Abstract
Purpose:
To evaluate the feasibility and efficacy of mini-scleral design (MSD) contact lenses to treat keratoconus patients who were unsatisfied with the results of corneal inlay.
Methods:
In this prospective interventional case series, 9 eyes of 6 keratoconus patients who were unsatisfied with the results of corneal inlay were fitted with MSD contact lenses. Demographic data, uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA), and higher order aberrations (HOAs) were evaluated before contact lens fitting. Corrected visual acuity by placing the MSD contact lens with or without over-refraction, and HOAs were measured one hour after contact lens fitting. One month after contact lens wearing, corrected visual acuity by placing the MSD contact lens with over-refraction and possible contact lens related problems were assessed. Ocular comfort and contact lens handling problems were asked in follow-up visits. The data was analyzed using descriptive statistical tests.
Results:
Nine eyes of 6 patients were successfully fitted with the mini-scleral lens. Fitting was ideal in 7 eyes and acceptable in 2 eyes. Mean corrected visual acuity by placing the MSD lens without over-refraction was 0.09 (range, 0.00-0.15) LogMAR which was significantly better than the mean BSCVA of 0.38 (range, 0.2-0.6) LogMAR (P = 0.007). The mean root mean square (RMS) of third-order coma and trefoil significantly decreased after MSD contact lens fitting (P = 0.012 and P = 0.015, respectively); however, changes in the fourth-order spherical aberration were not statistically significant (P = 0.336).
Conclusion:
Mini-scleral contact lenses may be helpful in the management of visually unsatisfied patients after corneal inlay.
Key words: Corneal Inlay, Keratoconus, Mini-scleral Design Contact Lens
INTRODUCTION
Management of moderate to severe keratoconus is a challenge to ophthalmologists. Until recently, the only option for patients with contact lens intolerance was penetrating corneal keratoplasty (PK). Unfortunately, significant regular or irregular astigmatism after PK commonly occurs, necessitating the use if contact lens in a significant percentage of these patients, which can be quite disappointing.[1,2,3] In order to give these patients a chance of being contact lens independent, intra corneal inlays were invented. It has been purposed that intra corneal lays can make the corneal center flatter and more regular and provide the patients with a better uncorrected visual acuity.[4,5,6,7,8]
Although the results of Kera Rings and Intacs for the management of keratoconus are promising, but there are still many issues to be addressed.[9,10] The main problem is predictability, which is not high sufficiently.[11,12] The introduction of femtosecond-assisted surgery was helpful but the results are still suboptimal for the time being.[13,14] Another issue is that the inlays cannot address the problem of the quality of vision or even alter the preexisting higher order aberrations.[13] Corneal inlay implantation may result in a multifocal cornea with a steeper corneal periphery and flatter mid-periphery.[15,16,17] Higher order aberrations (HOAs) in keratoconic eyes are much larger than those in normal eyes, and coma-like aberrations are dominant as compared with spherical-like aberrations.[18] Some studies have reported that rigid gas permeable (RGP) contact lenses improve visual performance by reducing HOAs in keratoconic eyes.[19] Diplopia and ghost images are also a concern, at least in some patients. Therefore, patients should be inferred that they may have to use the contact lens over the inlay.
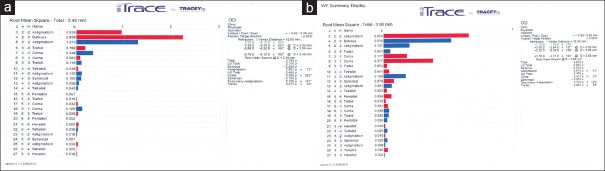
Managing unsatisfied patients is not only a continuum of our effort to give patients a good vision and quality of life, but also helps us to gain the patients' trust. Rigid gas-permeable contact lenses are considered a good choice in keratoconus patients, as they can mask corneal irregularity thus being helpful with reducing higher order aberrations. Occasionally, it is difficult to achieve an appropriate centration, especially in advanced stages of keratoconus or after corneal inlays. Another problem is reducing lens touch over the cornea while keeping the peripheral fit ideal. Additionally, it is better to avoid putting pressure over the inlay area to prevent corneal melting.[20] Contact lenses with a reverse geometry are helpful, but they are not easily available and have to be prepared individually. Given that, mini – scleral design (MSD) contact lenses may be a feasible option for reducing higher order aberrations-as well as correcting lower order aberrations-in these patients. Herein, we report the results of MSD contact lens fit in keratoconus patient who underwent intrastromal corneal ring (ISCR) implantation. To study the effect of MSD contact lens on HOAs, we measured wave front aberrations in these eyes before and after fitting these lenses which could vault the entire cornea and provide a more stable fit [Figure 1].
