Abstract
Purpose:
The purpose of this study is to evaluate the longevity of reduced disclusion time in treating and removing myofascial pain dysfunction symptoms following the T-Scan-based, immediate complete anterior guidance development (ICAGD) coronoplasty. This measured occlusal adjustment has been shown to reduce the muscle hyperactivity of myofascial pain.
Methods:
Myofascial pain symptomatic patients were recruited as per the diagnostic criteria for temporomandibular disorders (TMDs), including the clinical protocol and assessment instruments outlined by the international RDC/TMD consortium network (version: January 20, 2014) to assess the efficacy of reduced disclusion time in left and right lateral excursions to resolve the myofascial pain symptoms. As per the inclusion and exclusion criteria, 100 cases were treated with ICAGD in three visits, each 1 week apart. Recall disclusion time measurements were recorded every 3 months over 3 years. The RDC/TMD questionnaire was used for symptom assessment at every recall visit. ICAGD brought pretreatment prolonged disclusion time down to <0.4 s, as quantified from T-Scan force and time data records, while the subjects were assessed for symptom relief. The Wilcoxon signed-rank test was used for statistical analysis (P < 0.05).
Results:
Changes in the intensity of many symptoms from reducing the disclusion time to <0.4 s were statistically significant from treatment day 1, and onward through the 3-year period of observation (P < 0.05).
Conclusion:
The results indicate that ICAGD reduces the musculoskeletal symptoms of myofascial pain, such that this methodology increases clinical therapeutic success.
Keywords: Disclusion time, Myofascialimmediate complete anterior guidance development, myofascial pain, temporomandibular disorders
INTRODUCTION
In spite of its diverse etiology, occlusal instability has been long considered an important etiological factor in myofascial pain. Occlusal interferences can induce tooth pain, mobility, as well as masticatory muscle hyperactivity, although some papers do not indicate that occlusal interferences are the cause of chronic dysfunctional problems.[1,2] Occlusal equilibration had been advocated by numerous authors as a successful treatment modality for myofascial pain,[3,4,5,6,7] while others have shown improvements in symptoms by mock occlusal equilibration, as well as actual occlusal adjustments.[8,9,10,11,12] However, some authors contend that myofascial pain is a stress-related disorder not brought on by occlusal factors.[13,14,15]
One of the most common causes of chronic oro-facial pain is myofascial pain (Edmiston and Larsen, 1978). It is a complex disease situation that includes regions of pain called trigger points, which are taut bands of skeletal muscle, tendons, or ligaments near the temporomandibular joint (TMJ) region and jaw muscles but can refer pain to distant areas.[14,16] Patients present with variable symptoms such as localized pain in the TMJ, TMJ sounds (clicking or crepitation), restricted jaw opening, disturbances in their chewing pattern, and locking of the jaw. Tenderness in the jaw muscles can also lead to a diffuse headache, neck ache, earache, dizziness, tinnitus, and hearing loss.
An alternative, measurement-driven, computer-guided occlusal adjustment procedure whose primary therapeutic goal of measurably decreasing the time required for all molars and premolars to disclude from each other in fractions of seconds during mandibular excursions, (known as disclusion time reduction; <0.4 s/excursion), has been shown to be successful in treating myofascial pain patients.[17,18,19,20,21,22,23] Shortening the disclusion time can be accomplished with the immediate complete anterior guidance development (ICAGD) enameloplasty or by an additional procedure performed with the aid of computerized occlusal analysis (T-Scan III, Tekscan Inc., S. Boston, MA, USA) that records real-time measurements of excursive movements as dynamic force movies.[17]
A study performed on 25 subjects divided into treated(received ICAGD), untreated, and control group that received mock ICAGD, compared the results of disclusion time reduction and myofascial pain symptom remissions from pre- to post-ICAGD. Only the treated group showed a statistically significant reduction in disclusion time, as well as statistically significant reductions in the intensity and frequency of many myofascial pain-dysfunction syndrome symptoms.[22] The disclusion time is an entity measured by the T-Scan occlusal analysis system and its force movie software.[19,23,24,25,26,27,28]
The ICAGD procedure was only possible to perform because of the time measurement capability of T-Scan III occlusal analysis system (T-Scan versions I, II, and III, Tekscan Inc., S. Boston, MA, USA).[18,29] ICAGD is a computer guided, measured coronoplasty based on specific time-based numerical occlusal endpoints that verify it was performed properly.[19] Bilateral contact simultaneity can also be clinically established through measurement with the T-Scan of the closure occlusal contact sequence. This ensures no one region of the dental arch contacts too early (forced to absorb excess early stress) or too late (unable to assist the other regions in force dissipation). Both precision force and time control is afforded to the operator through measurement with the T-Scan high-definition recording sensor, which replaces the “hit or miss” operator subjective interpretation of colored ink marks on teeth.[30,31]
This study was undertaken to evaluate the possibility of successfully treating myofascial pain symptoms using a measurement-driven, diagnostic treatment protocol based upon the T-Scan-guided ICAGD coronoplasty. The therapeutic treatment goal was to reduce prolonged posterior disclusion time to <0.4 s in both the right and left mandibular excursions.
