Abstract
Purpose:
To evaluate the effects of prophylactic laser peripheral iridotomy on corneal endothelial cell density and cell morphology in subjects with primary angle closure suspect (PACS) within a one-year follow-up period.
Methods:
In this quasi-experimental prospective study, from June 2012 to November 2013, thirty-five PACS eyes underwent laser peripheral iridotomy at clinics affiliated to Shiraz University of Medical Sciences, Shiraz, Iran. After obtaining informed consent, specular microscopy was performed at baseline and at 3-month, 6-month and 12-month follow-up visits. Central, nasal and temporal endothelial cell counts and cell morphology were evaluated via non-contact specular microscopy.
Results:
The mean subject age was 53.4 ± 7.9 years, and the majority of subjects were women (88.2%). The mean central corneal endothelial cell count prior to laser peripheral iridotomy was 2528 ± 119.2, and this value changed to 2470 ± 175.9, 2425 ± 150.6, and 2407 ± 69.02 at the 3-month, 6-month, and 12-month follow-up visits, respectively; these differences did not reach statistical significance. Additionally, the changes in the number of cells, the hexagonality of cells, and the coefficient of variation (CV) in the central, nasal, and temporal areas were not significant.
Conclusion:
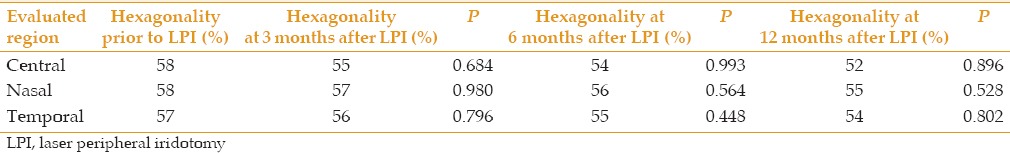
In PACS eyes, we did not find a decline in corneal endothelial cell density or a change in cell morphological characteristics, including cell hexagonality and CV, in the central, nasal, and temporal regions of the cornea in any of our subjects over a one-year follow-up period.
Key words: Corneal Endothelial Cell, Laser, Iris, Angle Closure Glaucoma
INTRODUCTION
Glaucoma, a progressive optic neuropathy, is the leading cause of vision loss.[1,2,3] Classifications for angle closure glaucoma have recently been proposed based on gonioscopy and clinical evaluation findings. It is unsurprising that primary angle closure glaucoma (PACG) is estimated to cause blindness in two to five times as many subjects as primary open angle glaucoma.[4,5] Studies revealed that 22% of subjects with primary angle closure suspect (PACS) may progress to primary angle closure (PAC) and that 28.5% of PAC subjects may develop PACG within 5 years if no treatment is prescribed.[6]
Laser peripheral iridotomy is considered as the standard treatment modality for PACS. This procedure can be used to eliminate the pupillary block and to extend the anterior chamber angle by balancing the pressure between the posterior and anterior spaces. This technique has essentially replaced surgical iridectomy as the modality of choice because laser peripheral iridotomy has been considered as a simple, non-invasive technique that can be completed in an outpatient setting without the risks and severe complications associated with invasive surgery.[7,8,9] However, there is a controversy regarding the safety of the laser peripheral iridotomy procedure to endothelial cells in terms of cell density and morphology. Given that this procedure can be used to prevent further vision loss in PACS subjects, it is important to determine whether this procedure is safe to endothelial cells in order to prevent further morbidity. In this study, we assessed the effects of prophylactic laser peripheral iridotomy on corneal endothelial cell density, cell hexagonality and coefficient of variation (CV) in PACS subjects over a 12-month follow-up period.
METHODS
This was a quasi-experimental prospective study approved by the ethics committee of Shiraz University of Medical Sciences, and informed consent was obtained from all subjects. This study adhered to the tenets of the Declaration of Helsinki. All enrolled patients were consecutively recruited from the Shahid Motahari and Poostchi Ophthalmology Clinics, Shiraz University of Medical Sciences, Shiraz, Iran, from June 2012 to November 2013. Each patient underwent slit-lamp examination, intraocular pressure (IOP) measurement via Goldmann applanation tonometry (GAT), and gonioscopy employing a Sussman four-mirror gonioscope to detect appositional or synechial closure, as well as stereoscopic evaluation of the optic disc using a + 90 diopter non-contact lens. All ophthalmic examinations and laser iridotomy procedures were performed by an ophthalmologist.