Figure 1.
(a) Miniscleral lens fitted on a cornea with a corneal inlay, (b) photo slit view of the same eye.
METHODS
This prospective interventional case series included keratoconus patients who were unsatisfied after intra-stromal ring segment implantation and were referred to the contact lens clinic from December 2011 to October 2012. Visual acuity was suboptimal with glasses or conventional corneal RGP lenses. The study was approved by the Eye Research Center Ethics Committee, affiliated to Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran and informed consent was obtained. Patients who had a history of amblyopia or other ocular diseases such as glaucoma or cataract were excluded.
Before contact lens fitting, all patients underwent a complete ophthalmologic examination including measurement of uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA), manifest refraction, keratometry, and slit lamp biomicroscopy. Furthermore, corrected visual acuity by placing the MSD contact lens with or without over-refraction were evaluated monocularly. The root –mean-square (RMS) of total, third, fourth, fifth, and sixth order Zernike coefficients were measured prior to and one hour after MSD contact lens fitting with the iTrace (Tracey Technologies, Houston, TX, USA) using software version 4.1. The iTrace combines a ray-tracing aberrometer with a corneal topographer to enable measurement of total, corneal, and internal aberrations. The software also has the capability of calculating aberrations for variable pupil sizes. Aberrations were measured under mesopic conditions without cycloplegia.
A trial set with the following parameters was used for fitting the mini scleral lens contact lenses:
Mini - scleral design (MSD) (Blanchard Contact Lens Inc., Manchester, Canada)
Non-fenestrated
Diameter: 15.8 mm
Available sagittal vaults: 3.80 to 5.60 mm; each in three different profile including D (Decreased), S (Standard), I (Increased)
DK/T: 100 (ISO/Fatt), 141 (gas to gas).
The main outcome measures were the ability to fit which was determined as either ideal (no central or mid-peripheral touch and fine alignment over the conjunctiva) or acceptable (no central or mid-peripheral touch and less than 3 clock hours conjunctival impingement), and an increase in visual acuity.
Fitting was assessed through evaluating the fluorescein pattern using diffuse cobalt light and assessment of the fluid reservoir over the cornea using a 30 degree oblique yellow slit beam through the cornea. Special attention was paid to clearance over the inlay site.
Statistical Methods
All statistical analyses were performed using SPSS software version 16.0 (Chicago: SPSS Inc.). Differences in visual acuity parameters and higher order aberrations with and without the MSD contact lens in the eye, were analyzed using the Willcoxon test. P value less than 0.05 was considered statistically significant.
RESULTS
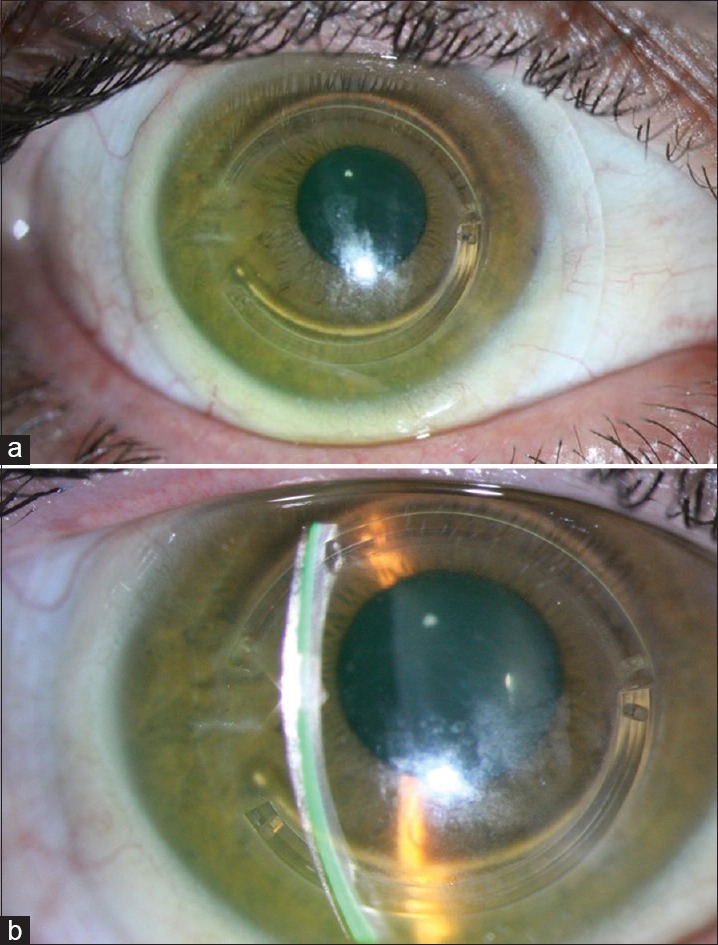
In this study, 9 eyes of 6 patients were fitted with mini scleral contact lenses. All patients were male with a mean age of 24 ± SD (range, 20-31) years. Demographic and fitting data are shown in Table 1. The interval between intrastromal ring implantation and the initial MSD contact lens fitting was 3 to 5 months (median: 4.5 months) and the patients were followed for at least for 3 months.
