Abstract
OBJECTIVE
This study evaluated associations among cardiovascular autonomic neuropathy (CAN), female sexual dysfunction (FSD), and urinary incontinence (UI) in women with type I diabetes mellitus (T1DM).
RESEARCH DESIGN AND METHODS
We studied 580 women with T1DM in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study (DCCT/EDIC). CAN was defined as: 1) R-R variation <15 with deep breathing or 2) R-R variation of 15–19.9 plus Valsalva ratio ≤1.5 or a supine-to-standing drop of 10 mmHg in diastolic blood pressure. A Sandvik Severity Index of 3–12 defined UI, and a Female Sexual Function Index (FSFI-R) score ≥22.75 defined FSD. Multivariable models estimated associations among CAN, FSD, and UI.
RESULTS
At EDIC year 17, FSD was observed in 41% of women and UI in 30%. No statistically significant associations were observed between measures of CAN at DCCT closeout and subsequent report of FSD or UI. At EDIC year 16/17, there was a 53% increased odds of having UI with a Valsalva ratio ≤1.5. At both EDIC year 13/14 and EDIC year 16/17, a 5-unit increase in R-R variation was associated with a 1.11 greater odds of having FSD.
CONCLUSIONS
In women with T1DM in the DCCT/EDIC, we found significant increased odds of FSD and UI with specific measures of CAN. In long-standing T1DM, CAN may predict development of FSD and may be a useful surrogate for generalized diabetic autonomic neuropathy.
Introduction
Female sexual dysfunction (FSD) and urinary incontinence (UI) have a significant negative effect on quality of life among women with diabetes (1–3). Previous work has demonstrated that up to 38% of women with type 1 diabetes mellitus (T1DM) have some incontinence and up to 35% meet criteria for FSD (4,5). Although FSD due to DM is likely multifactorial, an autonomic component has been proposed (6–8). Similarly, alterations in bladder innervation may contribute to overall bladder dysfunction and UI (9,10), and physiologic evaluation of autonomic neuropathy through sympathetic skin response has been explored in two small studies (11,12). However, the possible association of the various measures of cardiac autonomic neuropathy (CAN), which are the most common and earliest signs of autonomic neuropathy, with FSD and UI is unclear (13,14).
The autonomic nervous system plays a critical role in regulating multiple organ systems, through a broad network of small afferent and efferent unmyelinated nerve fibers. These nerve fibers are sensitive to diabetes-induced dysfunction and damage, known as autonomic neuropathy (15). Although the magnitude of signs and symptoms varies, from asymptomatic small fiber dysfunction to severe impairment of neurovascular function, glycemic control and diabetes duration are directly related to systemic autonomic nervous system dysfunction (14,16). Therefore, once diabetic autonomic neuropathy has affected one organ system, other organ systems are also likely to be involved.
The objective of this study was to evaluate the associations between CAN with FSD and UI in female participants of the Epidemiology of Diabetes Interventions and Complications (EDIC) study, the observational follow up to the Diabetes Control and Complications Trial (DCCT). The DCCT/EDIC cohort is a large and well-characterized cohort of individuals with T1DM, continuously monitored for ∼30 years, with available data on numerous diabetic complications, risk factors and medication use (17–19). We evaluated the association of CAN (assessed during DCCT and EDIC [20,21]) with FSD and UI (assessed during EDIC) as part of UroEDIC, an ancillary study of urologic complications (22,23).
Research Design and Methods
Population and Setting
The DCCT and EDIC studies have been described in detail (17–19). Briefly, 1,441 subjects with T1DM for 1–15 years with no (primary prevention cohort) or minimal diabetic retinopathy (secondary intervention cohort) were enrolled in DCCT. Subjects were randomly assigned to intensive or conventional treatment and were monitored for a mean of 6.5 years, (range 3–9) (18). At the end of DCCT, intensive therapy was recommended for all subjects. Annual EDIC examinations began in 1994, with 1,375 (96%) former DCCT subjects consenting to participate in EDIC. A detailed description of EDIC study procedures and baseline characteristics has been previously published (17).
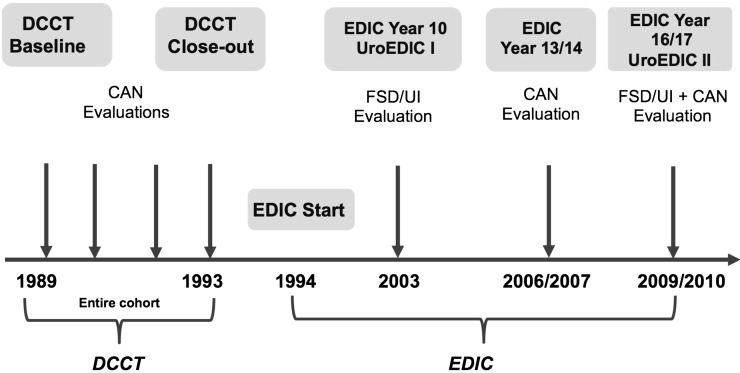
Of the original 680 women enrolled, 676 completed the DCCT in 1993, and 655 (96%) agreed to participate in the first annual examination of EDIC in 1994. UroEDIC, an ancillary study designed to examine urologic complications of diabetes, included the first FSD and UI evaluations in 2003, which were repeated in 2010 (Fig. 1). At EDIC year 17 (in 2010), 580 of the 618 active women (94%) agreed to participate in UroEDIC, and among them, 371 and 571 had valid FSD and UI information, respectively, and comprise the cohort for the current analyses. Figure 1 summarizes the timeline for data collection for FSD, UI, and neuropathy data for DCCT/EDIC. All DCCT/EDIC procedures were approved by institutional review boards of all participating centers. Written informed consent was provided by all participants.
