Abstract
Scleral buckling is a highly successful technique for the repair of rhegmatogenous retinal detachment that requires intra-operative examination of the retina and treatment of retinal breaks via indirect ophthalmoscopy. Data suggest that scleral buckling likely results in improved outcomes for many patients but is declining in popularity, perhaps because of significant advances in vitrectomy instrumentation and visualization systems. Emerging data suggest that chandelier-assisted scleral buckling is safe and has many potential advantages over traditional buckling techniques. By combining traditional scleral buckling with contemporary vitreoretinal visualization techniques, chandelier-assistance may increase the popularity of scleral buckling to treat primary rhegmatogenous retinal detachment for surgeons of the next generation, maintaining buckling as an option for appropriate patients in the future.
Key words: Chandelier, Chandelier-Assisted Scleral Buckle, Chandelier-Buckle, Endoilluminator-Assisted Scleral Buckle, Scleral Buckle, Scleral Buckling
INTRODUCTION
Since its introduction in the 1950s [1,2] scleral buckling has proven a highly successful technique for the repair of rhegmatogenous retinal detachment (RD). Although the technique of scleral buckling has developed since its inception, the contemporary procedure still requires intra-operative examination of the retina and treatment of retinal breaks via indirect ophthalmoscopy.
Despite significant advances in vitrectomy surgery, scleral buckling still likely results in improved outcomes for many patients with RD. The “Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment” (SPR) study is the only randomized, prospective, multi-center study that has compared scleral buckling to pars plana vitrectomy (PPV) for primary RD repair.[3] That study included European surgeons who had performed at least 100 scleral buckling procedures and 100 pars plana vitrectomies as primary surgeon prior to initiation of the study. The SPR study enrolled 681 patients with RD from 25 centers across 5 European countries and randomized them to undergo scleral buckling or PPV with or without concomitant scleral buckling (at the preference of the treating surgeon). Two sub-groups of patients were analyzed based on the status of their crystalline lens, either phakic or pseudophakic and aphakic. In the phakic sub-group, patients randomized to scleral buckling achieved improved mean visual acuity (−0.71 vs. −0.56 logMAR), less progression of cataract and required significantly less “retina affecting procedures” post-operatively compared to those randomized to PPV. In the pseudophakic/aphakic sub-group, patients randomized to PPV achieved similar visual acuity results but had a higher re-attachment rate and required less “retina affecting procedures” post-operatively compared to those randomized to scleral buckling. Additional retrospective data from a patient cohort of over 7500 patients corroborates the finding that scleral buckling may be superior for phakic patients.[4] Indeed, conventional wisdom also suggests that scleral buckling is the preferred method to treat young patients with attached hyaloid (especially myopes) or those with a retinal dialysis, as detaching the hyaloid in such patients may be technically challenging and may induce additional retinal tears. Scleral buckles are also conventionally preferred in patients who are phakic with an inferior detachment as the crystalline lens may result in inadequate shaving of the peripheral hyaloid with a smaller postoperative intraocular gas tamponade. In addition, scleral buckling has been shown to be a significantly less expensive option for retinal detachment repair in phakic patients.[5]
DECLINING POPULARITY OF SCLERAL BUCKLING
Despite the aforementioned advantages and favorable data regarding scleral buckling, recent polls suggest that the use of this procedure to treat RD is declining. The most recent American Society of Retinal Specialists (ASRS) Preferences and Trends Survey (PAT) asked surgeons: “In what percentage of cases of primary rhegmatogenous retinal detachment do you place a scleral buckle?” – 28.7% of US surgeons and 39.5% of European surgeons answered “0-10%.”[6] This trend may be in part due to advancement in vitrectomy surgery including improved platforms, instrumentation and wide field viewing systems that utilize the operating microscope. As a result of the declining popularity of the scleral buckle, vitreoretinal surgery trainees may feel less comfortable with scleral buckling compared to previous generations.
ENDOILLUMINATION-ASSISTED SCLERAL BUCKLING
All surgeons in the abovementioned studies performed scleral buckling using indirect ophthalmoscopy to identify and treat retinal tears in the traditional method (unless performing concomitantly with pars plana vitrectomy). One reason that scleral buckling may perform worse in patients with pseudo-phakia or aphakia is because of impaired visualization with indirect ophthalmoscopy compared to those who are phakic. Indeed, subsequent analysis of the SPR data suggested that the presence of a posterior YAG capsulotomy (suggesting a history of, and likely residual media opacity) predicted poorer outcomes for scleral buckling.[7] Endoilluminator-assisted scleral buckling may improve on this limitation.
