Abstract
Subchondral insufficiency fracture (SIF) of the femoral head occurs in the elderly and recipients of organ transplantation. Osteoporosis and deficient lateral coverage of the acetabulum are known risk factors for SIF. There has been no study about relation between spinopelvic alignment and anterior acetabular coverage with SIF. We therefore asked whether a decrease of lumbar lordosis and a deficiency in the anterior acetabular coverage are risk factors. We investigated 37 patients with SIF. There were 33 women and 4 men, and their mean age was 71.5 years (59-85 years). These 37 patients were matched with 37 controls for gender, age, height, weight, body mass index and bone mineral density. We compared the lumbar lordosis, pelvic incidence, pelvic tilt, sacral slope, acetabular index, acetabular roof angle, acetabular head index, anterior center-edge angle and lateral center-edge angle. Lumbar lordosis, pelvic tilt, sacral slope, lateral center edge angle, anterior center edge angle, acetabular index and acetabular head index were significantly different between SIF group and control group. Lumbar lordosis (OR = 1.11), lateral center edge angle (OR = 1.30) and anterior center edge angle (OR = 1.27) had significant associations in multivariate analysis. Decreased lumbar lordosis and deficient anterior coverage of the acetabulum are risk factors for SIF as well as decreased lateral coverage of the acetabulum.
Keywords: Subchondral Insufficiency Fracture, Lumbar Lordosis, Deficient Acetabular Coverage
Graphical Abstract
INTRODUCTION
Subchondral insufficiency fracture (SIF) of the femoral head occurs mainly in the elderly women or renal transplantation recipients (1,2). Although the pathomechanism of SIF is not clearly revealed, it seems to be a multifactorial disease. An excessive contact pressure at the femoral head is a risk factor as well as osteoporosis (3), Lumbar kyphosis leads to a posterior tilt of the pelvis to maintain the balance in a standing position (4). The posterior pelvic tilt causes a decrease in the anterior coverage of the acetabulum, which also induces an excessive pressure on the femoral head (5). Decrease of lateral center edge angle is a risk factor for osteoarthritis in hip dysplasia (6). Deficient anterior coverage of the acetabulum as well as deficient lateral coverage induces a decrease in the acetabular coverage.
Anterior and lateral deficiencies of the acetabular coverage should be discriminated in the pathogenesis of SIF. Most of the lateral deficiency is caused by hip dysplasia, which is a developmental abnormality. However, the anterior deficiency might be induced by a posterior pelvic tilt due to loss of lumbar lordosis, which is an aging phenomenon. To our knowledge, there has been no study, which related spinopelvic tilt and anterior acetabular coverage with SIF. We tested a hypothesis that loss of lumbar lordosis and decrease of anterior acetabular coverage are risk factors for SIF in the elderly.
MATERIALS AND METHODS
Recruitment of patients
From March 2005 to May 2014, 37 patients were diagnosed as having a SIF of the femoral head at two institutions. The femoral head SIF usually occurs in elderly patients or organ transplantation recipients without any obvious trauma. However, a subchondral fracture is also seen in femoral head osteonecrosis, bone marrow edema syndrome and fatigue fracture of the femoral head, which occurs in young military trainees. Magnetic resonance imaging (MRI) is the most sensitive technique for the diagnosis of SIF (2,7,8). Thus, the diagnosis of SIF was made using MRI in our patients. However, sometimes MRI cannot clearly discriminate SIF from osteonecrosis, bone marrow edema syndrome and subchondral fatigue fracture. Therefore, we considered patient's age, history of trauma and history of organ transplantation as well as radiologic features including MRI findings in making a diagnosis of SIF. We also considered the presence of risk factors for osteonecrosis, involvement of the opposite femoral head and histological findings in operated cases. In patients who underwent hip arthroplasty, histological findings of the resected femoral head were reviewed for the diagnosis of SIF.
Hips of patients, who were younger than 50 years, were excluded. Hips of patients, who had findings of osteonecrosis on radiographs and/or MRI in the contralateral hip and/or other joints, were excluded. Hips of patients, who had history of organ transplantation, alcohol abuse (9,10) and steroid use (11) were excluded.
