Abstract
Purpose:
To report the rate of flap-related complications in LASIK surgery performed by in-training ophthalmology residents and to analyze the risk factors for these complications.
Methods:
We analyzed 273 flap dissections in 145 patients from March 2013 to February 2014. We included all LASIK surgeries performed by 32 ophthalmology residents using a Moria M2 microkeratome. All the flap-related complications were noted. Comparison between both groups with and without complications was performed with an independent Student's t-test and relative risks were calculated.
Results:
There were 19 flap-related complications out of the 273 flap dissections (6.95%). The most common complication was incomplete flap dissection (n = 10; 3.66%), followed by free-cap (n = 5; 1.83%), and flap-buttonhole (n = 2; 0.73%). There was no significant difference between the complicated and uncomplicated cases in terms of the right versus the left eye, pachymetry results, white-to-white diameter, and spherical equivalent. But this difference was significant for mean keratometry (P = 0.008), K-min (P = 0.01), and K-max (P = 0.03) between these groups. Final visual acuity after rescheduling laser treatment was similar in both groups. Relative risks for flap-related complications were 2.03 for the first LASIK surgery (CI 95% 0.64 to 6.48; P = 0.22) and 1.26 (CI 95% 0.43 to 3.69; P = 0.66) for the surgeon's flap-related complications. Female gender presented an odds ratio of 2.48 (CI 95% 0.68 to 9.00; P = 0.16) for complications.
Conclusion:
Flap-related complications are common intraoperative event during LASIK surgery performed by in-training ophthalmologists. Keratometries and surgeon's first procedure represent a higher probability for flap related complications than some other biometric parameters of patient's eye.
Key words: Laser in situ keratomileusis, Intraoperative Complications, Academic Training, Refractive Surgery
INTRODUCTION
Laser in situ keratomileusis (LASIK) is a common method for the surgical correction of myopia, hyperopia, and astigmatism.[1] The creation of the corneal flap is the first and most critical step during LASIK surgery and may be associated with intraoperative complications affecting the rest of the procedure and postoperative course, thereby jeopardizing the patient's visual acuity.[2,3] Complications can occur at any time, so it is necessary to understand the etiology, pathophysiology, visual implications, and management of complications during and after refractive surgery. This knowledge will help surgeons obtain more consistent and predictable results.[4]
Regarding LASIK surgery for residents, most studies support a training program that includes lectures, observation of refractive surgery, wet labs, preoperative and post-operative management, and performing surgery under the supervision of an experienced refractive surgeon. As an evidence of its growing prominence, refractive surgery is no longer taught only in anterior segment or refractive surgery fellowship programs, but it is now a fundamental part of the ophthalmology residency program. In 2010, the Accreditation Council for Graduate Medical Education (ACGME) put forth the first refractive surgical requirement for ophthalmology residency programs with a minimum of 6 procedures, combining primary and assisted. This new requirement acknowledges the growing prominence of refractive surgery in the practice of ophthalmology.
In this study, we determined the incidence of flap complications at our institution and tried to determine if there are any biometric or surgeon-related factors associated with these complications in LASIK surgery performed by residents in training.
METHODS
Data Collection
We analyzed flap dissections performed during consecutive primary LASIK surgeries from March 2013 to February 2014 in a prospective observational manner. To meet inclusion criteria for this study, each case had to be performed either by second- or third-year ophthalmology residents or by novice cornea fellows. All patients were aware that a surgeon-in-training would be operating as part of the surgical team. Surgical case records were reviewed to identify each resident's number of corneal flap creation.
Patients
All patients signed an informed consent for LASIK surgery. The Ethics Committee of Instituto de Oftalmologia “Conde de Valenciana” approved this study. All patients had stable refraction for at least 6 months before surgery, a corrected distance visual acuity (CDVA) of 20/25 or better, and over 21 years of age. Patients were excluded if there was an abnormal ocular examination, topographic evidence of keratoconus, or warpage from contact lenses and pregnancy. Preoperative evaluation included a comprehensive ophthalmic examination: uncorrected distance visual acuity (UDVA), manifest and cycloplegic refractions, applanation tonometry, and computerized corneal tomography using Pentacam (Oculus Optikgeräte GmbH, Wetzlar, Germany) and/or Orbscan II (Bausch and Lomb, New York, USA). We obtained keratometry and pachymetry data from Pentacam tomography and white-to-white distance data from Orbscan tomography.
