Abstract
Homozygous truncating mutations in the helix-loop-helix transcription factor PTF1A are a rare cause of pancreatic and cerebellar agenesis. The correlation of Ptf1a dosage with pancreatic phenotype in a mouse model suggested the possibility of finding hypomorphic PTF1A mutations in patients with pancreatic agenesis or neonatal diabetes but no cerebellar phenotype. Genome-wide single nucleotide polymorphism typing in two siblings with neonatal diabetes from a consanguineous pedigree revealed a large shared homozygous region (31 Mb) spanning PTF1A. Sanger sequencing of PTF1A identified a novel missense mutation, p.P191T. Testing of 259 additional patients using a targeted next-generation sequencing assay for 23 neonatal diabetes genes detected one additional proband and an affected sibling with the same homozygous mutation. All four patients were diagnosed with diabetes at birth and were treated with insulin. Two of the four patients had exocrine pancreatic insufficiency requiring replacement therapy but none of the affected individuals had neurodevelopmental delay. Transient transfection assays of the mutant protein demonstrated a 75% reduction in transactivation activity. This study shows that the functional severity of a homozygous mutation impacts the severity of clinical features found in patients.
Introduction
Homozygous truncating mutations in the basic helix-loop-helix transcription factor PTF1A cause pancreatic agenesis and very severe neurodevelopmental problems, including central hypoventilation and total cerebellar agenesis (1–3), and all six affected individuals from four families showed a high degree of phenotypic concordance and none survived for more than 4 months.
A combined linkage, genome sequencing, and epigenomic annotation strategy recently identified homozygous mutations in a novel enhancer located 25 kb downstream from the PTF1A gene (4). Patients with biallelic mutations in this enhancer have isolated pancreatic agenesis without cerebellar involvement. Sparing of the cerebellum suggests that the enhancer is tissue specific to the pancreas.
A mouse model relating Ptf1a dosage to pancreatic phenotype (5) resulted in pancreatic hypoplasia and glucose intolerance in a dosage-dependent manner. The pancreatic phenotype consisted of reduced pancreatic bud size, misspecification of pancreatic progenitors, reduced branching morphogenesis of the exocrine pancreas, and a reduction in the ratio of β-cells to non–β-cells in pancreatic islets. In this model system, Ptf1a RNA levels were correlated with the endocrine and exocrine pancreatic phenotype.
Biallelic mutations in a second transcription factor gene, PDX1, also result in nonsyndromic pancreatic agenesis and have been identified in three unrelated cases (6–8). Hypomorphic mutations result in neonatal diabetes in the absence of exocrine pancreatic insufficiency (9,10). A hypomorphic mutation in the transcription factor gene Pdx1 in mice has also been modeled (11) and been shown to play a role in the transition from pancreatic progenitor to endocrine progenitor, with a reduction in the number of endocrine lineages.
To date, no PTF1A coding hypomorphic mutations have been identified. We now report four individuals from two separate sibships in each of whom the same novel PTF1A coding mutation, p.P191T, was identified. All four individuals were diagnosed with neonatal diabetes, but cerebellar pathology was absent. We performed functional studies on this mutation to investigate our hypothesis that p.P191T is a hypomorphic PTF1A mutation.
Research Design and Methods
Genetics
Homozygosity Mapping
Homozygosity mapping was carried out as described previously (12) in one patient with pancreatic agenesis of unknown etiology and their sibling with neonatal diabetes. Pancreatic agenesis was defined as neonatal diabetes requiring insulin treatment and exocrine pancreatic insufficiency defined as requiring enzyme replacement therapy (13).
Next-Generation Sequencing Assay
A targeted next-generation sequencing assay was used to sequence PTF1A and 22 other genes in which mutations have been reported to cause neonatal diabetes (14). We sequenced DNA samples from 259 probands with neonatal diabetes diagnosed before 6 months and no known genetic etiology. Nine of these patients had pancreatic agenesis. Mutations in ABCC8, KCNJ11, and INS had previously been excluded by Sanger sequencing. We had also excluded EIF2AK3 mutations in patients born to consanguineous parents.
Sanger Sequencing
Mutations were confirmed by PCR/Sanger sequencing and tested in other relatives.
