Abstract
In vitro liver cell culture models are gaining increasing importance in pharmacological and toxicological research. The source of cells used is critical for the relevance and the predictive value of such models. Primary human hepatocytes (PHH) are currently considered to be the gold standard for hepatic in vitro culture models, since they directly reflect the specific metabolism and functionality of the human liver; however, the scarcity and difficult logistics of PHH have driven researchers to explore alternative cell sources, including liver cell lines and pluripotent stem cells. Liver cell lines generated from hepatomas or by genetic manipulation are widely used due to their good availability, but they are generally altered in certain metabolic functions. For the past few years, adult and pluripotent stem cells have been attracting increasing attention, due their ability to proliferate and to differentiate into hepatocyte-like cells in vitro. However, controlling the differentiation of these cells is still a challenge. This review gives an overview of the major human cell sources under investigation for in vitro liver cell culture models, including primary human liver cells, liver cell lines, and stem cells. The promises and challenges of different cell types are discussed with a focus on the complex 2D and 3D culture approaches under investigation for improving liver cell functionality in vitro. Finally, the specific application options of individual cell sources in pharmacological research or disease modeling are described.
Keywords: Liver cell culture, in vitro models, 3D culture technologies, primary human hepatocytes, liver cell lines, stem cells
Introduction
Various in vitro liver cell culture models are under development to address the need for predictive models in drug development and research. Significant progress has been made within the last few years in the improvement of culture systems, leading to the enhanced stability and functionality of liver cells in vitro. However, a major bottleneck in the use of in vitro human hepatic models is the identification of suitable liver cell sources.
The main criterion for evaluation of the value of hepatic cells in basic research or pharmacological studies is the expression of typical hepatic functions and metabolic pathways. Important functions of the liver include: (i) metabolism of endogenous substrates (e.g. cell products) and exogenous compounds (e.g. drugs, chemicals); (ii) regulation of amino acids, carbohydrates, and fatty acids, (iii) synthesis of proteins, such as albumin or transferrin; and (iv) activation of inflammatory and immune reactions upon liver injury due to disease, drug, or toxin exposure.
Depending on the study aim and design, the cell type used in hepatic in vitro research has to fulfill each or some of those functions to reflect the situation in the native organ in vivo. Furthermore, preservation of hepatocyte functionality over several hours (e.g. for short-term studies on drug metabolism) or up to several days or even weeks (e.g. for long-term studies on subacute or subchronic drug toxicity) is needed to acquire relevant data. Since the stability and maintenance of the differentiated state of liver cells depends on both, the cell type used and the method of cultivation (e.g. 2D cultures or complex 3D cultures), the choice of culture model in association with a specific hepatic cell source is critical for the success of individual hepatic in vitro studies. In addition, standardization of experiments is required to provide reproducible and reliable results from in vitro hepatic cultures. Thus, a constant quality of the cells needs to be ensured and verified by appropriate quality control measures. Finally, the availability of cells is a critical factor for the usage of certain cell types in in vitro research. This aspect is of particular importance for studies requiring large numbers of cells and/or experiments.
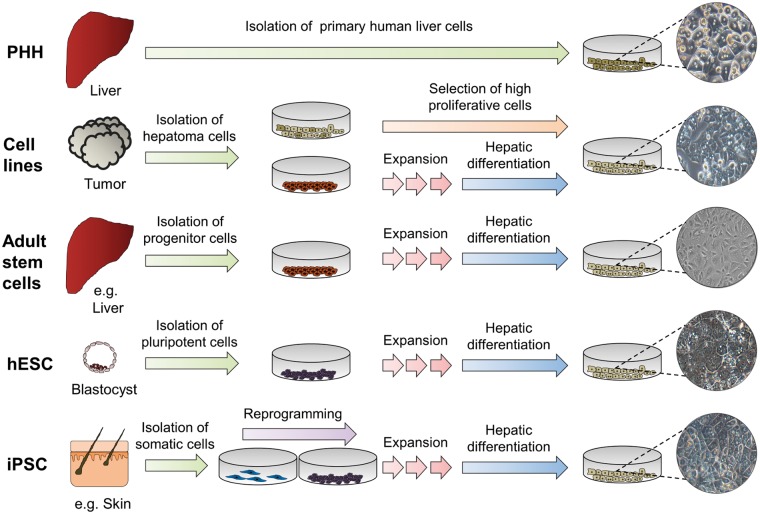
In this review, the liver cell sources currently used are critically reviewed with their respective advantages and disadvantages with regard to their in vitro applications in drug testing and hepatic disease research. Since the predictive value of animal-derived cells is limited due to species-dependent differences in the expression of metabolic enzymes and pathways, this review focuses on human hepatic cells from different sources, namely primary human liver cells, liver cell lines and stem cells, as shown schematically in Figure 1. In addition, approaches for increasing the functionality and stability of liver cells in vitro by the use of complex 2D and 3D culture models are discussed.
Figure 1.
Processing of cells derived from different sources for the generation of human in vitro liver cell culture models. Major cell types include primary human hepatocytes (PHH), hepatoma cell lines, adult stem cells, human embryonic stem cells (hESC), and induced pluripotent stem cells (iPSC). Whereas PHH can be used for in vitro cultivation immediately after isolation, liver cell lines or stem cells need to be expanded and/or differentiated prior to their use in experiments. (A color version of this figure is available in the online journal.)
Primary human liver cells
General characteristics of primary human liver cells
Primary human liver cells are still considered to be the gold standard for the creation of human-relevant in vitro liver cell culture models. Due to their origin in native liver, they reflect the complete functionality of the human organ in vivo and thus provide highly predictive results in pharmacological and toxicological in vitro research. Furthermore, the fact that each preparation is obtained by a different donor offers the opportunity to analyze a broad range of genetic polymorphisms using individual cell isolates. On the other hand, interindividual differences and cell alterations due to the isolation procedure also cause some variations in experimental results, which make the standardization of models difficult. In addition, the scarce availability and difficult logistics of primary human liver cells prevent a larger scale use of the cells. In the following, critical aspects of the use of primary human liver cells for in vitro research are reviewed, including approaches to isolation, cryopreservation, and cultivation.
Cell types of the liver
The composition of the liver can be divided into two major classes of cells. Parenchymal cells of epithelial origin, namely hepatocytes and cholangiocytes, form the main liver mass1 and represent 70 and 3–5% of the total liver cell population, respectively, as shown in rodents.2 Non-parenchymal cells (NPC) account for approximately 25% of the total liver cell population, consisting mainly of Kupffer cells, liver endothelial cells, and hepatic stellate cells.3
Isolation of primary human liver cells
Primary human hepatocytes (PHH) are usually isolated from whole livers (not used for orthotopic transplantation) or resected liver tissue.4 The development of the two-step collagenase perfusion technique introduced by Seglen and Reith5 in 1976 was a key step and has become the centerpiece of isolation protocols for PHH. Since then, this method has been modified and optimized in various regards.6 Recent modifications have involved adaptations for parallel isolation and separation of NPC. Supplementation of the collagenase P containing perfusion solution with 10% fetal calf serum (FCS) allows a prolonged but mild tissue digestion, resulting in a high yield and quality of parenchymal and non-parenchymal liver cells from a single donor’s tissue.3 In another approach, density gradient separation of NPC in iodixanol and magnetic-activated cell sorting has been used for efficient separation of individual NPC populations.7
The cell isolation outcome depends on donor characteristics and intraoperative factors, in addition to tissue processing and cell isolation conditions.8 Lee et al. investigated the PHH isolation outcome of 1034 donors.9 The study revealed that cell viability was significantly influenced by donor characteristics, such as age, body mass index, liver fat content, liver damage (e.g. fibrosis), and the resulting changes in the clinical parameters in the blood (e.g. liver enzymes, bilirubin). In addition, the blood coagulability, warm ischemic time in vivo during surgery, and cold ischemic time in vitro during tissue transport were identified as critical factors for the success of the isolation. Surgical procedures which involve increased warm ischemia times, e.g. due to clamping during surgery, can lead to an impaired yield and viability of PHH.8 In contrast, portal vein embolization showed no negative influence on isolation outcome,10 and the yield of PHH was even increased with warm ischemia times ex vivo, and when the patients received chemotherapeutic treatment.9 Furthermore, the type of disease was identified to have a significant impact upon the cell yield.11 In particular, alcohol-related liver diseases were shown to cause alterations in hepatocyte function in culture.11
Apart from resected liver tissue, liver grafts excluded from liver transplantation or explanted diseased livers are potential sources of PHH. Human liver cells isolated from explanted livers obtained from recipients with moderate alterations in blood parameters (low labMELD score) were comparable in viability and function to cells obtained from specimens following partial liver resection.4
Cryopreservation of primary human liver cells
One major limitation of primary human liver cells is the availability of human tissue of good quality. The logistics and the isolation process require the staff to be experienced and to cooperate closely with surgical clinics. Therefore, a well-organized network of surgeons, biologists, and technicians is needed to obtain high quantities of high quality cells. Cryopreservation was introduced to overcome this hurdle and to provide primary human liver cells on a regular basis. A multitude of cryopreservation protocols for hepatocytes is available, which are mostly based on the use of cryoprotectants such as dimethyl sulfoxide (DMSO), albumin, FCS, and/or polyvinylpyrrolidone.12 Successful cryopreservation critically depends on the cells being of good quality. In order to increase cell viability after freezing and thawing, preincubation with cryoprotectants like fructose and dithiothreitol or DMSO has been investigated.13,14 Other approaches use a modified basic cryopreservation solution, e.g. HepatoZYME-SFM15 or STEM-CELLBANKER®,16 resulting in increased cell viability and function after thawing.
The isolation of NPC is a younger discipline and cryopreservation is still under development. Successful cryopreservation of rat and human Kupffer cells with high post-thawing cell survival and no alterations in physiological characteristics were introduced by Walbrun et al.,17 using a standard cryopreservation technique based on RPMI medium with FCS and DMSO frozen down to -80℃ using a cooling gradient. The cryopreservation of hepatic stellate cells requires more elaborated preservation methods due to the sensitivity of intracellular lipid droplets to freezing. A complex protocol for the storage of rat hepatic stellate cells using a precultivation step, a cryopreservation medium containing FCS and DMSO as cryoprotectants, and a complex freezing gradient was demonstrated to maintain the functional and structural integrity of the cells after cryopreservation.18 A more simple protocol using the cryopreservation solution STEM-CELLBANKER® was applied by Nakamura et al.19 showing that cryopreservation of hepatic stellate cells in different stages of activation is possible. Cryopreservation protocols specific to liver endothelial cells have not yet been described. However, the cryopreservation of endothelial cells from other tissues has been recently shown.20 Furthermore, standardized protocols for the freezing of endothelial cells from umbilical cord veins under Good Manufacturing Practice conditions have been established,21 which may also be tested for the cryopreservation of liver endothelial cells.
In vitro processing of primary human liver cells
PHH display the in vivo hepatic situation best during short-term cultivation regimes; when cultured over extended periods these cells manifest a progressive loss of the hepatocellular phenotype, both in terms of morphology and functionality. This de-differentiation process starts during the isolation process.22 Hepatocytes are arranged in sheets of one or two cells in thickness in the liver lobule. The plasma membrane of hepatocytes is divided into different membrane areas exhibiting specific tasks, the apical membrane forming the bile canalicular network and the lateral membrane forming the cell–cell connection with adjunct hepatocytes. The basolateral membrane area is oriented toward the liver sinusoid and interacts with the collagen I-rich matrix in the space of Disse, which separates the liver sinusoidal endothelial cells from hepatocytes. During the isolation process, cell–cell connections and cell–matrix interactions are disrupted and as a consequence the hepatocytes lose their polarization. Moreover, the low-speed centrifugation of the hepatocyte cell suspension performed for removal of cell debris leads to partial loss of NPC, which are critical for the support of hepatocyte polarity in vitro.6
NPC, as well as other parenchymal cells, induce a quiescent G0 state in the hepatic cell cycle in vivo via cell–cell connections and soluble factors. Reperfusion injury during the isolation procedure induces oxidative stress, leading to activation of intracellular inflammatory pathways.23 Additionally, the hepatocytes may come into contact with lipopolysaccharides (LPS) contained in collagenase P preparations from bacterial origin. Disruption of the tissue integrity as well as activation of inflammatory signaling has been reported to trigger hepatocytes to re-enter the cell cycle in the G1 phase.24 The proliferative priming is associated with a change in the expression pattern and consequently a loss of differentiated functions, in particular xenobiotic metabolism, urea formation, and albumin synthesis, among others.25 This detrimental process of de-differentiation can be influenced by the cultivation strategy, as described in the following.
