Abstract
This study tested an innovative model for creating consumer-level content about precision medicine based on health literacy and learning style principles. “Knowledge pearl” videos, incorporating multiple learning modalities, were created to explain genetic and cancer medicine concepts. Cancer patients and caregivers (n=117) were randomized to view professional-level content directly from the My Cancer Genome (MCG) website (Group A; control), content from MCG with knowledge pearls embedded (Group B), or a consumer translation, targeted at the sixth grade level, with knowledge pearls embedded (Group C). A multivariate analysis showed that Group C, but not Group B, showed greater knowledge gains immediately after viewing the educational material than Group A. Statistically significant group differences in test performance were no longer observed three weeks later. These findings suggest that adherence to health literacy and learning style principles facilitates comprehension of precision medicine concepts and that ongoing review of the educational information is necessary.
Introduction
New initiatives for precision medicine come with greater opportunities for patients to receive truly individualized care. Oncology is at the forefront of precision medicine1, as new molecular targeted therapies and immunotherapies are increasingly used to treat cancer patients, including patients with melanoma2, lung cancer3, and renal cell carcinoma4. However, for the goals of precision cancer medicine to fully be realized, more genomic and clinical trial data must be collected, and the resulting knowledge must be properly communicated1. Patients will also increasingly need to be able to understand genetic testing results to fully comprehend their treatment options.
One barrier to the implementation of precision cancer medicine is a lack of understanding about basic genetic concepts5. Adults often have difficulty understanding genes, chromosomes, and other aspects of genetics6,7. National K-12 genetics standards do not currently cover important genetic concepts, such as mutations or gene expression and regulation, and interpretation of these standards may lead to wide variation in how and to what extent educators teach the included concepts8. Genetic knowledge deficits can be particularly detrimental to patients’ ability to understand and give informed consent for genetic testing9,10 or genomic sequencing11.
In light of these widespread deficits, easy-to-understand resources about precision medicine are needed. My Cancer Genome (MCG; mycancergenome.org) is a premier online informatics resource for precision cancer medicine knowledge providing information on therapies for specific tumor mutations12. Although it is written at the health professional-level, patients and caregivers still access the website. Other online resources available to patients include the National Library of Medicine’s Genetics Home Reference13, Massachusetts General’s Targeted Cancer Care website14, and 23andMe’s “Genetics 101” videos15. Approximately 36% of American adults have basic or inadequate health literacy. A lack of understanding about basic genetic concepts and low health literacy, defined as “the ability to use literacy skills to read and understand written health-related information encountered in everyday life”16, may make these resources difficult to understand17.
We conducted a set of studies to evaluate a model, incorporating health literacy and learning style principles, for delivering information about precision cancer medicine therapies to patients and caregivers. In the first study, conducted in fall of 201418 we developed a consumer translation of information from My Cancer Genome regarding the BRAF V600E mutation in melanoma. The content was adapted to the sixth grade reading level and designed to incorporate preferences for learning via several learning style modalities, including preferences for learning via reading, listening, and watching. The material contained hyperlinks to videos, called knowledge pearls, that were developed to provide easy-to-understand explanations of genetic and cancer medicine concepts. Using a randomized, controlled study design, we found that the consumer version of the information was more effective in educating melanoma patients about the BRAF V600E mutation in melanoma than the My Cancer Genome website version with or without the knowledge pearls embedded. Learning was assessed by administering a knowledge questionnaire before and immediately after viewing the educational content.
In this study, building on the above-mentioned findings, we tested the generalizability of the model for delivering consumer-friendly information about precision medicine. We also assessed whether the changes in knowledge were long-lasting. Content from MCG about targeted therapies and immunotherapies was used for the evaluation because of these topics’ broad applicability to multiple cancer types. The information was translated into a consumer-friendly format and hyperlinks to knowledge pearl videos were added to both the consumer and professional-level versions. A randomized, controlled study design with cancer patients and caregivers was used to evaluate differences in educational outcomes. We hypothesized that participants who received the consumer-friendly content with knowledge pearls would show greater improvements in knowledge test scores than participants who received the professional-level information with or without links to the knowledge pearls.
Methods
The study protocol was approved by the Vanderbilt University Institutional Review Board and the Vanderbilt-Ingram Cancer Center Scientific Review Committee.
Setting
This study was conducted at the Vanderbilt-Ingram Cancer Center (VICC). A member of the National Comprehensive Cancer Network and designated by the National Cancer Institute as a Comprehensive Cancer Center, the VICC is on the cutting edge of new cancer therapies. The VICC is ranked in the top 10 nationally for grant support of cancer research and regularly has access to over 150 clinical trials19. Members of the VICC team developed the My Cancer Genome website and collaborated in the creation of the consumer-level content.