On radiographs SIF appears as a focal depression at the superolateral potion of the femoral head. The fracture appears as a subchondral band lesion on MRI. The lesion has a low signal intensity on T1-weighted image and high signal intensity on T2-weighted image. In early stage, the band lesion is surrounded by bone marrow edema. In late reparative stage, fibrous tissue and fracture callus are seen around the fracture site.
All images were evaluated and diagnosis was made by three orthopaedic surgeons, who specialized joint arthroplasties. Among the three, one was a board-certified radiologist, who had specialized skeletal radiology, as well as an orthopaedic surgeon. Each decision was made on the basis of a consensus among the three surgeons.
Histological diagnosis of SIF was made according to the criteria by Yamamoto et al. (12). The microscopic criteria were presence of irregularly arranged fracture callus, reactive cartilage, and granulation tissue around the fracture site.
There were 33 women and 4 men. The mean patient age at the time of diagnosis was 71.5 years (range, 59-85 years). Eight patients, who had focal slight collapse (< 3 mm), were treated without surgical intervention: use of analgesics and teriparatide for 2 to 3 months with protected weight bearing (Fig. 1). The remaining 29 patients, who already had femoral head collapse and intractable pain at the time of presentation, were treated with total hip replacement (THR) (Fig. 2).
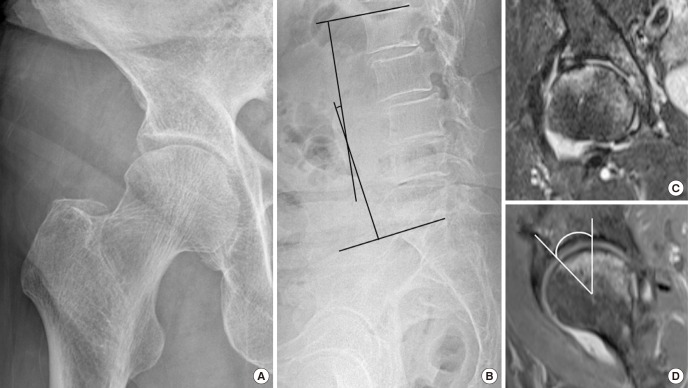
Fig. 1.
A 59-year-old woman had a pain on the right hip. (A) Radiograph shows a focal depression in the subchondral portion of the right femoral head. (B) Lateral radiograph of the lumbar spine shows a decrease of lumbar lordosis (7.8°). (C) T2-weighted coronal MRI shows subchondral collapse, which appears as a low signal band lesion, and surrounding edema, which appears as high signal intensity. (D) T2-weighted mid-sagittal MRI shows a decrease of anterior center-edge angle (31.4°).
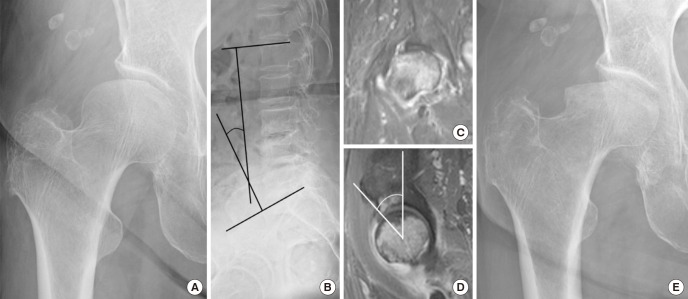
Fig. 2.
A 77-year-old woman with a subchondral insufficiency fracture of the right femoral head. (A) Radiograph after sudden onset of right hip pain shows subchondral collapse in the superolateral portion of the femoral head. (B) Lateral radiograph of the lumbar spine shows decreased lumbar lordosis (24.7°). (C) On the mid-coronal T2-weighted MRI, a diffuse bone marrow edema pattern with linear low signal intensity line at epiphysis of femoral head is seen. (D) On the mid-sagittal T2-weighted MRI, anterior center-edge angle was decreased to 29.2°. (E) Radiograph at 2 months follow-up shows rapidly progressive collapse of the femoral head.