Figure 1.
Neuropathy and FSD/UI data collection in DCCT/EDIC.
FSD and UI Evaluation
FSD was evaluated by the abbreviated version of the Female Sexual Function Index (FSFI-R), a widely used, well-validated, multidimensional, self-report measure that assesses sexual function across six domains, including sexual desire, arousal, lubrication, orgasm, satisfaction, and pain. Presence of FSD was defined by a score ≥22.75 on the FSFI-R (24). UI was determined by incontinence frequency and amount of urine lost per episode (drops, small splashes, more), using the validated Sandvik Severity Index (25). The Sandvik Severity Index is calculated from frequency and amount of urine loss on a scale of 0 to 12 (dry/mild: –0 to 2, moderate: –3 to 6, severe: –8 to 9, very severe: –12). For this study, presence of UI was defined as Sandvik Severity Index of 3 to 12 (moderate/very severe UI).
CAN Evaluations
Standardized CAN evaluations were established as part of DCCT and rigorously applied and interpreted throughout the study. Briefly, these included R-R response to paced breathing (R-R variation), Valsalva maneuver, and postural changes (supine-to-stand) in blood pressure measured at baseline, biennially during DCCT, and at years 13/14 and 16/17 during EDIC (20,26). These cardiovascular reflex tests are objective, highly reproducible, and still recommended by consensus in the field as the gold standard (27). All subjects were asked to fast and avoid vigorous exercise for 24 h and caffeine and tobacco products for 8 h before CAN testing and to hold all prescription and over-the-counter medicines (except for basal insulin) until testing was completed (20,26). Subjects who experienced hypoglycemia after midnight (blood glucose ≤50 mg/dL or signs/symptoms of hypoglycemia) and subjects with acute illnesses 48 h before testing were excluded from CAN testing. Subjects with proliferative retinopathy, recent history of laser therapy or vitrectomy, and/or no eye examination in the last 4 years and those who could not perform the required forced expiration were excluded from the Valsalva maneuver.
CAN testing was performed with Hokanson ANS2000 devices (Hokanson Inc., Bellevue, WA), and results were analyzed at a single reading center. All CAN measurements were reviewed by a single investigator, masked to DCCT treatment assignment, with extensive expertise in neurophysiology, who determined whether the technical quality of the recording and conditions of the test met study criteria. Intrasubject reproducibility of the CAN tests was evaluated using same-day, test-retest on a random subset of 185 DCCT/EDIC participants across all EDIC sites and revealed high test-retest correlations for R-R variation (κ = 0.78) and Valsalva (κ = 0.80, P < 0.0001 for both).
The standardized cut points for CAN measures used in DCCT included an R-R variation <15 and a Valsalva ratio ≤1.5. Abnormal CAN function was defined as R-R variation <15 or R-R variation between 15 and 19.9 plus a Valsalva ratio ≤1.5 or a supine-to-standing drop of 10 mmHg in diastolic blood pressure (DBP) (20). Because more recent evidence has demonstrated that categorical cutoffs for R-R and Valsalva may have limitations due to the important effect of age on heart rate variation (28,29), we have also included the changes in age-adjusted continuous measures of the R-R variation and Valsalva ratio in the analyses.
Other Evaluations
Hemoglobin A1c (HbA1c) level was measured at baseline and quarterly during DCCT and annually in EDIC using high-performance ion-exchange liquid chromatography, as previously described (30). Systolic blood pressure (SBP) and DBP were measured quarterly during the DCCT and annually during EDIC. The time-weighted mean values for HbA1c, SBP, and DBP were used, representing the running means up to each study visit in the DCCT and EDIC. Hypertension was defined as sitting SBP ≥140 mmHg and/or DBP ≥90 mmHg or the use of antihypertensive medication (31). β-Blocker use was assessed annually because this is known to have the most direct effect on heart rate variability. Information on additional medications such as tricyclics, clonidine, angiotensin receptor blockers, or ACE inhibitors was not available. In addition, although neuropathic pain was assessed, prevalence in our cohort was quite low. Retinopathy was assessed using 7-field stereoscopic fundus photographs that were centrally graded using the Early Treatment Diabetic Retinopathy Study scale. Albumin excretion rate (AER) was measured in half of the cohort annually. Nephropathy was defined as microalbuminuria (AER 30–300 mg/24 h) or albuminuria (AER >300 mg/24 h).
Statistical Analysis
Descriptive analysis examined the distribution of demographic and clinical characteristics, markers of diabetes control and treatment, blood pressure control, and neuropathy measures by FSD and UI status. The Kruskal-Wallis test assessed differences in quantitative variables, and the contingency χ2 test assessed categoric variables. Multivariable logistic regression models estimated the associations, using odds ratios and 95% CIs, between quantitative and qualitative neuropathy measures and the presence of FSD or UI at EDIC year 17 after adjustment for DCCT cohort assignment, DCCT/EDIC time-weighted HbA1c, DCCT/EDIC time-weighted SBP, age, duration of diabetes, BMI, smoking status, drinking status, postmenopausal status, parity, and any β-blocker medication use. Effects nominally significant at P ≤ 0.05 are cited. Analyses were performed using SAS 9.3 software (SAS Institute, Inc., Cary, NC).