2D and 3D culture models for PHH
The conventional 2D culture of hepatocytes is easily achievable and thus represents the most common culture strategy. In standard 2D culture systems, PHH are directly plated on collagen-coated plastic dishes that allow cell attachment to form a confluent monolayer.26 In comparison to hepatocytes maintained in suspension, these adherent cultures show increased enzyme stability and therefore can be used for the evaluation of metabolic stability of xenobiotics over several hours to days.27 Recent investigations into drug transporter expression in 2D hepatocyte cultures revealed a polarized location of major sinusoidal and canalicular transporters in conjunction with corresponding transporter activities.28 However, there is evidence that PHH cultured in conventional 2D systems for a prolonged time period display morphological alterations, provoked by an epithelial–mesenchymal transition leading to a loss of hepatocyte polarity and associated liver function.29
Typical strategies to prevent the de-differentiation of PHH in vitro aim to reestablish the microenvironment of the liver, consisting of cell–cell contacts, cell–matrix interactions, and soluble factors. In this regard, the 3D cultivation of PHH has gained increasing attention. It has been shown that 3D culture of PHH in a sandwich configuration between two layers of extracellular matrix (ECM) enables the hepatocytes to adhere three-dimensionally, leading to the formation of in vivo like cell–cell contacts and cell–matrix interactions.29,30 The ECM composition appears to influence the cell shape and cell–cell contacts between hepatocytes.31 It has been shown that the maintenance of xenobiotic metabolism in hepatocyte cultures depends primarily on the formation of proper cell–cell contacts,32 whereas hepatic transport processes are mainly dependent on the repolarization linked to cell–matrix interactions.22 The ECM components used for sandwich culture of hepatocytes are rat-tail collagen, Matrigel (a mixture of basal membrane components derived from mouse sarcoma) or various combinations of both matrices.33 Transcriptional profiling revealed an improved expression of effectors of energy metabolism and bile acid metabolic pathways in hepatocytes cultured between two layers of collagen.34 Similarly, covering hepatocytes with Matrigel has been shown to improve cellular stress responses by reducing the expression of pro-inflammatory mediators and the genes associated with integrin pathways.35 More advanced 3D cultures mimic the liver microenvironment in cross-linked hyaluronic acid gels supplemented with soluble ECM from de-cellularized organs to improve hepatocyte attachment and viability.36
A scaffold-free approach to establish 3D conditions for PHH is based on the self-aggregation of the cells leading to the formation of spheroids. Such spheroid cultures can be obtained either by gravity-enforced cellular assembly in a hanging drop37 or by seeding the cells in low-attachment culture vessels.38,39 In both cases the obtained spheroids were shown to exhibit liver-specific functions for up to five weeks for long-term toxicity testing.37,38 Spheroid cultures can also be used for the creation of larger constructs reflecting the physiological liver architecture. For example, PHH aggregates encapsulated in hydrogels maintained a stable hepatocyte phenotype for 21 days.40 Such cell-laden hydrogels can be assembled by multiphase liquid–liquid systems to create 3D tissue constructs, as shown initially for mouse fibroblasts.41 In another strategy the PHH spheroids are loaded into a bioprinter that deposits the cell aggregates simultaneously with a support structure (often hydrogel) according to a specific design template resembling the liver architecture.42,43 Such “liver-on-a-chip” approaches provide an attractive tool to generate 3D hepatocyte cultures reflecting the in vivo situation at a microscale with reduced cell numbers for toxicity studies.
Co-culture of hepatocytes with NPC
Apart from hepatocyte cell–cell connections and cell–matrix interactions, the crosstalk of hepatocytes with NPC via soluble factors and cell–cell connections plays a central role in liver physiology and the maintenance of hepatocyte differentiation.44 Recently described co-culture models of PHH and Kupffer cells enabled the evaluation of hepatocyte reactions in a pro-inflammatory environment.45,46 A co-culture model using established cell lines for hepatocytes and stellate cells displayed remodeling processes of ECM components after the induction of hepatic steatosis.47 Co-culture of PHH with endothelial cells was shown to support hepatocytes in the maintenance of their phenotypic morphology and in the improvement of their specific functions, in addition to the formation of capillary-like structures by co-cultured endothelial cells.48 Recent approaches to stabilize hepatic functions of PHH are based on micropatterning techniques, which allow controlling the cell arrangement in co-culture platforms (micropatterned co-culture [MPCC]). The co-cultures in MPCC are created by seeding the hepatocytes on collagen-coated spots, which are surrounded by supporting cells, e.g. fibroblasts.49,50 Using a number of clinically relevant drugs Khetani et al. could show a higher sensitivity of the MPCC as compared to conventional short-term cultures for prediction of human hepatic drug toxicity.51
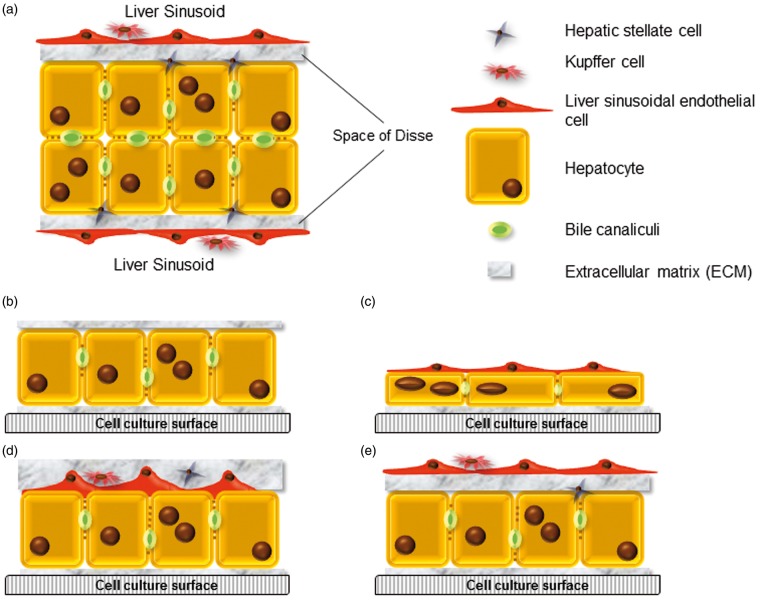
More sophisticated tissue engineering strategies, considering the specific requirements of individual cell types, have to be conceived for the co-cultivation of more than two cell populations. For example, Kupffer cells (but also other NPC) have to undergo a recovery phase before the start of experiments to avoid activation due to the cell stress induced by the isolation procedure.3,52 Two major approaches were attempted for the realization of complex co-culture models: One approach focuses on the use of mixtures of PHH and one or more NPC populations to allow for spontaneous re-aggregation and the formation of self-organized cell–cell contacts resulting in organoids.37 The second approach is based on targeted engineering of individual layers of PHH and NPC to create in vitro tissues reflecting the tissue architecture.53 Concepts for the establishment of co-culture models utilizing hepatocytes and various NPC fractions are shown in Figure 2.
Figure 2.
Approaches for improved co-culture liver models aim to approximate the structure of the native liver. (a) Schematic image of the tissue architecture in the liver sinusoid, (b) current 3D sandwich culture with primary human hepatocytes (PHH) embedded between two layers of extracellular matrix (ECM), e.g. gelled collagen,29 (c–e) Potential concepts for 3D co-cultivation of PHH with non-parenchymal cells (NPC): (c) PHH grown on an ECM layer and overlaid with NPC, e.g. liver sinusoidal endothelial cells, (d) mixture of PHH and NPC, cultured between two layers of ECM, (e) tissue-engineered liver model consisting of PHH and hepatic stellate cells cultured in a sandwich configuration and overlaid with NPC fractions, e.g. liver sinusoidal endothelial cells and Kupffer cells. Different cell culture surfaces, such as plastic or membranes permeable for gas or solutes can be used. (A color version of this figure is available in the online journal.)
Dynamic 3D culture technologies and bioreactor approaches
Dynamic 3D culture models are of increasing importance in in vitro hepatic research, since they better reflect the perfusion conditions in the native tissue when compared to static culture systems. A number of studies have shown the potential of 3D perfusion culture to support the organoid-like cell assembly of human hepatocytes. For example, a perfused 3D microfluidic human liver model was reported to support liver-typical cell arrangement and morphology.54 Similarly, human hepatocytes, maintained in the microfluidic LiverChip™ system showed differentiated tissue structures and cytochrome P450 (CYP)-dependent activities over seven days of culture.55 In further approaches, microfluidic devices were used with various combinations of cell types and ECM components, such as co-culture of hepatocytes with intestinal cells for investigations of drug adsorption and metabolism,56 hepatocyte culture in a collagen sandwich configuration with flow characteristics,57 or using de-cellularized scaffolds as a physiological matrix for cell maintenance under dynamic conditions.58,59
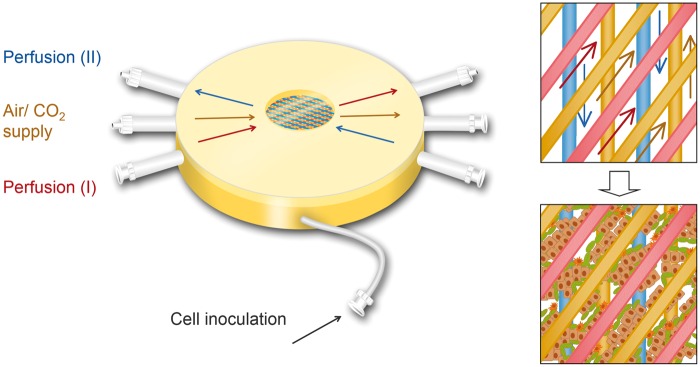
The need for both efficient medium and oxygen transfer to the cells while allowing 3D tissue assembly is addressed by a dynamic four-compartment 3D bioreactor technology for high-density liver cell culture.60 The bioreactor structure is illustrated in Figure 3. Cells are cultured within a 3D scaffold made of different types of hollow-fiber capillaries, which are arranged in two or more layers composed of medium and oxygen capillaries. The capillary membranes enable the transfer of solutes via hydrophilic membranes and gas exchange via hydrophobic membranes, in addition to their function as an adhesion matrix for the cells cultured between the capillaries. By this way, four compartments (two counter-currently perfused medium compartments, one gas compartment and the cell compartment) are created, which form multiple repetitive units for the decentralized supply of cell aggregates with low gradients. To ensure constant culture conditions, bioreactors are operated in a perfusion device, which enables electronic control of temperature, medium perfusion rates, gas mixture, and gas supply.
Figure 3.
Miniaturized four-compartment bioreactor for high-density perfusion culture of liver cells.66 The bioreactor technology is based on two or more layers of hollow-fiber capillaries, which serve for counter-current medium perfusion (marked in red and blue) and air/CO2 supply (yellow). Cells are inoculated into the extra-capillary space (cell compartment). The schematic pictures on the right show the capillary structure viewed from top before and after cell seeding. (A color version of this figure is available in the online journal.)