Trans-scleral fiber-optic-assisted scleral buckling was first described for the repair of RD in 2012 by Aras et al in Turkey.[8] This initial method used a torpedo-style chandelier light source through an un-cannulated sclerotomy. This permitted identification and treatment of retinal breaks using a non-contact wide-angle PPV-style viewing apparatus (BIOM, OCULUS Surgical Inc., Port St. Lucie, FL, USA). The report evaluated outcomes in 16 consecutive eyes of 16 patients. Of these, four eyes were pseudophakic, the remainder were phakic and 10 were macula-off. Overall, retinal re-attachment was achieved in 13 eyes, 3 requiring additional PPV. One patient experienced perforation of the sclera during cryopexy and underwent immediate PPV with silicone oil tamponade.
In 2013, Kita et al described an updated technique for endoilluminator-assisted scleral buckling that is now more commonly used. Instead of an un-cannulated torpedo-style light source, Kita et al described using a 25-gauge fiber-optic chandelier light source through a standard trans-scleral cannula (Alcon, Forth Worth, TX, USA) and a non-contact wide-field viewing system (Resight, Carl Zeiss Meditec AG, Jena, Germany) to identify and treat retinal breaks (cryotherapy) and drain subretinal fluid. The patient described in the report was a young myope in whom careful pre-operative examination could not identify a break and, following chandelier-buckle, he experienced persistent retinal reattachment with no complications.[9]
Later in 2013, Nam et al[10] and Nagpal et al[11] published case series regarding a similar technique using a 25-gauge chandelier but a contact (as opposed to non-contact) viewing system, with good results. Nam et al used a contact wide-field lens (Mini Quad; Volk, Mentor, OH, USA) to treat primary RD in 12 patients. Although Nam et al do not describe their patients or success rate in this report; they note that no sclerotomy required a suture and that no eye experienced crystalline lens damage from the chandelier. Nagpal et al described 10 patients who underwent chandelier-assisted identification and cryotherapy of retinal breaks and standard external subretinal fluid drainage with a cut-down, nine of whom experienced persistent re-attachment and none had a chandelier-associated complication.
In 2014, Gogia et al[12] described a series of 25 phakic and pseudophakic patients with RD in whom a retinal break could not be identified pre-operatively who were treated with a 25-gauge “self-retaining endoilluminator” and a “wide-angle viewing system.” In two cases, an intraoperative search could not identify any breaks and pars plana vitrectomy was performed instead. In the 23 eyes successfully treated with endoilluminator-assisted scleral buckling, 22 (95%) achieved persistent re-attachment after a single procedure and no patient experienced complications associated with the use of the endoilluminator.
In 2015, Yokoyama et al[13] used a non-contact viewing system and twin un-cannulated 27-gauge chandeliers (Eckard TwinLight Chandelier; DORC International, Zuidland, the Netherlands) to perform scleral buckling on 3 children with RD. The authors described removing the light sources after identifying and treating the retinal breaks, before suturing scleral explants or performing external subretinal fluid drainage. They would replace them if necessary after these steps to check the fundus. In two patients, retinal breaks were detected intraoperatively that were not found pre-operatively. All three patients experienced persistent retinal re-attachment, improvement in visual acuity, and no complications.
Later in 2015, Chhablani and Balakrishnan [14] described using a chandelier and wide-field viewing system successfully to assist in subretinal fluid drainage for a patient with a chronic exudative retinal detachment. Later that year, that group compared a group of patients who underwent chandelier-assisted scleral buckling with non-contact wide-angle viewing to a group that underwent scleral buckling with the indirect ophthalmoscope (14 patients in each group).[15] In summary, analysis of their data showed no chandelier-associated complications and a similarly high primary reattachment rate in both groups. Furthermore, duration of surgery was significantly shorter in the chandelier-assisted group (by approximately 20 minutes) that may be explained by avoiding the step of placing and removing of the indirect ophthalmoscope (which is often repeated several times throughout the procedure) and by improved visualization that may expedite steps such as cryotherapy.