Table 1.
Patients demographics and fitting data
Prior to contact lens fitting, mean UCVA was 0.6 ± 0.26 (range, 0.3-1) LogMAR, and mean BSCVA was 0.38 ± 0.16 (range, 0.2-0.6) LogMAR.
The MSD contact lens could be fitted in all eyes with the assessment of ideal fit in 7 eyes or acceptable fit in 2 eyes [Figure 2]. During the study period (9 months), three patients (5 eyes) received and used the contact lens for at least 3 months before the last follow-up visit. In the remaining eyes, the contact lenses could not be obtained as a consequence of sanctions and the patients received other options like corneal transplantation.
Figure 2.

Schematic illustration of the ideal fit of a mini scleral lens on a cornea with two segmental corneal inlay.
After MSD contact lens fitting, spherical equivalent and refractive astigmatism significantly reduced. Mean corrected visual acuity by placing the MSD contact lens without over-refraction was 0.09 ± 0.05 LogMAR which was significantly increased compared to the values prior to the contact lens fit (P value = 0.007, Wilcoxon test). Mean corrected visual acuity by placing the MSD contact lens with over-refraction was 0.08 ± 0.05 LogMAR which showed no statistically significant difference compared to mean corrected visual acuity by placing the MSD contact lens without over-refraction (P = 0.16). The manifest refraction spherical equivalent (SE) improved from an average of −5.3 ± 3.9 diopters (D) prior to contact lens fitting to −0.5 ± 1.5 D (P = 0.00) after fitting. Moreover, mean refractive cylinder was −0.5 ± 1.8 D before contact lens fitting which decreased to −0.75 ± 0.45 D after fitting (P value = 0.005, Willcoxon test).
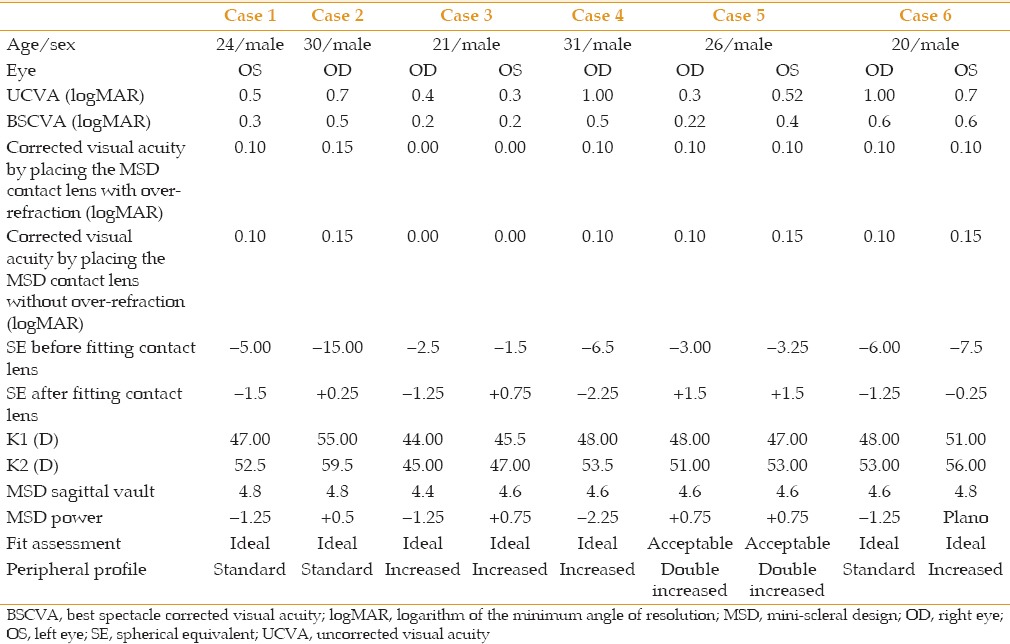
The mean RMS values of the higher order aberrations are summarized in Table 2. The mean RMS of third-order coma and trefoil aberrations decreased after mini scleral contact lens fitting (P = 0.012 and P = 0.015, respectively). Although no significant change was observed in the mean RMS of the fourth-order aberration after contact lens fitting, a tendency toward positive values was observed which might become significant in larger sample sizes [Figure 3].