Based on large-scaled versions of the technology used for clinical extracorporeal liver support therapy,61,62 the technology was scaled down to small-scale laboratory bioreactors to reduce the cell number and amount of reagents needed for in vitro pharmacological studies.63,64 Histological and immunohistochemical studies revealed the spontaneous reorganization of primary human parenchymal and non-parenchymal liver cells (biliary cells, endothelial cells, stellate cells, Kupffer cells) between the capillaries.63 These studies also showed hepatocyte polarization, as assessed by the detection of apical membrane transporters, such as multidrug-resistance-associated protein 2, multidrug-resistance protein 1, and breast cancer resistance protein. The stable maintenance of differentiated functions of primary human liver cells in the bioreactor under serum-free conditions was shown in miniaturized bioreactors.65 A better preservation of drug-metabolizing enzymes was also observed in the bioreactor system when compared to static 2D cultures.66 Thus, the technology provides suitable conditions for pharmacological studies with human hepatocytes and shows the benefit of dynamic 3D culture conditions for long-term preservation of liver-specific functions in vitro.
Liver cell lines
General characteristics of liver cell lines
Human hepatic cell lines generated from tumor tissue or by the genetic engineering of primary human liver cells are widely used in in vitro culture models due to their good availability. The high proliferation capacity and the stable metabolism of the cells make them an attractive tool for in vitro studies under standardized and reproducible conditions. However, the high proliferation potential of transformed cell lines generally is associated with a loss of differentiated functions, leading to some deficiencies in functional performance. Therefore, applications of liver cell lines in in vitro research have to take into account the specific functional properties of the cell line used.
Applications of liver cell lines in in vitro research
Tumor cell lines, such as the hepatoma cell line HepG2, are of particular interest for in vitro studies on cancer development and therapy. Reports focus on the investigation of specific metabolic pathways related to liver tumors or the testing of drug candidates for cancer therapy. In order to cover the different types of cancer with different sensitivities, assays are often performed in various tumor cell lines from different origins in parallel. For example, HepG2 cells and two human cholangiocarcinoma cell lines were used in a recent study to analyze the expression and regulation of cancer-related transcription factors and showed some variation in their responses.67 In another study, liposomal C8 ceramide was shown to have a tumor-suppressive effect in several hepatocellular carcinoma cell lines, including HepG2 cells, while non-tumor hepatocytes remained unaffected.68 The HepG2 cell line has also been used in various studies on drug metabolism and hepatotoxicity, e.g. on acetaminophen toxicity and prevention.69 However, alterations in the hepatocyte-specific functions of the cell line due to transformation limits how closely these results relate to results for humans.
The HepaRG cell line generated from human hepatoma cells represents a promising alternative to the use of PHH for many studies on drug metabolism, disposition, and toxicity.70,71 Differentiation of the cell line is induced by treatment with DMSO and leads to the generation of both hepatocytes and biliary cells. HepaRG cells show a high grade of differentiation and expression of typical hepatic functions, including CYP-dependent metabolism, CYP induction, and drug transporter expression.72 Evaluation of HepaRG cells as a model for drug toxicity testing showed a similar response to the effects of acetaminophen as PHH and a higher activation of genes related to liver damage as compared to HepG2 cells.73 However, other studies showed a reduced sensitivity of HepaRG cells to the detection of hepatotoxic drugs.74 These findings are in line with the discrepancy observed between HepaRG cells and PHH in the activation of apoptosis or necrosis upon exposure to acetaminophen.75 Thus, HepaRG cells could preferably be used as a substitute to PHH in screening studies for CYP induction.
Strategies for improving the functional performance of hepatoma cell lines
To increase the functional performance of hepatoma cell lines, various strategies for genetic modification of the cells have been described. For example, transfection of HepG2 cells with human augmenter of liver regeneration resulted in increased synthesis of alpha-fetoprotein, urea, and albumin in comparison to non-transfected control cells.76 An improvement in liver-specific functions, including expression of drug-metabolizing enzymes, was also observed after transient transfection of human hepatic cells with hepatocyte nuclear factor 4 alpha (HNF4α).77 Using a lentiviral expression system, a range of cell lines were generated that express specific CYP enzymes individually and thus can be used to assess metabolism-associated toxicity of drugs.78 In another strategy, transduction of PHH with selected immortalization genes was used to generate proliferating cell lines with liver-specific functionality.79
Further approaches to improving the functional performance of hepatoma cell lines are directed toward creating a microenvironment favoring cell differentiation and liver-typical cell assembly in vitro. For example, spheroid culture of HepG2 cells in a 3D matrix using different types of hydrogels (transglutaminase-cross-linked gelatin, collagen type I, and growth-factor depleted Matrigel) was associated with enhanced hepatocyte-like properties, when compared with conventional cell culture.80 Microencapsulation of HepaRG cells in alginate spheroids was shown to support polarization of hepatocyte-like cells, which were arranged in an interconnected bile canalicular network and showed biliary transporter activity.81 Tissue-like cell organization of HepaRG was also observed in four-compartment hollow-fiber bioreactors in conjunction with stable activities of several human-relevant CYP enzymes over several weeks.82 These studies emphasize the importance of a physiological environment to enhance the predictivity and stability of hepatic in vitro models.
Stem cell-derived hepatocytes
General characteristics of stem cells
Stem cells characterized by their ability to proliferate and to differentiate into specific cell types in vitro offer the option to generate mature hepatic cells in large amounts with constant quality for in vitro investigations. In accordance to their differentiation potential and origin, stem cells can be classified into two major groups: (i) adult stem cells originating from liver or from non-hepatic cells, e.g. mesenchymal stem cells (MSC), and (ii) pluripotent stem cells, represented mainly by human embryonic stem cells (hESC) and human-induced pluripotent stem cells (hiPSC). Differences in the proliferation and differentiation properties of adult and pluripotent stem cells are responsible for their individual advantages and drawbacks in in vitro applications.
Adult stem cells
Adult stem cells have been described in the liver as hepatic stem cells,83 small hepatocytes,84 or progenitor cells,85 based on functional and morphological criteria. Different methods for isolation, culture, and differentiation of liver stem cells from human adult or fetal liver have been described.86–88 In vitro studies on adult stem cells from human or mouse liver showed that their in vitro behavior is influenced by cytokines, growth factors, hormones, and ECM proteins.89–91 The importance of soluble factors is emphasized by the observation of progenitor activation in human liver cell bioreactors perfused with plasma from acute liver failure patients.60 However, the production of larger cell numbers and standardization of the isolation and culture methods for in vitro applications remain a challenge.
MSC, able to differentiate into hepatocyte-like cells, have been detected in various tissues, including bone marrow,92 adipose tissue,93 and umbilical cord blood or tissue.94 MSC are of particular interest in regenerative medicine, such as cell transplantation in liver diseases, since they allow autologous therapy with the patients’ own cells and the safety risk is low when compared, for example, with pluripotent stem cells. However, there is some evidence that they could also be used in in vitro research if differentiation of these cells into fully maturated cells is achieved.95,96 Approaches to enhance the differentiation potential of MSC in vitro are mainly based on improving the culture environment. For example, human umbilical cord MSC differentiated in embryonic body-like aggregates by the addition of insulin-like growth factor 1 and further growth factors showed hepatocyte-like functions, including the expression of hepatic cytokeratins and albumin, as well as glycogen storage.97 Hepatic differentiation of mesenchymal stromal cells was also accelerated by promoting mesenchymal-to-epithelial transition through Rac1 inhibition with small molecules.98 However, further research is required to provide evidence of the predictive value of mesenchymal-based models in pharmacological or toxicological research.
A further promising approach is based on the transdifferentiation of pancreas-derived progenitor cells by the addition of glucocorticoids.99 Studies using cells from rat pancreatic tissue showed stable expression of hepatic markers, including liver-typical CYP enzyme activities in 2D cultures100 or 3D bioreactors.101 More recently, this method was also successfully applied for hepatic transdifferentiation of acinar cells from human tissue.102 Thus, the technology could be used to generate an easily renewable and cost-efficient source of functional human hepatocytes in vitro for usage in hepatic metabolism and toxicity studies.
Human pluripotent stem cells
Sources for pluripotent stem cells
Pluripotent stem cells represent a promising source to produce different cell types for application in pharmacological drug screening and toxicity testing.103 Initial research on pluripotent stem cells was performed using hESC generated from blastocysts,104 which raised ethical concerns about the use of hESC in research. For the past few years, hiPSC generated by reprogramming of adult cell types from various tissues105,106 have been gaining increased importance as an ethically accepted alternative to embryonic stem cells. Similar to hESC, hiPSC are able to differentiate into all three primary germ layer derivatives, i.e. ectoderm, mesoderm, and endoderm, and show a nearly unlimited capacity for proliferation. In addition, hiPSC can be derived from various individuals and from different patient groups, making them an attractive model for studying specific diseases and therapeutic approaches, in addition to their applications in pharmacological research.
Protocols for hepatic differentiation of pluripotent stem cells
To date, a number of protocols have been established for hepatic differentiation of hESC or hiPSC. These approaches are generally based on mimicking the embryonic development of the liver by adding the different growth factors necessary for each developmental stage. Activin A and Wnt3a107,108 are the most important cytokines for definitive endodermal commitment, although fibroblast growth factor 2 and bone morphogenetic protein 4 also play important roles.109,110 Hepatocyte growth factor and oncostatin M are the most commonly used cytokines for hepatic maturation.109,111,112 Although various modifications of cytokine concentration, application periods, and combinations were investigated, all of the protocols so far show that the hepatocyte-like cells (HLC) obtained still show an immature phenotype with reduced hepatic functionality when compared to PHH.113,114
Approaches for the improvement of hepatic maturation
Strategies to improve the hepatic differentiation of pluripotent stem cells mainly focus on 3D culture approaches, co-culture with various cell types, and the direction of lineage-specific pathways.
One field of intense research is the development of 3D culture models, which address the needs of the cells in their natural environment. In particular, the maintenance of physiological cell–cell contacts has been shown to be crucial for the preservation of the mature hepatic phenotype.115 Under this view, hepatic differentiation was performed in differently scaled 3D culture models. Microscale approaches are mainly based on 3D cell aggregation in matrices like collagen,116 alginate,117 hydrogel,118 or Matrigel.119 Liver-specific parameters, such as albumin production, urea secretion, and CYP expression indicate a higher grade of hepatic differentiation in these models when compared to conventional 2D cultures. In a larger scale approach, hepatic differentiation of hESC was investigated in perfused 3D four-compartment hollow-fiber bioreactors with a cell compartment volume of 2–8 mL. Sivertsson et al.120 were able to show a down-regulation of pathways associated to apoptosis, cancer, and proliferation in these 3D bioreactors in addition to significantly higher expression of CYP7A7, CYP2C9, and CYP3A4. In addition, formation of bile duct-like structures positive for cytokeratin (CK) 19 and CK 7 were observed after hepatic differentiation of hESC in the bioreactor system.121
Different co-culture models were investigated in an effort to mimic the physiological environment during embryonic development, often in combination with 3D cultures. Seeding of hiPSC-derived hepatic endodermal cells with human umbilical vein endothelial cells and human MSC in 2D culture vessels resulted in the formation of 3D cell clusters that showed a significantly increased expression of early hepatic marker genes.122 Moreover, transplantation of these liver buds prevented drug-induced lethal liver failure in an in vivo mouse model. Other studies reported successful usage of fibroblasts123–125 or human hepatic stellate cells126 in co-culture with human pluripotent stem cells during hepatic differentiation. To simulate the in vivo liver architecture even more closely, co-culture of HLC with NPC and biliary cells generated from pluripotent stem cells has been investigated in some recent studies. Co-culture of hiPSC-derived hepatocytes and endothelial cells facilitated the vascularization of cell aggregates and resulted in increased albumin secretion.127 In addition, protocols for the directed differentiation of hiPSC into cholangiocytes were described.128–130 Sancho-Bru et al.131 observed the generation of mesodermal cells that expressed genes and proteins of liver endothelial cells and stellate cells during hepatic differentiation of mouse iPSC. Since hepatic stellate cells represent the central cells responsible for liver fibrosis132 these cells would be also of interest for the development and/or testing of specific antifibrotic drugs.