The largest series of chandelier-assisted scleral buckling was published by Imai et al in 2015.[16] They used a 25g cannulated chandelier and non-contact wide-field viewing system to identify and treat retinal breaks (and often drained subretinal fluid under direct visualization) in 79 patients with primary uncomplicated RD, the vast majority of whom were phakic. Overall, 92.4% of patients had primary success. Intraoperative complications associated with the use of the chandelier system occurred in two eyes. One patient experienced a new retinal break as the chandelier was removed from the cannula which was identified and treated immediately. Another patient had lens touch by the tip of the endoilluminating chandelier during cryopexy but no cataract developed over the follow-up period.
In 2015, our group described the first series of patients in the United States undergoing chandelier buckling [17,18] which are further described below. In 2016, Haug et al[19] described seven patients from the United States undergoing endoillluminator-assisted scleral buckling. In this series, patients underwent cryotherapy of retinal breaks using indirect ophthalmoscopy; however, a trans-scleral cannula and chandelier were placed for wide-angle viewing assisted subretinal fluid needle drainage. Six patients experienced persistent re-attachment following the initial surgery and one required subsequent pars plana vitrectomy to attain retinal re-attachment. No patients developed complications from the use of chandelier.
POTENTIAL ADVANTAGES OF CHANDELIER-ASSISTED SCLERAL BUCKLING OVER TRADITIONAL TECHNIQUES
Chandelier-assistance obviates the need for indirect ophthalmoscopy and capitalizes on the advantages provided by the operating microscope and contemporary wide-angle viewing systems such as an improved view of the peripheral retina with oblique lighting to perhaps improve identification of peripheral breaks. Indeed, several of the aforementioned studies report the identification of retinal breaks intraoperatively that were not seen on pre-operative examination. Wide-field viewing may also make subretinal fluid needle drainage safer as it may decrease the risk of losing the view of the needle, which may occur with indirect ophthalmoscopy. Moreover, chandelier-buckling permits the ability for all team members to share the same surgical view, which improves both surgeon-team communication and teaching as the instructor may directly supervise trainees during cryotherapy and subretinal fluid drainage. It is possible that trainees may experience greater success with their initial scleral buckling procedures when using a chandelier, as improved visualization may reduce the chance of missing retinal breaks (considered the most common cause of primary failure) and permit less extensive cryotherapy. Indeed, trainees may end up feeling more comfortable with chandelier-buckles compared to traditional techniques and gain more experience in scleral buckling after personally performing fewer procedures. In addition, chandelier-assisted scleral buckling permits standard microscope-facilitated recording of the important surgical steps of this procedure, which also facilitates dissemination of scleral buckling techniques. Many authors of the published literature regarding this technique also mention the improved ergonomics of using the operating microscope to perform examination and treatment of retinal breaks instead of indirect ophthalmoscopy. Indeed, neck and back injury is distressingly common among vitreoretinal surgeons.[20]
DUKE SERIES OF CHANDELIER-ASSISTED SCLERAL BUCKLING
Our group presented the first series of patients in the United States undergoing chandelier-buckling,[17,18] which is described in more detail below. This was a retrospective cohort study of patients undergoing repair of primary rhegmatogenous retinal detachment with chandelier-assisted scleral buckling alone between 1st February 2013 and 28th September 2014 at the Duke Eye Center with at least 3 months of follow-up. Patients were excluded if retinal detachment was secondary to trauma. Data collection included preoperative visual acuity, status of the crystalline lens, RD involvement of the central macula, location and size of breaks, presence of proliferative vitreoretinopathy, location and type of chandelier and buckles used, type of gas tamponade, and the postoperative course including visual acuity, reattachment rate and complications. Institutional Review Board approval of this study was obtained prior to data collection.
RESULTS
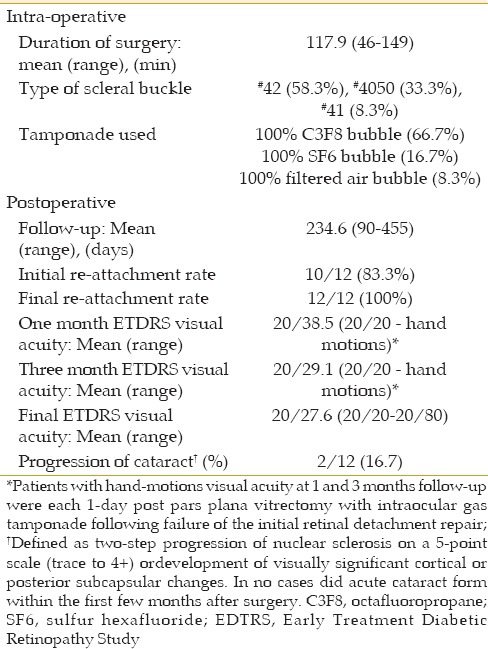
Twelve patients from three primary surgeons (TM, PM, and PH) met inclusion criteria. A chandelier buckle procedure was chosen in all cases when the surgeon determined that a primary scleral buckling would otherwise be a good option to treat the retinal detachment. Although experienced in traditional primary scleral buckling techniques, no surgeon in this series had performed a chandelier-assisted scleral buckling procedure prior to 2/1/2013. The pre-operative characteristics of patients are shown in Table 1. The intra-and post-operative data of patients are shown in Table 2. No eye exhibited proliferative vitreoretinopathy grade C or higher pre-operatively nor developed this complication post-operatively. There was also no appreciable change in intraocular pressure post-operatively.