Participants
Patients and caregivers from the melanoma, lung cancer, and renal cancer clinics at the Vanderbilt-Ingram Cancer Center were recruited from April 16 - May 15, 2015. To be eligible, participants had to be 18 or older, be able to read and speak English, and either be a patient with melanoma, lung cancer, or renal cancer or be the caregiver for a participating patient. Exclusion criteria were imprisonment or cognitive impairment as determined by the clinical provider.
Study Design
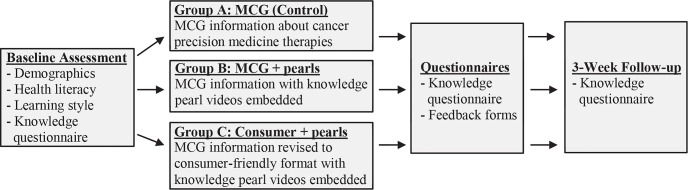
After obtaining informed consent, participants were randomized equally to one of three groups (Figure 1): Group A (control) received information on targeted therapies and immunotherapy in cancer taken directly from My Cancer Genome (http://www.mc.vanderbilt.edu/km/gl/pm/pmc-mcg.html); Group B received the same information from MCG embedded with hyperlinks to the knowledge pearl videos (http://www.mc.vanderbilt.edu/km/gl/pm/pmc-mcg-p.html); Group C received a consumer-level version of the information from MCG, including hyperlinks to the knowledge pearls (http://www. mc.vanderbilt.edu/km/gl/pm/pmc -c. html).
Figure 1.
Overview of Study Design
Randomization was carried out using stratified permuted-block randomization with a block size of 3. Stratification factors included “time since diagnosis disease” (within 12 months, 13 to 24 months, or over 24 months) and “type of study participant” (patient or caregiver). Treatment assignments were implemented using the randomization module in REDCap (Research Electronic Data Capture), a secure, web-based research data management tool developed at Vanderbilt University20.
Participants were asked to provide information about age, race, gender, education level, occupation status, participant status (cancer patient or caregiver), and contact information. They were also asked to complete a subjective health literacy assessment, consisting of 3 questions21 and to answer whether they would recall how to do something a year from now if they learned it by reading, listening, watching, and/or doing. Additionally, information about time since diagnosis, cancer stage, whether or not tumor profiling had been done, length of time as a Vanderbilt patient, and any current precision medicine therapies was determined via medical record review in StarPanel, VUMC’s electronic medical record system22.
To assess changes in knowledge, we developed a 10-item knowledge questionnaire, which included multiple choice and true/false questions about precision medicine therapies (http://tiny.mc.vanderbilt.edu/questionnaire). The information needed to answer questionnaire items was addressed in all three versions of the educational material. Participants were initially asked to complete the questionnaire prior to viewing the educational material. They were then given the educational materials to view on an iPad. Web analytics data were collected during this session to assess intervention fidelity. Immediately after participants viewed the educational information, we re-administered the knowledge questionnaire.
After completing the post-test, participants were asked to rate their level of agreement, with answer choices strongly disagree, disagree, neither agree or disagree, agree, or strongly agree, with the following statements: the information I received was easy to understand; some of the information I received was confusing; I am satisfied with the information I received; the information I received taught me something new. Participants in Groups B and C were additionally asked to rate their agreement about whether the videos (“knowledge pearls”) helped them understand the information they received, were easy to understand, or were confusing.
Participants were given a print copy of the materials they viewed to take home. Each handout also included a link to the online version of the content they viewed to allow participants to review the material after the clinic visit.
To assess participants’ retention of any knowledge gains over time, we re-administered the knowledge questionnaire during a follow-up phone call about three weeks later. During the follow-up call, participants were also asked if they read the handout they were given or visited the website address provided on the handout since leaving the clinic. Finally, they were given an opportunity to share any additional thoughts about the information they received. The phone calls were conducted from May 7 - June 11, 2015. Participants who completed the study received a $25 gift card.
Development of Intervention Materials
Information from MCG, which was written at the college level, regarding the use of precision medicine in cancer was translated into a consumer-friendly format using an iterative process developed and refined in previous research phases18,23. Briefly, the consumer-level content was aimed at the sixth grade reading level and informed by health literacy best practices. The scripts for the knowledge pearl videos were also targeted at the sixth grade reading level. The MCG knowledge pearl videos were each approximately one to two minutes long and incorporated multiple learning styles through the use of video, images, text, and narration. In creating the knowledge pearls, we chose to focus on fundamental genetic or cancer medicine concepts so that the pearls could be used in multiple applications and would not need as frequent updating as the consumer-translated text. The development of the knowledge pearls was informed by focus group studies, which included cancer patients and caregivers18,23. The materials reflect the diverse health literacy24 and content knowledge expertise of librarians, information scientists, oncologists, and members of the My Cancer Genome team.