Patients for whom both eyes were diagnosed with PACS were qualified for inclusion in this study. Based on the standard description, a PACS eye displayed an appositional contact between the surface level of the iris and the posterior portion of the trabeculum extending at least 180° based on gonioscopic evaluation and showing an IOP ≤21 mmHg as measured by GAT.[7] The exclusion criteria were any history of a previous episode of increased IOP, a history of intraocular surgery, a history of using anti-glaucoma medications, a history of acquired or genetic diseases of the cornea, any abnormality on specular microscopy prior to laser iridotomy, a history of ocular trauma or any retinal disease, and the presence of a systemic disease such as diabetes mellitus.
Following subject selection, all subjects underwent specular microscopy using a Topcon SP-3000P noncontact automated specular microscope (Topcon Corporation, Tokyo, Japan). This device autofocuses on the surface of the corneal endothelium and provides high magnification, beneficial image quality and the potential to measure cell density and to perform morphometric evaluation. We evaluated the cell size according to various factors, such as cell density, the CV in the cell area (SD/mean), and the proportion of hexagonal cells, based on standard methods.[10,11,12]
Subsequently, one drop of 2% pilocarpine (Sinadarou, Tehran, Iran) and one drop of 0.5% Tetracaine (Sinadarou, Tehran, Iran) were instilled into the eye. Conventional laser peripheral iridotomy was performed on the peripheral superior temporal region of the iris of one randomly selected eye by an ophthalmologist using a Nidek 1800-YC Nd:YAG Laser (Tokyo, Japan) and an Abraham lens. The laser iridotomy procedure began with a single 4-7 mJ pulse, and the laser power increased until patency was realized. If IOP increased significantly by more than 5 mmHg, the subjects were treated with anti-glaucoma medications accordingly. Furthermore, all subjects were prescribed 0.1% betamethasone eye drops four times a day for 10 days. All specular microscopy measurements were documented by a single technician, and the central, superior nasal and superior temporal regions were examined at baseline and at the 3-month, 6-month and 12-month follow-up visits. The sample size has been calculated according the simple sample size formula. Statistical analysis was performed using SPSS software (version 20, SPSS Inc., Chicago, IL, USA), and the paired t-test was used to assess the significance of differences. A P value of less than 0.05 was considered to indicate a significant difference.
RESULTS
Thirty-five eyes of 35 patients were enrolled in this study. One patient was excluded because her IOP increased during the follow-up period. The mean total pulse for each subject was 49.9 ± 12.6 mJ. The mean subject age was 53.4 ± 7.99 years (range: 62-36 years), and 30 subjects (88.2%) were female. In 3 cases, minimal hemorrhage from the iris was observed, and this complication was managed accordingly. The endothelial cell density, cell hexagonality and CV at baseline and at the 3-month, 6-month and over 12-month follow-up visits were recorded. The mean central corneal endothelial cell count prior to laser iridotomy was 2528 ± 119.2, and this value changed to 2470 ± 175.9, 2425 ± 150.6, and 2407 ± 69.02 at the 3-month, 6-month, and 12-month follow-up visits, respectively; these differences did not reach statistical significance (P > 0.05). Additionally, the change in the number of cells, the CV and the hexagonality of cells in the central, nasal, and temporal areas were not significant (P > 0.05) [Tables 1–3].
Table 1.
Endothelial cell density at baseline and at 3-month, 6-month and 12-month follow-up visits in 3 different regions
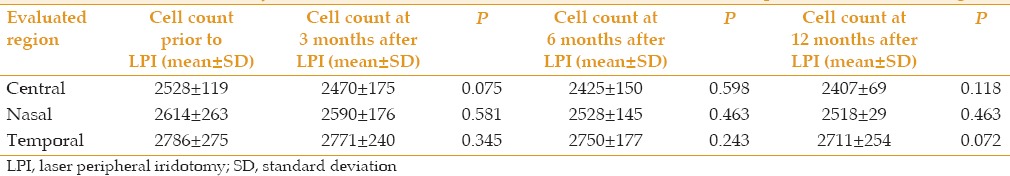
Table 3.
