Abstract
Brace is one of the most commonly used interventions to manage osteoporotic vertebral fracture. However, its authentic effectiveness remains unclear. The aim of this study was to investigate the efficacy of brace in patients with osteoporotic vertebral fractures. We conducted a literature review and meta-analysis following the guideline and handbook of the Cochrane collaboration. Ten published articles were included in this study and data from 4 randomized controlled trials were analyzed. Low quality evidence proved using Spinomed brace could bring large and significant beneficial effect to patients with sub-acute osteoporotic vertebral fractures. Very low quality evidence proved no significant difference between Spinomed orthosis, rigid brace and soft brace when they were used in patients with acute fractures. Therefore, it might be applicable to recommend middle term use of Spinomed orthosis to patients with subacute fracture. In addition, this study emphasized the need for high quality randomized controlled trials.
Keywords: Spine, Osteoporosis, Fracture, Brace, Meta-Analysis
Graphical Abstract
INTRODUCTION
Osteoporotic vertebral fracture (OVF) is one of the most severe osteoporotic fractures, which causes severe pain, disability, dyspnea, deformity and raises the risk of subsequent fracture and death (1,2). Among the conservative treatments to OVF, multifarious orthoses are used and expected to immobilize the fracture site, diminish pain and improve quality of life. However, their authentic effectiveness to patients with OVF remains unclear (1). Several trials investigated the efficacy of orthoses, but quality of them varied a lot and their outcome parameters were not standardized. Conclusions from previously published systematic reviews had limited generalizability, due to their indirectness in participants or limited number of included studies (3,4). Additionally, strength of recommending orthoses to patients with OVF remained inconclusive in reviews or guidelines (5,6).
In order to explore the efficacy of orthoses, we conducted this study through a systematic literature search and meta-analysis. We focused on patients with osteoporotic vertebral fracture and analyzed the outcomes of pain, kyphosis angle and quality of life. Furthermore, we discussed the reasons why some orthoses were effective and some were not.
MATERIALS AND METHODS
Data source and searching strategy
We searched electronic databases, including Medline, EMBASE, Central Register of Controlled Trials (CENTRAL) and Web of science, from May, 2015 and updated weekly until March, 2016. A search strategy included keywords of "clinical trial", "osteoporotic fracture", "spine", "orthosis", and "brace" was used. Details of the search strategy were presented in Supplementary 1. Reference lists of other reviews were also checked for relevant articles.
Study selection
Initially, one author identified the potentially relevant articles by screening titles and abstracts, and then two authors evaluated their eligibility for being included in this study through full text assessment. The evaluation mainly focused on characteristics of the studies. English published articles that recruited participants who had at least one diagnosed OVF and implemented orthoses as interventions were included. Trials were excluded if they recruited subjects with traumatic vertebral fractures or pooled participants with and without fracture together but did not separately report their outcomes. Disagreements were solved by discussion between two authors.
Data extraction
We extracted information with standardized tables which described characteristics of participants, interventions and outcomes. Unclear information and data in studies was clarified by contacting their authors through e-mails. Outcomes of pain, kyphosis angle and quality of life (Oswestry disability index, Well-being and Functional independence measure-motor score) were statistically analyzed.
Methods used for extracting and handling data were slightly different according to studies. In studies reported outcomes at multiple time points, data from the last visit was extracted; in cross-over designed trials, data before the cross-over procedure was extracted. When synthesized the data from studies with 3 arms, the number of participants in control group was separated evenly, and each compared with one intervention group, with the value of mean and standard deviation (SD) unchanged.
Measurement of risk of bias
We assessed the quality of included randomized controlled trials (RCTs) with a method recommended by Cochrane back and neck group (CBN) (7). The method measured the risk of bias in 6 domains: selection, performance, detection, attribution, reporting and others.
Data synthesis and analysis
We pooled data using the Review Manager (Revman 5.3) and implemented the meta-analysis with the random effect model. Change value from baseline was used because most trials reported outcomes in that data type. If value of SD was not reported and needed to be estimated, the formula presented as follows was used,
with an assignment of 0.5 as correlation value. The standardized mean difference (SMD) was used to synthesize the outcomes because the measuring scales were different between studies. Some mean values were multiplied by -1 to ensure results from different scales could point in the same direction. Expression of the magnitude of the results followed the rules of thumb (< 0.2, small effect; 0.2 to 0.8, moderate effect; > 0.8, large effect) (8). Statistical heterogeneity between studies was measured with the chi-squared test. The heterogeneity was considered as significant when P value was not bigger than 0.10 and was recognized as considerable when I2 value was bigger than 75% (7). To explore the heterogeneity, subgroup analysis was conducted. To prove our results were not depended on arbitrary decisions on including studies or assigning values, we conducted several sensitivity analyses. The analyses included estimating SD with the different correlation value (0.4), excluding some "dubious" articles and estimating results with the fixed effect model.