A different strategy for the improvement of hepatic maturation focuses on the inhibition of signals that drive differentiation into alternate lineage pathways, e.g. mesoderm and ectoderm, to obtain highly pure populations of differentiated endoderm.133 In a complementary approach, overexpression of certain hepatocyte genes such as hematopoietically expressed homeobox134 or HNF4α135 has been shown to improve hepatic differentiation.
There are some indications that the incomplete differentiation of hiPSC is caused by a residual donor cell memory, which may impact their capacity to differentiate into the desired cell type.136 The importance of epigenetic regulation in cell differentiation is supported by the finding that the DNA methylation of different CYP genes differs significantly between hESC-derived hepatocytes and PHH.137 Thus, the derivation of hiPSC lines from hepatic cells could lead to enhanced hepatic differentiation, as already reported for mouse iPSC.138 However, the so-called epigenetic memory is also influenced by the culture conditions, e.g. the number of passages.139 Moreover, the genetic variability of individual donors was shown to influence the differentiation outcome more than the parental cell type memory, underlining the importance to select cells from a large number of donors to obtain representative results.140
Quality control and standardization of hiPSC-derived cell preparations
Due to the lack of standardized criteria for hepatic cells derived from pluripotent stem cells, it is difficult to compare the success of different approaches and to identify promising modifications that may enhance hepatocyte maturation. In addition, a uniform benchmark for control and evaluation of the differentiation outcome is missing. Common benchmarks are internal controls (e.g. optimized versus previous method),118,121,127 hepatic cell lines112 and PHH from fetal or adult origin, cultured or freshly isolated.113,114
It is essential that differentiation protocols are highly reproducible for in vitro pharmacological and toxicity studies. Most of the current differentiation protocols apply defined serum-free culture media with recombinant growth factors. However, Matrigel, which is of biological origin with batch-to-batch variations, is still commonly used for the coating of culture vessels.117,134,137 To enable better defined culture conditions, Matrigel was replaced in a number of studies by defined matrix components such as E-cadherin,111,141 vitronectin,142 or laminin.107 A further possibility to increase reproducibility is to substitute recombinant growth factors with small molecules during the hepatic differentiation of pluripotent stem cells.143,144 To ensure a constant quality and functionality of differentiated cell preparations, cryopreservation of large batches of pluripotent stem cell-derived hepatocytes would be helpful, enabling an on-demand cell supply. To date there is little data available on freeze–thaw cycles for cryopreservation of HLC. Mandal et al.145 demonstrated that the cells were highly viable after long-term cryopreservation over several months, attached to the culture surface, and displayed a range of liver-specific markers and functions.
Application of hiPSC-derived hepatocytes
An important application for hiPSC is in pharmacological research and development. For example, maintenance of hiPSC-derived hepatocytes for up to two weeks was reported, enabling repeated–dose chronic exposure to hepatotoxic compounds.146,147 Studies on MPCC with hiPSC-derived human hepatocytes148 indicate a similar sensitivity toward drug toxicity as observed in MPCC using PHH.51 In addition, hepatocytes generated from pluripotent stem cells have been successfully applied in in vitro studies on infectious diseases like hepatitis B and C infection149,150 or malaria pathogenesis.151 Moreover, inherited metabolic liver diseases can be modeled by reprogramming cells from those patients and differentiating hiPSC into the affected cell type, as shown for α1-antitrypsin deficiency, familial hypercholesterolemia, and glycogen storage disease type 1a.152,153 Another exciting field of application can be seen in testing candidate compounds in cell-based assays from a large panel of patient-derived hiPSC in a so-called in vitro clinical trial. More evidence could be provided to show that hiPSC-derived hepatocytes can reproduce inter-individual differences in hepatic metabolism and responses to drugs.154,155 Thus, such strategies could be helpful to recapitulate genetic polymorphisms and to determine the range of drug responsiveness in different patients before these compounds are tested in clinical trials.
Conclusion
In order to meet the need for predictive in vitro hepatic models for studies in drug testing and disease research, human liver cells reflecting the functional performance of the organ in vivo are required. In addition, cells have to be available in large numbers and at a constant quality for use in larger scale screening studies. An ideal cell source would meet all of these criteria to be used in all kinds of studies (“one-for-all”). However, each of the currently available liver cell sources has specific advantages, but also deficiencies in one or more aspects, which implies individual scopes of application for each cell source, as summarized in Tables 1 and 2. For example, PHH exhibit liver-like functions, but their use in larger scale screening studies is restricted by their limited availability. In contrast, hepatoma cell lines and pluripotent stem cells are characterized by a high proliferation capacity and abundant availability, while their use is impeded by certain functional aberrations (hepatoma cells) or incomplete maturation (pluripotent stem cells). Thus, the choice of cell source for a specific investigation should take into account the individual characteristics of the cells to address the study requirements. Furthermore, researchers have to consider the physiological requirements of the cells in specific culture models and conditions to optimize the hepatic functionality of the cells and increase the stability of metabolic performances in vitro. In this regard, approaches based on complex 2D and 3D culture technologies are important to improve the predictive value and reliability of hepatic in vitro models in pharmacological research and disease modeling.
Table 1.
Comparison of available hepatic cell sources for in vitro liver cell culture models with respect to their properties and potential application fields
| Cell type | Characteristics |
Application examples | |
|---|---|---|---|
| Advantages | Disadvantages | ||
| Primary human liver cells | • High functionality • Reflect human metabolism • Detection of genetic polymorphisms possible | • Limited availability • Inter-donor variability • Rapid de-differentiation in vitro • No proliferation in vitro | • Toxicity studies51,156 • Investigation of specific human metabolism/metabolic pathways56 • Investigation of complex drug effects or diseases in advanced culture models (e.g. co-culture systems, 3D culture, bioreactors)29,31,45–47,52,53 |
| Hepatoma cell lines | • High proliferation activity • Good availability • Stable metabolic performance | • Alterations in liver specific functions (e.g. reduced activity of drug metabolizing enzymes) | • Studies on tumor biology67 • Testing of anticancer drugs68 • Analysis of specific metabolic/toxicity pathways according to cell line properties69 |
| HepG2 cell line | • Well characterized • Abundant data available | • Differs in metabolic properties from primary human hepatocytes | |
| HepaRG cell line | • Retains many liver-specific functions and many cytochrome P450s • Stable karyotype • Differentiation into both hepatocyte or biliary lineages | • Derived from one donor, does not allow analyzing inter-individual variations | • Studies on human drug metabolism and toxicity (e.g. enzyme induction)70–72,82 |
Table 2.
Comparison of available stem cell sources for hepatic differentiation and subsequent use in in vitro liver cell culture models with respect to their properties and potential application fields
| Cell type | Characteristics |
Application examples | |
|---|---|---|---|
| Advantages | Disadvantages | ||
| Adult stem cells | • Option for patient-specific derivation | • Limited proliferation capacity | • Characterization of differentiation/maturation processes for potential in vitro or clinical use92,94,95,97–99 |
| Liver progenitor cells | • Committed to the hepatic lineage, facilitating differentiation | • Scarce tissue availability • Low frequency in tissue | |
| Mesenchymal stem cells | • Good availability (e.g. from bone marrow, placenta, umbilical cord) | • Incomplete hepatic differentiation with current protocols | |
| Pluripotent stem cells | • Unlimited growth | • Fetal phenotype of differentiated cells with current protocols • Lack of standardized methods for cell differentiation and characterization | • Use in drug metabolism and toxicity studies119,146,147 • Research on applications in regenerative medicine122 |
| hESC | • Differentiation not affected by epigenetic memory | • Ethical considerations restrict research on hESC in dependence of national regulations | |
| hiPSC | • Good availability • No ethical restrictions • Option for derivation from different individuals and patient groups | • Epigenetic memory may impair hepatic differentiation | • Analysis of genetic polymorphisms • Establishment of disease models149–153 • Drug testing with patient-specific cell lines for personalized medicine155 |
Acknowledgements
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work was partly funded by the German Federal Ministry of Education and Research (BMBF) within the Competence Network “Virtual Liver” (FKZ 0315741).
Authors’ contributions
All authors contributed to the design, drafting and revision of the manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Tanimizu N, Mitaka T. Morphogenesis of liver epithelial cells. Hepatol Res. Epub ahead of print 19 January 2016. DOI: 10.1111/hepr.12654. [DOI] [PubMed]
- 2.Han Y, Glaser S, Meng F, Francis H, Marzioni M, McDaniel K, Alvaro D, Venter J, Carpino G, Onori P, Gaudio E, Alpini G, Franchitto A. Recent advances in the morphological and functional heterogeneity of the biliary epithelium. Exp Biol Med (Maywood) 2013; 238: 549–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pfeiffer E, Kegel V, Zeilinger K, Hengstler JG, Nüssler AK, Seehofer D, Damm G. Featured article: isolation, characterization, and cultivation of human hepatocytes and non-parenchymal liver cells. Exp Biol Med (Maywood) 2015; 240: 645–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kleine M, Riemer M, Krech T, DeTemple D, Jäger MD, Lehner F, Manns MP, Klempnauer J, Borlak J, Bektas H, Vondran FW. Explanted diseased livers – a possible source of metabolic competent primary human hepatocytes. PLoS One 2014; 9: e101386–e101386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seglen PO, Reith A. Ammonia inhibition of protein degradation in isolated rat hepatocytes. Quantitative ultrastructural alterations in the lysosomal system. Exp Cell Res 1976; 100: 276–80. [DOI] [PubMed] [Google Scholar]