The 37 patients were matched with 37 controls for age (1 year range), gender, height (5 cm range), weight (5 kg range), body mass index (1 kg/m2 range) and bone mineral density (BMD) of the proximal femur (0.1 g/cm2 range) (Table 1). The controls were selected from patients who had been studied with MRI of the hip due to hip pain or other diseases than SIF. In the selection of controls, we did not exclude non-involved hips of patients who had post-traumatic osteonecrosis in one hip because there has been no reported association between abnormal acetabular coverage and femoral head osteonecrosis. However, we excluded hip dysplasia, pincer type femoroacetabular impingement, osteoarthritis, ankylosing spondylitis and rheumatoid arthritis because patients with these diseases have deficient or excessive acetabular coverage. We also excluded patients who had leg length discrepancy 1 cm or more and patients who could not take radiographs in standing position. The non-painful opposite hip of the control patients were evaluated for the comparison with SIF hips. The diagnoses of control patients were previous infection in 8 hips, previous trauma in 7, and adhesive capsulitis in 6, trochanteric bursitis in 3 and post-traumatic osteonecrosis in 3. In the remaining 10 hips, no abnormal findings were noted on MRI.
Table 1. Demographic data of SIF patients and controls.
| Parameters | SIF patients (n = 37) | Controls (n = 37) | P value |
|---|---|---|---|
| Age, yr | 70.5 ± 7.4 | 70.7 ± 5.2 | 0.885 |
| Sex (female:male) | 33:4 | 33:4 | |
| Height, cm | 153.4 ± 7.2 | 155.9 ± 6.0 | 0.108 |
| Weight, kg | 57.3 ± 7.4 | 57.4 ± 7.8 | 0.953 |
| BMI, kg/m2 | 24.3 ± 2.4 | 23.6 ± 2.3 | 0.171 |
| BMD, g/cm2 | 0.721 ± 0.104 | 0.746 ± 0.115 | 0.386 |
Values are presented as mean ± standard deviation.
SIF, subchondral insufficiency fracture; BMI, body mass index; BMD, bone mineral density.
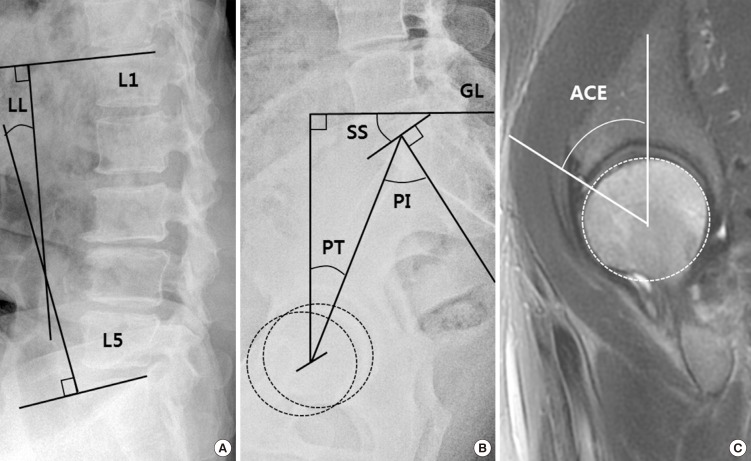
In each hip studied, the lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT) and sacral slope (SS) were measured on the standing lateral view of the spine radiographs (Fig. 3). For radiologic evaluation, the acetabular index (AI), acetabular roof (AR) angle, acetabular head index (AHI), and lateral center-edge (LCE) angle were measured on the hip anteroposterior view. The AI was measured as the angle formed between lateral margin of lateral sourcil and inferior aspect of the pelvic teardrop and the line between the inferior aspects of both pelvic teardrops. The AR angle was between the horizontal line between pelvic teardrops and the line between lateral edge of acetabular roof and intersection of horizontal and vertical components of acetabulum. The AHI was calculated as the ratio of distance between medial tip of femoral head and lateral edge of acetabular roof to the size of femoral head. LCE angle was between line between lateral edge of acetabular roof and center of femoral head and vertical line of hip.
Fig. 3.
Images of the lumbar spine, pelvis, and the hip. (A) The angle of lumbar lordosis (LL) was measured as an angle between line passing through the superior endplates of L1 and S1 by lateral radiograph of the lumber spine. (B) The pelvic incidence (PI) is defined as the angle between the line perpendicular to the sacral slope at its midpoint and the line connecting this point to the axis of the center of the right and left femoral heads by lateral radiograph of the pelvis. (C) On the mid-sagittal MRI, anterior center-edge (ACE) angle which is made by the intersection plane through the center of the femoral head.