METHODS
One hundred myofascial pain symptomatic patients, who met the below inclusion criteria [Chart 1], were recruited to assess the efficacy of reduced disclusion time in the left and right lateral excursions. The diagnostic criteria for temporomandibular disorders (TMDs), including the clinical protocol and assessment instruments outlined by the international RDC/TMD consortium network (version: January 20, 2014), was utilized for diagnosing and categorizing the study subjects.
Chart 1.
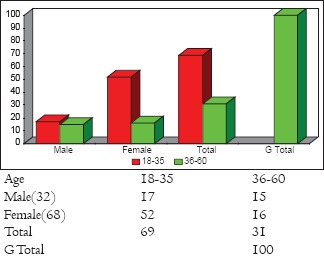
Age and sex distribution
Inclusion criteria
Patients who demonstrated myofascial pain symptoms that presented with Angle's Class I maxillomandibular relations
Patients who demonstrated myofascial pain symptoms that presented with Angle's Class III maxillomandibular relations but had shallow anterior guidance contacts
Patients who demonstrated myofascial pain symptoms that presented with Angle's Class II (Division 1) maxillomandibular relations that had definitive anterior guidance contacts.
Exclusion criteria
Patients who demonstrated myofascial pain symptoms that presented with Angle's Class II (Division 2) malocclusion, with no anterior guidance contacts
Patients who demonstrated myofascial pain symptoms having severe anterior open occlusion. These patients were not considered for the ICAGD protocol, as the amount of tooth adjustment required to effectively shorten the disclusion time would likely be excessive
Patients who demonstrated myofascial pain symptoms that had prior disc re-capture surgery.
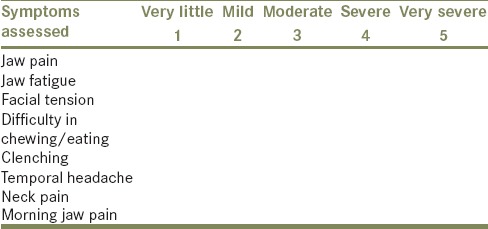
Symptom assessment questionnaire
At each study visit, subjects were asked to answer a diagnostic criteria symptom questionnaire that used an ordinal number scale to describe the current status of their condition [Table 1]. The ordinal scale ranged from 0 to 5 to describe symptom severity (0 - no symptoms, 1 - very little, 2 - mild, 3 - moderate, 4 - severe, and 5 - very severe). The common musculoskeletal symptoms that were graded were morning jaw pain, jaw fatigue, facial tension, difficulty in eating or chewing, clenching difficulty, temporal headaches, and neck pain. From study visit to study visit, the subjects were not allowed to review their previous answers, to avoid bias in their differing questionnaire responses. The 100 treated subjects' questionnaire scores were computed by means with standard deviations, and a standard error of the mean (SEM). The SEM is the standard deviation of the error in the sample mean relative to the true mean, since the sample mean is an unbiased estimator. Mean and mean differences, medians, and Z and P values were all computed using a one-way analysis of variance (SAS AppDev, Studio 4.4, North Carolina 27513, USA). Z scores are measures of the standard deviation, and both Z and P value statistics relate the standard deviations with probabilities that allow significance and confidence to be attached to Z scores and P values. Since the mean and median of different groups of individuals were compared, a nonparametric statistic (the Wilcoxon signed-ranks test) was used for statistical analysis.
Table 1.