- 6.Damm G, Pfeiffer E, Burkhardt B, Vermehren J, Nüssler AK, Weiss TS. Human parenchymal and non-parenchymal liver cell isolation, culture and characterization. Hepatol Int 2013; 7: 951–8. [DOI] [PubMed] [Google Scholar]
- 7.Werner M, Driftmann S, Kleinehr K, Kaiser GM, Mathé Z, Treckmann JW, Paul A, Skibbe K, Timm J, Canbay A, Gerken G, Schlaak JF, Broering R. All-in-one: advanced preparation of human parenchymal and non-parenchymal liver cells. PLoS One 2015; 10: e0138655–e0138655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richert L, Alexandre E, Lloyd T, Orr S, Viollon-Abadie C, Patel R, Kingston S, Berry D, Dennison A, Heyd B, Mantion G, Jaeck D. Tissue collection, transport and isolation procedures required to optimize human hepatocyte isolation from waste liver surgical resections. A multilaboratory study. Liver Int 2004; 24: 371–8. [DOI] [PubMed] [Google Scholar]
- 9.Lee SM, Schelcher C, Laubender RP, Fröse N, Thasler RM, Schiergens TS, Mansmann U, Thasler WE. An algorithm that predicts the viability and the yield of human hepatocytes isolated from remnant liver pieces obtained from liver resections. PLoS One 2014; 9: e107567–e107567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kluge M, Reutzel-Selke A, Napierala H, Hillebrandt KH, Major RD, Struecker B, Leder A, Siefert J, Tang P, Lippert S, Sallmon H, Seehofer D, Pratschke J, Sauer IM, Raschzok N. Human hepatocyte isolation: Does portal vein embolization affect the outcome? Tissue Eng Part C Methods 2016; 22: 38–48. [DOI] [PubMed] [Google Scholar]
- 11.Bhogal RH, Hodson J, Bartlett DC, Weston CJ, Curbishley SM, Haughton E, Williams KT, Reynolds GM, Newsome PN, Adams DH, Afford SC. Isolation of primary human hepatocytes from normal and diseased liver tissue: a one hundred liver experience. PLoS One 2011; 6: e18222–e18222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godoy P, Hewitt NJ, Albrecht U, Andersen ME, Ansari N, Bhattacharya S, Bode JG, Bolleyn J, Borner C, Böttger J, Braeuning A, Budinsky RA, Burkhardt B, Cameron NR, Camussi G, Cho CS, Choi YJ, Craig Rowlands J, Dahmen U, Damm G, Dirsch O, Donato MT, Dong J, Dooley S, Drasdo D, Eakins R, Ferreira KS, Fonsato V, Fraczek J, Gebhardt R, Gibson A, Glanemann M, Goldring CE, Gómez-Lechón MJ, Groothuis GM, Gustavsson L, Guyot C, Hallifax D, Hammad S, Hayward A, Häussinger D, Hellerbrand C, Hewitt P, Hoehme S, Holzhütter HG, Houston JB, Hrach J, Ito K, Jaeschke H, Keitel V, Kelm JM, Kevin Park B, Kordes C, Kullak-Ublick GA, LeCluyse EL, Lu P, Luebke-Wheeler J, Lutz A, Maltman DJ, Matz-Soja M, McMullen P, Merfort I, Messner S, Meyer C, Mwinyi J, Naisbitt DJ, Nussler AK, Olinga P, Pampaloni F, Pi J, Pluta L, Przyborski SA, Ramachandran A, Rogiers V, Rowe C, Schelcher C, Schmich K, Schwarz M, Singh B, Stelzer EH, Stieger B, Stöber R, Sugiyama Y, Tetta C, Thasler WE, Vanhaecke T, Vinken M, Weiss TS, Widera A, Woods CG, Xu JJ, Yarborough KM, Hengstler JG. Recent advances in 2D and 3D in vitro systems using primary hepatocytes, alternative hepatocyte sources and non-parenchymal liver cells and their use in investigating mechanisms of hepatotoxicity, cell signaling and ADME. Arch Toxicol 2013; 87: 1315–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aghdai MH, Jamshidzadeh A, Nematizadeh M, Behzadiannia M, Niknahad H, Amirghofran Z, Esfandiari E, Azarpira N. Evaluating the effects of dithiothreitol and fructose on cell viability and function of cryopreserved primary rat hepatocytes and HepG2 cell line. Hepat Mon 2013; 13: e7824–e7824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solanas E, Sostres C, Serrablo A, García-Gil A, Aranguren F, Jimenez P, Serrano MT. Incubation with dimethyl sulfoxide prior to cryopreservation improves functionality of thawed human primary hepatocytes. Biopreserv Biobank 2012; 10: 446–53. [DOI] [PubMed] [Google Scholar]
- 15.Hang H, Shi X, Gu G, Wu Y, Ding Y. A simple isolation and cryopreservation method for adult human hepatocytes. Int J Artif Organs 2009; 32: 720–7. [DOI] [PubMed] [Google Scholar]
- 16.Saliem M, Holm F, Tengzelius RB, Jorns C, Nilsson LM, Ericzon BG, Ellis E, Hovatta O. Improved cryopreservation of human hepatocytes using a new xeno free cryoprotectant solution. World J Hepatol 2012; 4: 176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walbrun P, Hellerbrand C, Weiss TS, Netter S, Neumaier D, Gaebele E, Wiest R, Schoelmerich J, Froh M. Characterization of rat and human Kupffer cells after cryopreservation. Cryobiology 2007; 54: 164–72. [DOI] [PubMed] [Google Scholar]
- 18.Neyzen S, Van de Leur E, Borkham-Kamphorst E, Herrmann J, Hollweg G, Gressner AM, Weiskirchen R. Cryopreservation of hepatic stellate cells. J Hepatol 2006; 44: 910–7. [DOI] [PubMed] [Google Scholar]
- 19.Nakamura A, Ueno T, Yagi Y, Okuda K, Ogata T, Nakamura T, Torimura T, Iwamoto H, Ramadoss S, Sata M, Tsutsumi V, Yasuda K, Tomiyasu Y, Obayashi K, Tashiro K, Kuhara S. Human primary cultured hepatic stellate cells can be cryopreserved. Med Mol Morphol 2010; 43: 107–15. [DOI] [PubMed] [Google Scholar]
- 20.Bogoslovsky T, Wang D, Maric D, Scattergood-Keepper L, Spatz M, Auh S, Hallenbeck J. Cryopreservation and enumeration of human endothelial progenitor and endothelial cells for clinical trials. J Blood Disord Transfus 2013; 4: 158–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polchow B, Kebbel K, Schmiedeknecht G, Reichardt A, Henrich W, Hetzer R, Lueders C. Cryopreservation of human vascular umbilical cord cells under good manufacturing practice conditions for future cell banks. J Transl Med 2012; 10: 98–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Treyer A, Müsch A. Hepatocyte polarity. Compr Physiol 2013; 3: 243–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tormos AM, Taléns-Visconti R, Bonora-Centelles A, Pérez S, Sastre J. Oxidative stress triggers cytokinesis failure in hepatocytes upon isolation. Free Radic Res 2015; 49: 927–34. [DOI] [PubMed] [Google Scholar]
- 24.Ramboer E, Vanhaecke T, Rogiers V, Vinken M. Primary hepatocyte cultures as prominent in vitro tools to study hepatic drug transporters. Drug Metab Rev 2013; 45: 196–217. [DOI] [PubMed] [Google Scholar]
- 25.Elaut G, Henkens T, Papeleu P, Snykers S, Vinken M, Vanhaecke T, Rogiers V. Molecular mechanisms underlying the dedifferentiation process of isolated hepatocytes and their cultures. Curr Drug Metab 2006; 7: 629–60. [DOI] [PubMed] [Google Scholar]
- 26.Jiang J, Wolters JE, van Breda SG, Kleinjans JC, de Kok TM. Development of novel tools for the in vitro investigation of drug-induced liver injury. Expert Opin Drug Metab Toxicol 2015; 11: 1523–37. [DOI] [PubMed] [Google Scholar]
- 27.Smith CM, Nolan CK, Edwards MA, Hatfield JB, Stewart TW, Ferguson SS, Lecluyse EL, Sahi J. A comprehensive evaluation of metabolic activity and intrinsic clearance in suspensions and monolayer cultures of cryopreserved primary human hepatocytes. J Pharm Sci 2012; 101: 3989–4002. [DOI] [PubMed] [Google Scholar]
- 28.Le Vee M, Jouan E, Noel G, Stieger B, Fardel O. Polarized location of SLC and ABC drug transporters in monolayer-cultured human hepatocytes. Toxicol In Vitro 2015; 29: 938–46. [DOI] [PubMed] [Google Scholar]
- 29.Schyschka L, Sánchez JJ, Wang Z, Burkhardt B, Müller-Vieira U, Zeilinger K, Bachmann A, Nadalin S, Damm G, Nussler AK. Hepatic 3D cultures but not 2D cultures preserve specific transporter activity for acetaminophen-induced hepatotoxicity. Arch Toxicol 2013; 87: 1581–93. [DOI] [PubMed] [Google Scholar]
- 30.Knobeloch D, Ehnert S, Schyschka L, Büchler P, Schoenberg M, Kleeff J, Thasler WE, Nussler NC, Godoy P, Hengstler J, Nussler AK. Human hepatocytes: isolation, culture, and quality procedures. Methods Mol Biol 2012; 806: 99–120. [DOI] [PubMed] [Google Scholar]
- 31.De Bruyn T, Chatterjee S, Fattah S, Keemink J, Nicolaï J, Augustijns P, Annaert P. Sandwich-cultured hepatocytes: utility for in vitro exploration of hepatobiliary drug disposition and drug-induced hepatotoxicity. Expert Opin Drug Metab Toxicol 2013; 9: 589–616. [DOI] [PubMed] [Google Scholar]
- 32.Hamilton GA, Jolley SL, Gilbert D, Coon DJ, Barros S, LeCluyse EL. Regulation of cell morphology and cytochrome P450 expression in human hepatocytes by extracellular matrix and cell-cell interactions. Cell Tissue Res 2001; 306: 85–99. [DOI] [PubMed] [Google Scholar]
- 33.Moghe PV, Berthiaume F, Ezzell RM, Toner M, Tompkins RG, Yarmush ML. Culture matrix configuration and composition in the maintenance of hepatocyte polarity and function. Biomaterials 1996; 17: 373–85. [DOI] [PubMed] [Google Scholar]
- 34.Kim Y, Lasher CD, Milford LM, Murali TM, Rajagopalan P. A comparative study of genome-wide transcriptional profiles of primary hepatocytes in collagen sandwich and monolayer cultures. Tissue Eng Part C Methods 2010; 16: 1449–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Page JL, Johnson MC, Olsavsky KM, Strom SC, Zarbl H, Omiecinski CJ. Gene expression profiling of extracellular matrix as an effector of human hepatocyte phenotype in primary cell culture. Toxicol Sci 2007; 97: 384–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deegan DB, Zimmerman C, Skardal A, Atala A, Shupe TD. Stiffness of hyaluronic acid gels containing liver extracellular matrix supports human hepatocyte function and alters cell morphology. J Mech Behav Biomed Mater 2015; 55: 87–103. [DOI] [PubMed] [Google Scholar]
- 37.Messner S, Agarkova I, Moritz W, Kelm JM. Multi-cell type human liver microtissues for hepatotoxicity testing. Arch Toxicol 2013; 87: 209–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bell CC, Hendriks DF, Moro SM, Ellis E, Walsh J, Renblom A, Fredriksson, Puigvert L, Dankers AC, Jacobs F, Snoeys J, Sison-Young RL, Jenkins RE, Nordling Å, Mkrtchian S, Park BK, Kitteringham NR, Goldring CE, Lauschke VM, Ingelman-Sundberg M. Characterization of primary human hepatocyte spheroids as a model system for drug-induced liver injury, liver function and disease. Sci Rep 2016; 6: 25187–25187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ohkura T, Ohta K, Nagao T, Kusumoto K, Koeda A, Ueda T, Jomura T, Ikeya T, Ozeki E, Wada K, Naitoh K, Inoue Y, Takahashi N, Iwai H, Arakawa H, Ogihara T. Evaluation of human hepatocytes cultured by three-dimensional spheroid systems for drug metabolism. Drug Metab Pharmacokinet 2014; 29: 373–8. [DOI] [PubMed] [Google Scholar]