Sample Size Determination
The primary objective of the study was to evaluate the educational effectiveness of consumer information about precision medicine therapies in cancer, which was assessed by comparing pre-, post-and follow-up knowledge test scores among the three intervention groups. With a two-sided significance level of 5% and 80% power, the study required a sample size of 27 individuals per study arm. To adjust for a 30% drop-out rate, the planned recruitment goal was 117 participants. The sample size calculation provided sufficient power to detect a 0.91x standard deviation (SD) difference between groups and was based on the assumption that the effect size is equal to the mean difference between groups divided by the standard deviation.
Statistical Analysis
All missing values were imputed using the multiple imputation approach with all relevant study variables: baseline score, post score, follow up score, group, cancer type, months since diagnosis, gender, education, age, and health literacy score. Multivariable linear regression was used to estimate the intervention effect on (1) post-knowledge test score and (2) follow-up knowledge test score, adjusted for pre-knowledge test score (baseline assessment), as well as other covariates (i.e. age, education and health literacy). Residual analysis was used to check the linear regression assumptions of homogeneity for variance, normality and linearity. The final model was decided based on likelihood ratio tests for comparing three models (with and without education or health literacy) as well as adjusted R2. All tests were significant at the two-sided 5% level. Analyses were performed in R 3.1.0, and the study statisticians were blinded to the group assignment.
Results
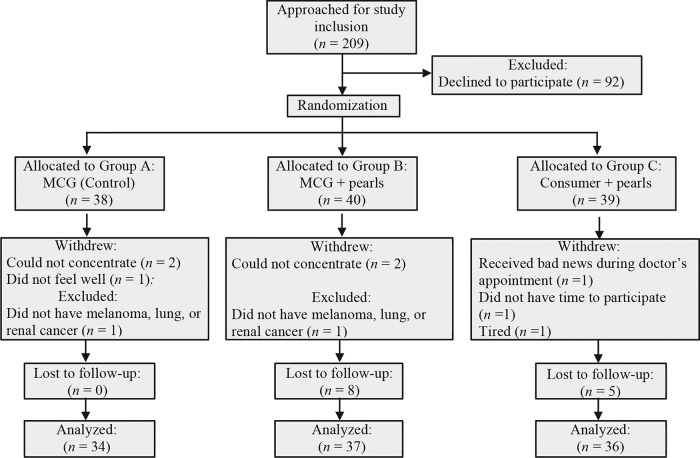
One-hundred and seventeen participants were randomized in a 1:1:1 ratio to one of the three groups (Figure 2). Eight participants withdrew during the clinic visit, and data for two participants were excluded from analysis as they did not meet eligibility criteria. Pre-and post-knowledge questionnaire data were analyzed for the remaining 107 participants (n = 34, 37, and 36 for Group A, B, and C, respectively). Thirteen participants were lost to follow-up.
Figure 2.
Participant flow diagram
Most of the participants were white and had at least a high school education (Table 1). A higher percentage of participants were cancer patients in Group A (65%) than in Groups B and C, (59% and 58%, respectively). A higher percentage of participants in Group B (52%) reported a household income greater than $75,000 than in Group A (23%) or Group C (35%). The percentage of participants with adequate health literacy in the three groups was 82% in Group A, 89% in Group B, and 83% in Group C (Table 2). Nearly half the participants in each group indicated preferences for learning via multiple modalities (Table 2).
Table 1.