Results
Table 1 summarizes the sociodemographic, clinical, and diabetic characteristics of study participants by FSD and UI status. At EDIC year 17,153 participants (41%) reported FSD and 172 (30%) reported UI. Women reporting FSD were significantly older and more likely to be married, postmenopausal, and nulliparous than women without FSD. Those with UI had significantly higher BMI values than those without UI.
Table 1.
Characteristics of DCCT/EDIC female participants by FSD and UI status at EDIC year 17
| No FSD (n = 218) | FSD (n = 153) | P value | No UI (n = 399) | UI (n = 172) | P value | |
|---|---|---|---|---|---|---|
| Sociodemographic/clinical | ||||||
| Attained age (years) | 447.7 ± 6.7 | 51.8 ± 7.1 | <0.0001 | 50.3 ± 7.4 | 51.6 ± 6.5 | 0.1 |
| Married | 157 (75) | 124 (84) | 0.04 | 269 (70) | 116 (69) | 0.8 |
| Current cigarette smoker | 28 (13) | 13 (9) | 0.2 | 44 (12) | 22 (13) | 0.6 |
| Current drinker | 86 (41) | 65 (44) | 0.6 | 161 (42) | 58 (35) | 0.1 |
| BMI (kg/m2) | 28.2 ± 6.0 | 28.2 ± 5.4 | 0.8 | 27.9 ± 5.5 | 30.1 ± 6.4 | <0.0001 |
| BMI category (kg/m2) | ||||||
| Normal (BMI <25) | 59 (29) | 40 (28) | 0.6 | 115 (31) | 35 (21) | 0.001 |
| Overweight (BMI 25 to <30) | 82 (40) | 66 (46) | 157 (42) | 60 (36) | ||
| Obese (BMI ≥30) | 63 (31) | 39 (27) | 103 (27) | 71 (43) | ||
| Postmenopausal | 87 (41) | 94 (64) | <0.0001 | 216 (56) | 105 (63) | 0.2 |
| Hysterectomy | 32 (15) | 27 (18) | 0.4 | 63 (16) | 35 (21) | 0.2 |
| Parity (n live births) | ||||||
| 0 | 107 (49) | 94 (61) | 0.05 | 239 (6) | 105 (61) | 0.9 |
| 1 | 42 (19) | 27 (18) | 67 (17) | 28 (16) | ||
| ≥2 | 68 (31) | 32 (21) | 92 (23) | 39 (23) | ||
| UTI within past year | 39 (19) | 23 (16) | 0.4 | 60 (16) | 33 (20) | 0.3 |
| Diabetes control and treatment | ||||||
| Primary prevention cohort | 117 (54) | 78 (51) | 0.6 | 207 (52) | 81 (47) | 0.3 |
| Intensive treatment group | 106 (49) | 82 (54) | 0.3 | 203 (51) | 96 (56) | 0.3 |
| Diabetes duration (years) | 29.3 ± 4.9 | 29.9 ± 5.1 | 0.3 | 29.6 ± 5.0 | 30.5 ± 5.3 | 0.06 |
| DCCT/EDIC time-weighted | ||||||
| HbA1c (%) | 8.0 ± 0.9 | 8.0 ± 0.9 | 0.6 | 8.0 ± 0.9 | 8.1 ± 1.0 | 0.5 |
| HbA1c (mmol/mol) | 63.6 ± 9.9 | 63.4 ± 10.2 | 0.6 | 64 ± 9.8 | 65 ± 10.9 | 0.5 |
| Diabetic complications | ||||||
| Retinopathy* | 28 (13) | 30 (20) | 0.08 | 63 (16) | 33 (19) | 0.3 |
| Nephropathy** | ||||||
| None (<30 mg) | 173 (82) | 124 (87) | 0.5 | 318 (84) | 136 (84) | 0.3 |
| Microalbuminuria (30–300 mg) | 33 (16) | 16 (11) | 52 (14) | 25 (15) | ||
| Albuminuria (≥300 mg) | 4 (2) | 3 (2) | 10 (3) | 1 (1) | ||
| eGFR <60 mL/min/1.73 m2 | 12 (6) | 6 (4) | 0.5 | 25 (6) | 5 (3) | 0.09 |
| Blood pressure control | ||||||
| DCCT/EDIC time-weighted | ||||||
| SBP (mmHg) | 114.9 ± 8.5 | 116.5 ± 8.8 | 0.1 | 115.7 ± 8.3 | 117.3 ± 8.2 | 0.05 |
| DBP (mmHg) | 72.4 ± 5.0 | 72.2 ± 5.2 | 0.9 | 72.3 ± 5.0 | 72.6 ± 4.9 | 0.5 |
| Hypertension# | 113 (55) | 89 (61) | 0.3 | 224 (59) | 112 (67) | 0.06 |
| Antihypertensive use | ||||||
| β-Blockers | 18 (9) | 20 (14) | 0.1 | 34 (9) | 29 (17) | 0.005 |
| ACE inhibitors or ARB | 97 (47) | 69 (47) | 0.9 | 193 (51) | 94 (56) | 0.3 |
| Calcium channel blockers | 12 (6) | 12 (8) | 0.4 | 27 (7) | 20 (12) | 0.06 |
Data are mean ± SD or n (%). Sample sizes may vary due to missing data. FSD defined as FSFI-R score ≥22.75. UI was defined as moderate to severe with a Sandvik Severity Index ≥3. P values are based on the Kruskal-Wallis test for quantitative variables or the contingency χ2 for qualitative variables. ARB, angiotensin receptor blocker; eGFR, estimated glomerular filtration rate calculated by the Chronic Kidney Disease Epidemiology Collaboration; UTI, urinary tract infection.