Symptoms assessment ordinal scale
The included subjects then underwent a T-Scan III digital occlusal analysis. This quantified their closure occlusal forces against time, and measured their right and left excursive disclusion times, such that pretreatment disclusion time values in seconds, were obtained for both right and left excursions.
Measurement of disclusion time
Before commencing any treatment, the force movie mode of the T-Scan was utilized to measure and calculate the pretreatment disclusion times in seconds.[1] Each excursive movement (right and left) was recorded 3 times to obtain a mean disclusion time values for each excursion per subject. These pretreatment values were later compared with the posttreatment disclusion time recordings made on day 1, day 7, 1 month, 6 months, 12 months, 18 months, 24 months, 30 months, and 36 months from the initial disclusion time recordings [Tables 2–4].
Table 2.
Analysis of disclusion time means (in seconds) pre to post treatment for left lateral excursion
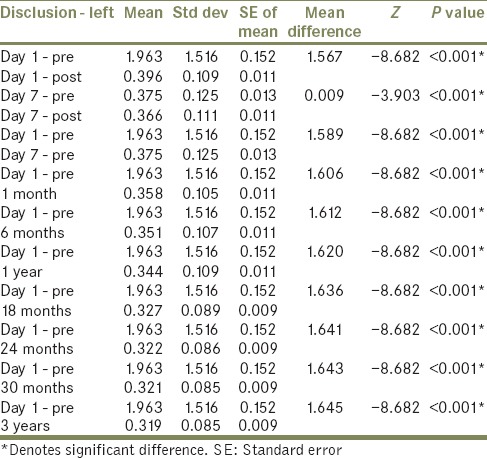
Table 4.
Analysis of combined disclusion time means (in seconds) pre to post treatment for left and right lateral excursions
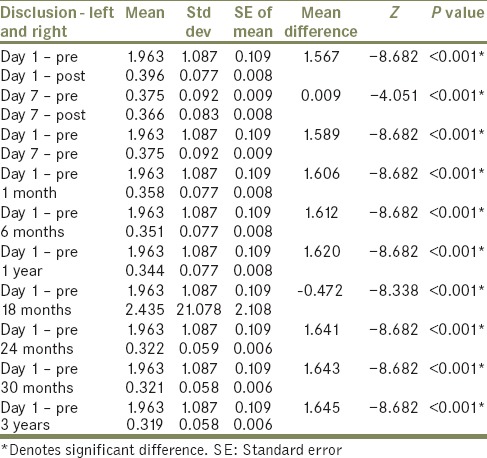
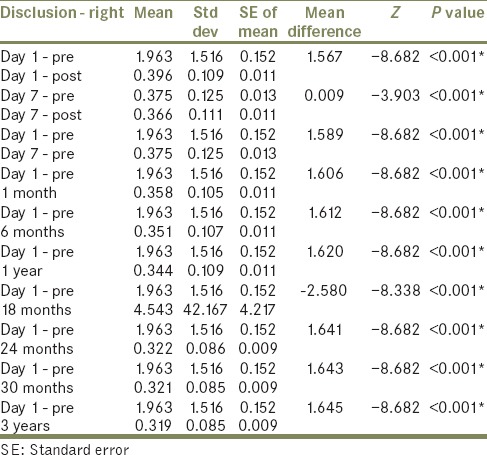
Table 3.
Analysis of disclusion time means (in seconds) pre to post treatment for Right Lateral excursion
ICAGD was performed in two phases as described by Kerstein.[19] Subsequent to the Phase 1 and Phase 2 correction visits, each subject was recalled at 1-month, 6-month, 12-month, 18-month, 24-month, 30-month, and 36-month intervals for observation of changes in their disclusion times and in their pretreatment symptoms.
Statistical analysis
The Wilcoxon signed-rank test was used for statistical analysis of the disclusion time means per study visit.
The null hypothesis—there would be no significant difference in the disclusion times (in seconds) between the pretreatment and post-ICAGD treatment disclusion time intervals (μ1 = μ2).
The alternate hypothesis—there would be a significant difference in the disclusion times (in seconds) between the pretreatment and posttreatment disclusion time intervals (μ1 ≠ μ2).
The level of significance of α =0.05, where if the compared P values differed with the level of significance of P < 0.05, the null hypothesis would be rejected, and the alternate hypothesis would be accepted. If P ≥ 0.05, the null hypothesis would then be accepted. Computations of the P values for disclusion time were based on the data reported in Tables 2–4.