Keratectomy and Surgical Technique
Corneal flaps were created using the Moria M2 microkeratome (Moria, Antony, France) with 90-μm or 130-μm plates according to the preference of the surgeon, and a superior hinge [Figure 1]. The cornea was marked with gentian violet staining, and the standard speed of pass (speed #2: 15,000 rpm, 2 seconds of cutting time) was used in all cases. One single head was used in both eyes of each patient (the right eye was always done first), and the head was discarded upon completion of the procedure. The microkeratome settings (suction ring, flap stop) were chosen according to the steepest K (manufacturer's nomogram), aiming for the maximum flap diameter. If a complication occurred, it was reported in the computerized patient record system and also by direct notification to any of the authors. The surgeon and its consultant physician adjudged if the complication deserved ablation cessation. Ablation was done using the Schwind Amaris 750 s excimer laser (Schwind Eye-tech-solutions GmbH, Germany); or the MEL 80 excimer laser (Carl Zeiss Meditec, Jena, Germany). After performing the laser ablation, the flap was floated back into position, and the stromal bed was irrigated with balanced salt solution. Flap alignment was checked using gentian violet premarkings on the cornea, and a striae test was performed to ensure proper flap adherence. In this test, a gentle downwards pressure was put on the corneal edge just beyond the edge of the flap; fine folds will be seen radiating into the flap if good adhesion was achieved. All patients were treated postoperatively with fluorometholone acetate 0.1% ophthalmic suspension every 4 hours for 1 week and then in tapering doses per week; moxifloxacin hydrochloride 0.5% ophthalmic solution 4 times a day for 10 days; and hyaluronic acid 0.4% every 2 hours for 1 week. If the patient did not receive ablation due to a complication, an individualized treatment was proposed after new refraction stability was confirmed.
Figure 1.

Moria M2 microkeratome, performing corneal flap cut.
If an incomplete flap was created, and there was sufficient surface area in the stromal bed to allow for laser ablation, with a reasonable ablation zone, then the procedure continued as planned. If the hinge was beyond the visual axis, but the stromal bed was smaller than intended, it was considered to reattempt flap creation with a second pass of the microkeratome. If the hinge was within the visual axis, the flap was replaced and the procedure postponed. If a free cap was created, and the stromal bed was irregular, the flap was replaced without laser ablation; if the stromal bed was regular, the cap was handled by being placed on a drop of balanced salt solution in a chamber and proceeded with ablation, and the cap re-positioned.
Data and Statistical Analysis
Data analysis was performed using MS Excel 2010 for Windows 7. Means, standard deviations, and ranges were used to express data. The two study groups were compared using independent Student's t-test. Relative risks were calculated using relative risk calculator from MedCalc (www.medcalc.org). Statistical significance was considered at P < 0.05.
RESULTS
All LASIK surgeries performed by 32 residents (29 second- and third-year ophthalmology residents and 3 cornea fellows) were included in this study. Of 279 programmed treatments, 273 flap dissections were done in 145 patients. These comprised 102 female patients (70.21%) and 43 (29.78%) male patients. Mean patient age was 28.39 ± 6.79 years (range: 18 to 52 years). The most common preoperative refraction was compound myopic astigmatism (199 eyes; 71.32%). Distribution of refractive status is shown in Table 1.
Table 1.
Preoperative refraction of eyes undergoing laser in situ keratomileusis

The mean preoperative uncorrected distance visual acuity (UDVA) was 0.99 ± 0.39 logMAR (range 0 to 1.82), and the corrected distance visual acuity (CDVA) was 0.01 ± 0.1 (range −0.1 to 0.17/Snellen equivalent of 20/20). The mean preoperative spherical equivalent refraction was – 3.04 ± 1.93 D (range −8.75 to +2.12). Preoperative astigmatism was in a range of −0.25 to −6.00 D. Other biometric characteristics are shown in Table 2.
Table 2.
Biometric characteristics of the patients

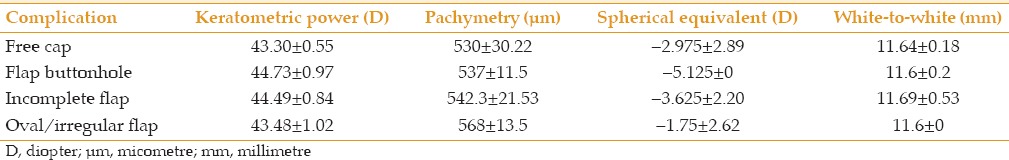
There were 19 flap-related complications out of the 273 flap dissections involved (6.95%). The most common complication was incomplete flap dissection (n = 10; 3.66%), followed by free-cap (n = 5; 1.83%), and flap-buttonhole (n = 2; 0.73%). There were 2 infrequent complications of an irregular flap and an oval flap that allowed ablation. Ablation treatment was not applied to 13 eyes out of the 19 flap-related complications (68.42%). Flap-related complications were the cause of only 4 contralateral eye surgical suspensions. Table 3 shows the overall comparison between the complicated and uncomplicated groups. There was a significant difference for the mean keratometry, minimum keratometry, and maximum keratometry between these groups. Table 4 shows biometric characteristics of complicated eyes divided by the type of flap complication.
