Abstract
Purpose:
The purpose of this study was to evaluate the results of a teamwork revision endoscopic dacryocystorhinostomy (DCR) in eyes with previously failed external DCR.
Methods:
This retrospective study was performed on 50 failed external DCR subjects who underwent a teamwork revision endoscopic DCR by an ophthalmologist and an otolaryngologist. Paranasal sinus CT scanning was performed for each patient before the revision surgery. During surgery, any abnormal tissue noticed before silicone intubation was sent for pathological evaluation.
Results:
Endoscopic revision DCR was performed on 50 failed external DCR subjects with one-year follow-up. Of these, 31 were female (62%). The age range of the subjects was 18-88 years (mean: 59.98 years). Sinus CT showed at least one abnormality in 94% of cases. Revision endoscopy showed septal deviation (66%), scar formation (32%), ostium problems (28%), and sump syndrome (6%). Pathologic and clinical findings showed that chronic inflammation had a significant association with scar tissue and septal synechia (P = 0.001 and 0.008, respectively). At the final follow-up, anatomical and functional success was achieved in 45 out of 50 (90%) of subjects.
Conclusion:
Endoscopic revision DCR when performed as cooperation of otolaryngologists and ophthalmologists may help resolve the endonasal problems and increase the success rate.
Key words: Endoscopic Dacryocystorhinostomy, External Dacryocystorhinostomy, Failure Rate, Success Rate
INTRODUCTION
Dacryocystorhinostomy (DCR) is the standard method of surgery for the treatment of NLDO.[1] In DCR surgery, an artificial and shorter lacrimal drainage pathway is produced through the lacrimal bone into the nasal cavity, in order to establish a permanent drainage route to bypass the previously obstructed drainage system.[2] External DCR and the endoscopic method are two widely accepted surgical techniques for the treatment of NLDO.[3] In external DCR, a cutaneous incision followed by tissue dissection allows access to the lacrimal sac. The procedure has become widely accepted due to its high success rates and relatively low complications.[1] Interestingly, the endonasal approach was first introduced by Caldwell in 1893 before the external approach introduced by Toti in 1904.[4] At that time, endonasal techniques were limited due to lack of proper instruments needed to access the surgical site.[5] Gradually, with development of the modern instrumentation and techniques since 1990, endonasal techniques gained popularity for both primary and failed revision NLDOs. The main advantages of endonasal approach include avoiding external approach problems such as skin scarring, infection, ectropion, and medial canthal tendon disruption.[6] Other advantages include good visualization, better localization and estimation of the rhinostomy site and size.[5] Good visualization helps prevent the disruption of angular vessels, periorbital hemorrhage, epistaxis, disruption of medial canthal tendon, tear pump dysfunction and CSF leakage.[7]
Although external DCR surgery is the gold standard method for NLDOs compared with the other methods,[8] its failure rate is still about 4-13%.[9] The major causes of failure in external DCR are canalicular obstruction and closed osteotomy, caused by cicatricial tissues.[10] Other causes of failure include middle turbinate abnormalities (concha bullosa, lateralization, hypertrophy), ostium problems (closed, small or too high ostium), mucosal abnormalities (intranasal adhesions, contact granuloma, scar formation, rhinosinusitis, and pouch formation known as sump syndrome), nasal wall abnormalities (preceding maxillofacial trauma, ipsilateral septal deviation, lateral nasal wall scarring) and aggernasi over pneumatization which partially overlaps the medial aspect of the lacrimal fossa, resulting in a DCR ostium located within the ethmoidal air cells.[11,12,13,14]
Anatomically, nasolacrimal systems are the common border of ophthalmology and otorhinolaryngology.[15] Observations show that most of the causes of failure are located within the nasal cavity, which are outside the ophthalmologists' territory. Nasal endoscopy, simultaneously helps treat the septal deviations, synechia formation or middle turbinate compression over the fistula.[16] Therefore; surgical teamwork may help increase the success rate in treatment of failed external DCRs. In this study we evaluate the most important findings in patients with external DCR failures and the success rate of teamwork endoscopic revision in failed external DCR.
METHODS
This retrospective study was conducted between the years of 2010 and 2014 in Shahid Mustafa Khomeini hospital, Tehran, Iran. The ethical committee of Shahed University approved the study and the authors followed the ethical principles advised in declaration of Helsinki.