RESULTS
Analysis of disclusion time means of the left lateral excursion and the right lateral excursion, pre- to post-treatment for the entire group of 100 treated subjects
The disclusion time changes from pre- to post-treatment were analyzed at various time intervals within the 36-month period of observation, and there were statistically significant differences found between the pre- and all post-treatment intervals (P < 0.5) [Tables 2–4]. The mean difference was greater following treatment on day 1 (both right and left excursions) and was reduced on day 7, and consistently reduced values of disclusion time were measured following ICAGD, where posttreatment disclusion time means per recall visit were <0.4 s duration.
The separate left and right excursive disclusion time values showed greater mean differences on day 1 pre- to post-treatment of 1.567. Thereafter, mean differences with day 1 pretreatment values, and the subsequent recall visits also showed greater mean differences that remained fairly constant through the 36-month period of observation [Table 2, the mean difference range: 1.589–1.645]. This mean difference showed that there was a statistically significant reductions of the separate left and right disclusion time from the ICAGD treatment.
Combined right and left excursions disclusion time means analysis
The disclusion time means for combined left and right excursions were also statistically significantly different from pre- to post-treatment (P < 0.001) [Table 4]. Additionally, there were statistically significant changes for the 36-month period of observation (P < 0.001). The mean differences of the combined right and left disclusion times compared to day 1 pretreatment values were greater and consistent for all recall visits [Table 4, mean differences range: 1.589–1.645].
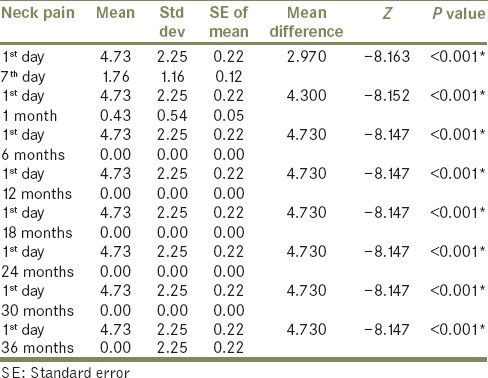
Intensity of muscular discomforts
An ordinal scale questionnaire was used to assess the severity of various TMD symptoms where the median values of the scores for the entire group were determined for statistical comparison. The changes in mean intensity and frequency of all myofascial pain symptoms studied was found to be statistically significant between day 1 and day 7 (P < 0.05), day 1 and 1 month (P < 0.05), day 1 and 6 months (P < 0.05), day 1 and 12 months (P < 0.05), day 1 and 18 months (P < 0.05), day 1 and 24 months (P < 0.05), day 1 and 30 months (P < 0.05), as well as day 1 and 36 months (P < 0.05) [Tables 5–12].
Table 5.
Comparison of mean intensity of ‘jaw pain’ from pre treatment day 1 to other time intervals
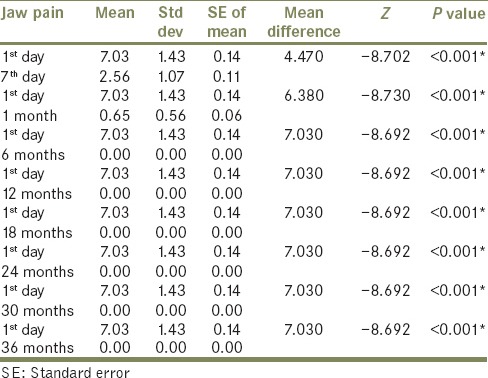
Table 12.
Comparison of mean intensity values of ‘morning jaw pain’ from pretreatment day 1 to other time intervals
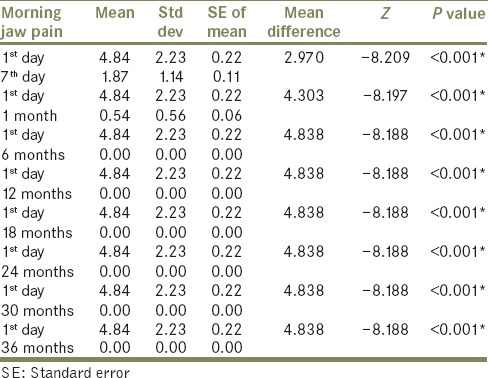
Table 6.