- 40.Gevaert E, Dollé L, Billiet T, Dubruel P, van Grunsven L, van Apeldoorn A, Cornelissen R. High throughput micro-well generation of hepatocyte micro-aggregates for tissue engineering. PLoS One 2014; 9: e105171–e105171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Du Y, Lo E, Ali S, Khademhosseini A. Directed assembly of cell-laden microgels for fabrication of 3D tissue constructs. Proc Natl Acad Sci USA 2008; 105: 9522–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhise NS, Manoharan V, Massa S, Tamayol A, Ghaderi M, Miscuglio M, Lang Q, Shrike Zhang Y, Shin SR, Calzone G, Annabi N, Shupe TD, Bishop CE, Atala A, Dokmeci MR, Khademhosseini A. A liver-on-a-chip platform with bioprinted hepatic spheroids. Biofabrication 2016; 8: 014101–014101. [DOI] [PubMed] [Google Scholar]
- 43.Skardal A, Devarasetty M, Kang HW, Seol YJ, Forsythe SD, Bishop C, Shupe T, Soker S, Atala A. Bioprinting cellularized constructs using a tissue-specific hydrogel bioink. J Vis Exp 2016; 110: e53606–e53606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhatia SN, Balis UJ, Yarmush ML, Toner M. Effect of cell-cell interactions in preservation of cellular phenotype: cocultivation of hepatocytes and nonparenchymal cells. FASEB J 1999; 13: 1883–900. [DOI] [PubMed] [Google Scholar]
- 45.Nguyen TV, Ukairo O, Khetani SR, McVay M, Kanchagar C, Seghezzi W, Ayanoglu G, Irrechukwu O, Evers R. Establishment of a hepatocyte-Kupffer cell coculture model for assessment of proinflammatory cytokine effects on metabolizing enzymes and drug transporters. Drug Metab Dispos 2015; 43: 774–85. [DOI] [PubMed] [Google Scholar]
- 46.Wu R, Cui X, Dong W, Zhou M, Simms HH, Wang P. Suppression of hepatocyte CYP1A2 expression by Kupffer cells via AhR pathway: the central role of proinflammatory cytokines. Int J Mol Med 2006; 18: 339–46. [PubMed] [Google Scholar]
- 47.Giraudi PJ, Becerra VJ, Marin V, Chavez-Tapia NC, Tiribelli C, Rosso N. The importance of the interaction between hepatocyte and hepatic stellate cells in fibrogenesis induced by fatty accumulation. Exp Mol Pathol 2015; 98: 85–92. [DOI] [PubMed] [Google Scholar]
- 48.Salerno S, Campana C, Morelli S, Drioli E, De Bartolo L. Human hepatocytes and endothelial cells in organotypic membrane systems. Biomaterials 2011; 32: 8848–59. [DOI] [PubMed] [Google Scholar]
- 49.March S, Ramanan V, Trehan K, Ng S, Galstian A, Gural N, Scull MA, Shlomai A, Mota MM, Fleming HE, Khetani SR, Rice CM, Bhatia SN. Micropatterned coculture of primary human hepatocytes and supportive cells for the study of hepatotropic pathogens. Nat Protoc 2015; 10: 2027–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trask OJ, Jr, Moore A, LeCluyse EL. A micropatterned hepatocyte coculture model for assessment of liver toxicity using high-content imaging analysis. Assay Drug Dev Technol 2014; 12: 16–27. [DOI] [PubMed] [Google Scholar]
- 51.Khetani SR, Kanchagar C, Ukairo O, Krzyzewski S, Moore A, Shi J, Aoyama S, Aleo M, Will Y. Use of micropatterned cocultures to detect compounds that cause drug-induced liver injury in humans. Toxicol Sci 2013; 132: 107–17. [DOI] [PubMed] [Google Scholar]
- 52.Kegel V, Pfeiffer E, Burkhardt B, Liu JL, Zeilinger K, Nüssler AK, Seehofer D, Damm G. Subtoxic concentrations of hepatotoxic drugs lead to Kupffer cell activation in a human in vitro liver model: an approach to study DILI. Mediators Inflamm 2015;2015:640631. [DOI] [PMC free article] [PubMed]
- 53.Kostadinova R, Boess F, Applegate D, Suter L, Weiser T, Singer T, Naughton B, Roth A. A long-term three dimensional liver co-culture system for improved prediction of clinically relevant drug-induced hepatotoxicity. Toxicol Appl Pharmacol 2013; 268: 1–16. [DOI] [PubMed] [Google Scholar]
- 54.Rennert K, Steinborn S, Gröger M, Ungerböck B, Jank AM, Ehgartner J, Nietzsche S, Dinger J, Kiehntopf M, Funke H, Peters FT, Lupp A, Gärtner C, Mayr T, Bauer M, Huber O, Mosig AS. A microfluidically perfused three dimensional human liver model. Biomaterials 2015; 71: 119–31. [DOI] [PubMed] [Google Scholar]
- 55.Vivares A, Salle-Lefort S, Arabeyre-Fabre C, Ngo R, Penarier G, Bremond M, Moliner P, Gallas JF, Fabre G, Klieber S. Morphological behaviour and metabolic capacity of cryopreserved human primary hepatocytes cultivated in a perfused multiwell device. Xenobiotica 2015; 45: 29–44. [DOI] [PubMed] [Google Scholar]
- 56.Bricks T, Hamon J, Fleury MJ, Jellali R, Merlier F, Herpe YE, Seyer A, Regimbeau JM, Bois F, Leclerc E. Investigation of omeprazole and phenacetin first-pass metabolism in humans using a microscale bioreactor and pharmacokinetic models. Biopharm Drug Dispos 2015; 36: 275–93. [DOI] [PubMed] [Google Scholar]
- 57.Hegde M, Jindal R, Bhushan A, Bale SS, McCarty WJ, Golberg I, Usta OB, Yarmush ML. Dynamic interplay of flow and collagen stabilizes primary hepatocytes culture in a microfluidic platform. Lab Chip 2014; 14: 2033–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uzarski JS, Bijonowski BM, Wang B, Ward HH, Wandinger-Ness A, Miller WM, Wertheim JA. Dual-purpose bioreactors to monitor noninvasive physical and biochemical markers of kidney and liver scaffold recellularization. Tissue Eng Part C Methods 2015; 21: 1032–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gao R, Wu W, Xiang J, Lv Y, Zheng X, Chen Q, Wang H, Wang B, Liu Z, Ma F. Hepatocyte culture in autologous decellularized spleen matrix. Organogenesis 2015; 11: 16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmelzer E, Mutig K, Schrade P, Bachmann S, Gerlach JC, Zeilinger K. Effect of human patient plasma ex vivo treatment on gene expression and progenitor cell activation of primary human liver cells in multi-compartment 3D perfusion bioreactors for extra-corporeal liver support. Biotech Bioeng 2009; 03: 817–27. [DOI] [PubMed] [Google Scholar]
- 61.Gerlach JC, Mutig K, Sauer IM, Schrade P, Efimova E, Mieder T, Naumann G, Grunwald A, Pless G, Mas A, Bachmann S, Neuhaus P, Zeilinger K. Use of primary human liver cells originating from discarded grafts in a bioreactor for liver support therapy and the prospects of culturing adult liver stem cells in bioreactors: a morphologic study. Transplantation 2003; 76: 781–86. [DOI] [PubMed] [Google Scholar]
- 62.Zeilinger K, Holland G, Sauer IM, Efimova E, Kardassis D, Obermayer N, Liu M, Neuhaus P, Gerlach JC. Time course of primary liver cell reorganization in three-dimensional high-density bioreactors for extracorporeal liver support: an immunohistochemical and ultrastructural study. Tissue Eng 2004; 10: 1113–24. [DOI] [PubMed] [Google Scholar]
- 63.Zeilinger K, Schreiter T, Darnell M, Söderdahl T, Lübberstedt M, Dillner B, Knobeloch D, Nüssler AK, Gerlach JC, Andersson T. Scaling down of a clinical 3D perfusion multi-compartment hollow fiber liver bioreactor developed for extracorporeal liver support to an analytical scale device useful for hepatic pharmacological in vitro studies. Tissue Eng Part C Methods 2011; 17: 549–56. [DOI] [PubMed] [Google Scholar]
- 64.Mueller D, Tascher G, Müller-Vieira U, Knobeloch D, Nuessler AK, Zeilinger K, Heinzle E, Noor F. In-depth physiological characterization of primary human hepatocytes in a 3D hollow-fiber bioreactor. J Tissue Eng Regen Med 2011; 5: e207–18. [DOI] [PubMed] [Google Scholar]
- 65.Lübberstedt M, Müller-Vieira U, Biemel KM, Darnell M, Hoffmann SA, Knöspel F, Wönne EC, Knobeloch D, Nüssler AK, Gerlach JC, Andersson TB, Zeilinger K. Serum-free culture of primary human hepatocytes in a miniaturized hollow-fiber membrane bioreactor for pharmacological in vitro studies. J Tissue Eng Regen Med 2015; 9: 1017–26. [DOI] [PubMed] [Google Scholar]
- 66.Hoffmann SA, Müller-Vieira U, Biemel K, Knobeloch D, Heydel S, Lübberstedt M, Nüssler AK, Andersson TB, Gerlach JC, Zeilinger K. Analysis of drug metabolism activities in a miniaturized liver cell bioreactor for use in pharmacological studies. Biotech Bioeng 2012; 109: 3172–81. [DOI] [PubMed] [Google Scholar]
- 67.Samatiwat P, Takeda K, Satarug S, Ohba K, Kukongviriyapan V, Shibahara S. Induction of MITF expression in human cholangiocarcinoma cells and hepatocellular carcinoma cells by cyclopamine, an inhibitor of the Hedgehog signaling. Biochem Biophys Res Commun 2016; 470: 144–9. [DOI] [PubMed] [Google Scholar]
- 68.Lv H, Zhang Z, Wu X, Wang Y, Li C, Gong W, Gui L, Wang X. Preclinical evaluation of liposomal C8 ceramide as a potent anti-hepatocellular carcinoma agent. PLoS One 2016; 11: e0145195–e0145195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Palabiyik SS, Karakus E, Halici Z, Cadirci E, Bayir Y, Ayaz G, Cinar I. The protective effects of carvacrol and thymol against paracetamol-induced toxicity on human hepatocellular carcinoma cell lines (HepG2). Hum Exp Toxicol. Epub ahead of print 22 January 2016. DOI: 0960327115627688. [DOI] [PubMed]
- 70.Guillouzo A, Corlu A, Aninat C, Glaise D, Morel F, Guguen-Guillouzo C. The human hepatoma HepaRG cells: a highly differentiated model for studies of liver metabolism and toxicity of xenobiotics. Chem Biol Interact 2007; 168: 66–73. [DOI] [PubMed] [Google Scholar]
- 71.Lübberstedt M, Müller-Vieira U, Mayer M, Biemel KM, Knöspel F, Knobeloch D, Nüssler AK, Gerlach JC, Zeilinger K. HepaRG human hepatic cell line utility as a surrogate for primary human hepatocytes in drug metabolism assessment in vitro. J Pharmacol Toxicol Methods 2011; 63: 59–68. [DOI] [PubMed] [Google Scholar]
- 72.Andersson TB, Kanebratt KP, Kenna JG. The HepaRG cell line: a unique in vitro tool for understanding drug metabolism and toxicology in human. Expert Opin Drug Metab Toxicol 2012; 8: 909–20. [DOI] [PubMed] [Google Scholar]
- 73.Rodrigues RM, Heymans A, De Boe V, Sachinidis A, Chaudhari U, Govaere O, Roskams T, Vanhaecke T, Rogiers V, De Kock J. Toxicogenomics-based prediction of acetaminophen-induced liver injury using human hepatic cell systems. Toxicol Lett 2016; 240: 50–9. [DOI] [PubMed] [Google Scholar]
- 74.Gerets HH, Tilmant K, Gerin B, Chanteux H, Depelchin BO, Dhalluin S, Atienzar FA. Characterization of primary human hepatocytes, HepG2 cells, and HepaRG cells at the mRNA level and CYP activity in response to inducers and their predictivity for the detection of human hepatotoxins. Cell Biol Toxicol 2012; 28: 69–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sjogren AK, Liljevald M, Glinghammar B, Sagemark J, Li XQ, Jonebring A, Cotgreave I, Brolén G, Andersson TB. Critical differences in toxicity mechanisms in induced pluripotent stem cell-derived hepatocytes, hepatic cell lines and primary hepatocytes. Arch Toxicol 2014; 88: 1427–37. [DOI] [PubMed] [Google Scholar]
- 76.Liu H, You S, Rong Y, Wu Y, Zhu B, Wan Z, Liu W, Mao P, Xin S. Newly established human liver cell line: a potential cell source for the bioartificial liver in the future. Hum Cell 2013; 26: 155–61. [DOI] [PubMed] [Google Scholar]
- 77.Novotna A, Doricakova A, Vrzal R, Pavek P, Dvorak Z. Construction and characterization of hepatocyte nuclear factor HNF4alpha1 over-expressing cell line derived from human hepatoma HepG2 cells. Eur J Pharmacol 2011; 669: 45–50. [DOI] [PubMed] [Google Scholar]