Functional Work
Cell Transfections
The reporter plasmids Ela1p.luc, with a minimal promoter directing the luciferase gene of pGL3 basic, and 3Rbpjl.Ela1p.luc, with three tandem repeats of the proximal PTF1 binding site of the Rbpj1 gene upstream of Ela1p.luc, have been described (15). The p.P191T mutation was introduced into the human PTF1A coding sequence by site-directed mutagenesis as previously described (16). DNA was introduced into the human embryonic kidney (HEK) 293 cell line (CRL-1573; American Type Culture Collection) with FuGene 6 (Roche, Indianapolis, IN), according to the manufacturer’s instructions. All transfections were normalized based on the β-galactosidase activity of a cotransfected reporter plasmid, pCMVbeta (Clontech, Mountain View, CA).
Electrophoretic Mobility Shift Assays
The subunits of PTF1 were synthesized by in vitro transcription and translation using a TnT Coupled Reticulocyte Lysate System (Promega, Madison, WI). The wild-type and p.P191T mutant PTF1A plasmids described above were also used for in vitro protein synthesis. The plasmid bearing human RBPJ has previously been described (16). The expression plasmid bearing a partial human E12/TCF3 cDNA in pCITE2a was a gift from Eric Olson, of The University of Texas Southwestern Medical Center, and was originally derived from E12R (20). The products of in vitro transcription and translation were quantified by [35S]methionine incorporation and adjustment according to the number of methionine residues in each protein.
Electrophoretic mobility shift assays (EMSAs) were performed with the method of Sawada and Littman (17) with slight modifications. The double-stranded oligonucleotide probe encompassed the proximal PTF1 binding site of the mouse Rbpjl gene (15) and was 5′-end labeled with 32P. The sequence of the top strand is GACACCTGCTGGGCAGATGTAGGCTTCCCACGG. ImageQuant software was used to analyze Phosphorimager scans of the EMSA gels (GE Healthcare, Life Sciences, Pittsburgh, PA).
Results
Homozygosity analysis of genome-wide single nucleotide polymorphisms identified a homozygous region (31 Mb) on chromosome 10 that was shared between two affected siblings born to consanguineous parents. Sanger sequencing of PTF1A identified a novel homozygous missense mutation, p.P191T (c.571C>A; p.Pro191Thr), in both siblings. Analysis of PTF1A by targeted next-generation sequencing of nine patients with pancreatic agenesis identified one additional proband with the p.P191T mutation. This patient’s affected sibling was also homozygous for p.P191T. No additional PTF1A mutations were identified in a further 259 patients with neonatal diabetes.
P191T Mutation Characteristics
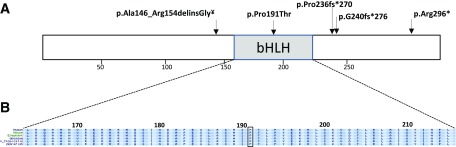
The p.P191 residue is located in the highly conserved helix-loop-helix domain that is critical for dimerization and DNA binding (Fig. 1). The p.P191T missense variant is not present in any public variant databases (1000 Genomes, NHLBI Exome Sequencing Project Exome Variant Server, or ExAC Browser). In silico analysis by SIFT and PolyPhen predicts the variant to be pathogenic. All four affected patients were homozygous for the p.P191T mutation and their parents were heterozygous carriers. The patients are from Saudi Arabia and Kuwait, raising the possibility of a founder mutation. Analysis of microsatellite markers flanking PTF1A showed a shared haplotype of 8 Mb (data not shown), consistent with a founder mutation segregating in the two families.
Figure 1.
A: Schematic representation of the PTF1A protein and location of the mutations identified in all previously reported cases (1–3) and the p.P191T mutation found in the four current cases. B: Amino acid conservation in the bHLH domain. The p.P191T is the only missense mutation identified to date. It is located at a conserved residue within the basic helix-loop-helix (bHLH) domain (highlighted). ¥The p.Ala146_Arg154delinsGly mutation was previously reported as c.437_460del, p.Ala146_Arg154delfsX115 (3).