Comparison of mean intensity of ‘jaw fatigue’ from pre treatment day 1 to other time intervals
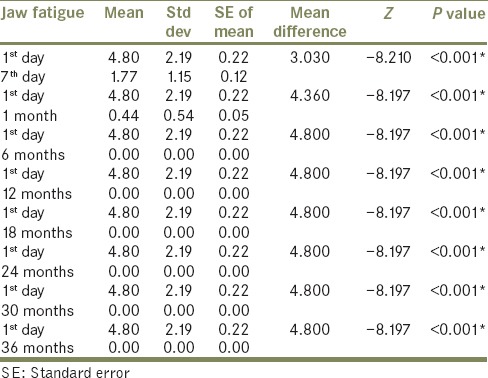
Table 7.
Comparison of mean intensity of ‘facial tension’ from pre treatment Day 1 to other time intervals
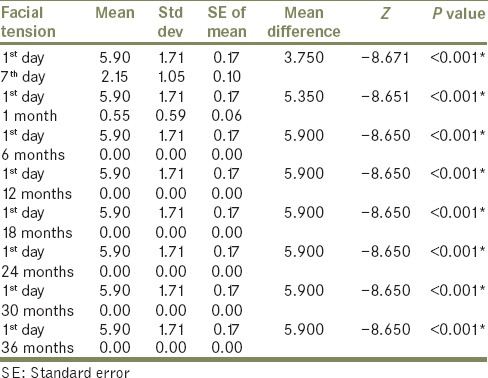
Table 8.
Comparison of mean intensity of ‘difficulty in chewing/eating’ from pretreatment day 1 to other time intervals
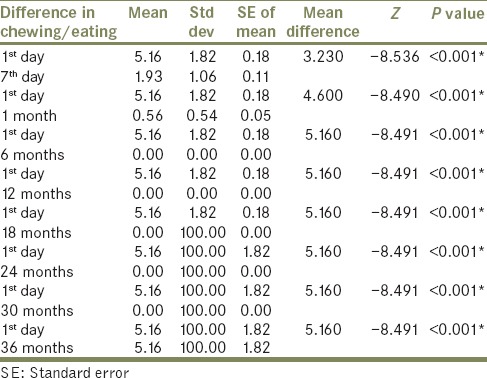
Table 9.
Comparison of mean intensity of ‘clenching’ from pre treatment day 1 to other time intervals
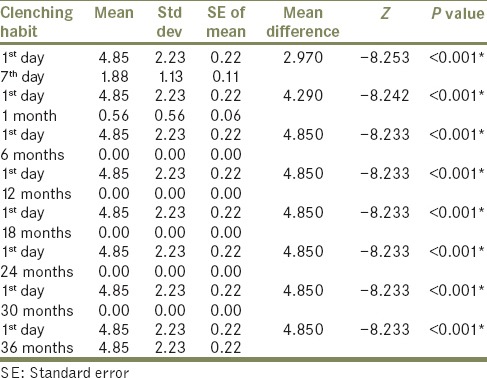
Table 10.
Comparison of mean intensity of ‘temporal headache’ from pretreatment day 1 to other time intervals
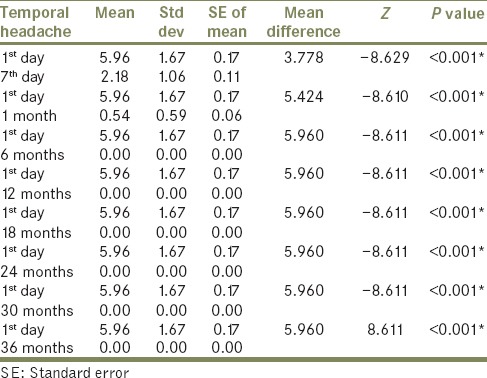
Table 11.
Comparison of mean intensity of ‘neck pain’ from pre treatment day 1 to other time intervals
DISCUSSION
The alternate hypothesis was accepted because there was a significant difference in the disclusion times between the pretreatment and posttreatment intervals (μ1 ≠ μ2) when lengthy disclusion time was shortened to <0.4 s per excursion. In addition, this study's results corroborate the findings of previous disclusion time reduction studies involving the ICAGD coronoplasty as a treatment for myofascial pain symptoms.[17,18,19,20,21,22,23] The role of occlusion in activating myofascial pain symptoms has long been debated. While some authors have shown occlusal equilibration to be a successful treatment modality in treatment of such disorders[5,6,7], other controlled studies have shown there were similar symptom resolutions in both the control and the treated groups.[8,9,10,11,12] The results of this study, and others that preceded this study, indicate that ICAGD treatment will predictably reduce myofascial pain symptoms because of the physiologic muscle activity lowering effect achieved by ICAGD,[28] which is a distinctly different occlusal adjustment approach to retruding the mandible into centric relation during traditional occlusal equilibration procedures.