Mean coefficient of variation in endothelial cells at baseline and at 3-month, 6-month and 12-month follow-up visits in 3 different regions
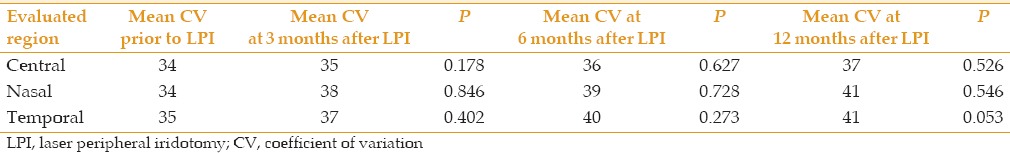
Table 2.
Hexagonality of endothelial cells (%) at baseline and at 3-month, 6-month and 12-month follow-up visits in 3 different regions
DISCUSSION
Several reports have demonstrated complications following laser peripheral iridotomy, including iris inflammation, IOP elevation, corneal decompensation, hemorrhage, and posterior synechiae. Thus, there is controversy regarding the safety of this procedure to the corneal endothelium, especially with respect to the relationship between laser peripheral iridotomy and corneal decompensation.[13,14,15,16] We assessed the effects of prophylactic laser peripheral iridotomy on corneal endothelial cell density, hexagonality, and CV in PACS eyes over a 12-month follow-up period. Our results revealed no decline in corneal endothelial cell density or alteration in cell morphology in the central, nasal, and temporal regions over the one-year follow-up period.
Other studies showed that laser iridotomy may affect the corneal endothelium, leading to varying outcomes. Although the procedure has been shown to be fairly safe, there remains a long-standing risk of corneal decompensation, as corneal transplantation may ultimately be required. The time period between laser iridotomy and corneal decompensation has been stated to be up to eight years.[16,17] However, since our results were produced over only 12 months, we are unable to conclude that this procedure is safe to the corneal endothelium, and we should follow our subjects for a longer duration.
Marraffa et al found a substantial decrease in corneal endothelial cell density after Nd:YAG iridotomy in the cases of angle closure glaucoma.[17] Among the findings in which Nd:YAG laser iridotomy was given as prophylaxis, Wu et al in a study revealed a significant cell density decrease at 1 year duration meanwhile no statistical correlation found between the change in endothelial cell density and the entire energy power used throughout the treatment procedure.[18]
Canning et al found that a majority of subjects exhibited serious focal endothelial impairment following Nd:YAG laser iridotomy, although there was no evidence of persistent injury based on short-term follow-up examinations.[19]
Using prophylactic sequential laser iridotomy, Kumar et al revealed declines in corneal endothelial cell density and central corneal thickness over 3 years, although these changes were comparable to those in the fellow eye, which had not been treated.[20] Kumar et al established follow-up study for 3 years duration of the central area of the cornea,[20] however we report our cases for a 12-month follow-up in 3 different areas of the cornea.
Panek et al revealed a slight but substantial decrease in corneal endothelial cell density following the Nd:YAG laser peripheral iridotomy.[21] Similarly, Wu et al found a meaningful decline in corneal endothelial cell density after 1 year;[18] however, Schwenn et al did not.[22] Our study also demonstrated no significant changes in corneal endothelial cell density within one year after laser peripheral iridotomy.
In the studies of Indian subjects by Ramani et al and of Iranian individuals by Faramarzi et al, no significant changes in central corneal thickness were observed following laser peripheral iridotomy.[22,23,24] Although we did not measure this parameter, it may be interesting to evaluate the effects of peripheral iridotomy on central corneal thickness and other parameters such as anterior chamber depth, anterior chamber angle, axial length, lens thickness, relative lens position, iris-ciliary process distance, and iris thickness, especially for comparison between races, as these anatomic parameters may vary according to ethnicity.
Kumaret al reported that polymegathism decreased while pleomorphism increased over 3 years after prophylactic laser iridotomy.[20] However, our study showed no changes in the hexagonality of cells or in the CV within one year after this procedure.
