Abstract
There is a recognised association between the "microscopic" forms of colitis and coeliac disease. There are a variety of subtle small intestinal changes in patients with "latent" gluten sensitivity, namely high intraepithelial lymphocyte (IEL) counts, abnormal mucosal permeability, and high levels of secretory IgA and IgM antibody to gliadin. These changes have hitherto not been investigated in microscopic colitis. Nine patients (four collagenous, five lymphocytic colitis) with normal villous architecture were studied. Small intestinal biopsies were obtained by Crosby capsule; small intestinal fluid was aspirated via the capsule. IEL counts were expressed per 100 epithelial cells, and intestinal IgA and IgM antigliadin antibody levels were measured by ELISA. Small intestinal permeability was measured by the lactulose:mannitol differential sugar permeability test. IEL counts were normal in all cases, median 17, range 7-30. Intestinal antigliadin antibodies were measured in six cases and were significantly elevated in two patients (both IgA and IgM). Intestinal permeability was measured in eight cases and was abnormal in two and borderline in one. These abnormalities did not overlap: four of nine patients had evidence of abnormal small intestinal function. Subclinical small intestinal disease is common in the two main forms of microscopic colitis.
Full text
PDF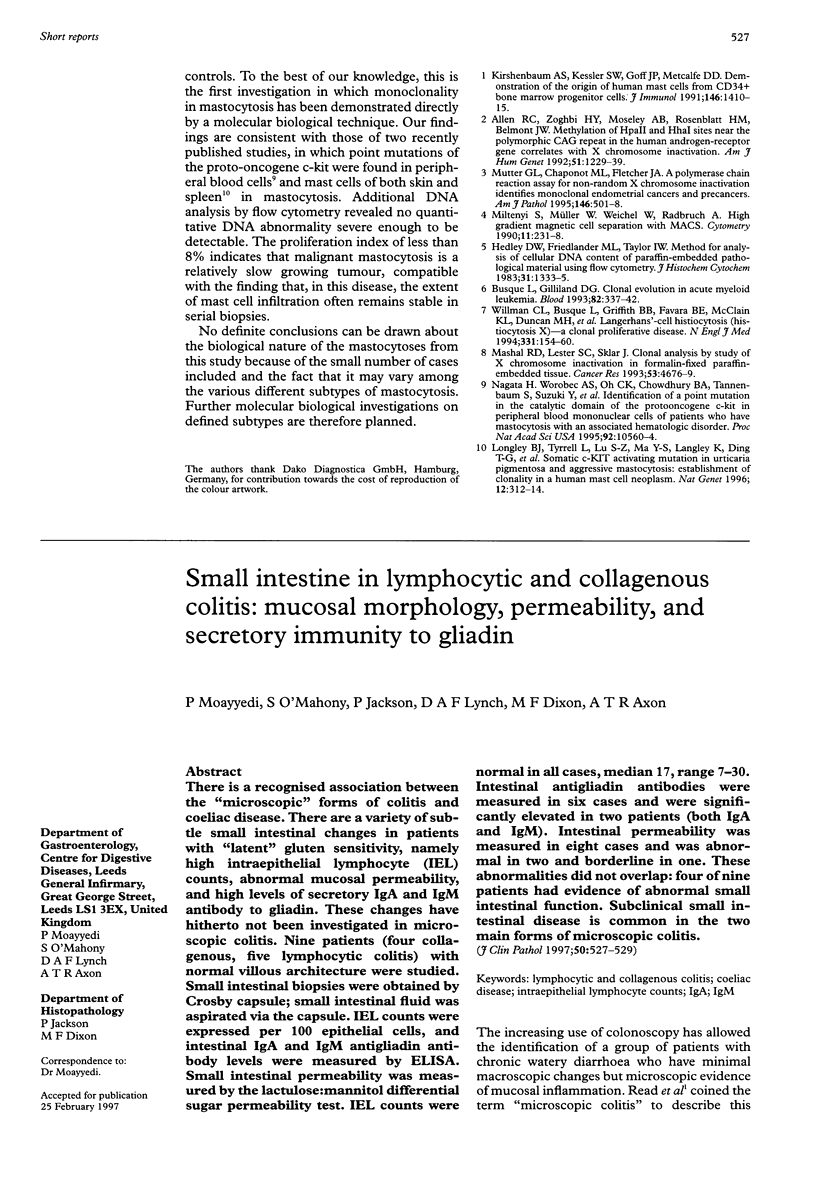

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Armes J., Gee D. C., Macrae F. A., Schroeder W., Bhathal P. S. Collagenous colitis: jejunal and colorectal pathology. J Clin Pathol. 1992 Sep;45(9):784–787. doi: 10.1136/jcp.45.9.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arranz E., Ferguson A. Intestinal antibody pattern of celiac disease: occurrence in patients with normal jejunal biopsy histology. Gastroenterology. 1993 May;104(5):1263–1272. doi: 10.1016/0016-5085(93)90333-8. [DOI] [PubMed] [Google Scholar]
- Cobden I., Dickinson R. J., Rothwell J., Axon A. T. Intestinal permeability assessed by excretion ratios of two molecules: results in coeliac disease. Br Med J. 1978 Oct 14;2(6144):1060–1060. doi: 10.1136/bmj.2.6144.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson A., Arranz E., O'Mahony S. Clinical and pathological spectrum of coeliac disease--active, silent, latent, potential. Gut. 1993 Feb;34(2):150–151. doi: 10.1136/gut.34.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giardiello F. M., Lazenby A. J., Bayless T. M., Levine E. J., Bias W. B., Ladenson P. W., Hutcheon D. F., Derevjanik N. L., Yardley J. H. Lymphocytic (microscopic) colitis. Clinicopathologic study of 18 patients and comparison to collagenous colitis. Dig Dis Sci. 1989 Nov;34(11):1730–1738. doi: 10.1007/BF01540051. [DOI] [PubMed] [Google Scholar]
- Giardiello F. M., Lazenby A. J., Yardley J. H., Bias W. B., Johnson J., Alianiello R. G., Bedine M. S., Bayless T. M. Increased HLA A1 and diminished HLA A3 in lymphocytic colitis compared to controls and patients with collagenous colitis. Dig Dis Sci. 1992 Apr;37(4):496–499. doi: 10.1007/BF01307569. [DOI] [PubMed] [Google Scholar]
- Lazenby A. J., Yardley J. H., Giardiello F. M., Jessurun J., Bayless T. M. Lymphocytic ("microscopic") colitis: a comparative histopathologic study with particular reference to collagenous colitis. Hum Pathol. 1989 Jan;20(1):18–28. doi: 10.1016/0046-8177(89)90198-6. [DOI] [PubMed] [Google Scholar]
- O'Mahony S., Arranz E., Barton J. R., Ferguson A. Dissociation between systemic and mucosal humoral immune responses in coeliac disease. Gut. 1991 Jan;32(1):29–35. doi: 10.1136/gut.32.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Mahony S., Vestey J. P., Ferguson A. Similarities in intestinal humoral immunity in dermatitis herpetiformis without enteropathy and in coeliac disease. Lancet. 1990 Jun 23;335(8704):1487–1490. doi: 10.1016/0140-6736(90)93029-o. [DOI] [PubMed] [Google Scholar]
- Read N. W., Krejs G. J., Read M. G., Santa Ana C. A., Morawski S. G., Fordtran J. S. Chronic diarrhea of unknown origin. Gastroenterology. 1980 Feb;78(2):264–271. [PubMed] [Google Scholar]