PT, pelvic tilt; SS, sacral slope; GL, ground line.
The anterior center-edge (ACE) angle was evaluated on the sagittal view of the MRI scan (Fig. 3C) (13). It was difficult to determine the center of the femoral head after collapse. In collapsed femoral head, the CE angle was measured form the center of the acetabulum instead of the center of the femoral head. Femoral and acetabular anteversion were evaluated on the axial view of the MRI (14). Bone mineral density (BMD) of the proximal femur was measured by dual-energy X-ray absorptiometry (DEXA).
Statistics
We performed a multivariate analysis to identify risk factors for SIF. Statistical analyses were performed using independent t-test with SPSS software version 19 (IBM, New York, NY, USA), and P values less than 0.05 were considered statistically significant.
Ethics statement
The design and protocol of this study were approved by the institutional review board in in Gangnam Severance Hospital (IRB # 3-2013-0197), which waived informed consents of patients.
RESULTS
In the univariate analysis of spinopelvic parameters, LL (P < 0.001) and SS (P < 0.001) were significantly lower and PT (P < 0.001) was higher in SIF patients than controls. Among the parameters of acetabular coverage, LCE angle (P < 0.001), AHI (P < 0.001) and ACE angle (P < 0.001) were significantly lower and AI (P < 0.001) was higher in SIF patients than controls (Table 2).
Table 2. Comparisons of spinopelvic alignment, acetabular coverage and femoral anteversion between SIF patients and controls.
| Variables | SIF patients (n = 37) | Controls (n = 37) | P value |
|---|---|---|---|
| Lumbar lordosis (°) | 26.2 ± 18.9 | 42.6 ± 12.3 | < 0.001 |
| Pelvic incidence (°) | 54.3 ± 12.2 | 55.4 ± 8.3 | 0.657 |
| Pelvic tilt (°) | 29.9 ± 13.1 | 20.5 ± 5.5 | < 0.001 |
| Sacral slope (°) | 24.6 ± 12.9 | 34.9 ± 6.4 | < 0.001 |
| Lateral center edge angle (°) | 21.1 ± 6.6 | 32.3 ± 5.4 | < 0.001 |
| Anterior center edge angle (°) | 43.3 ± 6.7 | 50.7 ± 4.9 | < 0.001 |
| Acetabular index (°) | 45.2 ± 5.7 | 39.5 ± 2.9 | < 0.001 |
| Acetabular roof angle (°) | 10.7 ± 5.0 | 10.2 ± 4.3 | 0.636 |
| Acetabular head index | 75.6 ± 8.1 | 81.9 ± 4.9 | < 0.001 |
| Femoral anteversion (°) | 24.9 ± 7.8 | 24.1 ± 5.7 | 0.598 |
| Acetabular anteversion (°) | 17.7 ± 5.1 | 16.9 ± 4.8 | 0.535 |
Values are presented as mean ± standard deviation.
SIF, subchondral insufficiency fracture.
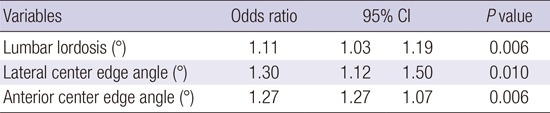
Multivariate logistic regression analysis showed that LL (OR = 1.11), LCE angle (OR = 1.30) and ACE angle (OR = 1.27) were risk factors for SIF (Table 3).
Table 3. Risk factors for SIF in the multiple logistic regression analysis.
| Variables | Odds ratio | 95% CI | P value | |
|---|---|---|---|---|
| Lumbar lordosis (°) | 1.11 | 1.03 | 1.19 | 0.006 |
| Lateral center edge angle (°) | 1.30 | 1.12 | 1.50 | 0.010 |
| Anterior center edge angle (°) | 1.27 | 1.27 | 1.07 | 0.006 |
SIF, subchondral insufficiency fracture.