The concept of treating the myofascial pain patients with ICAGD is not new. Various studies have been performed in the past evaluating their effect on symptoms. Lengthy disclusion time has been shown in a simultaneous electromyography study to elevate muscle activity levels, and that proper reduction of disclusion time <0.4 s can reduce the muscle hyperactivity and related myofascial pain symptoms.[21,28] A study by Kerstein in 1991 performed on seven female subjects with myofascial pain treated with ICAGD to reduce disclusion time to <0.4 s, showed statistically significant changes in pre- and post-treatment disclusion times with a significant symptom resolution.[21] Additionally, the same author showed that statistically significant muscle activity level reductions occurred in 45 symptomatic myofascial pain patients, when ICAGD was properly performed.[28] Finally, in a controlled occlusal adjustment study that compared treated, placebo, and untreated myofascial pain subject groups with respect to their differences in disclusion time, symptom remissions began in the treated group within 1 week after the disclusion time was reduced <0.4 s, and symptom resolution lasted for the 3-year period of posttreatment observation.[22] This study showed the multiple recall visit disclusion time means were statistically equivalent to the posttreatment day 1 disclusion time mean. Further, the standard deviations from recall visit-to-visit remained fairly constant throughout the 3-year period of observation. The mean differences also remained constant when a comparison between day 1 pretreatment and subsequent visit measurements was made. This suggests that once disclusion time is reduced <0.4 s, it is a lasting occlusal change. These findings are very similar to those of another disclusion time reduction study that verified that once the disclusion time was properly reduced, it remained constant, leading to the retention of proper muscle function and low symptom appearances.[27]
In this study, the population selected for treatment had their symptoms evaluated by a questionnaire at eight subsequent recall appointments (day 7, 1 month, 6 months, 12 months, 18 months, 24 months, 30 months, and 36 months), during which the subjects were not allowed to view their previous symptom responses. This made subjective symptom assessment visit-to-visit, far more reliable for the statistical analyses. The results obtained from the many recall date questionnaires showed there was a significant symptom resolution within the treated population that was maintained during the 3-year period of observation. These findings indicated there were physiologic benefits obtained from treating myofascial pain subjects using the ICAGD protocol.
CONCLUSION
The findings of this study corroborate prior evidence that when disclusion time is reduced <0.4 s per excursion, it is effective in reducing the myofascial pain symptoms. In this study, the significant change in disclusion time duration (P < 0.05) after the ICAGD coronoplasty was performed, led to statistically significant reductions in muscular-based myofascial pain symptoms that began immediately after day 1 of treatment was instituted (P < 0.05).
When the right and left lateral excursive disclusion times of 100 patients were compared from pre- to post-treatment with ICAGD:
The lateral excursive disclusion time, if prolonged, will be potentially etiologic for myofascial pain symptoms
Reducing the left and right excursive disclusion times to <0.4 s per excursion will bring down the symptoms of myofascial pain
When myofascial pain cases are treated by ICAGD technique using T-Scan III computerized occlusal analyses that measure the correctness of the ICAGD treatment result, symptoms will rapidly resolve shortly after the treatment is rendered.
The advent of disclusion time reduction therapy using properly performed ICAGD[16,20,32,33,34,35,36] is a potentially new direction in the treatment of myofascial pain dysfunction patients. Further studies with longer follow-up should be performed using ICAGD in the treatment of occluso-muscle pains of TMD disorders.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge my mentor Dr. Robert B. Kerstein, for his guidance and timely help while my team performed this study.
Robert B. Kerstein, DMD, Former Faculty Department of Restorative Dentistry, Tufts University School of Dental Medicine, Boston, MA, USA.