*Retinopathy defined through EDIC year 14 using the Early Treatment Diabetic Retinopathy Study on a scale of 0–23 (<12 nonproliferative or none, ≥12 proliferative).
**Nephropathy defined using AER (mg/24 h) at EDIC year 15/16.
#Hypertension defined as sitting SBP ≥140 mmHg and/or DBP ≥90 mmHg or the use of antihypertensive medication.
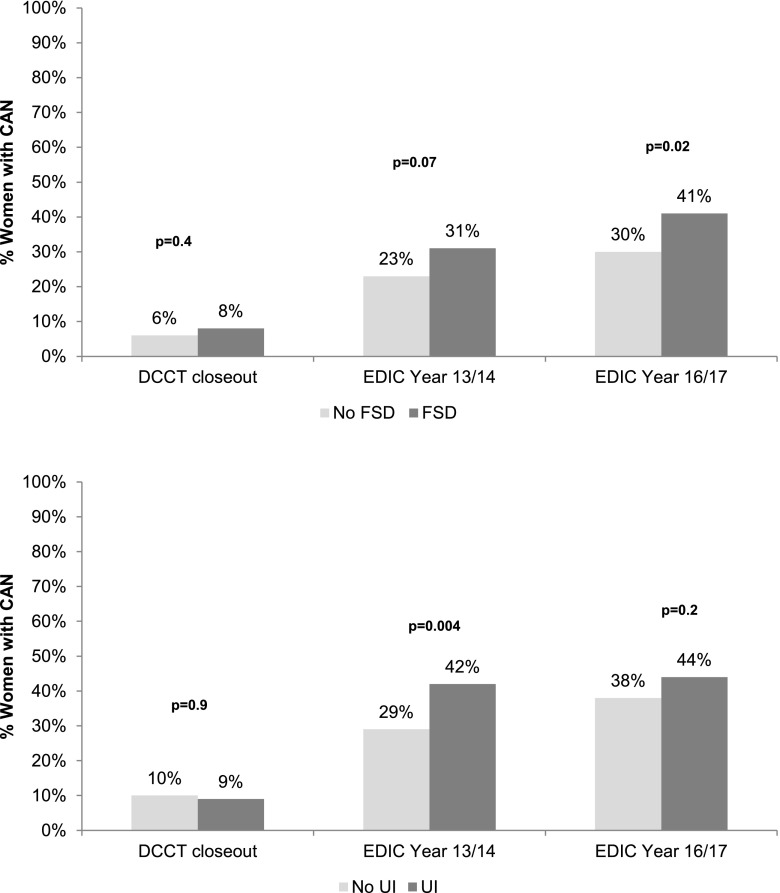
Figure 2 depicts the prevalence of the composite CAN outcome at DCCT closeout and at EDIC year 13/14 and 16/17 among those with and without FSD and UI. The prevalence of CAN at EDIC year 16/17 was significantly higher (41% vs. 30%, P = 0.02) in women who reported FSD at EDIC year 17 compared with those without FSD. No difference in prevalence of CAN at DCCT closeout was observed by UI status. The prevalence of CAN at EDIC year 13/14 was significantly increased in women reporting UI (42% vs. 29%, P = 0.004) compared with those without UI. This increased prevalence of CAN was also observed at EDIC year 16/17 in women with UI (44% vs. 38%, P = 0.2); however, the results were not statistically significant.
Figure 2.
Prevalence of CAN among women with FSD and UI in DCCT/EDIC. CAN defined as an R-R variation <15 or R-R variation between 15 and 19.9 plus a Valsalva ratio ≤1.5 or a supine-to-standing drop of 10 mmHg in DBP (20).
Individual measures of CAN by FSD and UI status are reported in Table 2. Women who had a lower mean R-R variation and R-R variation <15 at EDIC year 13/14 were significantly more likely to report FSD at EDIC year 17. All quantitative and qualitative measures of CAN at EDIC year 16/17, with the exception of the Valsalva ratio, were significantly associated with report of FSD at EDIC year 17. No differences in CAN measures at DCCT closeout were observed by UI status reported at EDIC year 17. Mean R-R variation and Valsalva ratio at EDIC year 13/14 were lower in women with UI compared with those without UI. Similarly, a greater proportion of women with UI had R-R variation <15 and a Valsalva ratio <1.5 at EDIC year 13/14. The mean Valsalva ratio and the proportion of women with a Valsalva ratio <1.5 at EDIC year 16/17 was significantly lower in women with UI than in those without UI.
Table 2.