Participant characteristics
| Characteristic | N | Group A (n = 34) |
Group B (n = 37) |
Group C (n = 36) |
|---|---|---|---|---|
| Participant type, n (%) | 107 | |||
| Patient | 22 (65) | 22 (59) | 21 (58) | |
| Caregiver | 12 (35) | 15 (41) | 15 (42) | |
| Cancer type, n (%) | 107 | |||
| Lung | 14 (41) | 11 (30) | 15 (42) | |
| Melanoma | 16 (47) | 16 (43) | 16 (44) | |
| Renal | 4 (12) | 10 (27) | 5 (14) | |
| Diagnosis range, n (%) | 107 | |||
| Within 12 months | 11 (32) | 10 (27) | 11 (31) | |
| 13-24 months | 3 (8.8) | 5 (14) | 5 (14) | |
| Over 24 months | 20 (59) | 22 (59) | 20 (56) | |
| Cancer stage, n (%) | ||||
| Stage I | 107 | 1 (2.9) | 0 (0) | 0 (0) |
| Stage II | 0 (0) | 3 (8.1) | 2 (5.6) | |
| Stage III | 4 (12) | 5 (14) | 5 (14) | |
| Stage IV | 17 (50) | 24 (65) | 19 (53) | |
| Not available | 7 (21) | 4 (11) | 8 (22) | |
| Other | 5 (15) | 1 (2.7) | 2 (5.6) | |
| Tumor sequencing conducted, n (%) | 107 | |||
| Yes | 21 (62) | 17 (46) | 17 (47) | |
| No/data was not available | 13 (38) | 20 (54) | 19 (53) | |
| Received precision medicine therapy, n (%) | 107 | |||
| Yes | 16 (47) | 14 (38) | 17 (47) | |
| No/data was not available | 18 (53) | 23 (62) | 19 (53) | |
| Days since first seen at Vanderbilt, median (Q1, Q3) | 106 | 714 (255, 1662) | 1288 (337, 3322) | 1339 (237, 2823) |
| Age in years, mean (SD) | 105 | 57 (15) | 55 (15) | 58 (9.7) |
| Gender, n (%) | 106 | |||
| Male | 15 (44) | 17 (47) | 14 (39) | |
| Female | 19 (56) | 19 (53) | 22 (61) | |
| Race, n (%) | 104 | |||
| White | 33 (97) | 35 (100) | 33 (94) | |
| Black or African American | 1 (2.9) | 0 (0) | 0 (0) | |
| American Indian or Alaska Native | 0 (0) | 0 (0) | 2 (5.7) | |
| Hispanic, Latino, or Spanish origin, n (%) | 104 | |||
| Yes | 0 (0) | 1 (2.9) | 1 (2.8) | |
| No | 33 (100) | 34 (97) | 35 (97) | |
| Education, n (%) | 107 | |||
| Between 9th and 12th grade | 1 (2.9) | 1 (2.7) | 3 (8.3) | |
| High school graduate, GED or equivalent | 4 (12) | 6 (16) | 8 (22) | |
| Some college - no degree | 8 (24) | 4 (11) | 4 (11) | |
| Vocational/technical degree | 6 (18) | 2 (5.4) | 7 (19) | |
| Bachelor’s degree | 10 (29) | 12 (32) | 6 (17) | |
| Master’s degree | 4 (12) | 9 (24) | 7 (19) | |
| Professional school degree | 0 (0) | 2 (5.4) | 1 (2.8) | |
| Doctoral degree | 1 (2.9) | 1 (2.7) | 0 (0) | |
| Household income, n (%) | 89 | |||
| $10,000 or less | 1 (3.3) | 4 (12) | 3 (12) | |
| $10,001 - $20,000 | 4 (13) | 2 (6.1) | 3 (12) | |
| $20,001 - $35,000 | 6 (20) | 2 (6.1) | 4 (15) | |
| $35,001 - $55,000 | 9 (30) | 4 (12) | 3 (12) | |
| $55,001 - $75,000 | 3 (10) | 4 (12) | 4 (15) | |
| more than $75,000 | 7 (23) | 17 (52) | 9 (35) |
Table 2.
Health literacy level and learning style preferences
| Characteristic | N | Group A (n = 34) |
Group B (n = 37) |
Group C (n = 36) |
|---|---|---|---|---|
| Health literacy level, n (%) | 106 | |||
| Adequate | 28 (82) | 33 (89) | 29 (83) | |
| Marginal | 2 (5.9) | 3 (8.1) | 4 (11) | |
| Inadequate | 4 (12) | 1 (2.7) | 2 (5.7) | |
| Learning style, n (%) a | 106 | |||
| Reading | 1 (2.9) | 6 (17) | 1 (2.8) | |
| Listening | 2 (5.9) | 0 (0) | 4 (11) | |
| Watching | 2 (5.9) | 4 (11) | 1 (2.8) | |
| Doing | 13 (38) | 8 (22) | 14 (39) | |
| Multimodal | 16 (47) | 18 (50) | 16 (44) |
Note:
Participants who selected more than one learning style were classified as multimodal learners.
The mean post-and follow-up test scores were higher for all groups compared to the pre-test scores (Table 3). A multivariable linear regression revealed that Group C showed a significantly greater improvement in post-test score (p = 0.0308) compared to Group A (Table 4). There was no significant difference detected between Groups A and B in post-test score (Table 4). Group C showed a greater improvement in three week follow-up test score compared to Group A; however, the multivariable linear regression showed that the group difference was not statistically significant at the two-sided 5% level (Table 5). There was also no significant difference detected between Group B and Group A in follow-up test score (Table 5).
Table 3.