REFERENCES
- 1.Halperin GC, Halperin AR, Norling BK. Thickness, strength, and plastic deformation of occlusal registration strips. J Prosthet Dent. 1982;48:575–8. doi: 10.1016/0022-3913(82)90367-5. [DOI] [PubMed] [Google Scholar]
- 2.Saraçoglu A, Ozpinar B. In vivo and in vitro evaluation of occlusal indicator sensitivity. J Prosthet Dent. 2002;88:522–6. doi: 10.1067/mpr.2002.129064. [DOI] [PubMed] [Google Scholar]
- 3.Dawson PE. Functional Occlusion: From TMJ to Smile Design. Vol. 1. Louis, MO: Mosby; 2007. p. 54. 266, 347, 393-9, 412. [Google Scholar]
- 4.Glickman I. Clinical Periodontics. 5th ed. Philadelphia, PA: Saunders and Co; 1979. p. 948. 978. [Google Scholar]
- 5.Ramfjord SP. Dysfunctional temporomandibular joint and muscle pain. J Prosthet Dent. 1966;11:353–74. [Google Scholar]
- 6.Dawson PE. Evaluation, Diagnosis, and Treatment of Occlusal Problems. 2nd ed. St Louis: CV Mosby Co; 1988. p. 105. [Google Scholar]
- 7.Schwartz L, Chayes C. Facial Pain and Mandibular Dysfunction. 1st ed. Philadelphia: WB Saunders Co; 1969. p. 1174. [Google Scholar]
- 8.Forssell H, Kirveskari P, Kangasniemi P. Changes in headache after treatment of mandibular dysfunction. Cephalalgia. 1985;5:229–36. doi: 10.1046/j.1468-2982.1985.0504229.x. [DOI] [PubMed] [Google Scholar]
- 9.Forssell H, Kirveskari P, Kangasniemi P. Effect of occlusal adjustment on mandibular dysfunction. A double-blind study. Acta Odontol Scand. 1986;44:63–9. doi: 10.3109/00016358609041309. [DOI] [PubMed] [Google Scholar]
- 10.Forssell H, Kirveskari P, Kangasniemi P. Response to occlusal treatment in headache patients previously treated by mock occlusal adjustment. Acta Odontol Scand. 1987;45:77–80. doi: 10.3109/00016358709098360. [DOI] [PubMed] [Google Scholar]
- 11.Tsolka P, Morris RW, Preiskel HW. Occlusal adjustment therapy for craniomandibular disorders: A clinical assessment by a double-blind method. J Prosthet Dent. 1992;68:957–64. doi: 10.1016/0022-3913(92)90558-r. [DOI] [PubMed] [Google Scholar]
- 12.Tsolka P, Preiskel HW. Kinesiographic and electromyographic assessment of the effects of occlusal adjustment therapy on craniomandibular disorders by a double-blind method. J Prosthet Dent. 1993;69:85–92. doi: 10.1016/0022-3913(93)90246-k. [DOI] [PubMed] [Google Scholar]
- 13.Greene CS, Lerman MD, Sutcher HD, Laskin DM. The TMJ pain-dysfunction syndrome: Heterogeneity of the patient population. J Am Dent Assoc. 1969;79:1168–72. doi: 10.14219/jada.archive.1969.0091. [DOI] [PubMed] [Google Scholar]
- 14.Butler JH, Folke LE, Bandt CL. A descriptive survey of signs and symptoms associated with the myofascial pain-dysfunction syndrome. J Am Dent Assoc. 1975;90:635–9. doi: 10.14219/jada.archive.1975.0147. [DOI] [PubMed] [Google Scholar]
- 15.Moulton RE. Emotional factors in non-organic temporomandibular joint pain. Dent Clin North Am. 1966:609–20. [PubMed] [Google Scholar]
- 16.Fricton J. Myogenous temporomandibular disorders: Diagnostic and management considerations. Dent Clin North Am. 2007;51:61–83. doi: 10.1016/j.cden.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Kerstein RB, Farrell S. Treatment of myofascial pain-dysfunction syndrome with occlusal equilibration. J Prosthet Dent. 1990;63:695–700. doi: 10.1016/0022-3913(90)90328-a. [DOI] [PubMed] [Google Scholar]
- 18.Kerstein RB. A comparison of traditional occlusal equilibration and immediate complete anterior guidance development. Cranio. 1993;11:126–39. doi: 10.1080/08869634.1993.11677954. [DOI] [PubMed] [Google Scholar]
- 19.Kerstein R. Disclusion time reduction therapy with immediate complete anterior guidance development: The technique. Quintessence Int. 1992;23:735–47. [PubMed] [Google Scholar]