Table 1.
Patient demographics/preoperative characteristics
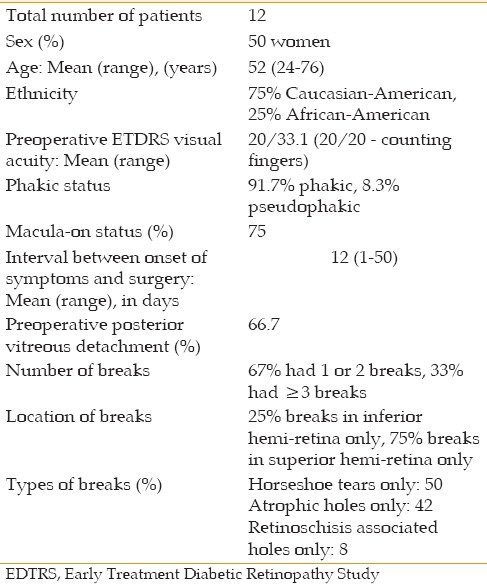
Table 2.
Intra-operative and postoperative data
For all patients, chandelier-assisted scleral buckling surgery consisted of a 360° conjunctival peritomy, isolation and looping of all rectus muscles, placement of a trans-scleral (pars plana) cannula to house a chandelier fiber-optic endo-illumination system, use of the operating microscope with wide-angle visualization to identify and treat breaks using external cryotherapy (instead of indirect ophthalmoscopy), suturing of a silicone encircling band (Dutch Ophthalmics, Exeter, New Hampshire, USA) to support all retinal breaks, anterior chamber paracentesis when needed, intraocular gas injection for tamponade, removal of the trans-scleral cannula/chandelier system, suturing of sclerotomy (ies), and conjunctival closure. In one case, subretinal fluid drainage via a short 26-gauge needle was performed instead of gas tamponade. In brief, any surgical step of a traditional scleral buckle that required indirect ophthalmoscopy was replaced by visualization through the operating microscope and wide-field viewing system with chandelier illumination [Supplemental Video 1]. In eleven eyes, a single valveless pars plana 25-gauge cannula/chandelier system was used (Alcon, Forth Worth, Texas, USA) and in one eye a dual 29-gauge chandelier/cannula system was used (Synergetics, O'Fallon, Missouri, USA). The chandeliers were placed 180 degrees away from the primary break in seven eyes, 90 degrees away in four eyes, and adjacent to the primary break in one eye. Wide-angle visualization through the microscope was achieved by using the non-contact BIOM (Oculus, Port St. Lucie, Florida, USA) or contact Volk system (Volk Optical Inc., Mentor, OH, USA). Intraoperative scleral depressed examination was performed using a scleral depressor while holding the rectus sutures for counter-traction.
In cases that the 25-gauge chandelier system was used, the light was removed and the cannula plugged after cryotherapy and external marking of the break which allowed better access to the scleral surface for suturing of the buckle and prevented accidental disconnection of the chandelier from the cannula. Paracentesis was always done after pulling up the buckle and after intravitreal gas injection to normalize the intraocular pressure before disconnecting the chandelier (or removing the cannula plug) to prevent vitreous prolapse. Any vitreous wick seen after removal of the cannula was trimmed with scissors. In all cases, the sclerotomy was sutured immediately after removal of the cannula.