Measurement of quality of evidence
To reflect our confidence in truthfulness of the results, we measured quality of evidence with the GRADE approach. The approach measures the limitations of results in 5 domains: study limitation (risk of bias), inconsistency, indirectness, imprecision and publication bias. Each item was downgraded 1 or 2 points if the result failed to meet the criteria (9). "Study limitation" was downgraded 1 point if 1 to 3 categories of risk of bias were rated as high or unclear. "Inconsistency" was downgraded 1 point if large statistical heterogeneity (P ≤ 0.10, I2 > 80%) existed, downgraded 2 points if both large statistical heterogeneity and obvious clinical heterogeneity existed. "Indirectness" was downgraded 1 to 2 points if we detected indirectness in domains of population, intervention, comparator, comparison and outcome. "Imprecision" was downgraded 1 point if the total sample size was smaller than 400 and was downgraded 2 points if there were few events and wide confidence intervals (CIs). "Publication bias" was downgraded by 1 point only when we strongly suspected the existence of publication bias.
RESULTS
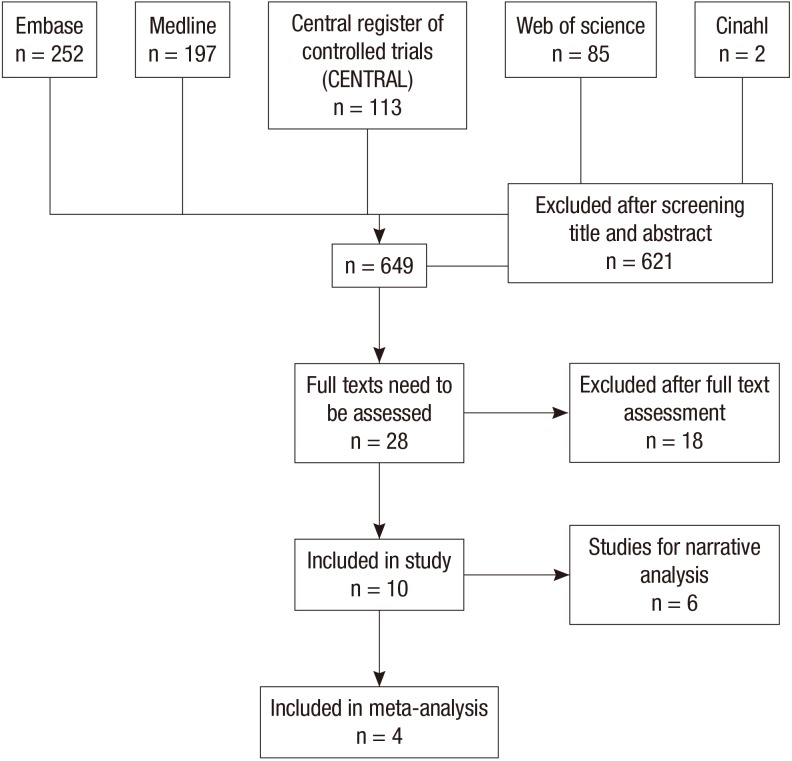
Initially we identified 649 relevant citations and then remained 28 articles for full-text assessment. Eventually, 10 articles were included in this study (10,11,12,13,14,15,16,17,18,19) and 4 RCTs, with 281 participants, were included in meta-analysis (10,11,12,14) (Fig. 1).
Fig. 1. Flow diagram of selection process.
Description of included studies
As summarized in Table 1 and 2, 6 RCTs (10,11,12,13,14,15), 1 non-randomized controlled trial (19) and 3 observational studies (16,17,18) were included. Characteristics of studies varied a lot but all had limited number of participants and only one trial had a sample size merely above 100 (12). Phase of fracture and recruiting sources of participants were different between studies. Participants had acute fractures in 3 trials (10,14,18) while those from another 3 trials had sub-acute fractures (11,12,13). Most of the studies recruited participants in hospital environment (10,13,14,15,17,18,19), while two trials recruited in community environment (11,12).
Table 1. Characteristics of studies included in MA.
| Study ID | Study design | Participants number | Phase of fracture | Participants source | Intervention | Follow up duration |
|---|---|---|---|---|---|---|
| Kim et al. (14), 2014 | RCT | 60 | Acute | Hospital | Soft brace: 8 wk | 12 wk |
| Rigid brace: 8 wk | ||||||
| Control group: no brace | ||||||
| Li et al. (10), 2014 | RCT | 51 | Acute | Hospital | Group 1: TLSO, the1st week; SpinoMed, the 2nd and the 3rd week | 3 wk |
| Group 2: TLSO, the 1st week; Soft brace, the 2nd and the 3rd week | ||||||
| Pfeifer et al. (12), 2011* | RCT | 108 | Subacute | Community | Group 1: Spinomed orthosis, 12 mon | 12 mon |
| Group 2: Spinomed active orthosis, 12 mon | ||||||
| Group 3: no brace | ||||||
| Pfeifer et al. (11), 2004* | RCT | 62 | Subacute | Community | Group 1: Spinomed, 12 mon | 12 mon |
| Group 2: no brace |
MA, meta-analysis; RCT, randomized controlled trial; TLSO, thoracolumbar sacral orthosis.