Clinical Characteristics of Patients With Homozygous P191T Mutation
The male proband in family I (I-1) was the first child born to first cousins of Arabic descent with a birth weight of 1.98 kg at 38 weeks’ gestation. He was noted to be hyperglycemic (350 mg/dL) on the first day of life while on a glucose infusion, which was discontinued and an insulin infusion commenced for 20 h. On day 6, when on no treatment, his plasma glucose remained high (240 mg/dL) with low insulin of 0.1 μU/L (normal range 1.4–14) and C-peptide of 0.1 ng/mL (normal range 0.9–4.3), confirming a diagnosis of neonatal diabetes. Insulin was recommended at 2 months of age as most of his glucose values were 200–300 mg/dL and his HbA1c was 7%. The treatment has continued, with HbA1c 8.1%. The baby continued to have poor weight gain despite recommencing insulin and steatorrhea was observed, suggesting pancreatic insufficiency, which was confirmed by elevated fecal fat, elevated stool chymotrypsin, and low serum trypsinogen (Table 1). Exocrine pancreatic replacement therapy was initiated at 3 months of age. Other clinical features were a small patent ductus arteriosus and a small atrial septal defect, which were detected by echo after a cardiac murmur was noted; these did not require any intervention.
Table 1.
Clinical characteristics of patients studied
| I-1 | I-2 | II-1 | II-2 | |
|---|---|---|---|---|
| Present age | 12 years | 9 years | Deceased at 12 weeks due to sepsis | 2 years |
| Sex | Male | Female | Male | Female |
| Country of origin | Saudi Arabia | Saudi Arabia | Kuwait | Kuwait |
| Birth weight (g) | 1,980 | 2,000 | 1,275 | 1,400 |
| Percentile | 0.4 | 2 | 0.1 | <0.1 |
| Gestational age | 38 weeks | 37 weeks | 34 weeks | 36 weeks |
| Age at diabetes diagnosis/ age of permanent insulin therapy | 1 day/2 months | 1 day/4 months | 1 day/1 day | 8 days/8 days |
| Diabetes treatment | Insulin | Insulin | Insulin | Insulin |
| Exocrine pancreatic insufficiency requiring replacement? | Yes | No | Yes | Yes |
| Clinical basis of exocrine insufficiency | Steatorrhea, failure to thrive | No symptoms of exocrine insufficiency | Failure to thrive | Steatorrhea, failure to thrive |
| Biochemical basis of exocrine insufficiency | Fecal fat: 3 g/24 h stool Stool chymotrypsin: 1 U/g (normal range 4–10 U/g) Serum trypsinogen: 4 μg/L (normal range 15–25 μg/L) | Fecal fat: 0.5 g/24 h Stool chymotrypsin: 5 U/g (4–10 U/g) Serum trypsinogen: 18 μg/L (15–25 μg/L) | Fecal elastase: undetectable (>200 μg elastase/g stool) | |
| Exocrine pancreatic replacement regimen | 10,000 U/day of lipase | None | 15,000 U/day of lipase | |
| Age at initiation of exocrine pancreatic replacement | 12 weeks | Not applicable | Not applicable | 10 weeks |
| Clinical neurocognitive function | Normal neurocognitive development with some disruption of eye movements on tracking | Normal neurocognitive development | Normal neurocognitive development | |
| Brain imaging | Not performed | Not performed | Not performed | Normal (MRI) |
His younger sister (I-2) was born at 37 weeks’ gestation with a birth weight 2.00 kg. Diabetes was diagnosed on the first day of life with a glucose of 300 mg/dL and and she was treated with insulin for 4 days. Insulin was commenced at 4 months due to consistently high blood glucose values (>200 mg/dL) and HbA1c of 7%; the treatment has continued with HbA1c 7–8%. Exocrine pancreatic supplementation has not been required and biochemical parameters (fecal fat, stool chymotrypsin, and serum trypsinogen) are within normal limits, albeit at the lower limit of the normal range (Table 1).
Ultrasound scanning of the abdomen of the two siblings in family I was performed in the first week of life and showed normal liver and contracted gallbladder but failed to identify the pancreas. Parents declined further imaging of the abdomen.