DISCUSSION
Subchondral insufficiency fracture of the femoral head mainly occurs in the osteoporotic elderly women and in organ transplant recipients (15). It often leads to a rapid and severe collapse of the femoral head, which necessitates a THR. Bone fragility due to osteoporosis is considered the most important cause of SIF, similar to compression fracture of vertebral body. In a recent study, the dysplastic acetabulum was associated with the occurrence of SIF of the femoral head. The deficiency of lateral coverage of the acetabulum, which results in an excessive amount of stress on the femoral head, is also a risk factor of further collapse of the femoral head (3).
We note several limitations of the current study. First, our study was a retrospective review of a small cohort. We might have undiagnosed patients and misdiagnosed patients during the period of enrollment. However, the SIF is not a common disease and a prospective study on a large cohort is difficult to conduct. Second, we did not consider the coronal deformity of the spine such as scoliosis, which might have affected the coronal tilt of the pelvis. In our patients, none had coronal pelvic obliquity more than 10°. Third, we measured the ACE angle on the sagittal view of the hip MRI, which was taken in supine position of the patient. Nevertheless, it was not feasible to obtain a standing lateral view of the pelvis in all of our patients and it was difficult to obtain diagnostic quality images of the pelvis lateral view.
In our study, decreased lumbar lordosis and deficient anterior coverage of the acetabulum were risk factors of SIF as well as deficient lateral coverage of the acetabulum. Since Offierski and MacNab described mechanical interactions between the spine and pelvis, the association between lumbar spine and hip lesions, so called “hip-spine syndrome” has been investigated (16). The incidence of symptomatic osteoarthritis of the hip and degenerative lumbar spinal stenosis is increasing in aging population.
Degenerative kyphosis and vertebral compression fracture are common in the elderly. These two conditions result in a decrease of lumbar lordosis, posterior tilt of the pelvis and subsequent a deficiency in the anterior coverage of the acetabulum. The deficient coverage of anterior acetabulum loads an excessive pressure on the femoral head, which leads to a SIF of the femoral head in osteoporotic patients (17).
The SIF of the femoral head should be differentiated from femoral head osteonecrosis (18,19,20). Both of them have similar radiological and clinical features. A low intensity band lesion, which corresponds to the fracture line, is seen at the subchondral region on T1-weighted MR images in both of the two lesions. However, another band, which represents the reparative zone around the osteonecrotic portion, is seen on MRIs of osteonecrosis, while it is not seen on those of SIF (Fig. 2) (21).
Another type of subchondral fracture of the femoral head, so called subchondral fatigue fracture, has been observed mainly in young military trainees who are not osteoporotic. This type of fracture is considered to be a fractures due to repeated stress on the healthy femoral head (22). In most of the subchondral fatigue fractures, the extent of fracture is small and the depression is focal usually less than 2 mm. Most of subchondral fatigue fracture in young adults heals spontaneously and does not need a surgical treatment while SIF in the elderly is frequently associated with severe collapse and necessitates THR (Fig. 2).
Although the precise prevalence of SIF is not known, a recent study of histopathological re-evaluation has showed that SIF was observed in 6.3% of patients with a preoperative diagnosis of osteoarthritis and 11.1% of patients with that of osteonecrosis (23). Failure to recognize the SIF may lead to a misdiagnosis and erroneous treatment.
This study showed that anterior deficiency of the acetabulum and decrease of lumbar lordosis are risk factors of SIF as well as lateral deficiency of the acetabulum. The results of our study could afford information to diagnose SIF in osteoporotic elderly patients.
ACKNOWLEDGMENT
Each author certifies that his or her institution has approved the human protocol for this investigation, and that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained. This work was performed at the Joint Reconstruction Center, Seoul National University Bundang Hospital.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study concept and design: Jo WL, Lee WS, Koo KH. Coordinated sampling and data collection: Chae DS, Yang IH. Writing the manuscript: Jo WL, Lee WS, Koo KH. Supported collecting the data: Jo WL, Lee KM. Critical review of the manuscript: Koo KH, Jo WL. Approval of final manuscript: all authors.