CAN measures at DCCT closeout and EDIC years 13/14 and 16/17 by FSD and UI status at EDIC Year 17
| Neuropathy measures* | No FSD (n = 218) | FSD (n = 153) | P value | No UI (n = 399) | UI (n = 172) | P value |
|---|---|---|---|---|---|---|
| CAN measures at DCCT closeout | ||||||
| R-R variation | 44.0 ± 22.2 | 38.4 ± 18.6 | 0.05 | 41.3 ± 21.9 | 40.3 ± 20.1 | 0.8 |
| R-R variation <15 | 12 (6) | 12 (9) | 0.4 | 34 (10) | 15 (10) | 0.9 |
| Valsalva ratio | 2.1 ± 0.4 | 2.0 ± 0.4 | 0.6 | 2.0 ± 0.4 | 2.0 ± 0.4 | 0.7 |
| Valsalva ratio ≤1.5 | 11 (6) | 6 (5) | 0.5 | 26 (8) | 6 (4) | 0.1 |
| Composite CAN** | 12 (6) | 12 (8) | 0.4 | 36 (10) | 15 (9) | 0.9 |
| CAN measures at EDIC year 13/14 | ||||||
| R-R variation | 32.1 ± 18.9 | 26.0 ± 16.2 | 0.002 | 28.5 ± 18.4 | 25.2 ± 17.3 | 0.03 |
| R-R variation <15 | 34 (17) | 38 (26) | 0.03 | 88 (24) | 53 (33) | 0.04 |
| Valsalva ratio | 1.8 ± 0.4 | 1.8 ± 0.3 | 0.5 | 1.8 ± 0.4 | 1.7 ± 0.3 | 0.001 |
| Valsalva ratio ≤1.5 | 43 (24) | 33 (27) | 0.5 | 76 (24) | 57 (40) | 0.001 |
| Composite CAN** | 46 (23) | 45 (31) | 0.07 | 106 (29) | 68 (42) | 0.004 |
| CAN measures at EDIC year 16/17 | ||||||
| R-R variation | 29.4 ± 18.5 | 22.7 ± 14.6 | 0.0008 | 25.5 ± 17.2 | 22.6 ± 16.5 | 0.05 |
| R-R variation <15 | 47 (23) | 50 (35) | 0.02 | 118 (31) | 61 (38) | 0.2 |
| Valsalva ratio | 1.8 ± 0.4 | 1.7 ± 0.3 | 0.1 | 1.7 ± 0.3 | 1.6 ± 0.3 | 0.02 |
| Valsalva ratio ≤1.5 | 55 (29) | 53 (39) | 0.05 | 116 (33) | 71 (46) | 0.005 |
| Composite CAN** | 61 (30) | 60 (41) | 0.02 | 142 (38) | 72 (44) | 0.2 |
Data are mean ± SD or n (%). Sample sizes may vary due to missing data. FSD defined as FSFI-R score ≥22.75. UI defined as moderate to severe with a Sandvik Severity Index ≥3. P values are based on the difference between those with and without FSD or UI using the Wilcoxon rank sum test for quantitative variables or the contingency χ2 for qualitative variables.
*Sample sizes vary based on data availability for individual measures of neuropathy.
**Composite CAN defined as R-R variation <15 or R-R variation between 15 and 19.9 plus a Valsalva ratio ≤1.5 or a supine-to-standing drop of 10 mmHg in DBP.
Odds of FSD and UI by quantitative and qualitative CAN measures adjusted for known risk factors of FSD and UI, including age, duration of diabetes, BMI, postmenopausal status, parity, smoking and alcohol consumption, DCCT/EDIC time-weighted HbA1c, the DCCT/EDIC time-weighted SBP, and any β-blocker medication use, are reported in Table 3. No statistically significant associations were observed between measures of CAN at DCCT closeout and subsequent report of FSD or UI. At EDIC year 13/14, there was a 68% increased odds of having UI with a Valsalva ratio ≤1.5 (odds ratio 1.68; 95% CI 1.01, 2.78). At both EDIC year 13/14 and EDIC year 16/17, a 5-unit increase in R-R variation was associated with a 1.11 greater odds of having FSD (P = 0.02 for both). The remainder of the results were not statistically significant.
Table 3.
Multivariable-adjusted odds ratios* for UI and FSD at EDIC year 16/17 by CAN measures at DCCT closeout and EDIC years 13/14 and 16/17
| Neuropathy measures* | FSD (n = 153) vs. no FSD (n = 218) | P value | UI (n = 172) vs. no UI (n = 399) | P value |
|---|---|---|---|---|
| CAN measures at DCCT closeout | ||||
| R-R variation | 1.03 (0.97–1.10) | 0.4 | 0.99 (0.94–1.04) | 0.6 |
| R-R variation <15 | 1.01 (0.39–2.57) | 0.9 | 0.83 (0.40–1.70) | 0.6 |
| Valsalva ratio | 1.16 (0.83–1.63) | 0.4 | 0.90 (0.69–1.17) | 0.4 |
| Valsalva ratio ≤1.5 | 0.74 (0.24–2.31) | 0.6 | 0.40 (0.14–1.10) | 0.07 |
| Composite CAN** | 1.00 (0.39–2.58) | 0.9 | 0.78 (0.39–1.58) | 0.5 |
| CAN measures at EDIC year 13/14 | ||||
| R-R variation | 1.11 (1.02–1.20) | 0.02 | 1.01 (0.95–1.07) | 0.8 |
| R-R variation <15 | 1.82 (0.94–3.52) | 0.08 | 1.13 (0.69–1.84) | 0.6 |
| Valsalva ratio | 1.09 (0.75–1.59) | 0.6 | 1.29 (0.92–1.80) | 0.1 |
| Valsalva ratio ≤1.5 | 1.01 (0.52–1.94) | 0.9 | 1.68 (1.01–2.78) | 0.05 |
| Composite CAN** | 1.51 (0.83–2.75) | 0.2 | 1.32 (0.83–2.10) | 0.2 |
| CAN measures at EDIC year 16/17 | ||||
| R-R variation | 1.11 (1.02–1.21) | 0.02 | 1.01 (0.95–1.08) | 0.7 |
| R-R variation <15 | 1.80 (1.01–3.21) | 0.05 | 1.03 (0.66–1.61) | 0.9 |
| Valsalva ratio | 1.35 (0.90–2.04) | 0.2 | 1.23 (0.87–1.73) | 0.2 |
| Valsalva ratio ≤ 1.5 | 1.61 (0.92–2.84) | 0.1 | 1.53 (0.98–2.39) | 0.06 |
| Composite CAN** | 1.52 (0.89–2.61) | 0.1 | 0.92 (0.59–1.42) | 0.7 |
Multivariable logistic regression model with UI or FSD status as the dependent variable and neuropathy measures as the independent variables. Data are odds ratios (95% CIs) from separate multivariable logistic regression models. The odds ratios were evaluated according to the presence or absence of an R-R <15, Valsalva ≤1.5, abnormal CAN function, or confirmed clinical neuropathy or according to a 5-unit decrease in R-R variation or a half-unit decrease in Valsalva ratio. Adjustments were made for DCCT cohort assignment, DCCT/EDIC time-weighted HbA1c, DCCT/EDIC time-weighted SBP, and the following EDIC year 17 characteristics: age, duration of diabetes, BMI, smoking status, drinking status, postmenopausal status, parity, and any β-blocker medication use.