*This trial was designed as a cross-over study. We extracted the data before cross-over procedure, on the 6th month.
Table 2. Characteristics of studies included in study but excluded from MA.
| Study ID | Study type | Participants number | Phase of fracture | Participants source | Interventions | Follow up duration | Conclusion |
|---|---|---|---|---|---|---|---|
| Dionyssiots et al. (13), 2015* | RCT | 50 | Subacute | Hospital | Group 1: Semi-rigid orthosis | 6 mon | Wearing Spinomed orthosis decreased back pain significantly and increased trunk muscle strength significantly. |
| Group 2: Elastic orthosis | |||||||
| Group 3: Control group | |||||||
| Sinaki and Lynn (15), 2002 | Pilot RCT | 7 | NA | Hospital | Group 1: PTS + Exercise | 1 mon | Subjects who had abnormal balance had the most significant improvement in balance. |
| Group 2: Exercise | |||||||
| Valentin et al. (16), 2014 | Case series study | 13 | NA | NA | Spinomed III | 3 mon | The improvement in the back extensor strength was significant; but not in pain or physical function. |
| Talic et al. (19), 2012 | N-RCT | 59 | NA | Hospital | Group 1: Three-point orthosis | 1-4 mon | Plaster corset offered stability; but patients with orthoses were more mobile. |
| Group 2: Plaster corset | Duration of immobilization was significantly longer in orthosis group. | ||||||
| Murata et al. (18), 2012 | Retrospective study | 55 | Acute | Hospital | Plastic TLSO orthosis | 6 mon | TLSO promoted the healing of OVF. |
| Mean kyphosis angle deteriorated from 11.4° to 17.2°. | |||||||
| Liaw et al. (17), 2009 | Case series study | 47 | NA | Hospital | Knight-Taylor orthosis | Immediately | Knight-Taylor brace improved in static and dynamic motor balance but decreased the directional control. |
MA, meta-analysis; RCT, randomized controlled trial; PTS, posture training support; NA, not available; TLSO, thoracolumbar sacral orthosis; N-RCT, non-randomized controlled trial.
*The data reported in this article was insufficient to be included in meta-analysis.
Most of the trials implemented semi-rigid brace (Spinomed orthosis) and rigid brace for middle to long term. Efficacy of the Spinomed orthosis was investigated in 4 RCTs (10,11,12,13) and 1 case series study (16). Three of the 4 RCTs were included in the meta-analysis (10,11,12) (Table 1), while Dionyssiotis et al.'s study (13) was excluded due to their insufficiently reported data. Efficacy of rigid brace was investigated in 2 observational studies (17,18) and 2 controlled trials (14,19), one of which evaluated the efficacy of thoracolumbar sacral orthosis (TLSO) was included in meta-analysis (14) (Table 1). Implementation and follow-up periods ranged from 1 to 6 months in most studies, except one case series study that immediately measured effect of the Knight-Taylor brace after it was implemented (17).
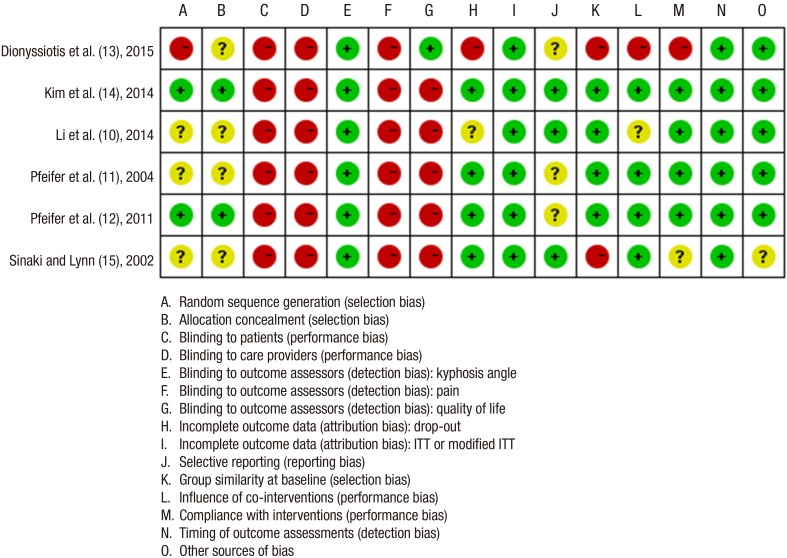
Risk of bias of included RCTs
All trials had high risk of bias in at least 1 category (Fig. 2). Most trials had unclear risk of selection bias, due to their briefly reported procedures of random sequence generation and allocation concealment. All trials had high risk of performance bias because it was relatively difficult to maintain double blind while implemented braces. Risk of detection bias was evaluated separately in different outcomes, and only the measurement of the kyphosis angle was rated as low risk. Risk of attribution bias was rated as low in 4 trials (11,12,14,15). Risk of reporting bias was rated as unclear in half of the trials (11,12,13). Risk of other bias was evaluated as low in 5 trials that clarified no conflict of interest in conducting and publishing the researches (10,11,12,13,14). We presented the rationales for the judgements of risk of bias in Supplementary 2.