- 78.Xuan J, Chen S, Ning B, Tolleson WH, Guo L. Development of HepG2-derived cells expressing cytochrome P450s for assessing metabolism-associated drug-induced liver toxicity. Chem Biol Interact. Epub ahead of print 22 October 2015. DOI: S0009-2797(15)30088-0. [DOI] [PMC free article] [PubMed]
- 79.Ramboer E, De Craene B, De Kock J, Berx G, Rogiers V, Vanhaecke T, Vinken M. Development and characterization of a new human hepatic cell line. EXCLI J 2015; 14: 875–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dubiak-Szepietowska M, Karczmarczyk A, Jönsson-Niedziółka M, Winckler T, Feller KH. Development of complex-shaped liver multicellular spheroids as a human-based model for nanoparticle toxicity assessment in vitro. Toxicol Appl Pharmacol 2016; 294: 78–85. [DOI] [PubMed] [Google Scholar]
- 81.Rebelo SP, Costa R, Estrada M, Shevchenko V, Brito C, Alves PM. HepaRG microencapsulated spheroids in DMSO-free culture: novel culturing approaches for enhanced xenobiotic and biosynthetic metabolism. Arch Toxicol 2014; 89: 1347–58. [DOI] [PubMed] [Google Scholar]
- 82.Darnell M, Schreiter T, Zeilinger K, Urbaniak T, Söderdahl T, Rossberg I, Dillnér B, Berg AL, Gerlach JC, Andersson TB. Cytochrome P450-dependent metabolism in HepaRG cells cultured in a dynamic three-dimensional bioreactor. Drug Metab Dispos 2011; 39: 1131–8. [DOI] [PubMed] [Google Scholar]
- 83.Theise ND, Saxena R, Portmann BC, Thung SN, Yee H, Chiriboga L, Kumar A, Crawford JM. The canals of Hering and hepatic stem cells in humans. Hepatology 1999; 30: 1425–33. [DOI] [PubMed] [Google Scholar]
- 84.Mitaka T, Mizuguchi T, Sato F, Mochizuki C, Mochizuki Y. Reconstruction of hepatic organoid by rat small hepatocytes and hepatic nonparenchymal cells. Hepatology 1999; 29: 111–25. [DOI] [PubMed] [Google Scholar]
- 85.Tan J, Hytiroglou P, Wieczorek R, Park YN, Thung SN, Arias B, Theise ND. Immunohistochemical evidence for hepatic progenitor cells in liver diseases. Liver 2002; 22: 365–73. [DOI] [PubMed] [Google Scholar]
- 86.Quante M, Wang TC. Stem cells in gastroenterology and hepatology. Nat Rev Gastroenterol Hepatol 2009; 6: 724–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schmelzer E, Wauthier E, Reid LM. The phenotypes of pluripotent human hepatic progenitors. Stem cells 2006; 24: 1852–58. [DOI] [PubMed] [Google Scholar]
- 88.Schmelzer E, Zhang L, Bruce A, Wauthier E, Ludlow J, Yao H, Moss N, Melhem A, McClelland R, Turner WS, Kulik M, Sherwood S, Tallheden T, Cheng N, Furth ME, Reid LM. Human hepatic stem cells from fetal and postnatal donors. J Exp Med 2007; 204: 1973–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stachelscheid H, Urbaniak T, Ring A, Spengler B, Gerlach JC, Zeilinger K. Isolation and characterization of adult human liver progenitors from ischemic liver tissue derived from therapeutic hepatectomies. Tissue Eng Part A 2009; 15: 1633–43. [DOI] [PubMed] [Google Scholar]
- 90.Sakai Y, Jiang J, Kojima N, Kinoshita T, Miyajima A. Enhanced in vitro maturation of fetal mouse liver cells with oncostatin M, nicotinamide and dimethylsulfoxide. Cell Transplant 2002; 11: 435–41. [PubMed] [Google Scholar]
- 91.Kinoshita T, Sekiguchi T, Xu MJ, Ito Y, Kamiya A, Tsuji K, Nakamura T. Hepatic differentiation induced by oncostatin M attenuates fetal liver hematopoiesis. Proc Natl Sci USA 1999; 96: 7265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schwartz RE, Reyes M, Koodie L, Jiang Y, Blackstad M, Lund T, Lenvik T, Johnson S, Hu WS, Verfaillie CM. Multipotent adult progenitor cells from bone marrow differentiate into functional hepatocyte-like cells. J Clin Invest 2002; 109: 1291–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Okura H, Komoda H, Saga A, Kakuta-Yamamoto A, Hamada Y, Fumimoto Y, Lee CM, Ichinose A, Sawa Y, Matsuyama A. Properties of hepatocyte-like cell clusters from human adipose tissue derived mesenchymal stem cells. Tissue Eng Part C Methods 2010; 16: 761–70. [DOI] [PubMed] [Google Scholar]
- 94.Campard D, Lysy PA, Najimi M, Sokal EM. Native umbilical cord matrix stem cells express hepatic markers and differentiate into hepatocyte-like cells. Gastroenterology 2008; 134: 833–48. [DOI] [PubMed] [Google Scholar]
- 95.Snykers S, De Kock J, Tamara V, Rogiers V. Hepatic differentiation of mesenchymal stem cells: in vitro strategies. Methods Mol Biol 2011; 698: 305–14. [DOI] [PubMed] [Google Scholar]
- 96.Buyl K, De Kock J, Najar M, Lagneaux L, Branson S, Rogiers V, Vanhaecke T. Characterization of hepatic markers in human Wharton's Jelly-derived mesenchymal stem cells. Toxicol In Vitro 2014; 28: 113–9. [DOI] [PubMed] [Google Scholar]
- 97.Talaei-Khozani T, Borhani-Haghighi M, Ayatollahi M, Vojdani Z. An in vitro model for hepatocyte-like cell differentiation from Wharton's jelly derived-mesenchymal stem cells by cell-base aggregates. Chem Biol Drug Des 2016; 87: 296–305. [PMC free article] [PubMed] [Google Scholar]
- 98.Teng NY, Liu YS, Wu HH, Liu YA, Ho JH, Lee OK. Promotion of mesenchymal-to-epithelial transition by Rac1 inhibition with small molecules accelerates hepatic differentiation of mesenchymal stromal cells. Tissue Eng Part A 2015; 21: 1444–54. [DOI] [PubMed] [Google Scholar]
- 99.Fairhall EA, Charles MA, Wallace K, Schwab CJ, Harrison CJ, Richter M, Hoffmann SA, Charlton KA, Zeilinger K, Wright MC. The B-13 hepatocyte progenitor cell resists pluripotency induction and differentiation to non-hepatocyte cells. Toxicol Res 2013; 2: 308–20. [Google Scholar]
- 100.Wallace K, Fairhall EA, Charlton KA, Wright MC. AR42J-B-13 cell: an expandable progenitor to generate an unlimited supply of functional hepatocytes. Toxicology 2010; 278: 277–87. [DOI] [PubMed] [Google Scholar]
- 101.Richter M, Fairhall EA, Hoffmann SA, Tröbs S, Knöspel F, Probert PME, Oakley F, Stroux A, Wright MC, Zeilinger K. Pancreatic progenitor-derived hepatocytes are viable and functional in a 3D high density bioreactor culture system. Toxicol Res 2016; 5: 278–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fairhall EA, Wallace K, White SA, Huang GC, Shaw JA, Wright SC, Charlton KA, Burt AD, Wright MC. Adult human exocrine pancreas differentiation to hepatocytes – potential source of a human hepatocyte progenitor for use in toxicology research. Toxicol Res 2013; 2: 80–87. [Google Scholar]
- 103.Zuba-Surma EK, Józkowicz A, Dulak J. Stem cells in pharmaceutical biotechnology. Curr Pharm Biotechnol 2011; 12: 1760–73. [DOI] [PubMed] [Google Scholar]
- 104.Thomson J, Itskovitz-Eldor J, Shapiro S, Waknitz M, Swiergiel J, Marshall V, Jones J. Embryonic stem cell lines derived from human blastocysts. Science 1998; 282: 1145–47. [DOI] [PubMed] [Google Scholar]
- 105.Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 2007; 131: 861–72. [DOI] [PubMed] [Google Scholar]
- 106.Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA, Ruotti V, Stewart R, Slukvin II, Thomson JA. Induced pluripotent stem cell lines derived from human somatic cells. Science 2007; 318: 1917–20. [DOI] [PubMed] [Google Scholar]
- 107.Cameron K, Tan R, Schmidt-Heck W, Campos G, Lyall MJ, Wang Y, Lucendo-Villarin B, Szkolnicka D, Bates N, Kimber SJ, Hengstler JG, Godoy P, Forbes SJ, Hay DC. Recombinant laminins drive the differentiation and self-organization of hESC-derived hepatocytes. Stem Cell Reports 2015; 5: 1250–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hay DC, Fletcher J, Payne C, Terrace JD, Gallagher RC, Snoeys J, Black JR, Wojtacha D, Samuel K, Hannoun Z. Highly efficient differentiation of hESCs to functional hepatic endoderm requires Activin A and Wnt3a signaling. Proc. Natl. Acad. Sci. USA 2008; 105: 12301–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hannan NR, Segeritz CP, Touboul T, Vallier L. Production of hepatocyte-like cells from human pluripotent stem cells. Nat Protoc 2013; 8: 430–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Touboul T, Hannan NR, Corbineau S, Martinez A, Martinet C, Branchereau S, Mainot S, Strick-Marchand H, Pedersen R, Di Santo J, Weber A, Vallier L. Generation of functional hepatocytes from human embryonic stem cells under chemically defined conditions that recapitulate liver development. Hepatology 2010; 51: 1754–65. [DOI] [PubMed] [Google Scholar]
- 111.Cai J, DeLaForest A, Fisher J, Urick A, Wagner T, Twaroski K, Cayo M, Nagaoka M, Duncan SA. Protocol for directed differentiation of human pluripotent stem cells toward a hepatocyte fate. StemBook [Internet]. Cambridge, MA: Harvard Stem Cell Institute, 2012. [PubMed]
- 112.Czysz K, Minger S, Thomas N. DMSO efficiently down regulates pluripotency genes in human embryonic stem cells during definitive endoderm derivation and increases the proficiency of hepatic differentiation. PLoS One 2015; 10: e0117689–e0117689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Baxter M, Withey S, Harrison S, Segeritz CP, Zhang F, Atkinson-Dell R, Rowe C, Gerrard DT, Sison-Young R, Jenkins R, Henry J, Berry AA, Mohamet L, Best M, Fenwick SW, Malik H, Kitteringham NR, Goldring CE, Piper Hanley K, Vallier L, Hanley NA. Phenotypic and functional analyses show stem cell-derived hepatocyte-like cells better mimic fetal rather than adult hepatocytes. J Hepatol 2015; 62: 581–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Godoy P, Schmidt-Heck W, Natarajan K, Lucendo-Villarin B, Szkolnicka D, Asplund A, Björquist P, Widera A, Stöber R, Campos G, Hammad S, Sachinidis A, Chaudhari U, Damm G, Weiss TS, Nüssler A, Synnergren J, Edlund K, Küppers-Munther B, Hay DC, Hengstler JG. Gene networks and transcription factor motifs defining the differentiation of stem cells into hepatocyte-like cells. J Hepatol 2015; 63: 934–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Vinken M, Papeleu P, Snykers S, De Rop E, Henkens T, Chipman JK, Rogiers V, Vanhaecke T. Involvement of cell junctions in hepatocyte culture functionality. Crit Rev Toxicol 2006; 36: 299–318. [DOI] [PubMed] [Google Scholar]
- 116.Gieseck RL, 3rd, Hannan NR, Bort R, Hanley NA, Drake RA, Cameron GW, Wynn TA, Vallier L. Maturation of induced pluripotent stem cell derived hepatocytes by 3D-culture. PLoS One 2014; 9: e86372–e86372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ramasamy TS, Yu JS, Selden C, Hodgson H, Cui W. Application of three-dimensional culture conditions to human embryonic stem cell-derived definitive endoderm cells enhances hepatocyte differentiation and functionality. Tissue Eng Part A 2013; 19: 360–7. [DOI] [PubMed] [Google Scholar]
- 118.Yao R, Wang J, Li X, Jung Jung D, Qi H, Kee KK, Du Y. Hepatic differentiation of human embryonic stem cells as microscaled multilayered colonies leading to enhanced homogeneity and maturation. Small 2014; 10: 4311–23. [DOI] [PubMed] [Google Scholar]