- 20.Thumati P, Manwani R, Mahantshetty M. The effect of reduced disclusion time in the treatment of myofascial pain dysfunction syndrome using immediate complete anterior guidance development protocol monitored by digital analysis of occlusion. Cranio. 2014;32:289–99. doi: 10.1179/2151090314Y.0000000004. [DOI] [PubMed] [Google Scholar]
- 21.Kerstein RB, Wright N. An electromyographic and T-Scan analysis of patients suffering from chronic myofascial pain dysfunction syndrome; pre and post treatment with immediate complete anterior guidance development. J Prosthet Dent. 1991;66:677–86. doi: 10.1016/0022-3913(91)90453-4. [DOI] [PubMed] [Google Scholar]
- 22.Kerstein RB, Chapman R, Klein M. A comparison of ICAGD immediate complete anterior guidance development to mock ICAGD for symptom reductions in chronic myofascial pain dysfunction patients. Cranio. 1997;15:21–37. doi: 10.1080/08869634.1997.11745990. [DOI] [PubMed] [Google Scholar]
- 23.Kerstein R. Disclusion time measurement studies: Stability of disclusion time – A 1-year follow-up. J Prosthet Dent. 1994;72:164–8. doi: 10.1016/0022-3913(94)90075-2. [DOI] [PubMed] [Google Scholar]
- 24.Mannes WL. Force movie: A time and force view of occlusion. Compendium. 1989;10:404–8. [Google Scholar]
- 25.Maness WL, Benjamin M, Podoloff R, Bobock G, Golden RF. Computerized occlusal analysis: A new technology, Chicago. Quintessence Int. 1986;15:287. [PubMed] [Google Scholar]
- 26.Kerstein RB. Time-sequencing and force-mapping with integrated electromyography to measure occlusal parameters. In: Daskalaki A, editor. Informatics in Oral Medicine. Hershey, PA: IGI Global; 2010. pp. 88–110. [Google Scholar]
- 27.Kerstein RB. Treatment of myofascial pain dysfunction syndrome with occlusal therapy to reduce lengthy disclusion time a recall study. Cranio. 1995;13:105–15. doi: 10.1080/08869634.1995.11678053. [DOI] [PubMed] [Google Scholar]
- 28.Kerstein RB, Radke J. Masseter and temporalis excursive hyperactivity decreased by measured anterior guidance development. Cranio. 2012;30:243–54. doi: 10.1179/crn.2012.038. [DOI] [PubMed] [Google Scholar]
- 29.Kerstein RB. Reducing chronic massetter and temporalis muscular hyperactivity with computer guided occlusal adjustments. Compendium. 2010;31:530–43. [PubMed] [Google Scholar]
- 30.Kerstein RB, Grundset K. Obtaining bilateral simultaneous occlusal contacts with computer analyzed and guided occlusal adjustments. Quintessence Int. 2001;32:7–18. [Google Scholar]
- 31.Carey JP, Craig M, Kerstein RB, Radke J. Determining a relationship between applied occlusal load and articulating paper mark area. Open Dent J. 2007;1:1–7. doi: 10.2174/1874210600701010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blass JL. Occlusal equilibration in periodontal treatment. N Y Dent J. 1956;12:121–9. [Google Scholar]
- 33.Ramfjord SP. Bruxism, a clinical and electromyographic study. J Am Dent Assoc. 1961;62:21–44. doi: 10.14219/jada.archive.1961.0002. [DOI] [PubMed] [Google Scholar]
- 34.Schuyler CH. Fundamental principles in the correction of occlusal disharmony, natural and artificial. J Am Dent Assoc. 1935;22:1193–202. [PubMed] [Google Scholar]
- 35.Kerstein RB. Disclusion time measurement studies; Part 2: A comparison of disclusion time length of 49 chronic myofascial pain dysfunction syndrome patients to 40 non-patients. A population analysis. J Prosthet Dent. 1994;72:473–80. doi: 10.1016/0022-3913(94)90117-1. [DOI] [PubMed] [Google Scholar]
- 36.Kerstein RB, Radke J. The effect of disclusion time reduction on maximal clench muscle activity levels. Cranio. 2006;24:156–65. doi: 10.1179/crn.2006.026. [DOI] [PubMed] [Google Scholar]