Table 2.
Higher order aberrations with and without mini scleral lens
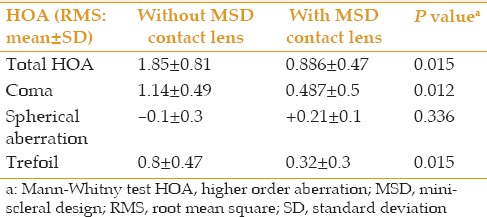
Figure 3.
(a) Higher order abberation (HOA) before mini scleral contact lens fitting, (b) HOA after mini scleral design contact lens fitting.
Case 3
The patient reported that he could wear the lenses comfortably for 5-7 hours a day, but he still had some difficulties with handling the lenses. The visual acuity was 0.00 LogMAR (20/20) OD and OS with the contact lenses one month after using the contact lenses. The over-refraction was plano OU. No corneal staining was observed. At the 3-month follow-up visit, he did not complain of handling the lenses.
Case 4
This patient had the longest period of follow-up (7 months). Visual acuity of the right eye with the MSD lens was 0.1 LogMAR (20/25) one month after using the contact lens. On the last follow-up examination, the patient was still wearing his contact lenses more than 10 hours a day without any problem. His contact lens-corrected visual acuity was stable at 20/25 in the right eye (the only eye which had a corneal inlay). Interestingly, he opted to wear a mini scleral contact lens in the left eye which did not have corneal inlay. He insisted on removing the inlay from the right cornea.
Case 6
The patient complained of dry eye symptoms within 1 to 2 hours of mini scleral contact lens wearing. The presenting visual acuity with the contact lens [Table 1] was 0.1 LogMAR (20/25) OD and 0.15 LogMAR (20/30) OS with a +0.75 over-refraction OD and a +0.5 over-refraction OS after 1 month. Both lenses were well settled in the eye with central and mid-peripheral clearance and only mild impingement on the inferonasal conjunctiva. He was advised to use artificial tear drops 3-4 times a day over the lenses and before and after using them. He had no problems with contact lens handling and needed no help. After 3 months, he was satisfied with the comfort of MSD lenses and reported that he was able to wear the lenses for 4-5 consecutive hours. After removing the lenses at midday for one hour, he was able to wear them for another 4-5 hours comfortably.
DISCUSSION
ICRS placement is an additive keratorefractive procedure which has been used for keratoconic eyes in Europe since 1997.[21,22] Several studies have shown an improvement in uncorrected and best spectacle corrected visual acuity over baseline measures in keratoconic patients with contact lens intolerance and clear central corneas. Corneal topography after ICRS shows a decrease in surface asymmetry.[21,22,23,24] After ICRS surgery, the majority of patients still need some types of visual correction, either spectacles or contact lenses.[21,22,24,25,26] However, the greatest flattening effect of the ring segment is exerted on the mid-peripheral region of the cornea directly over the ICRS which creates an abnormal artificial steepening of the peripheral cornea relative to the mid-periphery; this can make RGP fitting difficult.[15,16,17]
Mini scleral lenses have shown to be safe and are well tolerated in various corneal disorders.[27,28,29] In our study, the mini scleral contact lens was successfully fitted in all patients and, the visual acuity improved in all eyes after contact lens fitting. Mean corrected visual acuity by placing the MSD contact lens without over refraction (was 0.09 that was significantly better than mean BSCVA (P value = 0.007). Moreover, the reduction in the mean spherical equivalent and refractive astigmatism after MSD contact lens fitting was significant (P = 0.001 and P = 0.005, respectively). Because of the peripheral circumferential anterior corneal elevation caused by the ICRS, RGP contact lenses which their back optic zone diameter (BOZD) is not sufficiently large may tend to center over the ICRS and periphery rather than the corneal apex. This lens decenteration may cause significant vision problems including diplopia, ghosting, and blurring. Our study showed that MSD contact lenses could overcome the problem of poor lens centeration by vaulting the entire irregular corneal surface.