Both siblings in family I underwent detailed neurodevelopmental assessment by a neurodevelopmental pediatrician at the age of 12 years in the older and at 9 years in the younger sibling. Evaluation revealed normal neurological examination apart from searching eye movements with horizontal nystagmus in patient I-1. There are no other clinical abnormalities referable to cerebellar function. Parents declined to perform brain MRIs. The rest of the clinical neurodevelopmental assessment was age-appropriate, including vision, hearing, expressive and receptive language, gross motor and fine motor skills, social skills, and school performance. Their clinical neurodevelopmental assessment is similar to their unaffected siblings. However, formal neuropsychological testing was not performed.
The male proband in family II (II-1) was the first child born to consanguineous parents of Arabic descent. Birth weight was 1.275 kg at 34 weeks’ gestation. Neonatal diabetes was diagnosed on the first day of life and treated with insulin. There was severe failure to thrive gaining only 250 g in the first 12 weeks of life, but biochemical tests for pancreatic malabsorption were not performed. The patient died of necrotizing enterocolitis and overwhelming sepsis at the age of 12 weeks. No further clinical details are available.
His younger sibling is a female child (II-2) born at 36 weeks’ gestation with a birth weight 1.40 kg. Neonatal diabetes was diagnosed at the age of 8 days and treated with insulin. She failed to thrive and fecal elastase was undetectable, confirming a diagnosis of exocrine pancreatic insufficiency. Exocrine replacement therapy was initiated at 10 weeks of age. Neurocognitive development and neurological examination are normal at the age of 2 years. Brain and cerebellar MRI scan was normal at 3 months of age.
Functional Work
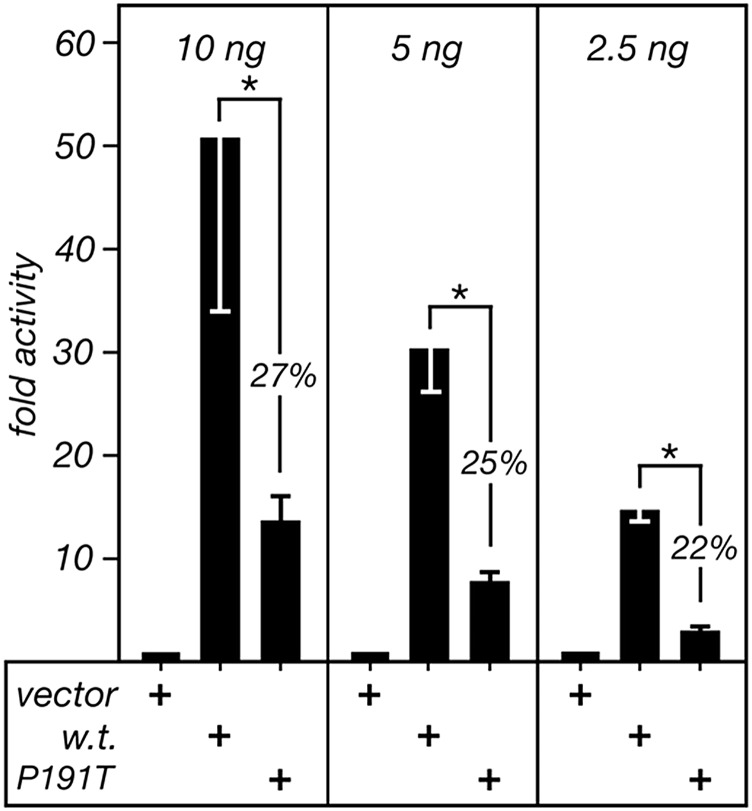
Transfection of the p.P191T mutation into HEK293 cells resulted in a 75% reduction in transcriptional activity compared with the wild-type protein (Fig. 2). A range in the amount of expression plasmids was tested to ensure that the activities of the wild-type plasmids were proportional to the plasmid quantity and, thus, not saturated in the assay. The mean ± SD activity of the mutant PTF1A at three different concentrations within the linear range was 25 ± 4.9% of the activity of the wild-type protein (P < 0.001) (Fig. 2).
Figure 2.
The activity of human PTF1A-P191T in transfected cells. The reporter plasmid 3Rbpjl.Ela1p.luc was cotransfected with expression plasmids for wild-type (w.t.) PTF1A, PTF1A-P191T, or an insertless vector into HEK293 cells. Three different amounts of each expression plasmid were used to determine whether response was proportional to plasmid quantity and, therefore, that the proteins produced were not in excess. Four independent transfections were analyzed for 10 and 5 ng and two for 2.5 ng. Error bars are SD. The asterisks indicate P values <0.05 for each pairwise comparison.