Fig. 2. Risk of bias table of included randomized controlled trials. Green represents "low risk of bias"; yellow, "unclear risk of bias"; red, "high risk of bias".
Effects of intervention: results from meta-analysis
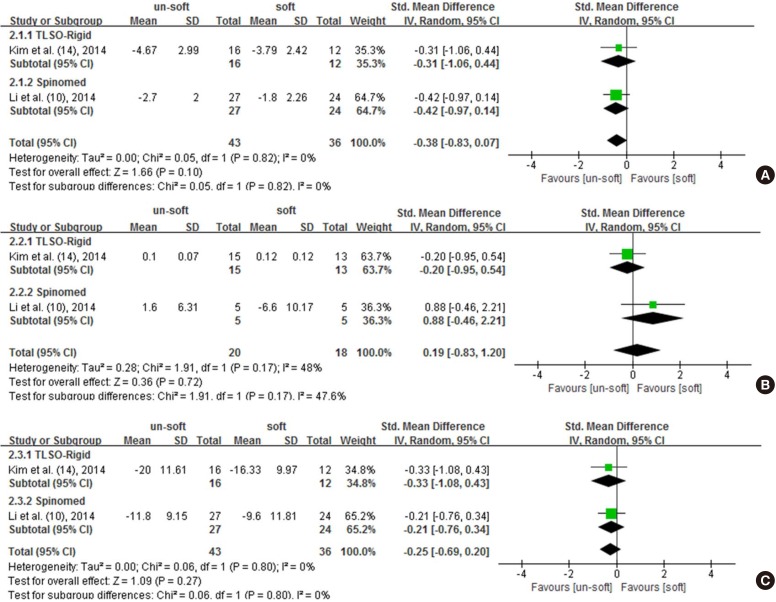
Three studies investigated the efficacy of braces by comparing to no brace groups, including 230 participants (11,12,14). We analyzed the outcomes of pain, kyphosis angle and quality of life with subgroup analysis.
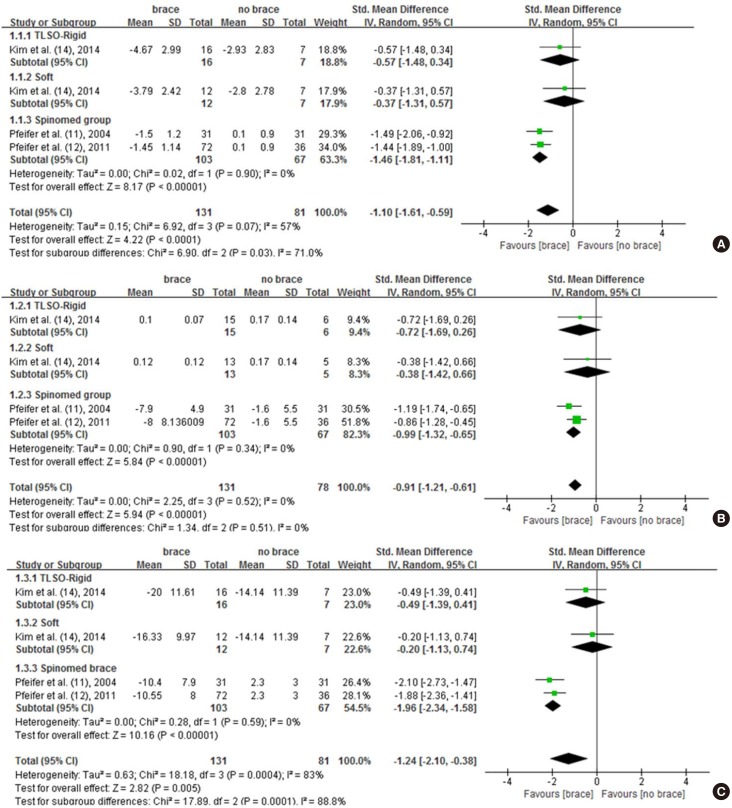
In the outcome of pain, the pooled data showed large and significant beneficial effect brought by using brace (SMD, -1.10; 95% CIs, -1.61 to -0.59; P < 0.001, Fig. 3A). The heterogeneity was significant but its magnitude was acceptable (P = 0.070, I2 = 57%, Fig. 3A). However, the overall quality of the result was rated as low, due to the serious study limitation and serious imprecision (Table 3). From the subgroup analysis, we noticed only the efficacy of Spinomed was significant (P < 0.001, Fig. 3A); and so was the difference between subgroups (P = 0.030, Fig. 3A).
Fig. 3. Forest plot. Comparison between brace group and no brace group. Use of brace showed significant efficacy on pain (A), kyphosis angle correction (B), and quality of life (C).