Few studies have evaluated contact lens fitting in keratoconic patients who undergo ICRS surgery with unsatisfactory results.[15,16,17,30,31] There is only one case report of MSD contact lens fitting in advanced keratoconus with INTACS. Recently, Dalton and Sorbara described one patient with keratoconus who was successfully fitted with a mini scleral contact lens for residual refractive error after ICRS surgery.[30]
Hladun and Harris reported successful fitting of the piggyback contact lens in a patient with keratoconus after ICRS placement. They used the Acuvue daily disposable soft contact lens with a modified Burger Kone keratoconic design RGP. The main complication of the piggyback contact lens was corneal hypoxia because of the limitation in oxygen availability to the cornea by combination of two contact lenses.[31]
Smith and Carrel described another keratoconic patient with ICRS who was fitted with a high-Dk piggyback contact lens. The patient was fitted with Purevision soft contact lens with a Dk of 101 and a modified Tru-Kone RGP design with a Dk of 58. The lens combination was well tolerated by the patient.[15] Although the high-Dk piggyback lens system often works quite well, patients sometimes complain of increased dry eye symptoms and some patients are unsatisfied with the trouble of cleaning two lenses.
In the current study, we measured HOAs with the iTrace aberrometer. We noticed that after mini scleral contact lens fitting, the mean RMS of third-order coma and trefoil aberrations decreased significantly. However, we found no evidence of the significant effect of mini scleral contact lens on spherical aberration. There was a tendency toward positive values in spherical aberrations after mini scleral contact lens fitting but the change was not statistically significant, which might be due to the small sample size of the study. To the best of our knowledge, this is the first study which evaluates the effect of the mini scleral contact lens on HOAs in keratoconus patients with ICRS.
Several studies have addressed HOA changes following the use of contact lenses.[32,33,34,35,36] Fitting of the rigid corneal and scleral contact lenses leads to a significant decrease in defocus, regular astigmatism, and HOAs.[34] The principle behind this finding is that the irregular corneal surface is replaced by the regular anterior surface of the contact lens. However, the effect of the RGP lens on HOAs remains a subject of controversy. One study showed that using the RGP contact lens might reduce or enhance HOAs based on the original existing ocular aberrations mainly through changes in vertical coma.[37]
The limitation of our study was small sample size which was partially caused by loss to follow-up of half of our patients due to the long waiting period for receiving the mini scleral contact lens.