Mean scores on the knowledge assessment questionnaire
| Mean number of correct answers (SD) | N | Group A (n = 34) |
Group B (n = 37) |
Group C (n = 36) |
|---|---|---|---|---|
| Pre-assessment score, mean (SD) | 107 | 4 (2.5) | 5.4 (2.0) | 4.2 (2.3) |
| Post-assessment score, mean (SD) | 107 | 6.2 (1.7) | 6.5 (1.7) | 7.1 (1.8) |
| Follow-up score, mean (SD) | 94 | 5.7 (1.8) | 6.8 (1.6) | 6.7 (1.6) |
| Post-test minus pre-test score, mean (SD) | 107 | 2.2 (1.9) | 1.1 (2.0) | 2.9 (2.3) |
| Follow-up minus post-test score, mean (SD) | 94 | 1.7 (2.0) | 1.2 (2.0) | 2.1 (2.1) |
Abbreviations: SD = standard deviation
Table 4.
Multivariate linear regression of post-test score
| Posttest score (N = 107) |
||||
|---|---|---|---|---|
| Variable | B | (SE) | t | p (two-tailed) |
| Intercept | 4.78 | (0.93) | 5.15 | <0.0001 |
| Pretest score | 0.34 | (0.069) | 4.85 | <0.0001 |
| Group B | −0.29 | (0.38) | −0.75 | 0.453 |
| Group C | 0.83 | (0.38) | 2.19 | 0.0308 |
| Age | −0.0053 | (0.011) | −0.47 | 0.639 |
| College-level education | 0.53 | (0.42) | 1.25 | 0.215 |
| Master or Doctoral degree | 0.82 | (0.50) | 1.66 | 0.0998 |
| Health literacy score | −0.03 | (0.068) | −0.44 | 0.662 |
Abbreviations: SE = standard error
Table 5.
Multivariate linear regression of follow-up test score
| Follow-up test score (N = 107) |
||||
|---|---|---|---|---|
| Variable | B | (SE) | t | p (two-tailed) |
| Intercept | 4.59 | (0.94) | 4.9 | <0.0001 |
| Pretest score | 0.36 | (0.072) | 5.01 | <0.0001 |
| Group B | 0.34 | (0.41) | 0.83 | 0.411 |
| Group C | 0.65 | (0.38) | 1.72 | 0.0881 |
| Age | −0.0074 | (0.011) | −0.66 | 0.512 |
| College-level education | 0.083 | (0.45) | 0.18 | 0.856 |
| Master or Doctoral degree | 0.48 | (0.53) | 0.9 | 0.372 |
| Health literacy score | 0.001 | (0.080) | 0.01 | 0.99 |
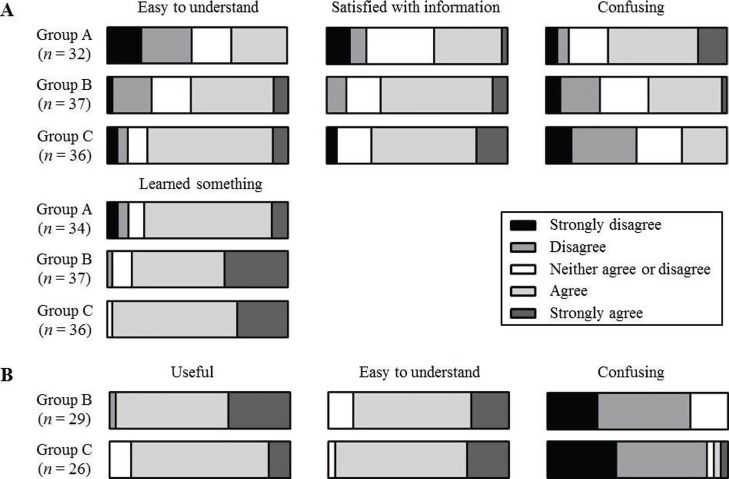
There were significant group differences (Figure 3), as assessed by Fisher’s exact tests, in whether the participants thought the information was easy to understand (p = 0.01), was confusing (p = 0.014), and if they were satisfied with the information (p = 0.03). The percentage of participants who either agreed or strongly agreed that the information was easy to understand was highest in Group C (77.3%) compared to Group B (54.1%) and Group A (31%). The percentage of participants who agreed or strongly agreed that they were satisfied with the information was also highest in Group C (75%) compared to Group B (70.1%) and Group A (41%). There were no statistically significant group differences in participant responses regarding whether they thought that they learned something from the information (p = 0.063). There were also no statistically significant differences between Groups B and C regarding responses to whether the videos were useful (p = 0.052), easy to understand (p = 0.44), or confusing (p = 0.215). The percentage of participants in Group B who agreed or strongly agreed that the videos were useful, easy to understand, and confusing were 96%, 87%, and 0%, respectively. For Group C, the percentage of participants who agreed or strongly agreed that the videos were useful, easy to understand, and confusing were 89%, 96%, and 7.8%, respectively.
Figure 3.