Overall, ten of twelve patients achieved primary re-attachment following chandelier-assisted scleral buckling. One eye did not achieve primary re-attachment and another re-detached before the three-month follow-up time point. In neither case were new retinal breaks found near the area of previous chandelier placement. In the first patient, significant vitreous opacity likely limited an adequate view of retinal breaks intra-operatively. In the second patient, a small hole was found at edge of a cryotherapy scar at the time of subsequent pars plana vitrectomy. Both of these patients achieved re-attachment following a single PPV. In a third patient, a deep suture pass occurred during the initial scleral buckling procedure which caused a retinal break and limited vitreous hemorrhage and required intravitreal air injection to maintain intraocular pressure; however, this eye achieved persistent re-attachment following initial surgery. This complication was not attributed to the use of a chandelier. No focal lens changes attributed to the chandelier were seen in any patients. Furthermore, use of the chandelier did not seem to result in an unduly long duration of surgery [Table 2].
DISCUSSION OF DUKE SERIES
All new procedures have a learning curve. However, a reasonable primary success rate was achieved in our series with chandelier-assisted scleral buckling. In our experience, the most salient benefit of the use of chandelier lighting and wide-field viewing system was superior identification of breaks compared to indirect ophthalmoscopy given the improved view and oblique lighting [Supplemental Video 1].
Based on our experience, certain techniques appear important for surgeons during their initial experience with chandelier-assisted scleral buckling. If using a standard valveless trans-scleral cannula, it is important that this cannula be plugged when not filled by the chandelier to avoid vitreous from being inadvertently expelled. When using the Alcon 25-gauge valveless cannula, the plug that is included with the Alcon 20 to 25-gauge adaptor has worked well for our patients. Plugging is especially important when the intraocular pressure is higher such as after pulling up the buckle and after injecting gas into the vitreous cavity; for the same reason, care must also be taken to reduce intraocular pressure (i.e. with an anterior chamber paracentesis) before removing the plug or cannula, and to use scissors to cut any vitreous wick that presents. Some published series of this technique describe suturing of the sclerotomy in all cases, whereas others do so only for select cases. We suture the sclerotomy immediately when the cannula is removed in all patients. We have also noted that performing the scleral depressed examination under the operating microscope in these cases has a learning curve. Vitreoretinal surgeons are accustomed to performing a scleral depressed exam under a wide-field viewing situation during PPV, when eye movement may be controlled with instruments within sclerotomies or cannulas. However, with chandelier-buckles the sutures around the muscles must be used to control eye movement, which do not provide the same degree of control. We recommend that surgeons unfamiliar with this technique initially select patients with one or two retinal breaks that can be seen readily in pre-operative examination. We believe that as the surgeon gains experience, cases similar to those in our series with more difficult to detect breaks may be performed.
LOOKING FORWARD
Although the popularity of the scleral buckle is declining, conventional wisdom and a significant amount of data suggest that it results in improved outcomes for many patients. The reason for the decline of scleral buckling is unclear, but may be secondary to the improved visualization afforded by contemporary wide-field viewing systems used during PPV. However, these visualization advantages may be gained during scleral buckling by the addition of a chandelier, which emerging data suggest is safe. By combining traditional scleral buckling with contemporary vitreoretinal visualization techniques (that were not available when the original surgery was introduced), chandelier-buckling may improve the popularity of buckling to treat primary rhegmatogenous retinal detachment. This may particularly be important in the training of the next generation of vitreoretinal surgeons so that the art of scleral buckling, which has many indications and advantages in selected situations, can survive.
Financial Support and Sponsorship
This work was supported by the Heed Ophthalmic Foundation and was presented at the American Society for Retinal Specialists Annual Meeting in Vienna, Austria in July, 2015.
Conflicts of Interest
There are no conflicts of interest.