In conclusion, mini-scleral contact lenses are relatively easy to fit and can be considered for many patients including post-ICRS subjects, and patients with severe dry eye.[28] We believe that mini scleral contact lenses are an excellent option for keratoconic patients after ICRS who achieve unsatisfactory outcomes with spectacles or corneal contact lens.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Randleman JB, Song CD, Palay DA. Indications for and outcomes of penetrating keratoplasty performed by resident surgeons. Am J Ophthalmol. 2003;136:68–75. doi: 10.1016/s0002-9394(02)02295-x. [DOI] [PubMed] [Google Scholar]
- 2.Skeens HM, Holland EJ. Large-diameter penetrating keratoplasty: Indications and outcomes. Cornea. 2010;29:296–301. doi: 10.1097/ICO.0b013e3181b6489e. [DOI] [PubMed] [Google Scholar]
- 3.Pan Q, Li X, Gu Y. Indications and outcomes of penetrating keratoplasty in a tertiary hospital in the developing world. Clin Experiment Ophthalmol. 2012;40:232–238. doi: 10.1111/j.1442-9071.2011.02598.x. [DOI] [PubMed] [Google Scholar]
- 4.Rabinowitz YS. Intacs for keratoconus. Curr Opin Ophthalmol. 2007;18:279–283. doi: 10.1097/ICU.0b013e3281fc94a5. [DOI] [PubMed] [Google Scholar]
- 5.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–1029. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 6.Tan BU, Purcell TL, Torres LF, Schanzlin DJ. New surgical approaches to the management of keratoconus and post-LASIK ectasia. Trans Am Ophthalmol Soc. 2006;104:212–220. [PMC free article] [PubMed] [Google Scholar]
- 7.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: Safety and efficacy. J Cataract Refract Surg. 2007;33:1886–1891. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 8.Sansanayudh W, Bahar I, Kumar NL, Shehadeh-Mashour R, Ritenour R, Singal N, et al. Intrastromal corneal ring segment SK implantation for moderate to severe keratoconus. J Cataract Refract Surg. 2010;36:110–113. doi: 10.1016/j.jcrs.2009.07.040. [DOI] [PubMed] [Google Scholar]
- 9.Kubaloglu A, Cinar Y, Sari ES, Koytak A, Ozdemir B, Ozertürk Y. Comparison of 2 intrastromal corneal ring segment models in the management of keratoconus. J Cataract Refract Surg. 2010;36:978–985. doi: 10.1016/j.jcrs.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 10.Piñero DP, Alio JL, Morbelli H, Uceda-Montanes A, El Kady B, Coskunseven E, et al. Refractive and corneal aberrometric changes after intracorneal ring implantation in corneas with pellucid marginal degeneration. Ophthalmology. 2009;116:1656–1664. doi: 10.1016/j.ophtha.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Piñero DP, Alió JL, El Kady B, Pascual I. Corneal aberrometric and refractive performance of 2 intrastromal corneal ring segment models in early and moderate ectatic disease. J Cataract Refract Surg. 2010;36:102–109. doi: 10.1016/j.jcrs.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 12.Kamburoglu G, Ertan A, Saraçbasi O. Measurement of depth of Intacs implanted via femtosecond laser using Pentacam. J Refract Surg. 2009;25:377–382. doi: 10.3928/1081597X-20090401-05. [DOI] [PubMed] [Google Scholar]
- 13.Piñero DP, Alio JL, El Kady B, Coskunseven E, Morbelli H, Uceda-Montanes A, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: Mechanical versus femtosecond-assisted procedures. Ophthalmology. 2009;116:1675–1687. doi: 10.1016/j.ophtha.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Rabinowitz YS, Li X, Ignacio TS, Maguen E. INTACS inserts using the femtosecond laser compared to the mechanical spreader in the treatment of keratoconus. J Refract Surg. 2006;22:764–771. doi: 10.3928/1081-597X-20061001-06. [DOI] [PubMed] [Google Scholar]
- 15.Smith KA, Carrell JD. High-Dk piggyback contact lenses over Intacs for keratoconus: A case report. Eye Contact Lens. 2008;34:238–241. doi: 10.1097/ICL.0b013e31815b7d91. [DOI] [PubMed] [Google Scholar]
- 16.Nepomuceno RL, Boxer Wachler BS, Weissman BA. Feasibility of contact lens fitting on keratoconus patients with INTACS inserts. Cont Lens Anterior Eye. 2003;26:175–180. doi: 10.1016/S1367-0484(03)00049-3. [DOI] [PubMed] [Google Scholar]
- 17.Uçakhan OO, Kanpolat A, Ozdemir O. Contact lens fitting for keratoconus after Intacs placement. Eye Contact Lens. 2006;32:75–77. doi: 10.1097/01.icl.0000174749.96423.ca. [DOI] [PubMed] [Google Scholar]