*Sample sizes vary based on data availability for individual measures of CAN.
**CAN defined as either R-R variation <15 or R-R variation between 15 and 19.9 plus a Valsalva ratio ≤1.5 or a supine-to-standing drop of 10 mmHg in DBP (20).
Conclusions
This study examined the association between measures of CAN with FSD and UI among a large cohort of women with long-standing T1DM participating in the DCCT/EDIC. We found that CAN was significantly more prevalent among women with FSD and/or UI, because 41% of women with FSD and 44% with UI had positive measures of CAN compared with 30% without FSD and 38% without UI at EDIC year 16/17. We also observed bivariate associations between FSD and several measures of CAN, including R-R variation <15, the mean R-R variation, and Valsalva ratio ≤1.5, some as early as DCCT closeout. Similar associations were observed between CAN and UI at EDIC year 13/14. In multivariable analyses adjusting for known risk factors, such as age, BMI, postmenopausal status, parity, smoking, alcohol consumption, HbA1c, SBP, duration of diabetes, and β-blocker use, lower R-R variation at EDIC year 16/17 was associated with significantly increased odds of FSD, and Valsalva ratio ≤1.5 was associated with increased odds of UI at EDIC year 13/14. Although autonomic dysfunction has been considered an important factor in the etiology of many diabetic complications, including constipation, exercise intolerance, bladder dysfunction, erectile dysfunction, orthostatic hypotension, and impaired neurovascular function, our study is among the first to systematically demonstrate a link between CAN and FSD in a large cohort of well-characterized patients with T1DM (14).
Compared with erectile dysfunction, there are limited studies on the prevalence and predictors of FSD in diabetes. No demographic or macrovascular/microvascular complications have been identified to be predictive of FSD in previous studies (6). Although FSD due to diabetes is likely multifactorial, a neurogenic component has been proposed. A small study found women with diabetes had reduced reflexive capillary engorgement measured by vaginal photoplethysmography in response to erotic stimuli compared with control subjects without diabetes (8). Another study evaluated biothesiometric (vibratory) sensation of multiple genital and extragenital sites among 30 women with diabetes and 20 control subjects (7). Although women with diabetes showed significantly higher mean FSFI-R scores and higher biothesiometric values (reduced sensation) at each genital and extragenital site, there was no significant difference in biothesiometric values between women with diabetes with and without FSD. Notable limitations of previous studies on FSD in women with diabetes include the small number of subjects, incomplete evaluation of associated diabetic complications, use of nonvalidated questionnaires of FSD, and failure to distinguish between type 1 and type 2 diabetes (6). Several of these limitations have been addressed in the current study through use of a well-characterized cohort of women with T1DM and consistent measures of CAN and associated diabetic complications. In contrast to prior studies, 47% of the FSD patients had evidence of CAN at EDIC year 16/17, which is a quite high prevalence overall compared with reported prevalence rates of various forms of autonomic neuropathy in general in other cohorts of T1D and significantly higher compared with those without CAN (32).
Likewise, beyond studies of bladder dysfunction and UI prevalence, limited data are available on mechanisms and predictors of UI among women with diabetes. Mechanistically, alterations in bladder innervation, detrusor smooth muscle function, and urothelial dysfunction may contribute to overall bladder dysfunction and UI (9,10). Physiologic evaluation of autonomic neuropathy in diabetes as a marker of bladder dysfunction has been explored in two previous studies (11,12). In a study of 52 men with diabetes, Bansal et al. (11) reported an association between autonomic and peripheral neuropathy and diabetic cystopathy. Sympathetic skin response and motor and sensory nerve condition studies from the hands and feet were moderately predictive of urodynamic profiles, consistent with diabetic cystopathy. Similarly, Ueda et al. (12) found an association between decreased sympathetic skin response and cystometrogram findings in 23 patients with diabetes and 10 control subjects. However, small sample sizes, underrepresentation of female patients, nonstandardized physiologic evaluations, lack of distinction between type 1 and type 2 diabetes, and the possible confounding relationship with obesity on UI are important limitations of these previous studies.
Therefore, these data demonstrating associations between measures of UI, FSD, and CAN in our study provide new insights into the natural history of various forms of autonomic dysfunction and the role of subclinical changes in measures of CAN that may predict the development of FSD and UI in women with T1DM. Our findings suggest CAN measures may be sensitive markers of FSD and UI and may serve as potential clinical indicators for implementing specific prevention and treatment strategies for FSD and UI among women with T1DM earlier in the course of the disease. However, given that only a few of the CAN metrics were independently predictive of FSD and UI, other factors included in the multivariate models may be contributing to the causal pathway between CAN and these urologic complications.