Fifty patients who had failed external DCR and had the symptom of failure (epiphora) up to one year after the surgery were included in this study. All patients gave informed consent and were examined by an ophthalmologist. Anatomical obstruction was defined if tearing continued with a closed irrigation test. Functional obstruction was defined if tearing continued despite an open irrigation test. Functional and anatomical success was defined if complete cessation of the tearing was ensued after surgical interventions.[10] Regardless of results of the patients' previous scintigraphy, all the functional cases were excluded from the study by an open irrigation test. Before planning the endoscopic surgery coronal and axial para-nasal sinus CT scans were performed. All the surgeries were performed by two surgeons, an otolaryngologist and an ophthalmologist. Under general anesthesia, the nasal cavity was assessed by 0 and 30 degree nasal endoscopes. After infiltration of lateral nasal wall with epinephrine 1:100,000 and lidocaine 1%, the mucosal flap was prepared with a sickle knife under a 0 degree endoscope, and then a 30 degree endoscopic lens was used for better visualization of the lateral wall. Then the excess mucosa and scar tissues were carefully removed by a special punch and then sent for pathologic investigations in order to discover any correlation between clinical findings and chronic inflammation or fibrotic or granulation tissues formation not visible with direct observation. The excess bone was meticulously removed with drill and chisel. Under close observation of an ophthalmologist, the desired rhinostomy was performed by applying gentle pressure over the globe and probing, to locate the incision site over the bulged remnants of the lacrimal sac. Silicone intubation was inserted by the ophthalmologist and kept for 3 months. The process was difficult in some cases due to previous manipulations. Associated intranasal problems such as nasal septal deviation, concha bullosa, and synechia that caused the recurrence of epiphora were corrected during the same session. After the operation, eye drop and oral antibiotics as well as saline solution for nasal irrigation were prescribed. In order to prevent the formation of granulation tissue, the nasal cavity was cleansed with irrigation of normal saline and suction of the fluid weekly for two months. The patients' statuses were monitored for up to 12 months. Patients were also examined by an ophthalmologist at their 1st week, 1st month, 3rd month, 6th month and 1st year after the surgery. At these visits, the patients were asked about presence of epiphora or any discharge and their rate of satisfaction of the surgery. Findings were analyzed by SPSS software version 16 (SPSS Inc., Chicago, Illinois, USA).
RESULTS
Fifty eyes of 50 patients with failed external DCR complaining of epiphora were included in this study. Of these, 31 (62%) were female. The age range of patients was between 18 and 88 years (mean: 59.98 years). The mean interval of primary operation to revision surgery was 3 years. There were not any important intra- or post-operative complications except mild to moderate hemorrhage.
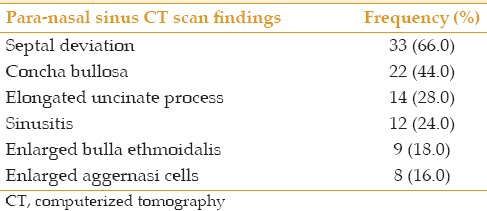
Para-nasal sinus CT showed at least one abnormality in 94% of patients. The most common findings in para-nasal sinus CT scan were septal deviation (66%), concha bullosa (44%), elongated uncinate process (28%), and sinusitis (24%), [Table 1].
Table 1.
Frequency of para-nasal sinus computerized tomography scan findings in failed external dacryocystorhinostomy
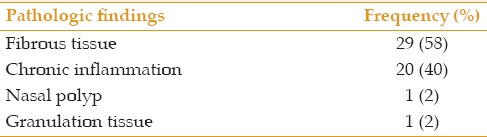
The most prevalent findings in the endoscopic revision before incision were septal deviation (66%), enlarged middle turbinate (48%), and septal adhesion to the lateral nasal wall (48%), [Table 2]. However, the most common findings after surgical incision were scar formation (32%), ostium problems (28%), underlying adhesion (16%), and sump syndrome (3%), [Table 3]. The most common pathologic findings were fibrosis (58%) and chronic inflammation (40%), [Table 4]. Pathological and clinical findings showed that chronic inflammation had a significant relation with scar tissue formation and septal synechia to the lateral nasal wall (P = 0.001 and 0.008, respectively).
Table 2.
Frequency of endoscopic findings before incision in failed external dacryocystorhinostomy
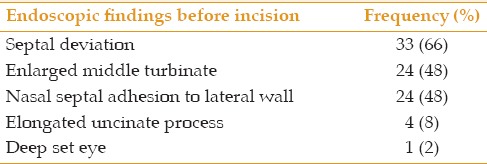
Table 3.
Frequency of endoscopic findings after incision in failed external dacryocystorhinostomy
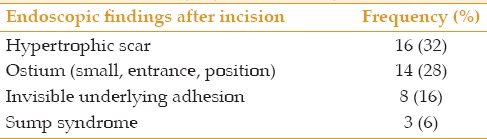
Table 4.