- 18.Maeda N, Fujikado T, Kuroda T, Mihashi T, Hirohara Y, Nishida K, et al. Wavefront aberrations measured with Hartmann-Shack sensor in patients with keratoconus. Ophthalmology. 2002;109:1996–2003. doi: 10.1016/s0161-6420(02)01279-4. [DOI] [PubMed] [Google Scholar]
- 19.Griffiths M, Zahner K, Collins M, Carney L. Masking of irregular corneal topography with contact lenses. CLAO J. 1998;24:76–81. [PubMed] [Google Scholar]
- 20.Ferrer C, Alió JL, Montañés AU, Pérez-Santonja JJ, del Rio MA, de Toledo JA, et al. Causes of intrastromal corneal ring segment explantation: Clinicopathologic correlation analysis. J Cataract Refract Surg. 2010;36:970–977. doi: 10.1016/j.jcrs.2009.12.042. [DOI] [PubMed] [Google Scholar]
- 21.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–1122. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 22.Colin J, Cochener B, Savary G, Malet F, Holmes-Higgin D. INTACS inserts for treating keratoconus: One-year results. Ophthalmology. 2001;108:1409–1414. doi: 10.1016/s0161-6420(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 23.Siganos CS, Kymionis GD, Kartakis N, Theodorakis MA, Astyrakakis N, Pallikaris IG. Management of keratoconus with Intacs. Am J Ophthalmol. 2003;135:64–70. doi: 10.1016/s0002-9394(02)01824-x. [DOI] [PubMed] [Google Scholar]
- 24.Boxer Wachler BS, CHristie JP, Chandra NS. Intacs for keratoconus with Intacs. Am J Ophthalmol. 2003;110:1031–1040. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 25.Alió JL, Artola A, Hassanein A, Haroun H, Galal A. One or 2 Intacs segments for the correction of keratoconus. J Cataract Refract Surg. 2005;31:943–953. doi: 10.1016/j.jcrs.2004.09.050. [DOI] [PubMed] [Google Scholar]
- 26.Hellstedt T, Mäkelä J, Uusitalo R, Emre S, Uusitalo R. Treating keratoconus with intacs corneal ring segments. J Refract Surg. 2005;21:236–246. doi: 10.3928/1081-597X-20050501-06. [DOI] [PubMed] [Google Scholar]
- 27.Tomalla M, Cagnolati W. Modern treatment options for the therapy of keratoconus. Cont Lens Anterior Eye. 2007;30:61–66. doi: 10.1016/j.clae.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 28.Ye P, Sun A, Weissman BA. Role of mini-scleral gas-permeable lenses in the treatment of corneal disorders. Eye Contact Lens. 2007;33:111–113. doi: 10.1097/01.ICL.0000258593.20221.c6. [DOI] [PubMed] [Google Scholar]
- 29.Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35:272–276. doi: 10.1016/j.clae.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 30.Dalton K, Sorbara L. Fitting an MSD (mini scleral design) rigid contact lens in advanced keratoconus with INTACS. Cont Lens Anterior Eye. 2011;34:274–281. doi: 10.1016/j.clae.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Hladun L, Harris M. Contact lens fitting over intrastromal corneal rings in a keratoconic patient. Optometry. 2004;75:48–54. doi: 10.1016/s1529-1839(04)70010-x. [DOI] [PubMed] [Google Scholar]
- 32.Atchison DA. Aberrations associated with rigid contact lenses. J Opt Soc Am A Opt Image Sci Vis. 1995;12:2267–2273. doi: 10.1364/josaa.12.002267. [DOI] [PubMed] [Google Scholar]
- 33.Hong X, Himebaugh N, Thibos LN. On-eye evaluation of optical performance of rigid and soft contact lenses. Optom Vis Sci. 2001;78:872–880. doi: 10.1097/00006324-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Lu F, Mao X, Qu J, Xu D, He JC. Monochromatic wavefront aberrations in the human eye with contact lenses. Optom Vis Sci. 2003;80:135–141. doi: 10.1097/00006324-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Xie PY, Wang D, Yang LN, Zhou WJ. The evaluation of visual quality in keratoconus eyes corrected by rigid gas-permeable contact lens. Zhonghua Yan Ke Za Zhi. 2005;41:1086–1091. [PubMed] [Google Scholar]
- 36.Dorronsoro C, Barbero S, Llorente L, Marcos S. On-eye measurement of optical performance of rigid gas permeable contact lenses based on ocular and corneal aberrometry. Optom Vis Sci. 2003;80:115–125. doi: 10.1097/00006324-200302000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Choi J, Wee WR, Lee JH, Kim MK. Changes of ocular higher order aberration in on-and off-eye of rigid gas permeable contact lenses. Optom Vis Sci. 2007;84:42–51. doi: 10.1097/01.opx.0000254036.45989.65. [DOI] [PubMed] [Google Scholar]