This study has several limitations. The lack of FSD and UI assessment at DCCT closeout and EDIC year 13/14 and only having concomitant CAN and FSD and UI evaluations at one time point are notable limitations. However, given the mean age of 50.6 ± 7.2 years at EDIC year 17, the prevalence of FSD and UI at DCCT closeout was likely to be very low. An adjustment for specific medications and cardiorespiratory fitness, which may affect heart rate variability, was not made and may confound test measures of CAN. In addition, the cohort primarily included Caucasian women, which limits the generalizability of our results to women with diabetes of other races.
However, strengths of this study include the large sample size of women with T1DM, standardized CAN assessments performed at more than one instance during DCCT and EDIC, FSD and UI assessment using validated questionnaires, and concomitantly obtaining CAN evaluation and FSD and UI assessments at EDIC year 16/17. In addition, patients with T1DM within DCCT/EDIC have been carefully evaluated for many associated cardiovascular risk factors, including blood pressure, lipids, BMI, smoking, and other microvascular and macrovascular complications.
Conclusion
In women with T1DM in the DCCT/EDIC, we found associations of CAN with the development of FSD and UI. CAN and specific measures of CAN, including R-R variation and Valsalva ratio, may predict development of FSD and UI with long-standing T1DM and may be a useful surrogate for generalized diabetic autonomic neuropathy. Future studies evaluating systematic CAN evaluations for development and progression of sexual and urinary dysfunction in diabetes are warranted.
Article Information
Funding. The DCCT/EDIC has been supported by U01 Cooperative Agreement grants (1982–1993, 2011–2016) and contracts (1982–2011) with the Division of Diabetes, Endocrinology, and Metabolic Diseases of the National Institute of Diabetes and Digestive and Kidney Diseases (current grant numbers U01-DK094176 and U01-DK094157) and through support by the National Eye Institute, the National Institute of Neurological Disorders and Stroke, the General Clinical Research Centers Program (1993–2007), and Clinical and Translational Science Center Program (2006–present), Bethesda, MD. Additional support for this DCCT/EDIC collaborative study was provided by an R01 grant (2009–2013) with the National Institute of Diabetes and Digestive and Kidney Diseases (5R01-DK-083927-03).
Industry contributors have had no role in the DCCT/EDIC study but have provided free or discounted supplies or equipment to support participants’ adherence to the study: Abbott Diabetes Care (Alameda, CA), Animas (Westchester, PA), Bayer Diabetes Care (North American Headquarters, Tarrytown, NY), Becton Dickinson (Franklin Lakes, NJ), Eli Lilly (Indianapolis, IN), Extend Nutrition (St. Louis, MO), LifeScan (Milpitas, CA), Medtronic Diabetes (Minneapolis, MN), Nipro Home Diagnostics (Ft. Lauderdale, FL), Nova Diabetes Care (Billerica, MA), Omron (Shelton, CT), OmniPod Insulin Management System (Bedford, MA), Perrigo Diabetes Care (Allegan, MI), Roche Diabetes Care (Indianapolis, IN), and Sanofi (Bridgewater, NJ).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.M.H., E.F., W.H.H., C.L.M., A.M.J., H.W., and R.P.-B. contributed to discussion and reviewed and edited the manuscript. A.V.S. researched data, contributed to discussion, and reviewed and edited the manuscript. D.P.P. wrote and drafted the manuscript. B.H.B. and P.A.C. researched data, contributed to statistical analyses, and reviewed and edited the manuscript. All authors reviewed and approved of the final manuscript. A.V.S. and R.P.-B. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. nos. NCT00360815 and NCT00360893, clinicaltrials.gov.
*A complete list of participants in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group can be found in N Engl J Med 2011;365:2366–2376.
References
- 1.Jacobson AM, Braffett BH, Cleary PA, et al. DCCT/EDIC Research Group . Relationship of urologic complications with health-related quality of life and perceived value of health in men and women with type 1 diabetes: the Diabetes Control and Complications/Epidemiology of Diabetes Interventions and Complications cohort. Diabetes Care 2015;38:1904–1912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pontiroli AE, Cortelazzi D, Morabito A. Female sexual dysfunction and diabetes: a systematic review and meta-analysis. J Sex Med 2013;10:1044–1051 [DOI] [PubMed] [Google Scholar]
- 3.Ogbera AO, Chinenye S, Akinlade A, Eregie A, Awobusuyi J. Frequency and correlates of sexual dysfunction in women with diabetes mellitus. J Sex Med 2009;6:3401–3406 [DOI] [PubMed] [Google Scholar]
- 4.Enzlin P, Rosen R, Wiegel M, et al.; DCCT/EDIC Research Group . Sexual dysfunction in women with type 1 diabetes: long-term findings from the DCCT/ EDIC study cohort. Diabetes Care 2009;32:780–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarma AV, Kanaya AM, Nyberg LM, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group . Urinary incontinence among women with type 1 diabetes--how common is it? J Urol 2009;181:1224–1230; discussion 1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhasin S, Enzlin P, Coviello A, Basson R. Sexual dysfunction in men and women with endocrine disorders. Lancet 2007;369:597–611 [DOI] [PubMed] [Google Scholar]
- 7.Erol B, Tefekli A, Sanli O, et al. Does sexual dysfunction correlate with deterioration of somatic sensory system in diabetic women? Int J Impot Res 2003;15:198–202 [DOI] [PubMed] [Google Scholar]