Frequency of pathologic findings in failed external dacryocystorhinostomy
Most of the patients had some degrees of epiphora during the first week after the endoscopic surgery which gradually stopped within the following 6 months. The rate of satisfaction at the postoperative periods gradually increased and peaked at month 6. Considering the exclusion of the functional cases before the study as mentioned in the Methods, there were no functional obstruction and the final success rate was measured as high as 90% after surgical intervention.
DISCUSSION
Present study showed that, overall, the most common problems associated with previous external DCR failures include nasal septal deviation (66%), fibrous tissue formation (58%), enlarged middle turbinate, septal adhesion to lateral nasal wall (48%), concha bullosa (44%) ostium problems (28%) and sump syndrome (3%). Functional cases were excluded by irrigation tests before inclusion and none had functional epiphora after their one year follow-up.
Common causes of failure reported in other studies include improper osteotomy, ostial stenosis, synechia, septal deviation, middle turbinate hypertrophy with synechia, incomplete removal of the lacrimal bone and granulation tissue.[11,14,17,18,19]
Using a 30 degree endoscopic lens, as well as the presence of an expert otolaryngologist helps better visualization of intranasal abnormalities. In this study the most common endoscopic finding was hypertrophic scar followed by ostium problems such as ostium size, ostium entrance into the ethmoidal air cells, and high ostium position. One of the findings accompanied with the other causes of failure in external DCR, is the sac remnants. In some cases, the inferior part of the lacrimal sac remnants may form a pouch-like space with fluid retention, known as sump syndrome.[20] Sump syndrome was identified many years ago.[21,22] Difficult osteotomy over the triangular edge of the maxillary bone adjacent to the inferior part of the lacrimal sac prevents the surgeon from performing an open handed osteotomy in external DCR.[23] Therefore, the inferior part of the lacrimal sac may remain like a fluid-retaining pouch and may cause unwanted sump syndrome. One may presume that as the ostium size gets larger, the probability of sump syndrome becomes smaller, for example, in primary DCR.[24] However, sump syndrome may occur independently from ostium size, and even larger ostium sizes may be accompanied by sump syndrome.[25]
Because of the high number of variables involved in external DCR failures, it is difficult to determine the role of each one independently.[26] Deep set eyes and deep nasal roots may force the surgeons to do osteotomy too deeply and directly enter the ethmoidal air cells. We encountered this problem while trying to pass the probe in one of our revision cases. None of the studies in literature have reported such dilemma. Saving a mucosal flap to cover the bare bone and anastomosis between the nasal and lacrimal mucosa are other challenging issues. In this experiment, the mucosal flap was raised and saved to cover the bare bone at the end of the procedure. Similarly, some studies have reported acceptable success rates while preserving the mucosal flap in primary surgery.[23,27]
The success rate in most of the revision endoscopic DCR studies have been reported to be between 75% to 85%.[14,28,29,30,31] The success rate in the current study however was revealed to be 90%. A few studies with a smaller sample size have reported success rates up to 94%, but considering the functional epiphora, the true success rate in these studies were still below 90%.[17,32] We simultaneously corrected all obstructive lesions, such as septal deviation, abnormal middle turbinate and uncinate processes, as is recommended in another similar study.[33] Pathologic evaluation from the site of surgery has rarely been investigated in the literature. In this study, excess tissues were sent for pathologic investigation. We found that chronic inflammatory reactions had a significant association with clinically visible scar tissues and nasal septal synechia. The lateral nasal wall should be protected carefully during the surgery because this location has critical importance due to the entrance of the common canaliculus and the ostium into the nasal cavity.
Silicone intubation is another controversy. In this study, silicone intubation was inserted by the ophthalmologist and kept for 3 months. Since postoperative adhesion is another reason for failure,[30] and since silicone intubation prevents adhesion, it may help enhance the patency of the lacrimal drainage system. Therefore, besides teamwork and cooperation, our other recommendations that may enhance success rate include: Preoperative paranasal sinus CT scanning and otolaryngologist consultation, good visualization, simultaneous surgical treatment of additional obstructive lesions, silicone intubation, avoiding manipulation of the lateral nasal wall of the sac, saving a mucosal flap over the bared bone, and finally, postoperative regular and frequent endoscopic cleaning of nasal cavity and removal of all granulation tissues.
In summary, simultaneous teamwork in performing revision endoscopic DCR for failed external DCR cases may not only help decrease ocular and endonasal complications but can also enhance the surgical success rate.