Table 3.
Comparison between complicated and uncomplicated groups

Table 4.
Flap complications and its biometric characteristics
Relative risks for flap-related complications were 2.03 for the first LASIK surgery (CI 95% 0.64 to 6.48, P = 0.22) and 1.26 (CI 95% 0.43 to 3.69, P = 0.66) for the surgeon's first twenty flap dissections. Female gender presented a 2.2 (CI 95% 0.69 to 7.32, P = 0.17) relative risk for complications. Table 5 shows relative risks according to refractive status with no statistically significant results. Relative risks for other commonly known risk factors were obtained with no statistical significance [Table 6].
Table 5.
Relative risks according to refractive status

Table 6.
Relative risks for other factors

When complications presented after the surgeon's twentieth procedure, they occurred only in the left eye. Other characteristics such as pachymetry, keratometries, or refraction were within normal values and were not different in complicated or uncomplicated patients.
DISCUSSION
Following the introduction of LASIK, an increased prevalence of flap-related complications was documented among both the novice and the experienced ophthalmic surgeons.[5,6,7] Flap complications varied from 4.8% to 6.0% during the early learning curve which declined to 1% or less after the completion of more than 500 procedures.[8] In our study, there were 19 flap-related complications out of the 273 flap dissections involved (6.95%). This incidence compares favorably with those reported by other authors, which vary from 0.3-10%.[5,6,9,10,11,12,13] However, in most studies executed with trained LASIK surgeons, the rates are about 0.5-2%, indicating that residents in training present a higher complication rate. On the contrary, some authors proposed that lack of experience with LASIK surgery does not correlate with a lack of safety and efficacy.[14] Other studies have reported the incidence of some specific complications like incomplete flaps in the hand of inexperienced surgeons.[15] We decided to include information from the procedures of both the ophthalmology residents and the cornea fellows as in our academic center, some of the cornea fellows acquire their learning curve and perform their first procedures. We did not find difference between residents and novice cornea fellows. There was no objective result that contradicted to these findings.
Only keratometry values showed a statistically significant difference between the study groups. There were no significant differences between two groups in laterality (right or left eye), age, pachymetry findings, white-to-white distance, plate size used, preoperative visual acuity, or spherical equivalent refraction. Final visual acuity after rescheduling laser treatment was also similar between the complicated and uncomplicated groups.
In a study of 1019 eyes by Lin and Maloney,[7] 88 (8.6%) eyes had flap-related complications, but there was no loss of best-corrected visual acuity with proper management of complications. They concluded that flap complications decrease with the surgeon's experience. They also noted a significant learning curve in the use of microkeratome.
Although we found similar results to those reported in the literature, this paper shows that the first flap dissection involves a 2.0 relative risk of complication and that the first 20 flap dissections, which is the mean number of required flap creation for an ophthalmology resident at our institution, represent a 1.23 relative risk of complications during this step; however, these risk factors were not statistically significant. We also found that there was no significant relationship between free caps and flattest keratometries, and buttonholes with steepest keratometries.
These types of complications are a major cause of surgical suspension, and the incidence should be considered as part of the informed consent in training hospitals, although it does not seem to affect final visual outcome when the laser treatment is rescheduled.
With the increasing use of the femtosecond-assisted LASIK flaps, some concepts must be taken into consideration, and although these lasers are exceedingly safe, complications do still occur.[16] Suction loss may occur during flap creation for an improper technique in applying the suction ring or inadequate fixation, which can lead to an incomplete flap, but when it occurs with a femto-second microkeratome laser, the surgeon could proceed immediately and get satisfactory outcomes which may have implications in training hospitals for patient safety.[17] However, a retrospective analysis of flap complications using microkeratome or femtosecond laser indicated that the total complication rates between the 2 groups were similar (14.2% and 15.2%, respectively).[18]
