geneva: 2010. [DOI] [Google Scholar]
- 33.Humeniuk RE, Ali R, Babor TF, et al. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- 34.Humeniuk RE, Ali R. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) and pilot brief intervention: A technical report of phase II findings of the WHO ASSIST project. Geneva, Switzerland: 2005. [Google Scholar]
- 35.Lin N, Dean A, Ensel W. Social support, life events, and depression. Academic Press; New York: 1986. [Google Scholar]
- 36.108th Congress . H.R. 2673: Consolidated appropriations act. 108th Congress; 2003. Available at: http://www.govtrack.us/congress/bills/108/hr2673. [Google Scholar]
- 37.111th Congress . Homeless emergency assistance and rapid transition to housing (HEARTH) Act of 2009. United States: 2009. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ22/html/PLAW-111publ22.htm. [Google Scholar]
- 38.Saitz R, Gaeta J, Cheng DM, Richardson JM, Larson MJ, Samet JH. Risk of mortality during four years after substance detoxification in urban adults. J Urban Heal. 2007;84:272–282. doi: 10.1007/s11524-006-9149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boothroyd RA, Chen HJ. The psychometric properties of the Colorado symptom index. Adm Policy Ment Heal Ment Heal Serv Res. 2008;35(5):370–378. doi: 10.1007/s10488-008-0179-6. [DOI] [PubMed] [Google Scholar]
- 40.Conrad KJ, Yagelka JR, Matters MD, Rich AR, Williams V, Buchanan M. Reliability and validity of a modified Colorado symptom index in a national homeless sample. Ment Health Serv Res. 2001;3(3):141–153. doi: 10.1023/a:1011571531303. [DOI] [PubMed] [Google Scholar]
- 41.Shern DL, Wilson NZ, Coen AS, et al. Client outcomes II: Longitudinal client data from the Colorado treatment outcome study. Milbank Q. 1994;72(1):123–148. Available at: http://www.ncbi.nlm.nih.gov/pubmed/8164605. [PubMed] [Google Scholar]
- 42.Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. 2nd ed Sage Publications, Inc.; Thousand Oaks, CA: 2011. [Google Scholar]
- 43.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 alcohol use disorder. JAMA Psychiatry. 2015;20852:1–10. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grant BF, Goldstein RB, Saha TD, et al. Epidemiology of DSM-5 drug use disorder: Results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiatry. 2015;20852:1–10. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64(5):566–76. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 46.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64(7):830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 47.Breslau J, Kendler KS, Su M, Gaxiloa-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35(3):317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lopez-Quintero C, Hasin DS, de los Cobos JP, et al. Probability and predictors of remission from lifetime nicotine, alcohol, cannabis, or cocaine dependence: Results from the national epidemiologic survey on alcohol and related conditions. Addiction. 2011;106(3):657–669. doi: 10.1111/j.1360-0443.2010.03194.x.Probability. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zapolski TCB, Pedersen SL, McCarthy DM, Smith GT. Less drinking, yet more problems: Understanding African American drinking and related problems. Psychol Bull. 2014;140(1):188–223. doi: 10.1037/a0032113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fazel PS, Geddes JR, Kushel M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–1540. doi: 10.1016/S0140-6736(14)61132-6.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: A 3-year follow-up. Alcohol Clin Exp Res. 2007;31(12):2036–2045. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- 52.Mertens JR, Kline-Simon AH, Delucchi KL, Moore C, Weisner CM. Ten-year stability of remission in private alcohol and drug outpatient treatment: Non-problem users versus abstainers. Drug Alcohol Depend. 2012;125(1-2):67–74. doi: 10.1016/j.drugalcdep.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ducharme LJ, Chandler RK, Harris AHS. Implementing effective substance abuse treatments in general medical settings: Mapping the research terrain. J Subst Abuse Treat. 2015 doi: 10.1016/j.jsat.2015.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Polen MR, Whitlock EP, Wisdom JP, Nygren P, Bougatsos C. Screening in primary care settings for illicit drug use: Staged systematic review for the U.S. preventive services task force. Evidence synthesis No. 58, Part 1. (Prepared by the Oregon evidence-based practice center under contract No. 290-02-0024) Rockville, MD: 2008. [PubMed] [Google Scholar]