Video Available at: www.jovr.org
REFERENCES
- 1.Custodis E. Treatment of retinal detachment by circumscribed diathermal coagulation and by scleral depression in the area of tear caused by imbedding of a plastic implant. Klin Monbl Augenheilkd Augenarztl Fortbild. 1956;129:476–495. [PubMed] [Google Scholar]
- 2.Schepens CL, Okamura ID, Brockhurst RJ. The scleral buckling procedures. I. Surgical techniques and management. AMA Arch Ophthalmol. 1957;58:797–811. doi: 10.1001/archopht.1957.00940010819003. [DOI] [PubMed] [Google Scholar]
- 3.Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, Foerster MH. Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: A prospective randomized multicenter clinical study. Ophthalmology. 2007;114:2142–2154. doi: 10.1016/j.ophtha.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Adelman RA, Parnes AJ, Ducournau D. European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Strategy for the management of uncomplicated retinal detachments: The European vitreo-retinal society retinal detachment study report 1. Ophthalmology. 2013;120:1804–1808. doi: 10.1016/j.ophtha.2013.01.070. [DOI] [PubMed] [Google Scholar]
- 5.Seider MI, Naseri A, Stewart JM. Cost comparison of scleral buckle versus vitrectomy for rhegmatogenous retinal detachment repair. Am J Ophthalmol. 2013;156:661–666. doi: 10.1016/j.ajo.2013.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stone TW. ASRS 2015 Preferences and Trends Membership Survey. Chicago, IL: American Society of Retina Specialists; 2015. [Google Scholar]
- 7.Feltgen N, Heimann H, Hoerauf H, Walter P, Hilgers RD, Heussen N. Writing Group for the SPR Study Investigators*. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR study): Risk assessment of anatomical outcome. SPR study report no 7. Acta Ophthalmol. 2013;91:282–287. doi: 10.1111/j.1755-3768.2011.02344.x. [DOI] [PubMed] [Google Scholar]
- 8.Aras C, Ucar D, Koytak A, Yetik H. Scleral buckling with a non-contact wide-angle viewing system. Ophthalmologica. 2012;227:107–110. doi: 10.1159/000333101. [DOI] [PubMed] [Google Scholar]
- 9.Kita M, Fujii Y, Kawagoe N, Hama S. Scleral buckling with a noncontact wide-angle viewing system in the management of retinal detachment with undetected retinal break: A case report. Clin Ophthalmol. 2013;7:587–589. doi: 10.2147/OPTH.S42923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nam KY, Kim WJ, Jo YJ, Kim JY. Scleral buckling technique using a 25-gauge chandelier endoilluminator. Retina. 2013;33:880–882. doi: 10.1097/IAE.0b013e31827e2602. [DOI] [PubMed] [Google Scholar]
- 11.Nagpal M, Bhardwaj S, Mehrotra N. Scleral buckling for rhegmatogenous retinal detachment using vitrectomy-based visualization systems and chandelier illumination. Asia Pac J Ophthalmol (Phila) 2013;2:165–168. doi: 10.1097/APO.0b013e3182929b75. [DOI] [PubMed] [Google Scholar]
- 12.Gogia V, Venkatesh P, Gupta S, Kakkar A, Garg S. Endoilluminator-assisted scleral buckling: Our results. Indian J Ophthalmol. 2014;62:893–894. doi: 10.4103/0301-4738.141068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yokoyama T, Kanbayashi K, Yamaguchi T. Scleral buckling procedure with chandelier illumination for pediatric rhegmatogenous retinal detachment. Clin Ophthalmol. 2015;9:169–173. doi: 10.2147/OPTH.S75648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chhablani J, Balakrishnan D. Chandelier-assisted external drainage of subretinal fluid. Retin Cases Brief Rep. 2015;9:223–225. doi: 10.1097/ICB.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 15.Narayanan R, Tyagi M, Hussein A, Chhablani J, Apte RS. Scleral buckling with wide-angled endoillumination as a surgical educational tool. Retina. 2016;36:830–833. doi: 10.1097/IAE.0000000000000792. [DOI] [PubMed] [Google Scholar]
- 16.Imai H, Tagami M, Azumi A. Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25 G chandelier endoilluminator. Clin Ophthalmol. 2015;9:2103–2107. doi: 10.2147/OPTH.S91339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seider M, Nomides R, Hahn P, Mruthyunjaya P, Mahmoud T. Chandelier-assisted Scleral Buckling for Repair of Primary Rhegmatogenous Retinal Detachment: Initial US Experience. American Society of Retinal Specialists Annual Meeting, Vienna; July, 2015. [Google Scholar]
- 18.Nomides R, Seider M, Mahmoud T. Chandelier-assisted scleral buckling. Retina. 2015:30–2. [Google Scholar]
- 19.Haug SJ, Jumper JM, Johnson RN, McDonald HR, Fu AD. Chandelier-assisted external subretinal fluid drainage in primary scleral buckling for treatment of rhegmatogenous retinal detachment. Retina. 2016;36:203–205. doi: 10.1097/IAE.0000000000000820. [DOI] [PubMed] [Google Scholar]
- 20.Mehta S, Hubbard GB., 3rd Avoiding neck strain in vitreoretinal surgery: An ergonomic approach to indirect ophthalmoscopy and laser photocoagulation. Retina. 2013;33:439–441. doi: 10.1097/IAE.0b013e318276cbca. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