- 8.Wincze JP, Albert A, Bansal S. Sexual arousal in diabetic females: physiological and self-report measures. Arch Sex Behav 1993;22:587–601 [DOI] [PubMed] [Google Scholar]
- 9.Daneshgari F, Liu G, Birder L, Hanna-Mitchell AT, Chacko S. Diabetic bladder dysfunction: current translational knowledge. J Urol 2009;182(Suppl.):S18–S26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frimodt-Møller C. Diabetic cystopathy. A review of the urodynamic and clinical features of neurogenic bladder dysfunction in diabetes mellitus. Dan Med Bull 1978;25:49–60 [PubMed] [Google Scholar]
- 11.Bansal R, Agarwal MM, Modi M, Mandal AK, Singh SK. Urodynamic profile of diabetic patients with lower urinary tract symptoms: association of diabetic cystopathy with autonomic and peripheral neuropathy. Urology 2011;77:699–705 [DOI] [PubMed] [Google Scholar]
- 12.Ueda T, Yoshimura N, Yoshida O. Diabetic cystopathy: relationship to autonomic neuropathy detected by sympathetic skin response. J Urol 1997;157:580–584 [DOI] [PubMed] [Google Scholar]
- 13.Schönauer M, Thomas A, Morbach S, Niebauer J, Schönauer U, Thiele H. Cardiac autonomic diabetic neuropathy. Diab Vasc Dis Res 2008;5:336–344 [DOI] [PubMed] [Google Scholar]
- 14.Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care 2003;26:1553–1579 [DOI] [PubMed] [Google Scholar]
- 15.Pop-Busui R. Cardiac autonomic neuropathy in diabetes: a clinical perspective. Diabetes Care 2010;33:434–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tesfaye S, Boulton AJ, Dyck PJ, et al.; Toronto Diabetic Neuropathy Expert Group . Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 2010;33:2285–2293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group Epidemiology of Diabetes Interventions and Complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the Diabetes Control and Complications Trial cohort. Diabetes Care 1999;22:99–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Molitch ME, Steffes MW, Cleary PA, Nathan DM; The Diabetes Control and Complications Trial Research Group . Baseline analysis of renal function in the Diabetes Control and Complications Trial [published correction appears in Kidney Int 1993;43:1196]. Kidney Int 1993;43:668–674 [DOI] [PubMed] [Google Scholar]
- 19.Nathan DM, Lachin J, Cleary P, et al.; Diabetes Control and Complications Trial; Epidemiology of Diabetes Interventions and Complications Research Group . Intensive diabetes therapy and carotid intima-media thickness in type 1 diabetes mellitus. N Engl J Med 2003;348:2294–2303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pop-Busui R, Low P, Waberski B, et al.DCCT/EDIC Research Group . Effects of prior intensive insulin therapy on cardiac autonomic nervous system function in type 1 diabetes mellitus: the DCCT/EDIC Study. Circulation 2009;119:2886–2893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albers J, Herman W, Pop-Busui R, et al. Effect of prior intensive insulin treatment during the DCCT on peripheral neuropathy in type 1 diabetes during the EDIC Study. Diabetes Care 2010;33:1090–1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wessells H, Penson DF, Cleary P, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group . Effect of intensive glycemic therapy on erectile function in men with type 1 diabetes. J Urol 2011;185:1828–1834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Den Eeden SK, Sarma AV, Rutledge BN, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Research Group . Effect of intensive glycemic control and diabetes complications on lower urinary tract symptoms in men with type 1 diabetes: Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) study. Diabetes Care 2009;32:664–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosen R, Brown C, Heiman J, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 2000;26:191–208 [DOI] [PubMed] [Google Scholar]
- 25.Sandvik H, Hunskaar S, Vanvik A, Bratt H, Seim A, Hermstad R. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. J Clin Epidemiol 1995;48:339–343 [DOI] [PubMed] [Google Scholar]
- 26.The Diabetes Control and Complications Trial Research Group The effect of intensive diabetes therapy on measures of autonomic nervous system function in the Diabetes Control and Complications Trial (DCCT). Diabetologia 1998;41:416–423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spallone V, Ziegler D, Freeman R, et al.; Toronto Consensus Panel on Diabetic Neuropathy . Cardiovascular autonomic neuropathy in diabetes: clinical impact, assessment, diagnosis, and management. Diabetes Metab Res Rev 2011;27:639–653 [DOI] [PubMed] [Google Scholar]
- 28.Low PA, Denq JC, Opfer-Gehrking TL, Dyck PJ, O’Brien PC, Slezak JM. Effect of age and gender on sudomotor and cardiovagal function and blood pressure response to tilt in normal subjects. Muscle Nerve 1997;20:1561–1568 [DOI] [PubMed] [Google Scholar]
- 29.Gelber DA, Pfeifer M, Dawson B, Schumer M. Cardiovascular autonomic nervous system tests: determination of normative values and effect of confounding variables. J Auton Nerv Syst 1997;62:40–44 [DOI] [PubMed] [Google Scholar]
- 30.Barrett-Connor E, Kritz-Silverstein D, Edelstein SL. A prospective study of dehydroepiandrosterone sulfate (DHEAS) and bone mineral density in older men and women. Am J Epidemiol 1993;137:201–206 [DOI] [PubMed] [Google Scholar]
- 31.Chobanian AV, Bakris GL, Black HR, et al.; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 32.Tesfaye S, Stevens LK, Stephenson JM, et al. Prevalence of diabetic peripheral neuropathy and its relation to glycaemic control and potential risk factors: the EURODIAB IDDM Complications Study. Diabetologia 1996;39:1377–1384 [DOI] [PubMed] [Google Scholar]