Financial Support and Sponsorship
Shahed University, Tehran, Iran.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgment
The authors kindly thank Shahed University, Tehran, Iran, for the spiritual and financial supports.
REFERENCES
- 1.Karim R, Ghabrial R, Lynch T, Tang B. A comparison of external and endoscopic endonasal dacryocystorhinostomy for acquired nasolacrimal duct obstruction. Clin Ophthalmol. 2011;5:979–989. doi: 10.2147/OPTH.S19455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sinha V, Gupta D, Prajapati B, More Y, Khandelwal P, Singh SN, et al. Endoscopic dacryocystorhinostomy with conventional instruments: Results and advantages over external dacryocystorhinostomy. Indian J Otolaryngol Head Neck Surg. 2008;60:207–209. doi: 10.1007/s12070-008-0078-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cokkeser Y, Evereklioglu C, Er H. Comparative external versus endoscopic dacryocystorhinostomy: Results in 115 patients (130 eyes) Otolaryngol Head Neck Surg. 2000;123:488–491. doi: 10.1067/mhn.2000.105470. [DOI] [PubMed] [Google Scholar]
- 4.Onerci M. Dacryocystorhinostomy. Diagnosis and treatment of nasolacrimal canal obstructions. Rhinology. 2002;40:49–65. [PubMed] [Google Scholar]
- 5.Metson R. The endoscopic approach for revision dacryocystorhinostomy. Laryngoscope. 1990;100:1344–1347. doi: 10.1288/00005537-199012000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Preechawai P. Results of nonendoscopic endonasal dacryocystorhinostomy. Clin Ophthalmol. 2012;6:1297–1301. doi: 10.2147/OPTH.S33030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.David S, Raju R, Job A, Richard J. A comparative study of external and endoscopic endonasal dacryocystorhinostomy – A preliminary report. Indian J Otolaryngol Head Neck Surg. 1999;52:37–39. doi: 10.1007/BF02996430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaman M, Babar TF, Saeed N. A review of 120 cases of dacryocystorhinostomies (Dupuy Dutemps and Bourguet technique) J Ayub Med Coll Abbottabad. 2003;15:10–12. [PubMed] [Google Scholar]
- 9.Tarbet KJ, Custer PL. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 1995;102:1065–1070. doi: 10.1016/s0161-6420(95)30910-4. [DOI] [PubMed] [Google Scholar]
- 10.Ali MJ, Psaltis AJ, Wormald PJ. Dacryocystorhinostomy ostium: Parameters to evaluate and DCR ostium scoring. Clin Ophthalmol. 2014;8:2491–2499. doi: 10.2147/OPTH.S73998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elmorsy SM, Fayk HM. Nasal endoscopic assessment of failure after external dacryocystorhinostomy. Orbit. 2010;29:197–201. doi: 10.3109/01676831003669961. [DOI] [PubMed] [Google Scholar]
- 12.Hull S, Lalchan SA, Olver JM. Success rates in powered endonasal revision surgery for failed dacryocystorhinostomy in a tertiary referral center. Ophthal Plast Reconstr Surg. 2013;29:267–271. doi: 10.1097/IOP.0b013e3182916556. [DOI] [PubMed] [Google Scholar]
- 13.Liang J, Hur K, Merbs SL, Lane AP. Surgical and anatomic considerations in endoscopic revision of failed external dacryocystorhinostomy. Otolaryngol Head Neck Surg. 2014;150:901–905. doi: 10.1177/0194599814524700. [DOI] [PubMed] [Google Scholar]
- 14.Paik JS, Cho WK, Yang SW. Comparison of endoscopic revision for failed primary external versus endoscopic dacryocystorhinostomy. Clin Experiment Ophthalmol. 2013;41:116–121. doi: 10.1111/j.1442-9071.2012.02844.x. [DOI] [PubMed] [Google Scholar]
- 15.Paulsen F. The human nasolacrimal ducts. Adv Anat Embryol Cell Biol. 2003;170:III. [PubMed] [Google Scholar]
- 16.Allen KM, Berlin AJ, Levine HL. Intranasal endoscopic analysis of dacrocystorhinostomy failure. Ophthal Plast Reconstr Surg. 1988;4:143–145. doi: 10.1097/00002341-198804030-00004. [DOI] [PubMed] [Google Scholar]