The major limitations of our study were its short follow-up duration, the lack of a control group in the study design, and the sample size, although the required sample size was estimated based on the simple sample size formula. Hence, the absence of a finding does not establish that prophylactic laser iridotomy is completely safe. Despite these limitations, we believe that the strengths of this study, which include its prospective nature, examination of a homogenous population, and use of non-contact measurement to assess the nasal, central and temporal areas of the cornea, make its findings particularly significant.
More studies involve larger sample size maybe required in order to show changes in corneal endothelium following laser iridotomy. Since it may present opportunities in term of preventive strategies, it may allow us to guarantee that the laser iridotomy does not cause additional morbidity to the patients.
In conclusion, our findings demonstrated the safety status of laser iridotomy over a short follow-up duration. In PACS eyes, we did not detect a decline in corneal endothelial cell density or alterations in cell morphological characteristics, including cell hexagonality and CV, in the central, nasal, and temporal areas of the cornea in any of our subjects over a one-year follow-up period.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the staff of the Poostchi and Motahari eye clinics, Shiraz University of Medical Sciences for providing technical support as well as the Poostchi Eye Research Center and the Department of Ophthalmology, Shiraz University of Medical Sciences, for providing academic support. This project was assigned grant No 91-5391 in the office of the Vice Chancellor of Research Affairs, Shiraz University of Medical Sciences. This study represents part of the thesis work performed by Sara Jahanian MD in order to complete a residency program in ophthalmology.
REFERENCES
- 1.Roy Chowdhury U, PFautsch M. Intracranial pressure and its relationship to glaucoma: Current understanding and future directions. Med Hypothesis Discov Innov Ophthalmol. 2015;4:71–80. [PMC free article] [PubMed] [Google Scholar]
- 2.Heidary F, Heidary R, Jamali H, Gharebaghi R. Afraid of the dark; raising awareness of societies each year during world glaucoma week. Iran J Public Health. 2015;44:716–717. [PMC free article] [PubMed] [Google Scholar]
- 3.Sosa I, Culina K, Bosnar A. Review on hypothetical implementing TGF-ß family members in glaucoma therapy. Med Hypothesis Discov Innov Ophthalmol. 2012;1:57–62. [PMC free article] [PubMed] [Google Scholar]
- 4.Foster PJ, Oen FT, Machin D, Ng TP, Devereux JG, Johnson GJ, et al. The prevalence of glaucoma in Chinese residents of Singapore: A cross-sectional population survey of the Tanjong Pagar district. Arch Ophthalmol. 2000;118:1105–1111. doi: 10.1001/archopht.118.8.1105. [DOI] [PubMed] [Google Scholar]
- 5.Razeghinejad MR, Banifatemi M. Ocular biometry in angle closure. J Ophthalmic Vis Res. 2013;8:17–24. [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas R, Parikh R, Muliyil J, Kumar RS. Five-year risk of progression of primary angle closure to primary angle closure glaucoma: A population-based study. Acta Ophthalmol Scand. 2003;81:480–485. doi: 10.1034/j.1600-0420.2003.00135.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee JR, Choi JY, Kim YD, Choi J. Laser peripheral iridotomy with iridoplasty in primary angle closure suspect: Anterior chamber analysis by pentacam. Korean J Ophthalmol. 2011;25:252–256. doi: 10.3341/kjo.2011.25.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boey PY, Singhal S, Perera SA, Aung T. Conventional and emerging treatments in the management of acute primary angle closure. Clin Ophthalmol. 