Graphical representation of the percentage of participants who strongly disagreed, disagreed, neither agreed or disagreed, agreed, or strongly agreed to statements about whether the information was easy to understand, if they were satisfied with the information, if some of the information was confusing, and if they learned something (A) and whether the knowledge pearl videos helped them understand the information they received (labeled “useful” in the figure), were easy to understand, or were confusing (B). Note that the legend in A also applies to B.
Web analytics data revealed that 78% of participants in Group B and 86% of participants in Group C viewed at least one of the knowledge pearl videos. The knowledge pearls viewed by at least half of participants were antibody, protein, and targeted therapy for Group B and genetic testing and targeted therapy for Group C (Table 6). The mean duration participants spent viewing the intervention materials was 12.1 (SD = 7.03 minutes; n = 30), 21.6 (SD = 17.6 minutes; n = 34), and 17.3 (SD = 35.3 minutes; n = 36) minutes, for Groups A, B, and C, respectively.
Table 6.
Knowledge pearl views
| Group B (n = 36) |
Group C (n = 36) |
|
|---|---|---|
| Pearl, n (%) | ||
| Antibody | 22 (61) | 6 (17) |
| Chromosome | 2 (5.6) | N/A |
| Expression | 10 (28) | N/A |
| Fusion | 4 (11) | N/A |
| Genetic testing | N/A | 23 (64) |
| Immune system | 12 (33) | 11 (31) |
| Exon | 4 (11) | N/A |
| Kinase inhibitor | 12 (33) | N/A |
| Mutation | 4 (11) | N/A |
| Protein | 19 (53) | 5 (14) |
| Receptor | 16 (44) | N/A |
| Targeted therapy | 24 (67) | 23 (64) |
| Wildtype | 2 (5.6) | N/A |
The median follow-up phone call interval was 22 days for all three groups (Table 7). At follow-up, 32 participants (94%) in Group A, 25 participants (86%) in Group B, and 28 participants (90%) in Group C reported that they kept the educational information handout they were given during their clinic visit. Fifteen participants (44%) in Group A, 7 participants (24%) in Group B, and 12 participants (39%) in Group C indicated that they read the handout since leaving the clinic. Only one participant reported viewing the website version of the material after leaving the clinic.
Table 7.
Follow-up interview
| Characteristic | N | Group A (n = 34) |
Group B (n = 29) |
Group C (n = 31) |
|---|---|---|---|---|
| Follow-up interval in days, median (Q1, Q3) | 94 | 22 (21, 24) | 22 (21, 23.5) | 22 (21, 24) |
| Kept handout, n (%) | 94 | |||
| Yes | 32 (94) | 25 (86) | 28 (90) | |
| No | 2 (5.9) | 3 (10) | 3 (9.7) | |
| Don’t know | 0 (0) | 1 (3.5) | 0 (0) | |
| Read handout, n (%) | 94 | |||
| Yes | 15 (44) | 7 (24) | 12 (39) | |
| No | 19 (56) | 22 (76) | 18 (58) | |
| Don’t know | 0 (0) | 0 (0) | 1 (3.2) | |
| Viewed website, n (%) | 94 | |||
| Yes | 0 (0) | 1 (3.5) | 0 (0) | |
| No | 34 (100) | 28 (97) | 31 (100) |
Discussion
In this study, we found that participants who viewed the consumer version of the information about precision medicine with the knowledge pearls embedded (Group C) showed significantly greater knowledge gains immediately after viewing the information than the control group (Group A). Participants who viewed knowledge pearls (Groups B and C) showed a high level of satisfaction with the videos. These findings were consistent with our previous study18 in which we evaluated understanding of information about a specific tumor mutation in melanoma. Taken together, these studies suggest that adherence to health literacy and learning style principles when designing consumer educational information can facilitate comprehension of complex information regarding genetics and cancer medicine.
While Group C showed greater gains in knowledge immediately after viewing the information relative to Group A, these differences were no longer apparent at the three week follow-up. The majority of the participants in the study indicated that they had not read the information given to them or visited the website version of the information since their clinic visit. These findings suggest that patients may need reminders to re-examine the information periodically and that patients would benefit from ongoing review of the information.
One limitation of the study is the lack of racial diversity among the study population. Most the participants were white. It will be important in future studies to determine whether the findings from this study are still applicable in non-white populations. Another limitation is that a majority of the participants had adequate health literacy. Given that the consumer information was written at the sixth grade level and developed by adhering to health literacy and suitability guidelines, we would predict that our findings would still be applicable in more diverse populations, particularly those with lower health literacy.
Research has shown that cancer patients want to participate in decisions about their care25. Although healthcare providers are often cancer patients’ main source of information, patients increasingly seek information from other sources, especially the Internet26. Patients looking for genetic information may be more likely to turn to the Internet instead of a healthcare provider6. However, evaluations of the state of online consumer health information indicate that attempts to keep it current are often a losing battle. To help meet the need for reliable, patient-friendly cancer information, the consumer content that we have developed will be made freely available online.