- 17.Choussy O, Retout A, Marie JP, Cozlean A, Dehesdin D. Endoscopic revision of external dacryocystorhinostomy failure. Rhinology. 2010;48:104–107. doi: 10.4193/Rhin08.115. [DOI] [PubMed] [Google Scholar]
- 18.Demarco R, Strose A, Araújo M, Valera FC, Moribe I, Anselmo-Lima WT. Endoscopic revision of external dacryocystorhinostomy. Otolaryngol Head Neck Surg. 2007;137:497–499. doi: 10.1016/j.otohns.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 19.Konuk O, Kurtulmusoglu M, Knatova Z, Unal M. Unsuccessful lacrimal surgery: Causative factors and results of surgical management in a tertiary referral center. Ophthalmologica. 2010;224:361–366. doi: 10.1159/000313818. [DOI] [PubMed] [Google Scholar]
- 20.Fayet B, Racy E, Assouline M. Complications of standardized endonasal dacryocystorhinostomy with unciformectomy. Ophthalmology. 2004;111:837–845. doi: 10.1016/j.ophtha.2003.08.023. [DOI] [PubMed] [Google Scholar]
- 21.Migliori ME. Endoscopic evaluation and management of the lacrimal sump syndrome. Ophthal Plast Reconstr Surg. 1997;13:281–284. doi: 10.1097/00002341-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Jordan DR, McDonald H. Failed dacryocystorhinostomy: The sump syndrome. Ophthalmic Surg. 1993;24:692–693. [PubMed] [Google Scholar]
- 23.Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. Br J Ophthalmol. 2003;87:43–47. doi: 10.1136/bjo.87.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balikoglu-Yilmaz M, Yilmaz T, Taskin U, Taskapili M, Akcay M, Oktay MF, et al. Prospective comparison of 3 dacryocystorhinostomy surgeries: External versus endoscopic versus transcanalicular multidiode laser. Ophthal Plast Reconstr Surg. 2015;31:13–8. doi: 10.1097/IOP.0000000000000159. [DOI] [PubMed] [Google Scholar]
- 25.Qian Z, Tu Y, Xiao T, Wu W. A lacrimal sump syndrome with a large intranasal ostium. J Craniofac Surg. 2015;26:e386–8. doi: 10.1097/SCS.0000000000001864. [DOI] [PubMed] [Google Scholar]
- 26.Lee J, Choi SY, Lee H, Chang M, Park M, Baek S. The clinical effectiveness of transcanalicular diode laser-assisted revision surgery for failed endoscopic endonasal dacryocystorhinostomy. Br J Ophthalmol. 2015;99:1130–1133. doi: 10.1136/bjophthalmol-2014-306270. [DOI] [PubMed] [Google Scholar]
- 27.Kansu L, Aydin E, Avci S, Kal A, Gedik S. Comparison of surgical outcomes of endonasal dacryocystorhinostomy with or without mucosal flaps. Auris Nasus Larynx. 2009;36:555–559. doi: 10.1016/j.anl.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 28.El-Guindy A, Dorgham A, Ghoraba M. Endoscopic revision surgery for recurrent epiphora occurring after external dacryocystorhinostomy. Ann Otol Rhinol Laryngol. 2000;109:425–30. doi: 10.1177/000348940010900414. [DOI] [PubMed] [Google Scholar]
- 29.Korkut AY, Teker AM, Yazici MZ, Kahya V, Gedikli O, Kayhan FT. Surgical outcomes of primary and revision endoscopic dacryocystorhinostomy. J Craniofac Surg. 2010;21:1706–1708. doi: 10.1097/SCS.0b013e3181f3c6c1. [DOI] [PubMed] [Google Scholar]
- 30.Korkut AY, Teker AM, Ozsutcu M, Askiner O, Gedikli O. A comparison of endonasal with external dacryocystorhinostomy in revision cases. Eur Arch Otorhinolaryngol. 2011;268:377–381. doi: 10.1007/s00405-010-1339-3. [DOI] [PubMed] [Google Scholar]
- 31.Tsirbas A, Davis G, Wormald PJ. Revision dacryocystorhinostomy: A comparison of endoscopic and external techniques. Am J Rhinol. 2005;19:322–325. [PubMed] [Google Scholar]
- 32.Ali MJ, Psaltis AJ, Wormald PJ. Long-term outcomes in revision powered endoscopic dacryocystorhinostomy. Int Forum Allergy Rhinol. 2014;4:1016–1019. doi: 10.1002/alr.21398. [DOI] [PubMed] [Google Scholar]
- 33.Fayet B, Katowitz WR, Racy E, Ruban JM, Katowitz JA. Endoscopic dacryocystorhinostomy: The keys to surgical success. Ophthal Plast Reconstr Surg. 2014;30:69–71. doi: 10.1097/IOP.0000000000000038. [DOI] [PubMed] [Google Scholar]