2012;6:417–424. doi: 10.2147/OPTH.S16400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ang LP, Higashihara H, Sotozono C, Shanmuganathan VA, Dua H, Tan DT, et al. Argon laser iridotomy-induced bullous keratopathy a growing problem in Japan. Br J Ophthalmol. 2007;91:1613–1615. doi: 10.1136/bjo.2007.120261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosa N, Lanza M, Borrelli M, Filosa ML, De Bernardo M, Ventriglia VM, et al. Corneal thickness and endothelial cell characteristics in patients with myotonic dystrophy. Ophthalmology. 2010;117:223–225. doi: 10.1016/j.ophtha.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Doughty MJ. Evaluation of possible error sources in corneal endothelial morphometry with a semiautomated noncontact specular microscope. Cornea. 2013;32:1196–1203. doi: 10.1097/ICO.0b013e318295e72a. [DOI] [PubMed] [Google Scholar]
- 12.Hatipoglu E, Arici C, Arslan OS, Dikkaya F, Sultan P, Kadioglu P, et al. Corneal endothelial cell density and morphology in patients with acromegaly. Growth Horm IGF Res. 2014;24:260–263. doi: 10.1016/j.ghir.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Kataoka T, Zako M, Takeyama M, Ohno-Jinno A, Sugenoya J, Iwaki M. Cooling prevents induction of corneal damage by argon laser peripheral iridotomy. Jpn J Ophthalmol. 2007;51:317–324. doi: 10.1007/s10384-007-0460-3. [DOI] [PubMed] [Google Scholar]
- 14.Liang YB, Wang NL, Rong SS, Thomas R. Initial treatment for primary angle-closure glaucoma in China. J Glaucoma. 2015;24:469–473. doi: 10.1097/IJG.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 15.Golan S, Levkovitch-Verbin H, Shemesh G, Kurtz S. Anterior chamber bleeding after laser peripheral iridotomy. JAMA Ophthalmol. 2013;131:626–629. doi: 10.1001/jamaophthalmol.2013.1642. [DOI] [PubMed] [Google Scholar]
- 16.Wang PX, Koh VT, Loon SC. Laser iridotomy and the corneal endothelium: A systemic review. Acta Ophthalmol. 2014;92:604–616. doi: 10.1111/aos.12367. [DOI] [PubMed] [Google Scholar]
- 17.Marraffa M, Marchini G, Pagliarusco A, Perfetti S, Toscano A, Brunelli C, et al. Ultrasound biomicroscopy and corneal endothelium in Nd: YAG-laser iridotomy. Ophthalmic Surg Lasers. 1995;26:519–523. [PubMed] [Google Scholar]
- 18.Wu SC, Jeng S, Huang SC, Lin SM. Corneal endothelial damage after neodymium: YAG laser iridotomy. Ophthalmic Surg Lasers. 2000;31:411–416. [PubMed] [Google Scholar]
- 19.Canning CR, Capon MR, Sherrard ES, Kerr Muir MG, Pearson R, Cooling RJ. Neodymium: YAG laser iridotomies – Short-term comparison with capsulotomies and long-term follow-up. Graefes Arch Clin Exp Ophthalmol. 1988;226:49–54. doi: 10.1007/BF02172718. [DOI] [PubMed] [Google Scholar]
- 20.Kumar RS, Baskaran M, Friedman DS, Xu Y, Wong HT, Lavanya R, et al. Effect of prophylactic laser iridotomy on corneal endothelial cell density over 3 years in primary angle closure suspects. Br J Ophthalmol. 2013;97:258–261. doi: 10.1136/bjophthalmol-2012-302013. [DOI] [PubMed] [Google Scholar]
- 21.Panek WC, Lee DA, Christensen RE. The effects of Nd: YAG laser iridotomy on the corneal endothelium. Am J Ophthalmol. 1991;111:505–507. doi: 10.1016/s0002-9394(14)72388-8. [DOI] [PubMed] [Google Scholar]
- 22.Schwenn O, Sell F, Pfeiffer N, Grehn F. Prophylactic Nd: YAG-laser iridotomy versus surgical iridectomy: a randomized, prospective study. Ger J Ophthalmol. 1995;4:374–379. [PubMed] [Google Scholar]
- 23.Ramani KK, Mani B, George RJ, Lingam V. Follow-up of primary angle closure suspects after laser peripheral iridotomy using ultrasound biomicroscopy and A-scan biometry for a period of 2 years. J Glaucoma. 2009;18:521–527. doi: 10.1097/IJG.0b013e318193c12d. [DOI] [PubMed] [Google Scholar]
- 24.Faramarzi A, Yazdani S, Pakravan M. Central anterior chamber depth changes after prophylactic laser iridotomy. Optom Vis Sci. 2013;90:707–710. doi: 10.1097/OPX.0b013e3182968c62. [DOI] [PubMed] [Google Scholar]