Table 3. Summary of findings (SOF) table of brace vs. no brace.
| Outcomes | Anticipated absolute effects (95% CI) | No. of participants (studies) | Overall quality of evidence (GRADE) |
|---|---|---|---|
| Pain reduction-pooled data | SMD 1.1 fewer (1.61 fewer to 0.59 fewer) | 212 (3 studies) | ⨁⨁◯◯ |
| LOW*,† | |||
| Pain reduction-TLSO | SMD 0.57 fewer (1.48 fewer to 0.34 more) | 23 (1 study) | ⨁◯◯◯ |
| VERY LOW‡,§ | |||
| Pain reduction-soft brace | SMD 0.37 fewer (1.31 fewer to 0.57 more) | 19 (1 study) | ⨁◯◯◯ |
| VERY LOW‡,§ | |||
| Pain reduction-Spinomed group | SMD 1.46 fewer (1.81 fewer to 1.11 fewer) | 170 (2 studies) | ⨁⨁◯◯ |
| LOW∥,† | |||
| Kyphosis angle-pooled data | SMD 0.91 fewer (1.21 fewer to 0.61 fewer) | 209 (3 studies) | ⨁⨁◯◯ |
| LOW¶,† | |||
| Kyphosis angle-TLSO | SMD 0.72 fewer (1.69 fewer to 0.26 more) | 21 (1 study) | ⨁◯◯◯ |
| VERY LOW**,§ | |||
| Kyphosis angle-soft brace | SMD 0.38 fewer (1.42 fewer to 0.66 more) | 18 (1 study) | ⨁◯◯◯ |
| VERY LOW**,§ | |||
| Kyphosis angle-Spinomed group | SMD 0.99 fewer (1.32 fewer to 0.65 fewer) | 170 (2 studies) | ⨁⨁◯◯ |
| LOW†,†† | |||
| Quality of life-pooled data | SMD 1.24 fewer (2.1 fewer to 0.38 fewer) | 212 (3 studies) | ⨁◯◯◯ |
| VERY LOW*,†,†† | |||
| Quality of life-TLSO | SMD 0.49 fewer (1.39 fewer to 0.41 more) | 23 (1 study) | ⨁◯◯◯ |
| VERY LOW‡,§ | |||
| Quality of life-soft brace | SMD 0.2 fewer (1.13 fewer to 0.07 more) | 19 (1 study) | ⨁◯◯◯ |
| VERY LOW‡,§ | |||
| Quality of life-Spinomed brace | SMD 1.96 fewer (2.34 fewer to 1.58 fewer) | 170 (2 studies) | ⨁⨁◯◯ |
| LOW∥,† |
CIs, confidence intervals; SMD, standardized mean difference; RCT, randomized controlled trial; TLSO, thoracolumbar sacral orthosis.
*Serious study limitation: three trials were included, with high risk of performance bias and detection bias; †Serious imprecision: sample size was smaller than 400; ‡Serious study limitation: one trial was included, with high risk of detection bias and performance bias; §Very serious imprecision: sample size was too small and CIs was wide; ∥Serious study limitation: two trials were included, with high risk of performance bias and detection bias; ¶Serious study limitation: three trials were included, with high risk of performance bias; **Serious study limitation: one trial was included, with high risk of performance bias; ††Serious study limitation: two trials were included, with high risk of performance bias; ‡‡Very serious inconsistency: the statistical heterogeneity was large (I2 > 80%) and the clinical heterogeneity existed.
In the outcome of kyphosis angle, pooled data was similar to that of pain: the efficacy brought by brace was large and significant (SMD, -0.91; 95% CIs, -1.21 to -0.61; P < 0.001, Fig. 3B). Still, the overall quality of this evidence was rated as low for the serious study limitation and serious imprecision (Table 3). The difference between subgroups was insignificant (P = 0.510, Fig. 3B), though only the Spinomed orthosis showed significant efficacy (Fig. 3B). The consistency between subgroups might be a result of the similarity in their effect sizes and the relatively well overlapped CIs (Fig. 3B).
