Abstract
Purpose:
To report a case of post laser in situ keratomileusis (LASIK), nebulomacular corneal opacity following a trauma induced flap dehiscence and was managed with superficial anterior lamellar keratoplasty (SALK).
Case Report:
A 32-year-old female underwent LASIK 2.5 years back, with a postoperative unaided visual acuity (VA) of 6/6 in both eyes. She was involved in a road traffic accident and sustained blunt trauma to the right eye 5 months before. At the time of presentation, the VA was 1/60 in the right eye. Slit lamp examination revealed flap dehiscence, stromal scar and descemet folds in that eye. There was a small macular scar in the parafoveal area due to a resolved Berlin's edema. SALK was performed in the affected eye. Unaided VA of 6/36 was noted on post- operative day 1. After 4 weeks of SALK surgery, best corrected VA was 6/24.
Conclusion:
This case highlights that flap adhesions are not very strong even years after LASIK and SALK may be an effective treatment option for post refractive surgery corneal opacities.
Key words: Descemet Folds, Flap Dehiscence, Laser in situ Keratomileusis, Superficial Anterior Lamellar Keratoplasty
INTRODUCTION
Post laser in situ keratomileusis (LASIK) traumatic flap displacement is a known complication occurring in 1% to 2% of cases within the first 24 hours after surgery.[1,2] Late flap dislocations, occurring after postoperative week 1, have also been reported.[3] Herein, we report a patient who experienced a post LASIK flap dehiscence and developed descemet folds and stromal scarring following a blunt trauma 2 years after an uneventful LASIK surgery. The patient's corneal problem was managed with superficial anterior lamellar keratoplasty (SALK).
CASE REPORT
A 32-year-old woman with a history of LASIK presented with a gradual painless reduction of vision in her right eye after a blunt trauma to the same eye in a road traffic accident five months before. LASIK had been done in both eyes 2.5 years earlier for a myopic refractive error of −6.00 diopters (D) with the reported post LASIK unaided visual acuity (VA) of 6/6 in both eyes. At the presentation, VA was 1/60 and 6/6 in the right and left eyes, respectively. Slit lamp examination revealed flap dehiscence, stromal scarring, and descemet folds with scarring in the right eye which had been caused by the flap dehiscence at the time of accident [Figure 1]. There was a small macular scar in the parafoveal area due to the resolved Berlin's edema. Because of late presentation, flap repositioning was not a treatment option; therefore the affected eye underwent SALK Postoperatively, the patient received moxifloxacin hydrochloride 0.5% and prednisolone acetate 1% eye drops three times daily, and carboxymethylcellulose 0.5% eye drops four times daily for 6 weeks. Bandage contact lens was removed four days after surgery. Small amount of glue was cleared from the interface at the postoperative week 3. Uncorrected VA was 6/36 on postoperative day 1 [Figure 2] and the best corrected VA (BCVA) was 6/24 four weeks postoperatively [Figure 3]. The reason for suboptimal vision was the presence of macular scar. This patient maintained the same vision with a 1.5-year follow up with no signs of epithelial ingrowth or graft dehiscence.
Figure 1.
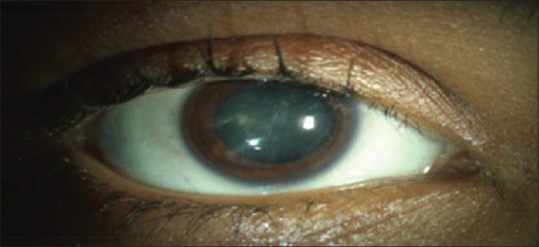
Flap dislocation with macrostriae. Preoperative clinical picture.
Figure 2.
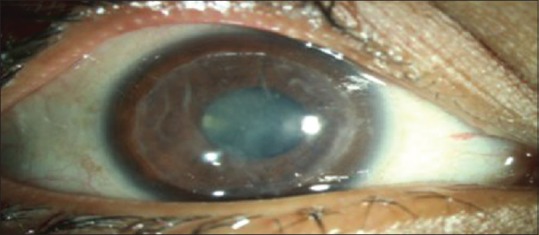
Post-operative day one after superficial anterior lamellar keratoplasty (SALK).
Figure 3.
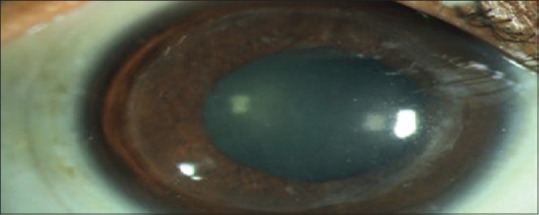
Post-operative four weeks after superficial anterior lamellar keratoplasty (SALK).
Surgical Technique
Anterior segment optical coherence tomography (Brand name, company, city, country) was used to determine the depth of scarring (154 μm). Accordingly, dissection was performed at the depth of 160 μm with the help of microkeratome, which was determined by intraoperative pachymetry (Corneo-Gage Plus; Sonogage, Inc., Cleveland, Ohio, USA). To perform SALK, demarcation, separation and dissection of previous plane beneath the flap were performed using LASIK spatula and Sinskey hook: The flap was removed after freeing nasal, temporal and central parts sequentially and dissection was done cautiously in the scarred area.