We conclude that flap-related complications are a common intraoperative issue during LASIK surgery performed by in-training ophthalmologists. The surgeon's inexperience may impose a higher risk for flap-related complications than biometric parameters of the patient's eye. Flap complications do not seem to affect final visual outcome when the laser treatment is rescheduled.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Jacobs JM, Taravella MJ. Incidence of intraoperative flap complications in laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:23–28. doi: 10.1016/s0886-3350(01)01097-5. [DOI] [PubMed] [Google Scholar]
- 2.Tham VM, Maloney RK. Microkeratome complications of laser in situ keratomileusis. Ophthalmology. 2000;107:920–924. doi: 10.1016/s0161-6420(00)00004-x. [DOI] [PubMed] [Google Scholar]
- 3.Nakano K, Nakano E, Oliveira M, Portellinha W, Alvarenga L. Intraoperative microkeratome complications in 47,094 laser in situ keratomileusis surgeries. J Refract Surg. 2004;20(5 Suppl):S723–S726. doi: 10.3928/1081-597X-20040903-19. [DOI] [PubMed] [Google Scholar]
- 4.Sridhar MS, Rao SK, Vajpayee RB, Aasuri MK, Hannush S, Sinha R. Complications of laser in situ keratomileusis. Indian J Ophthalmol. 2002;50:265–282. [PubMed] [Google Scholar]
- 5.Gimbel HV, Basti S, Kaye GB, Ferensowicz M. Experience during the learning curve of laser in situ keratomileusis. J Cataract Refract Surg. 1996;22:542–550. doi: 10.1016/s0886-3350(96)80006-x. [DOI] [PubMed] [Google Scholar]
- 6.Gimbel HV, Penno EE, van Westenbrugge JA, Ferensowicz M, Furlong MT. Incidence and management of intraoperative and early postoperative complications in 1000 consecutive laser in situ keratomileusis cases. Ophthalmology. 1998;105:1839–1847. doi: 10.1016/s0161-6420(98)91026-0. [DOI] [PubMed] [Google Scholar]
- 7.Lin RT, Maloney RK. Flap complications associated with lamellar refractive surgery. Am J Ophthalmol. 1999;127:129–136. doi: 10.1016/s0002-9394(98)00320-1. [DOI] [PubMed] [Google Scholar]
- 8.Wagoner MD, Wickard JC, Wandling GR, Jr, Milder LC, Rauen MP, Kitzmann AS, et al. Initial resident refractive surgical experience: Outcomes of PRK and LASIK for myopia. J Refract Surg. 2011;27:181–188. doi: 10.3928/1081597X-20100521-02. [DOI] [PubMed] [Google Scholar]
- 9.Walker MB, Wilson SE. Lower intraoperative flap complication rate with the Hansatome microkeratome compared to the Automated Corneal Shaper. J Refract Surg. 2000;16:79–82. doi: 10.3928/1081-597X-20000101-11. [DOI] [PubMed] [Google Scholar]
- 10.Gimbel HV, van Westenbrugge JA, Penno EE, Ferensowicz M, Feinerman GA, Chen R. Simultaneous bilateral laser in situ keratomileusis: Safety and efficacy. Ophthalmology. 1999;106:1461–1467. doi: 10.1016/s0161-6420(99)90438-4. [DOI] [PubMed] [Google Scholar]
- 11.Waring GO, 3rd, Carr JD, Stulting RD, Thompson KP, Wiley W. Prospective randomized comparison of simultaneous and sequential bilateral laser in situ keratomileusis for the correction of myopia. Ophthalmology. 1999;106:732–738. doi: 10.1016/S0161-6420(99)90158-6. [DOI] [PubMed] [Google Scholar]
- 12.Stulting RD, Carr JD, Thompson KP, Waring GO, 3rd, Wiley WM, Walker JG. Complications of laser in situ keratomileusis for the correction of myopia. Ophthalmology. 1999;106:13–20. doi: 10.1016/S0161-6420(99)90000-3. [DOI] [PubMed] [Google Scholar]
- 13.Farah SG, Azar DT, Gurdal C, Wong J. Laser in situ keratomileusis: Literature review of a developing technique. J Cataract Refract Surg. 1998;24:989–1006. doi: 10.1016/s0886-3350(98)80056-4. [DOI] [PubMed] [Google Scholar]
- 14.LeBoyer RM, Deutsch TA, Rubenstein JB. Results of resident-performed laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:771–775. doi: 10.1016/j.jcrs.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 15.Ito M, Hori-Komai Y, Toda I, Tsubota K. Risk factors and retreatment results of intraoperative flap complications in LASIK. J Cataract Refract Surg. 2004;30:1240–1247. doi: 10.1016/j.jcrs.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 16.Shah DN, Melki S. Complications of femtosecond-assisted laser in situ keratomileusis flaps. Semin Ophthalmol. 2014;29:363–375. doi: 10.3109/08820538.2014.959194. [DOI] [PubMed] [Google Scholar]
- 17.Santhiago MR, Kara-Junior N, Waring GO., 4th Microkeratome versus femtosecond flaps: Accuracy and complications. Curr Opin Ophthalmol. 2014;25:270–274. doi: 10.1097/ICU.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 18.Moshirfar M, Gardiner JP, Schliesser JA, Espandar L, Feiz V, Mifflin MD, et al. Laser in situ keratomileusis flap complications using mechanical microkeratome versus femtosecond laser: Retrospective comparison. J Cataract Refract Surg. 2010;36:1925–1933. doi: 10.1016/j.jcrs.2010.05.027. [DOI] [PubMed] [Google Scholar]