Several studies of popular online resources for various cancers have found that much of the content available has not been recently updated or does not indicate the last date of update27 –32. Failure to revise online materials to reflect new developments can lead to significant inaccuracies in the information patients access. For instance, one study29 found that 12 of 38 websites (32%) with bladder cancer information included inaccuracies, largely due to outdated information. It has been suggested that one way to circumvent this problem is to redirect patients to clinicaltrials.gov and similar resources so they can stay abreast of emerging therapies28. However, many patients who discover a new precision medicine therapy in this manner may still have difficulty fully understanding its implications for their care. The MCG website was created using a template structure to facilitate updating. By adhering to a similar template design, the consumer versions may more easily be revised concurrently with the professional-level text.
Conclusion and Future Directions
As precision medicine moves to the forefront of patient care, it is becoming increasingly important to ensure that patients are readily able to understand their genetic results and communicate with their care team members. The knowledge pearls created through this project may be reused by oncologists and others to help patients understand complex precision medicine concepts and facilitate patient engagement in the healthcare process. Future opportunities for broader scalability could easily include the integration of the knowledge pearls into a variety of information systems, such as online patient portals designed to communicate to patients their health information. Informed by awareness of the difficulties and limitations of translating constantly evolving information to the consumer level, our approach of providing freely available consumer-friendly explanations of fundamental concepts offers a reusable and scalable alternative to traditional patient education efforts that can be applied to expand consumer knowledge in a variety of medical fields.
Acknowledgements
This research was funded in part by an IMLS grant (IMLS LG-06-13-0180-13). The targeted therapies and immunotherapies pages on My Cancer Genome were supported by the Joyce Family Foundation, the Robert J. Kleberg, Jr., and Helen C. Kleberg Foundation, the T. J. Martell Foundation, an anonymous foundation, and a corporate gift from Bristol-Myers Squibb. Support for REDCap was through National Center for Advancing Translational Sciences/National Institutes of Health UL1 TR000445. The authors wish to acknowledge Mallory Blasingame, Marcia Epelbaum, Patricia Lee, and Dan McCollum for their assistance in recruiting and interviewing participants for the study and aiding with content development. We additionally would like to acknowledge Mallory Blasingame for her assistance with the manuscript. Finally, we would like to acknowledge the patients, their caregivers, and their health care providers for supporting this study.
References
- 1.Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015 Feb 26;372(9):793–5. doi: 10.1056/NEJMp1500523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaufman HL. Melanoma as a model for precision medicine in oncology. Lancet Oncol. 2014 Mar;15(3):251–3. doi: 10.1016/S1470-2045(14)70059-2. [DOI] [PubMed] [Google Scholar]
- 3.Politi K, Herbst RS. Lung cancer in the era of precision medicine. Clin Cancer Res Off J Am Assoc Cancer Res. 2015 May 15;21(10):2213–20. doi: 10.1158/1078-0432.CCR-14-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sonpavde G, Choueiri TK. Precision medicine for metastatic renal cell carcinoma. Urol Oncol. 2014 Jan;32(1):5–15. doi: 10.1016/j.urolonc.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Christensen KD, Jayaratne TE, Roberts JS, Kardia SLR, Petty EM. Understandings of basic genetics in the United States: results from a national survey of black and white men and women. Public Health Genomics. 2010;13(7-8):467–76. doi: 10.1159/000293287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dougherty MJ, Lontok KS, Donigan K, McInerney JD. The critical challenge of educating the public about genetics. Curr Genet Med Rep. 2014 Apr 5;2(2):48–55. [Google Scholar]
- 7.Haga SB, Barry WT, Mills R, et al. Public knowledge of and attitudes toward genetics and genetic testing. Genet Test Mol Biomark. 2013 Apr 1;17(4):327–35. doi: 10.1089/gtmb.2012.0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lontok KS, Zhang H, Dougherty MJ. Assessing the genetics content in the Next Generation Science Standards. PLoS ONE. 2015 Jul 29;10(7):e0132742. doi: 10.1371/journal.pone.0132742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Condit CM. Public understandings of genetics and health. Clin Genet. 2010 Jan;77(1):1–9. doi: 10.1111/j.1399-0004.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- 10.Cuffe S, Hon H, Qiu X, et al. Cancer patients’ acceptance, understanding, and willingness-to-pay for pharmacogenomic testing. Pharmacogenet Genomics. 2014 Jul;24(7):348–55. doi: 10.1097/FPC.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 11.Tomlinson AN, Skinner D, Perry DL, Scollon SR, Roche MI, Bernhardt BA. “Not tied up neatly with a bow”: professionals’ challenging cases in informed consent for genomic sequencing. J Genet Couns. 2015 Apr 26 doi: 10.1007/s10897-015-9842-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swanton C. My Cancer Genome: a unified genomics and clinical trial portal. Lancet Oncol. 2012 Jul;13(7):668–9. [Google Scholar]
- 13.Spatz MA. Genetics Home Reference. J Med Libr Assoc. 2004 Apr;92(2):282–3. [Google Scholar]
- 14.Massachusetts General Cancer Center. Targeted cancer care: about [Internet]. [cited 2016 Jan 5] Available from: https://targetedcancercare.massgeneral.org/About.aspx.