References
- 1.Yoon PW, Kwak HS, Yoo JJ, Yoon KS, Kim HJ. Subchondral insufficiency fracture of the femoral head in elderly people. J Korean Med Sci. 2014;29:593–598. doi: 10.3346/jkms.2014.29.4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: a case report. Arthritis Rheum. 2005;52:1293–1296. doi: 10.1002/art.20994. [DOI] [PubMed] [Google Scholar]
- 3.Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y. Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fractures of the femoral head. AJR Am J Roentgenol. 2013;201:W97-103. doi: 10.2214/AJR.12.9615. [DOI] [PubMed] [Google Scholar]
- 4.Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, Yanagibashi Y. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine. 2005;30:1650–1657. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]
- 5.Tsuchie H, Yamada S, Tazawa H, Kijima H, Shimada Y. Anterior hip subluxation due to lumbar degenerative kyphosis and posterior pelvic tilt. Case Rep Orthop. 2014;2014:806157. doi: 10.1155/2014/806157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120–1129. doi: 10.2106/JBJS.G.00144. [DOI] [PubMed] [Google Scholar]
- 7.Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol. 1997;168:159–163. doi: 10.2214/ajr.168.1.8976940. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto T, Schneider R, Iwamoto Y, Bullough PG. Subchondral insufficiency fracture of the femoral head in a patient with systemic lupus erythematosus. Ann Rheum Dis. 2006;65:837–838. doi: 10.1136/ard.2005.041095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shibata A, Fukuda K, Inoue A, Higuchi F, Miyake H, Nishi M, Mori M, Ishii S, Nagao M, Yanagawa H. Flushing pattern and idiopathic avascular necrosis of the femoral head. J Epidemiol. 1996;6:37–43. doi: 10.2188/jea.6.37. [DOI] [PubMed] [Google Scholar]
- 10.Sakata R. A case-control study of association between life-style, alcohol dehydrogenase 2 and aldehyde dehydrogenase 2 genotype and idiopathic osteonecrosis of the femoral head. Kurume Med J. 2003;50:121–130. doi: 10.2739/kurumemedj.50.121. [DOI] [PubMed] [Google Scholar]
- 11.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88:1117–1132. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42:2719–2723. doi: 10.1002/1529-0131(199912)42:12<2719::AID-ANR31>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 13.Stelzeneder D, Hingsammer A, Bixby SD, Kim YJ. Can radiographic morphometric parameters for the hip be assessed on MRI? Clin Orthop Relat Res. 2013;471:989–999. doi: 10.1007/s11999-012-2654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Botser IB, Ozoude GC, Martin DE, Siddiqi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy. 2012;28:619–627. doi: 10.1016/j.arthro.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto T. Subchondral insufficiency fractures of the femoral head. Clin Orthop Surg. 2012;4:173–180. doi: 10.4055/cios.2012.4.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Offierski CM, MacNab I. Hip-spine syndrome. Spine. 1983;8:316–321. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Ishihara K, Miyanishi K, Ihara H, Jingushi S, Torisu T. Subchondral insufficiency fracture of the femoral head may be associated with hip dysplasia: a pilot study. Clin Orthop Relat Res. 2010;468:1331–1335. doi: 10.1007/s11999-009-1213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis) N Engl J Med. 1992;326:1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto T, Schneider R, Bullough PG. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol. 2000;24:464–468. doi: 10.1097/00000478-200003000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol. 2001;30:247–254. doi: 10.1007/s002560100348. [DOI] [PubMed] [Google Scholar]
- 21.Ikemura S, Yamamoto T, Motomura G, Nakashima Y, Mawatari T, Iwamoto Y. MRI evaluation of collapsed femoral heads in patients 60 years old or older: differentiation of subchondral insufficiency fracture from osteonecrosis of the femoral head. AJR Am J Roentgenol. 2010;195:W63-8. doi: 10.2214/AJR.09.3271. [DOI] [PubMed] [Google Scholar]
- 22.Song WS, Yoo JJ, Koo KH, Yoon KS, Kim YM, Kim HJ. Subchondral fatigue fracture of the femoral head in military recruits. J Bone Joint Surg Am. 2004;86-A:1917–1924. doi: 10.2106/00004623-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Yamamoto T, Iwamoto Y, Schneider R, Bullough PG. Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis. 2008;67:150–153. doi: 10.1136/ard.2006.066878. [DOI] [PubMed] [Google Scholar]