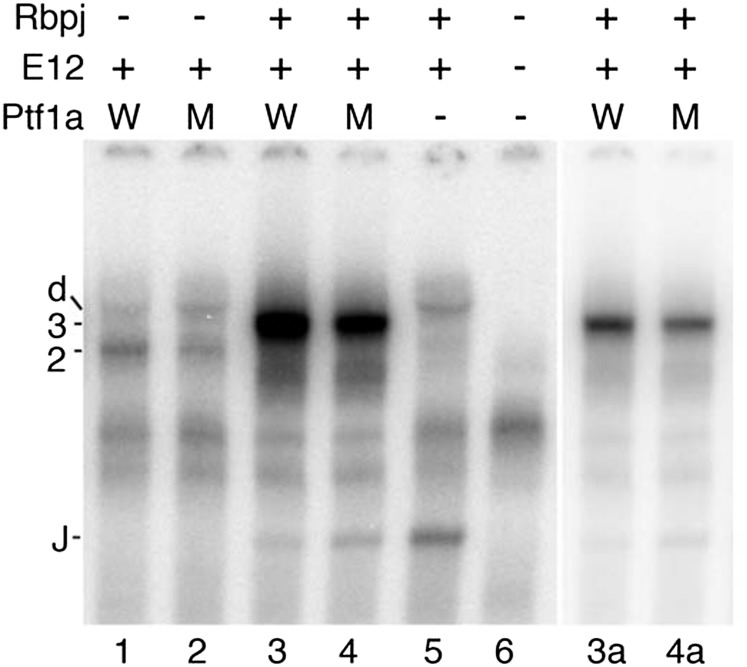
To determine the DNA binding characteristics of human PTF1A-P191T relative to wild type, EMSAs were performed with an Rbpjl proximal PTF1 binding site as the radiolabeled probe (Fig. 3). For the PTF1A:E12 dimer, the binding of the p.P191T mutant was 34 ± 7% of wild type (n = 3), whereas for the PTF1A:E12:RBPJ trimer, the binding of the p.P191T mutant was 88 ± 19% of wild type (n = 4).
Figure 3.
The DNA binding of wild-type PTF1A and PTF1A-P191T as part of the PTF1A:E12 dimer or PTF1A:E12:RBPJ trimer in EMSA. The relative abilities of wild-type and p.P191T mutant PTF1A to form complexes with E12 and RBPJ on the PTF1 binding site of the Rbpj1 gene was tested in vitro. Lanes 3a and 4a show lanes 3 and 4 with an expanded grayscale such that the PTF1 trimeric complex bands are not saturated. PTF1A alone does not bind DNA. 2, PTF1A:E12 dimer; 3, PTF1A:E12:RBPJ trimer; d, E12 homodimer; J, RBPJ monomer; M, p.P191T mutant; W, PTF1A wild type.
Discussion
We report a novel hypomorphic homozygous PTF1A mutation in four affected individuals from two families who are likely to have inherited the mutation from a common distant ancestor. The clinical phenotype is of neonatal diabetes with reduced exocrine function and normal neurological function and appearance. This clinical phenotype is distinct from the previously reported syndrome caused by homozygous PTF1A truncating mutations where all six patients (from four families) died in the first 4 months of life (1–3) of severe neurological complications and had pancreatic and cerebellar agenesis. In vitro functional studies are consistent with the p.P191T missense mutation being a hypomorphic mutation.
The main clinical feature of homozygosity for the p.P191T missense mutation is pancreatic aplasia/hypoplasia. All four patients had neonatal diabetes and two of the four have clinical and biochemical evidence of clinically significant exocrine dysfunction of the pancreas requiring replacement therapy. The third patient had clinical features suggestive of exocrine insufficiency but died of sepsis at the age of 12 weeks, and the fourth patient had diabetes requiring insulin treatment but no clinical features of exocrine failure, albeit with pancreatic enzyme levels close to the lower limit of the normal range.