- 15.23andMe. Genetics 101 - Learn about DNA [Internet]. 23andMe. [cited 2016 Jan 6] Available from: https://www.23andme.com/gen101/
- 16.National Center for Education Statistics. The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy [Internet]. 2006 [cited 2016 Jan 5] Available from: http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483.
- 17.Crumb SI. An evaluation framework to assess educational genetic websites: Are they meeting public needs? [Internet] [Thesis]. 2014 [cited 2016 Jan 5] Available from: https://digital.lib.washington.edu/researchworks/handle/1773/25159.
- 18.Giuse NB, Kusnoor SV, Koonce TY, et al. Guiding oncology patients through the maze of precision medicine. J Health Commun. doi: 10.1080/10810730.2015.1131772. Forthcoming 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanderbilt-Ingram Cancer Center. Fast facts [Internet]. About us. [cited 2016 Jan 5] Available from: http://www.vicc.org/about/facts.php.
- 20.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-- a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004 Sep;36(8):588–94. [PubMed] [Google Scholar]
- 22.Giuse DA. Supporting communication in an integrated patient record system; AMIA Annu Symp Proc AMIA Symp AMIA Symp.; 2003. p. 1065. [PMC free article] [PubMed] [Google Scholar]
- 23.Kusnoor SV, Justiss K, Stamm MD, et al. Using health literacy and learning styles to improve patient understanding of genetics and personalized medicine; Medical Library Association Annual Meeting; Austin, TX. 2015 May 19. [Google Scholar]
- 24.Giuse NB, Kusnoor SV, Koonce TY, Ryland CR, Walden RR, Naylor HM, Williams AM, Jerome RN. Strategically aligning a mandala of competencies to advance a transformative vision. J Med Libr Assoc. 2013 Oct;101(4):261–7. doi: 10.3163/1536-5050.101.4.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient Educ Couns. 2012 Jan;86(1):9–18. doi: 10.1016/j.pec.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finney Rutten LJ, Agunwamba AA, Wilson P, et al. Cancer-related information seeking among cancer survivors: trends over a decade (2003-2013) J Cancer Educ Off J Am Assoc Cancer Educ. 2015 Feb 26 doi: 10.1007/s13187-015-0802-7. [DOI] [PubMed] [Google Scholar]
- 27.Black PC, Penson DF. Prostate cancer on the Internet—information or misinformation? J Urol. 2006 May;175(5):1836–42. doi: 10.1016/S0022-5347(05)00996-1. discussion 1842. [DOI] [PubMed] [Google Scholar]
- 28.Ogah I, Wassersug RJ. How reliable are “reputable sources” for medical information on the Internet? The case of hormonal therapy to treat prostate cancer. Urol Oncol. 2013 Nov;31(8):1546–52. doi: 10.1016/j.urolonc.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Yeo H, Roman S, Air M, et al. Filling a void: thyroid cancer surgery information on the internet. World J Surg. 2007 Jun;31(6):1185–91. doi: 10.1007/s00268-007-9010-x. discussion 1192-3. [DOI] [PubMed] [Google Scholar]
- 30.Lee CT, Smith CA, Hall JM, Waters WB, Biermann JS. Bladder cancer facts: accuracy of information on the Internet. J Urol. 2003 Nov;170(5):1756–60. doi: 10.1097/01.ju.0000092696.20128.9b. [DOI] [PubMed] [Google Scholar]
- 31.King SJ, Livingston PM, Turner L, et al. Mapping the information resources available to patients with colorectal cancer. Eur J Cancer Care (Engl). 2010 Jul;19(4):492–500. doi: 10.1111/j.1365-2354.2009.01080.x. [DOI] [PubMed] [Google Scholar]
- 32.Air M, Roman SA, Yeo H, et al. Outdated and incomplete: a review of thyroid cancer on the World Wide Web. Thyroid Off J Am Thyroid Assoc. 2007 Mar;17(3):259–65. doi: 10.1089/thy.2006.0300. [DOI] [PubMed] [Google Scholar]