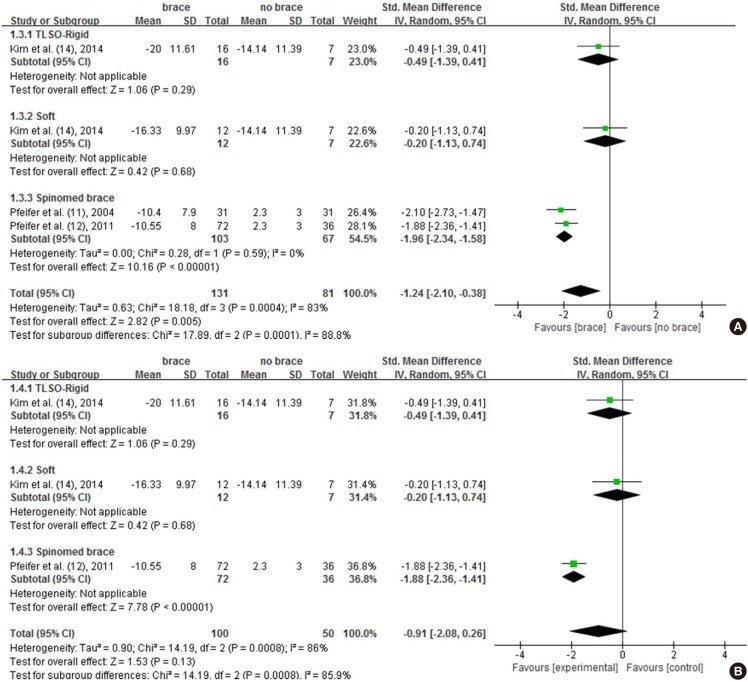
Very low quality evidence indicated large and significant beneficial effect on quality of life brought by bracing (SMD, -1.24; 95% CIs, -2.10 to -0.38; P = 0.005, Fig. 3C). The heterogeneity and the difference between subgroups were significant (P < 0.001, Fig. 3C). The large magnitude of I2 and the existence of clinical heterogeneity suggested downgrading 2 scores for the inconsistency (Fig. 3). Thus, quality of this evidence was rated as very low, due to the serious study limitation, serious imprecision and the very serious inconsistency (Table 3). The untrustworthy of this outcome was also reflected by the result of sensitivity analysis, in which the pooled outcome changed to insignificant after excluding one of the two trials that had unclear risk of reporting bias (11) (Fig. 4).
Fig. 4. Result of the sensitivity analysis of excluding one of the two trials with unclear risk of reporting bias. The outcome of quality of life became insignificant after excluding data of Pfeifer et al., 2004 (A→B).
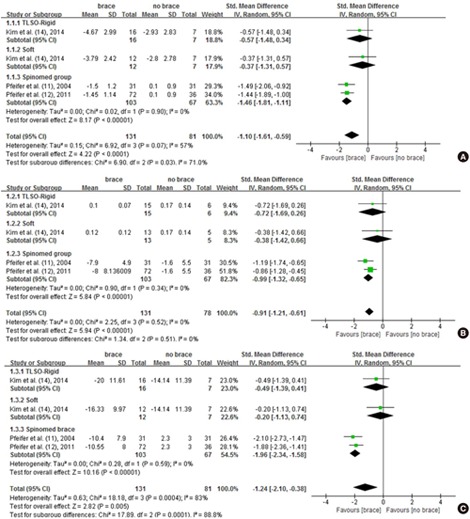
Analysis that compared soft brace with un-soft brace included two RCTs whose participants had acute vertebral fractures (10,14). The pooled data showed un-soft brace had no significant difference compared with soft brace (Fig. 5). The result was different from the one previously observed, in which Spinomed brace showed significantly better efficacy compared to soft brace (Fig. 3). The quality of evidence of pooled data was rated as very low in all outcomes, due to the serious study limitation and very serious imprecision (Table 4).
Fig. 5. Forest plot. Comparison between un-soft brace group and soft brace group. The results showed no significant difference between braces in pain (A), kyphosis angle (B) and quality of life (C).
Table 4. Summary of findings (SOF) table of un-soft brace vs. soft brace.
| Outcomes | Anticipated absolute effects (95% CIs) | No. of participants (studies) | Overall quality of evidence (GRADE) |
|---|---|---|---|
| Pain reduction-pooled data | SMD 0.38 fewer (0.83 fewer to 0.07 more) | 79 (2 studies) | ⊕◯◯◯ |
| VERY LOW*,†,‡ | |||
| Pain reduction-TLSO | SMD 0.31 fewer (1.06 fewer to 0.44 more) | 28 (1 study) | ⊕◯◯◯ |
| VERY LOW§,∥ | |||
| Pain reduction-Spinomed orthosis | SMD 0.42 fewer (0.97 fewer to 0.14 more) | 51 (1 study) | ⊕⊕◯◯ |
| LOW¶,‡ | |||
| Kyphosis angle-pooled data | SMD 0.19 fewer (0.83 fewer to 1.2 more) | 38 (2 studies) | ⊕◯◯◯ |
| VERY LOW**,†,∥ | |||
| Kyphosis angle-TLSO | SMD 0.2 fewer (0.95 fewer to 0.54 more) | 28 (1 study) | ⊕◯◯◯ |
| VERY LOW††,∥ | |||
| Kyphosis angle-Spinomed orthosis | SMD 0.88 more (0.46 fewer to 2.21 more) | 10 (1 study) | ⊕◯◯◯ |
| VERY LOW‡‡,∥ | |||
| Quality of life-pooled data | SMD 0.25 fewer (0.69 fewer to 0.02 more) | 79 (2 studies) | ⊕◯◯◯ |
| VERY LOW*,†,‡ | |||
| Quality of life-TLSO | SMD 0.33 fewer (1.08 fewer to 0.43 more) | 28 (1 study) | ⊕◯◯◯ |
| VERY LOW§,∥ | |||
| Quality of life-Spinomed brace | SMD 0.21 fewer (0.76 fewer to 0.34 more) | 51 (1 study) | ⊕⊕◯◯ |
| LOW¶,‡ |
CIs, confidence intervals; SMD, standardized mean difference; RCT, randomized controlled trial; TLSO, thoracolumbar sacral orthosis.