All four patients had normal neurological development and function. This is in contrast to the patients with homozygous null PTF1A mutations who had very severe neurological developmental problems, central hypoventilation, and total cerebellar agenesis. One patient had some disrupted eye movements, but the phenotype was not consistent with significant cerebellar dysfunction. A normal cerebellum was seen in the patient who had brain imaging.
The moderate phenotypic variability seen in these four patients is also seen in patients who have other pancreatic transcription factor mutations affecting the pancreatic stem cell. Different phenotypes due to the same mutation are seen in patients with mutations in GATA6 (18) and HNF1B (19). Phenotypic variability is also seen in patients with mutations in the homeodomain transcription factor PDX1: biallelic mutations in this gene have been reported in patients with pancreatic agenesis (6–8), neonatal diabetes with biochemical but not clinical evidence of exocrine insufficiency (9,10), and neonatal diabetes with normal exocrine function, both clinically and biochemically (10).
The p.P191T missense mutation is located in the highly conserved helix-loop-helix domain of PTF1A, a region that is critical for dimerization with a common basic helix-loop-helix E-protein, such as E12/E47, and DNA binding. Proline 191 terminates helix 1, and substitution of threonine at that position could favor the extension of the first α-helix almost a full turn and thereby shorten the loop region, misposition the second α-helix, and make binding to the E-protein partner less favorable. Indeed, in vitro functional studies demonstrated an effect on DNA binding and that transactivation activity was reduced by 75% compared with the wild-type protein. This residual activity is consistent with p.P191T being a hypomorphic mutation.
Reduced Ptf1a dosage in a mouse model (5) resulted in pancreatic hypoplasia and glucose intolerance in a dosage-dependent manner. In hypomorphic mutant mice, pancreatic bud size was small and substantial proportions of pancreatic progenitors were misspecified to the common bile duct and duodenal cells. Exocrine pancreatic branching morphogenesis was reduced, and there was a reduction in the ratio of β-cells to non–β-cells in pancreatic islets. In this model system, Ptf1a RNA levels could be correlated with the endocrine and exocrine pancreatic phenotype. We have clearly shown a similar correlation between mutation severity and phenotype in humans.
We conclude that hypomorphic PTF1A missense mutations can cause isolated pancreatic agenesis or neonatal diabetes. Hypomorphic mutations in this gene should be considered in patients presenting with diabetes in the neonatal period.
Article Information
Acknowledgments. The authors thank the families for participating in this study. They are grateful to Annet Damhuis and Anna-Maria Bussell and the Research Center, College of Medicine, King Saud University for their technical assistance and to Ward Coats (Department of Molecular Biology, The University of Texas Southwestern Medical Center) for helpful discussions regarding PTF1A structure.
Funding. G.H.S. and R.J.M. were supported by a National Institutes of Health grant R01-DK061220. A.T.H. and S.E. are the recipients of a Wellcome Trust Senior Investigator award, which funded the genetic/clinical part of this study (WT098395). A.T.H. is employed as a core member of staff within the National Institute for Health Research (NIHR)-funded Exeter Clinical Research Facility and is an NIHR senior investigator.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.A.L.H., S.E.F., E.d.F., R.C., and S.E. designed, performed, and interpreted the genetic studies. C.S.-S., K.H., S.M., M.A., and A.T.H. designed and performed the clinical studies. G.H.S. and R.J.M. designed, performed, and interpreted the functional studies. J.A.L.H. and G.H.S. wrote the first draft of the manuscript with input from A.T.H., R.J.M., and S.E. All authors reviewed and commented on the draft manuscript and reviewed the submitted manuscript. S.E. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Sellick GS, Barker KT, Stolte-Dijkstra I, et al. . Mutations in PTF1A cause pancreatic and cerebellar agenesis. Nat Genet 2004;36:1301–1305 [DOI] [PubMed] [Google Scholar]