At the completion of dissection, interface bed which was clear was thoroughly washed to avoid any epithelial ingrowth in future. Donor tissue was then cut using an automated lamellar microkeratome and artificial anterior chamber (ALTK; automated lamellar therapeutic keratoplasty system, Moria, Paris, France). The microkeratome head size was 200 μm which was the smallest available. Donor tissue was punched with an 8-mm disposal trephine. Donor anterior lamella was then put on the host dissected area with the help of fibrin glue applied on the periphery as well as in the center. A bandage contact lens was placed and one drop of moxifloxacin hydrochloride 0.5% eye drops was instilled.
DISCUSSION
Early and late traumatic flap displacement after LASIK due to blunt or sharp trauma has previously been reported.[3] Philipp et al[4] analyzed post lasik corneas and found that there was minimal increased staining of the dermatan sulfate proteoglycan in the stroma which was adjacent to the lamellar flap. Few fiber crossings between the flap and residual stroma were observed. These findings indicate weak adhesions between the flap and the stroma which is in contrast to the previous belief that flap is resistant to dislocation because of the progressive fibrosis of flap taking place over time. Few studies conducted on rabbit models to demonstrate the corneal healing pattern post LASIK showed that healing process only occurs at the periphery of the flap and not at the center.[5] This mechanism is beneficial for the patient as it causes less visual axis scarring and is helpful to the surgeon as well, if flap lift is required for any future enhancement surgery.[5] However, flap displacement is always a complication of trivial ocular trauma.
When patients present early after traumatic flap dehiscence, flap lifting and refloatation with thorough scraping of the undersurface of the flap to remove the epithelial cells from the interface are the treatment of choice. Few studies have reported the occurrence of epithelial ingrowth after replacement of a displaced lenticule after LASIK.[6] Exact cause cannot be traced in such situations, but plausible mechanisms are imprecise alignment of the flap edge with the corneal bed and irregularity of the two interface surfaces. In our patient, we had thoroughly washed the interface and used glue to attach lenticule as an adjunctive to prevent epithelial ingrowth.
Anderson and Hardten study demonstrated the mechanical barrier function of the glue, which may help by preventing epithelial migration and growth underneath the flap till it heals.[7] The two main drawbacks of the glue are its cost and the stromal interface haze usually being resolved 3 to 4 weeks after surgery. An experimental study done by Cho et al compared the difference in wound repair in lamellar grafts using tissue adhesives versus sutures and concluded that for lamellar keratoplasty, human fibrin tissue adhesives can be used as an alternative to sutures.[8]
In summary, SALK is a viable and effective option for the management of the refractive surgery induced nebulomacular corneal opacities associated with anterior stromal scaring.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Lin RT, Maloney RK. Flap complications associated with lamellar refractive surgery. Am J Ophthalmol. 1999;127:129–136. doi: 10.1016/s0002-9394(98)00320-1. [DOI] [PubMed] [Google Scholar]
- 2.Gimbel HV, Penno EE, van Westenbrugge JA, Ferensowicz M, Furlong MT. Incidence and management of intraoperative and early postoperative complications in 1000 consecutive laser in situ keratomileusis cases. Ophthalmology. 1998;105:1839–1847. doi: 10.1016/s0161-6420(98)91026-0. [DOI] [PubMed] [Google Scholar]
- 3.Cheng AC, Rao SK, Leung GY, Young AL, Lam DS. Late traumatic flap dislocations after LASIK. J Refract Surg. 2006;22:500–504. doi: 10.3928/1081-597X-20060501-13. [DOI] [PubMed] [Google Scholar]
- 4.Philipp WE, Speicher L, Göttinger W. Histological and immunohistochemical findings after laser in situ keratomileusis in human corneas. J Cataract Refract Surg. 2003;29:808–820. doi: 10.1016/s0886-3350(02)01611-5. [DOI] [PubMed] [Google Scholar]
- 5.Pérez-Santonja JJ, Linna TU, Tervo KM, Sakla HF, Alió y Sanz JL, Tervo TM. Corneal wound healing after laser in situ keratomileusis in rabbits. J Refract Surg. 1998;14:602–609. doi: 10.3928/1081-597X-19981101-06. [DOI] [PubMed] [Google Scholar]
- 6.Kim EK, Choe CM, Kang SJ, Kim HB. Management of detached lenticule after in situ keratomileusis. J Refract Surg. 1996;12:175–179. doi: 10.3928/1081-597X-19960101-30. [DOI] [PubMed] [Google Scholar]
- 7.Anderson NJ, Hardten DR. Fibrin glue for the prevention of epithelial ingrowth after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29:1425–1429. doi: 10.1016/s0886-3350(02)01989-2. [DOI] [PubMed] [Google Scholar]
- 8.Cho SY, Kim MS, Oh SJ, Chung SK. Comparison of synthetic glues and 10-0 nylon in rabbit lamellar keratoplasty. Cornea. 2013;32:1265–1268. doi: 10.1097/ICO.0b013e31829a3760. [DOI] [PubMed] [Google Scholar]