*Serious study limitation: two trials were included, with high risk of performance bias and detection bias; †Serious inconsistency: measurement time was different between studies; ‡Serious imprecision: sample size was smaller than 400; §Serious study limitation: one study was included, with high risk of performance bias and detection bias; ∥Very serious imprecision: sample size was too small and CIs was wide; ¶Serious study limitation: one study was included, with high risk of performance and detection bias; **Serious study limitation: two trials were included, with high risk of performing bias; ††Serious study limitation: one study was included, with high risk of performance bias; ‡‡Serious study limitation: one study was included, with high risk of performance and unclear risk of selection bias.
Results from narrative analysis
The narrative results were summarized in Table 2. Though most of the results showed benefits from using brace, the strength of them was relatively weak. Two RCTs had limitations in their methodologies: one had high risk of bias (13) and the other one had a small sample size (15). Also, we had limited confidence in conclusions of observational studies, because they might lack the power of proving causal relationship between the utilization of orthoses and the benefit.
Publication bias
The publication bias cannot be detected through the funnel plot because the number of trials included in our meta-analysis was less than 10.
DISCUSSION
We included 10 trials in this study and 4 RCTs in meta-analysis. All trials had high risk of performance bias and most of them had unclear risk of selection bias. Low to very low quality evidence proved that using brace was effective in reducing pain, preventing kyphosis angle deterioration and improving quality of life. However, as observed in the subgroup analyses, only middle term use of Spinomed orthosis could bring significant improvement to the patients who had subacute fractures. Very low quality evidence indicated there was no significant difference between the efficacy of TLSO, Spinomed and soft brace, when they were implemented to the patients with acute fractures.
The pooled results were difficult to interpret and were relatively unreliable due to the limited information. Therefore, rather than solving the prescribe questions, current evidence might be more proper to find possible explanations or patterns of the efficacy. The result showed Spinomed orthosis could bring large and significant beneficial effects to patients with sub-acute fracture, but it was relatively unreliable because of the interference from chance and the limited detective ability in our study. Nevertheless, it also might be a result of the special mechanism of this brace. Unlike most of the braces that offer immobilization to the fracture site, the Spinomed orthosis worked with a concept of improving the strength of users' trunk muscle. The stronger muscle of the users might subsequently reduce their pain and kyphosis angle deterioration, and improve their quality of life (12).
TLSO is one of the most widely used braces and should have shown beneficial effects in trials, but there was little evidence proving it in our study. The main reason for this contradiction should be the limited detective ability of our study. Other reasons might include the inadequate immobilization and the poor compliance of the brace (13,18). The inadequate immobilization might cause by the skin and soft tissues lie between orthosis and skeletal (6); while the poor compliance might cause by inappropriate implementation of the brace or complications like skin ulceration (6).
We noticed improvement in a single outcome cannot guarantee the improvements in others. Some equipment could reduce the kyphosis angle by exerting backward force to shoulders and forward force in thoracic region. But their efficacy in deformity was not always associated with improvement in mobility or quality of life (16,20). Also, the significant improvement in back muscle strength does not always accompany with relief of pain or improvement in physical function (16).
Two reviews investigated the subject recently, which had minor differences with ours. Newman et al. included osteoporosis and osteopenia participants and stated a descriptive review (3). Compared with theirs, our study focused on patients with OVF and conducted statistical analysis, which should bring more direct conclusions. Rzewuska et al. (4) investigated the efficacy of conservative treatments to OVF patients and included 3 RCTs about orthoses. Compared with them, we included 1 more trial that investigated the efficacy of rigid and soft braces. Also, we had different conclusions in the outcome of functional independence, while ours was more consistent with that of original article (10). Additionally, we analyzed the outcome of kyphosis angle, which was another critical parameter related to OVF patients. Excluding those differences, our results all revealed the need for high quality clinical trials.
There are several limitations in this study. The existence of publication bias might be covered by the absence of ongoing studies, grey literatures and trials from regional databases. The estimation of the treatment efficacy might be influenced by the language restriction in our inclusion criteria. The generalizability of results might be diminished by our relatively stringent criteria for evaluating the quality of evidence. Besides them, the biggest limitations were the limited number of included trials and the inconsistency between studies. All the limitations raised the difficulty in interpreting the results to some extent and fairly lowered the quality of evidence.
To obtain more dependable evidence, more RCTs with low risk of bias and big sample size are needed. Authors could lower the risk of selection bias through adequate description of the random sequence generation and allocation concealment. A cross-over study might be a proper design to minimize the risk of performance bias, since it might be inevitable for a trial about orthoses (12).
In conclusion, it might be appropriate to recommend middle term use of Spinomed orthoses to patients with subacute fractures. The evidence that could prove the efficacy of other brace was insufficient.