- 2.Tutak E, Satar M, Yapicioğlu H, et al. . A Turkish newborn infant with cerebellar agenesis/neonatal diabetes mellitus and PTF1A mutation. Genet Couns 2009;20:147–152 [PubMed] [Google Scholar]
- 3.Al-Shammari M, Al-Husain M, Al-Kharfy T, Alkuraya FS. A novel PTF1A mutation in a patient with severe pancreatic and cerebellar involvement. Clin Genet 2011;80:196–198 [DOI] [PubMed] [Google Scholar]
- 4.Weedon MN, Cebola I, Patch AM, et al.; International Pancreatic Agenesis Consortium . Recessive mutations in a distal PTF1A enhancer cause isolated pancreatic agenesis. Nat Genet 2014;46:61–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fukuda A, Kawaguchi Y, Furuyama K, et al. . Reduction of Ptf1a gene dosage causes pancreatic hypoplasia and diabetes in mice. Diabetes 2008;57:2421–2431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stoffers DA, Zinkin NT, Stanojevic V, Clarke WL, Habener JF. Pancreatic agenesis attributable to a single nucleotide deletion in the human IPF1 gene coding sequence. Nat Genet 1997;15:106–110 [DOI] [PubMed] [Google Scholar]
- 7.Schwitzgebel VM, Mamin A, Brun T, et al. . Agenesis of human pancreas due to decreased half-life of insulin promoter factor 1. J Clin Endocrinol Metab 2003;88:4398–4406 [DOI] [PubMed] [Google Scholar]
- 8.Thomas IH, Saini NK, Adhikari A, et al. . Neonatal diabetes mellitus with pancreatic agenesis in an infant with homozygous IPF-1 Pro63fsX60 mutation. Pediatr Diabetes 2009;10:492–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Franco E, Shaw-Smith C, Flanagan SE, et al. . Biallelic PDX1 (insulin promoter factor 1) mutations causing neonatal diabetes without exocrine pancreatic insufficiency. Diabet Med 2013;30:e197–e200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nicolino M, Claiborn KC, Senée V, Boland A, Stoffers DA, Julier C. A novel hypomorphic PDX1 mutation responsible for permanent neonatal diabetes with subclinical exocrine deficiency. Diabetes 2010;59:733–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oliver-Krasinski JM, Kasner MT, Yang J, et al. . The diabetes gene Pdx1 regulates the transcriptional network of pancreatic endocrine progenitor cells in mice. J Clin Invest 2009;119:1888–1898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubio-Cabezas O, Minton JA, Kantor I, Williams D, Ellard S, Hattersley AT. Homozygous mutations in NEUROD1 are responsible for a novel syndrome of permanent neonatal diabetes and neurological abnormalities. Diabetes 2010;59:2326–2331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lango Allen H, Flanagan SE, Shaw-Smith C, et al.; International Pancreatic Agenesis Consortium . GATA6 haploinsufficiency causes pancreatic agenesis in humans. Nat Genet 2011;44:20–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellard S, Lango Allen H, De Franco E, et al. . Improved genetic testing for monogenic diabetes using targeted next-generation sequencing. Diabetologia 2013;56:1958–1963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masui T, Long Q, Beres TM, Magnuson MA, MacDonald RJ. Early pancreatic development requires the vertebrate Suppressor of Hairless (RBPJ) in the PTF1 bHLH complex. Genes Dev 2007;21:2629–2643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beres TM, Masui T, Swift GH, Shi L, Henke RM, MacDonald RJ. PTF1 is an organ-specific and Notch-independent basic helix-loop-helix complex containing the mammalian Suppressor of Hairless (RBP-J) or its paralogue, RBP-L. Mol Cell Biol 2006;26:117–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawada S, Littman DR. A heterodimer of HEB and an E12-related protein interacts with the CD4 enhancer and regulates its activity in T-cell lines. Mol Cell Biol 1993;13:5620–5628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Franco E, Shaw-Smith C, Flanagan SE, Shepherd MH, Hattersley AT, Ellard S; International NDM Consortium . GATA6 mutations cause a broad phenotypic spectrum of diabetes from pancreatic agenesis to adult-onset diabetes without exocrine insufficiency. Diabetes 2013;62:993–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edghill EL, Stals K, Oram RA, Shepherd MH, Hattersley AT, Ellard S. HNF1B deletions in patients with young-onset diabetes but no known renal disease. Diabet Med 2013;30:114–117 [DOI] [PubMed] [Google Scholar]
- 20.Murre C, McCaw PS, Baltimore D. A new DNA binding and dimerization motif in immunoglobulin enhancer binding, daughterless, MyoD, and myc proteins. Cell 1989;56:777–783 [DOI] [PubMed] [Google Scholar]