- 55.Saitz R, Palfai TPA, Cheng DM, et al. Screening and brief intervention for drug use in primary care. JAMA. 2014;312(5):502. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings. JAMA. 2014;312(5):492. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Young MM, Stevens A, Porath-Waller A, et al. Effectiveness of brief interventions as part of the screening, brief intervention and referral to treatment (SBIRT) model for reducing the non-medical use of psychoactive substances: a systematic review protocol. Syst Rev. 2014;3(50):1–18. doi: 10.1186/2046-4053-1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Upshur C, Weinreb L, Bharel M, Reed G, Frisard C. A randomized control trial of a chronic care intervention for homeless women with alcohol use problems. J Subst Abuse Treat. 2014;51:19–29. doi: 10.1016/j.jsat.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gelberg L, Andersen RM, Afifi AA, et al. Project QUIT (Quit Using Drugs Intervention Trial): A randomized controlled trial of a primary care-based multi-component brief intervention to reduce risky drug use. Addiction. 2015;110(11):1777–1190. doi: 10.1111/add.12993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gordon AJ, Haibach J. Screening and Intervening on Alcohol and Other Drug Use in General Wellness Programs: Challenges and Opportunities. Subst Abus. 2015;36(3):255–256. doi: 10.1080/08897077.2015.1073975. [DOI] [PubMed] [Google Scholar]
- 61.Weiner SJ, Schartz A, Weaver F, et al. Contextual errors and failures in individualizing patient care. Ann Intern Med. 2010;153:69–76. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]
- 62.Weiner SJ. Contextualizing medical decisions to individualize care. J Gen Intern Med. 2004;19:281–285. doi: 10.1111/j.1525-1497.2004.30261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bohnert ASB. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 64.Saitz R. Commentary on Gelberg et al. 2015: Alcohol and other drug screening and brief intervention - evidence in crisis. Addiction. 2015;110(11):1791–1793. doi: 10.1111/add.13054. [DOI] [PubMed] [Google Scholar]
- 65.Saitz R. Screening and brief intervention for unhealthy drug use: little or no efficacy. Front psychiatry. 2014 Sep;5:1–5. doi: 10.3389/fpsyt.2014.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Friedmann PD, Mello D, Lonergan S, Bourgault C, O’Toole TP. Aversion to injection limits acceptability of extended-release naltrexone among homeless, alcohol-dependent patients. Subst Abus. 2013;34(2):94–96. doi: 10.1080/08897077.2012.763083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Collins SE, Duncan MH, Smart BF, et al. Extended-release naltrexone and harm reduction counseling for chronically homeless people with alcohol dependence. Subst Abus. 2014 Aug;7077:37–41. doi: 10.1080/08897077.2014.904838. [DOI] [PubMed] [Google Scholar]
- 68.Tsemberis S, Kent D, Respress C. Housing stability and recovery among chronically homeless persons with co-occuring disorders in Washington, DC. Am J Public Health. 2012;102(1):13–16. doi: 10.2105/AJPH.2011.300320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Harrell AV, Kapsak KA, Cisin IH, Wirtz PW. The validity of self-reported drug use data: The accuracy of responses on confidential self-administered answer sheets. Rockville, MD: 1986. [PubMed] [Google Scholar]
- 70.Nyamathi A, Leake BD, Longshore D, Gelberg L. Reliability of homeless women’s reports: Concordance between hair assay and self report of cocaine use. Nurs Res. 2001;50(3):165–171. doi: 10.1097/00006199-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 71.United States Department of Housing and Urban Development . The 2013 annual homeless assessment report (AHAR) to Congress: Point-in-time estimates of homelessness. Washington, D.C.: 2013. [Google Scholar]
- 72.Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27–32. doi: 10.7205/milmed-d-11-00128. [DOI] [PubMed] [Google Scholar]