Footnotes
Funding: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2013R1A1A2061858).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study conception and design: Lee JH. Data acquisition: Jin YZ. Data analysis, interpretation: Jin YZ, Lee JH. Writing manuscript: Jin YZ, Lee JH. Revision: all authors. Approval of final manuscript: all authors.
Supplementary Materials
Search strategy for MEDLINE (via PubMed)
Rationales for the judgement of the risk of bias
References
- 1.Gerdhem P. Osteoporosis and fragility fractures: vertebral fractures. Best Pract Res Clin Rheumatol. 2013;27:743–755. doi: 10.1016/j.berh.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42. doi: 10.1007/s00198-003-1490-4. [DOI] [PubMed] [Google Scholar]
- 3.Newman M, Minns Lowe C, Barker K. Spinal orthoses for vertebral osteoporosis and osteoporotic vertebral fracture: a systematic review. Arch Phys Med Rehabil. 2016;97:1013–1025. doi: 10.1016/j.apmr.2015.10.108. [DOI] [PubMed] [Google Scholar]
- 4.Rzewuska M, Ferreira M, McLachlan AJ, Machado GC, Maher CG. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J. 2015;24:702–714. doi: 10.1007/s00586-015-3821-5. [DOI] [PubMed] [Google Scholar]
- 5.Esses SI, McGuire R, Jenkins J, Finkelstein J, Woodard E, Watters WC, 3rd, Goldberg MJ, Keith M, Turkelson CM, Wies JL, et al. The treatment of symptomatic osteoporotic spinal compression fractures. J Am Acad Orthop Surg. 2011;19:176–182. doi: 10.5435/00124635-201103000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Agabegi SS, Asghar FA, Herkowitz HN. Spinal orthoses. J Am Acad Orthop Surg. 2010;18:657–667. doi: 10.5435/00124635-201011000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, van Tulder MW, Editorial Board of the Cochrane Back, Neck Group 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine. 2015;40:1660–1673. doi: 10.1097/BRS.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 8.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions: version 5.1.0 [Internet] [updated March 2011]. [accessed on 2 March 2015]. Available at http://handbook.cochrane.org/
- 9.Chaparro LE, Furlan AD, Deshpande A, Mailis-Gagnon A, Atlas S, Turk DC. Opioids compared with placebo or other treatments for chronic low back pain: an update of the Cochrane Review. Spine. 2014;39:556–563. doi: 10.1097/BRS.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 10.Li M, Law SW, Cheng J, Kee HM, Wong MS. A comparison study on the efficacy of SpinoMed® and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int. 2015;39:270–276. doi: 10.1177/0309364614528204. [DOI] [PubMed] [Google Scholar]
- 11.Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83:177–186. doi: 10.1097/01.phm.0000113403.16617.93. [DOI] [PubMed] [Google Scholar]
- 12.Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011;90:805–815. doi: 10.1097/PHM.0b013e31821f6df3. [DOI] [PubMed] [Google Scholar]
- 13.Dionyssiotis Y, Trovas G, Thoma S, Lyritis G, Papaioannou N. Prospective study of spinal orthoses in women. Prosthet Orthot Int. 2015;39:487–495. doi: 10.1177/0309364614545416. [DOI] [PubMed] [Google Scholar]
- 14.Kim HJ, Yi JM, Cho HG, Chang BS, Lee CK, Kim JH, Yeom JS. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. J Bone Joint Surg Am. 2014;96:1959–1966. doi: 10.2106/JBJS.N.00187. [DOI] [PubMed] [Google Scholar]
- 15.Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study. Am J Phys Med Rehabil. 2002;81:241–246. doi: 10.1097/00002060-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Valentin GH, Pedersen LN, Maribo T. Wearing an active spinal orthosis improves back extensor strength in women with osteoporotic vertebral fractures. Prosthet Orthot Int. 2014;38:232–238. doi: 10.1177/0309364613497393. [DOI] [PubMed] [Google Scholar]
- 17.Liaw MY, Chen CL, Chen JF, Tang FT, Wong AM, Ho HH. Effects of Knight-Taylor brace on balance performance in osteoporotic patients with vertebral compression fracture. J Back Musculoskeletal Rehabil. 2009;22:75–81. doi: 10.3233/BMR-2009-0218. [DOI] [PubMed] [Google Scholar]
- 18.Murata K, Watanabe G, Kawaguchi S, Kanaya K, Horigome K, Yajima H, Morita T, Yamashita T. Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine. 2012;17:469–475. doi: 10.3171/2012.7.SPINE122. [DOI] [PubMed] [Google Scholar]
- 19.Talic A, Kapetanovic J, Dizdar A. Effects of conservative treatment for osteoporotic thoracolumbal spine fractures. Mater Sociomed. 2012;24:16–20. doi: 10.5455/msm.2012.24.16-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greig AM, Bennell KL, Briggs AM, Hodges PW. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man Ther. 2008;13:249–257. doi: 10.1016/j.math.2007.01.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy for MEDLINE (via PubMed)
Rationales for the judgement of the risk of bias