- 119.Takayama K, Kawabata K, Nagamoto Y, Kishimoto K, Tashiro K, Sakurai F, Tachibana M, Kanda K, Hayakawa T, Furue MK, Mizuguchi H. 3D spheroid culture of hESC/hiPSC-derived hepatocyte-like cells for drug toxicity testing. Biomaterials 2013; 34: 1781–9. [DOI] [PubMed] [Google Scholar]
- 120.Sivertsson L, Synnergren J, Jensen J, Björquist P, Ingelman-Sundberg M. Hepatic differentiation and maturation of human embryonic stem cells cultured in a perfused three-dimensional bioreactor. Stem Cells Dev 2013; 22: 581–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Miki T, Ring A, Gerlach J. Hepatic differentiation of human embryonic stem cells is promoted by three-dimensional dynamic perfusion culture conditions. Tissue Eng Part C Methods 2011; 17: 557–68. [DOI] [PubMed] [Google Scholar]
- 122.Takebe T, Sekine K, Enomura M, Koike H, Kimura M, Ogaeri T, Zhang RR, Ueno Y, Zheng YW, Koike N, Aoyama S, Adachi Y, Taniguchi H. Vascularized and functional human liver from an iPSC-derived organ bud transplant. Nature 2013; 499: 481–4. [DOI] [PubMed] [Google Scholar]
- 123.Berger DR, Ware BR, Davidson MD, Allsup SR, Khetani SR. Enhancing the functional maturity of induced pluripotent stem cell-derived human hepatocytes by controlled presentation of cell-cell interactions in vitro. Hepatology 2015; 61: 1370–81. [DOI] [PubMed] [Google Scholar]
- 124.Nagamoto Y, Tashiro K, Takayama K, Ohashi K, Kawabata K, Sakurai F, Tachibana M, Hayakawa T, Furue MK, Mizuguchi H. The promotion of hepatic maturation of human pluripotent stem cells in 3D co-culture using type I collagen and Swiss 3T3 cell sheets. Biomaterials 2012; 33: 4526–34. [DOI] [PubMed] [Google Scholar]
- 125.Yu YD, Kim KH, Lee SG, Choi SY, Kim YC, Byun KS, Cha IH, Park KY, Cho CH, Choi DH. Hepatic differentiation from human embryonic stem cells using stromal cells. J Surg Res 2011; 170: e253–61. [DOI] [PubMed] [Google Scholar]
- 126.Javed MS, Yaqoob N, Iwamuro M, Kobayashi N, Fujiwara T. Generation of hepatocyte-like cells from human induced pluripotent stem (iPS) cells by co-culturing embryoid body cells with liver non-parenchymal cell line TWNT-1. J Coll Physicians Surg Pak 2014; 24: 91–6. [PubMed] [Google Scholar]
- 127.Du C, Narayanan K, Leong MF, Wan AC. Induced pluripotent stem cell-derived hepatocytes and endothelial cells in multi-component hydrogel fibers for liver tissue engineering. Biomaterials 2014; 35: 6006–14. [DOI] [PubMed] [Google Scholar]
- 128.De Assuncao TM, Sun Y, Jalan-Sakrikar N, Drinane MC, Huang BQ, Li Y, Davila JI, Wang R, O'Hara SP, Lomberk GA, Urrutia RA, Ikeda Y, Huebert RC. Development and characterization of human-induced pluripotent stem cell-derived cholangiocytes. Lab Invest 2015; 95: 684–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dianat N, Dubois-Pot-Schneider H, Steichen C, Desterke C, Leclerc P, Raveux A, Combettes L, Weber A, Corlu A, Dubart-Kupperschmitt A. Generation of functional cholangiocyte-like cells from human pluripotent stem cells and HepaRG cells. Hepatology 2014; 60: 700–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sampaziotis F, Cardoso de Brito M, Madrigal P, Bertero A, Saeb-Parsy K, Soares FA, Schrumpf E, Melum E, Karlsen TH, Bradley JA, Gelson WT, Davies S, Baker A, Kaser A, Alexander GJ, Hannan NR, Vallier L. Cholangiocytes derived from human induced pluripotent stem cells for disease modeling and drug validation. Nat Biotechnol 2015; 33: 845–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sancho-Bru P, Roelandt P, Narain N, Pauwelyn K, Notelaers T, Shimizu T, Ott M, Verfaillie C. Directed differentiation of murine-induced pluripotent stemcells to functional hepatocyte-like cells. J Hepatol 2011; 54: 98–107. [DOI] [PubMed] [Google Scholar]
- 132.Friedman SL. Stellate cells: a moving target in hepatic fibrogenesis. Hepatology 2004; 40: 1041–43. [DOI] [PubMed] [Google Scholar]
- 133.Loh KM, Ang LT, Zhang J, Kumar V, Ang J, Auyeong JQ, Lee KL, Choo SH, Lim CY, Nichane M, Tan J, Noghabi MS, Azzola L, Ng ES, Durruthy-Durruthy J, Sebastiano V, Poellinger L, Elefanty AG, Stanley EG, Chen Q, Prabhakar S, Weissman IL, Lim B. Efficient endoderm induction from human pluripotent stem cells by logically directing signals controlling lineage bifurcations. Cell Stem Cell 2014; 14: 237–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Watanabe H, Takayama K, Inamura M, Tachibana M, Mimura N, Katayama K, Tashiro K, Nagamoto Y, Sakurai F, Kawabata K, Furue MK, Mizuguchi H. HHEX promotes hepatic-lineage specification through the negative regulation of eomesodermin. PLoS One 2014; 9: e90791–e90791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Takayama K, Inamura M, Kawabata K, Katayama K, Higuchi M, Tashiro K, Nonaka A, Sakurai F, Hayakawa T, Furue MK, Mizuguchi H. Efficient generation of functional hepatocytes from human embryonic stem cells and induced pluripotent stem cells by HNF4α transduction. Mol Ther 2012; 20: 127–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Vaskova EA, Stekleneva AE, Medvedev SP, Zakian SM. “Epigenetic memory” phenomenon in induced pluripotent stem cells. Acta Naturae 2013; 5: 15–21. [PMC free article] [PubMed] [Google Scholar]
- 137.Park HJ, Choi YJ, Kim JW, Chun HS, Im I, Yoon S, Han YM, Song CW, Kim H. Differences in the epigenetic regulation of cytochrome P450 genes between human embryonic stem cell-derived hepatocytes and primary hepatocytes. PLoS One 2015; 10: e0132992–e0132992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lee SB, Seo D, Choi D, Park KY, Holczbauer A, Marquardt JU, Conner EA, Factor VM, Thorgeirsson SS. Contribution of hepatic lineage stage-specific donor memory to the differential potential of induced mouse pluripotent stem cells. Stem Cells 2012; 30: 997–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nishino K, Toyoda M, Yamazaki-Inoue M, Fukawatase Y, Chikazawa E, Sakaguchi H, Akutsu H, Umezawa A. DNA methylation dynamics in human induced pluripotent stem cells over time. PLoS Genet 2011; 7: e1002085–e1002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kyttälä A, Moraghebi R, Valensisi C, Kettunen J, Andrus C, Pasumarthy KK, Nakanishi M, Nishimura K, Ohtaka M, Weltner J, Van Handel B, Parkkonen O, Sinisalo J, Jalanko A, Hawkins RD, Woods NB, Otonkoski T, Trokovic R. Genetic variability overrides the impact of parental cell type and determines iPSC differentiation potential. Stem Cell Reports 2016; 6: 200–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Haque A, Hexig B, Meng Q, Hossain S, Nagaoka M, Akaike T. The effect of recombinant E-cadherin substratum on the differentiation of endoderm-derived hepatocyte-like cells from embryonic stem cells. Biomaterials 2011; 32: 2032–42. [DOI] [PubMed] [Google Scholar]
- 142.Nagaoka M, Kobayashi M, Kawai C, Mallanna SK, Duncan SA. Design of a vitronectin-based recombinant protein as a defined substrate for differentiation of human pluripotent stem cells into hepatocyte-like cells. PLoS One 2015; 10: e0136350–e0136350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Siller R, Greenhough S, Naumovska E, Sullivan GJ. Small-molecule-driven hepatocyte differentiation of human pluripotent stem cells. Stem Cell Reports 2015; 4: 939–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tasnim F, Phan D, Toh YC, Yu H. Cost-effective differentiation of hepatocyte-like cells from human pluripotent stem cells using small molecules. Biomaterials 2015; 70: 115–25. [DOI] [PubMed] [Google Scholar]
- 145.Mandal A, Raju S, Viswanathan C. Long-term culture and cryopreservation does not affect the stability and functionality of human embryonic stem cell-derived hepatocyte-like cells. In Vitro Cell Dev Biol Anim 2016; 52: 243–51. [DOI] [PubMed] [Google Scholar]
- 146.Holmgren G, Sjögren AK, Barragan I, Sabirsh A, Sartipy P, Synnergren J, Björquist P, Ingelman-Sundberg M, Andersson TB, Edsbagge J. Long-term chronic toxicity testing using human pluripotent stem cell-derived hepatocytes. Drug Metab Dispos 2014; 42: 1401–6. [DOI] [PubMed] [Google Scholar]
- 147.Szkolnicka D, Farnworth SL, Lucendo-Villarin B, Storck C, Zhou W, Iredale JP, Flint O, Hay DC. Accurate prediction of drug-induced liver injury using stem cell-derived populations. Stem Cells Transl Med 2014; 3: 141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ware BR, Berger DR, Khetani SR. Prediction of drug-induced liver injury in micropatterned co-cultures containing iPSC-derived human hepatocytes. Toxicol Sci 2015; 145: 252–62. [DOI] [PubMed] [Google Scholar]
- 149.Schwartz RE, Trehan K, Andrus L, Sheahan TP, Ploss A, Duncan SA, Rice CM, Bhatia SN. Modeling hepatitis C virus infection using human induced pluripotent stem cells. Proc Natl Acad Sci USA 2012; 109: 2544–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Shlomai A, Schwartz RE, Ramanan V, Bhatta A, de Jong YP, Bhatia SN, Rice CM. Modeling host interactions with hepatitis B virus using primary and induced pluripotent stem cell-derived hepatocellular systems. Proc Natl Acad Sci USA 2014; 111: 12193–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ng S, Schwartz RE, March S, Galstian A, Gural N, Shan J, Prabhu M, Mota MM, Bhatia S.N. Human iPSC-derived hepatocyte-like cells support Plasmodium liver-stage infection in vitro. Stem Cell Rep 2015; 4: 348–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dianat N, Steichen C, Vallier L, Weber A, Dubart-Kupperschmitt A. Human pluripotent stem cells for modelling human liver diseases and cell therapy. Curr Gene Therapy 2013; 13: 120–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rashid ST, Corbineau S, Hannan N, Marciniak SJ, Miranda E, Alexander G, Huang-Doran I, Griffin J, Ahrlund-Richter L, Skepper J, Semple R, Weber A, Lomas DA, Vallier L. Modeling inherited metabolic disorders of the liver using human induced pluripotent stem cells. J Clin Invest 2010; 120: 3127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Asplund A, Pradip A, van Giezen M, Aspegren A, Choukair H, Rehnström M, Jacobsson S, Ghosheh N, El Hajjam D, Holmgren S, Larsson S, Benecke J, Butron M, Wigander A, Noaksson K, Sartipy P, Björquist P, Edsbagge J, Küppers-Munther B. One standardized differentiation procedure robustly generates homogenous hepatocyte cultures displaying metabolic diversity from a large panel of human pluripotent stem cells. Stem Cell Rev 2016; 12: 90–104. [DOI] [PubMed] [Google Scholar]
- 155.Takayama K, Morisaki Y, Kuno S, Nagamoto Y, Harada K, Furukawa N, Ohtaka M, Nishimura K, Imagawa K, Sakurai F, Tachibana M, Sumazaki R, Noguchi E, Nakanishi M, Hirata K, Kawabata K, Mizuguchi H. Prediction of interindividual differences in hepatic functions and drug sensitivity by using human iPS-derived hepatocytes. Proc Natl Acad Sci USA 2014; 111: 16772–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Xie Y, McGill MR, Dorko K, Kumer SC, Schmitt TM, Forster J, Jaeschke H. Mechanisms of acetaminophen-induced cell death in primary human hepatocytes. Toxicol Appl Pharmacol 2014; 279: 266–74. [DOI] [PMC free article] [PubMed] [Google Scholar]