Abstract
Purpose
To examine how age of onset of sexual intercourse is associated with past-year and lifetime sexually transmitted infections (STIs) and depression in young adulthood.
Methods
We examined how occurrence of a lifetime and past-year STI, lifetime diagnosis of depression, and past-week depressive symptoms differed as a function of age of onset of sexual intercourse using data from the National Longitudinal Study of Adolescent to Adult Health (Add Health; N = 8,938 individuals). Time-varying effect models (TVEMs) were used to examine how age of onset, measured as continuous age, was associated with these outcomes in young adulthood, with all analyses stratified to examine gender differences.
Results
Individuals who engaged in first intercourse prior to age 16 reported higher than average rates of all outcomes studied; for example, an estimated 35% of women and 12% of men who initiated at age 14 reported a lifetime STI, compared to about 5% of those who initiated at age 24. Timing of first intercourse past the mid-twenties was associated with lower than average rates of STIs and lifetime depression diagnoses, but was associated with a somewhat higher level of past-year depressive symptoms. Patterns were similar by gender, although there was little difference in men's depression diagnoses by age of onset.
Discussion
Results suggest that sexual intercourse prior to age 16 may be associated with higher rates of STIs and depression. Findings provide support for comprehensive programs that both promote delay of first intercourse and provide safe-sex and psychological support for those who initiate early.
Keywords: first sexual intercourse, sexually transmitted infections, depressive symptoms, young adulthood, time-varying effect models
Early sexual intercourse is associated with negative physical and mental health outcomes, such as sexually transmitted infections (STIs) and depressive symptoms. Studies have found higher rates of STIs in individuals who engage in early (definitions ranging from ages 13-16) sexual intercourse [1-4]. Possible explanations include biological factors, more years of sexual activity to accumulate a greater number of partners, and riskier young adult sexual behavior (e.g., condom nonuse, higher-risk partners) among early initiators [2; 5-6]. Similarly, associations between early sexual intercourse and increased depressive symptoms have been documented, particularly among adolescent girls [7-8]. One explanation, according to life course theory [9] is that experiencing life transitions during periods that are “off-time” relative to peers may lead to distress. The stronger associations for adolescent girls compared to boys may be influenced by internalized norms about the inappropriateness of sexual behavior for women, women's greater tendency to engage in sex to please a partner, or by conflict or breakups with sexual and romantic partners [7; 10-12]. Less is known about how later timing may be associated with health outcomes. Because late onset of sex is also “off-time”, individuals who initiate sex at later ages may feel more distressed about their lack of sexual experience. This may be especially true for men, as research has suggested that sexual prowess is a critical component of masculinity that is tied to well-being [13]. One study found that late initiation of intercourse is associated with poorer sexual functioning for men, suggesting the possibility that both early and late sexual initiation may be problematic for adult health [4]. Prevention efforts to delay sexual intercourse do not generally address potential negative outcomes of late initiation, and thus more information about how specific timing of sexual initiation may be associated with different outcomes is necessary.
Most studies of this topic have grouped individuals into early, normative or late timing by either choosing cutoff ages based on unspecified criteria or assessing timing relative to peers in the sample (e.g., upper or lower age of onset quartiles, z-score cutoffs). Although intuitive, this leads to different definitions across studies, which makes it difficult to interpret the body of evidence as a whole; for example, definitions of “early” sexual behavior range from prior to age 13 [1] to prior to age 16 [7-8]. However, because age of onset has typically been studied with age groups, the “lumping” of ages into categories may obscure or attenuate associations that may be better represented as a function of continuous time. Consistent with prior research, one study that assessed age of onset as a continuous variable documented greater prevalence of STI in young adulthood for individuals who initiated early compared to later; for example, those who initiated at age 10 had an estimated 10% probability of a past-year STI, compared to 7% of those who initiated at 16 and 4% of those who initiated at age 20 [2]. However, this study did not examine the effect of initiation after age 20 or examine associations with mental health, making it unknown whether later initiation may be associated with poorer psychological functioning. In addition, this study examined the linear effect of time, which may obscure more nuanced changes.
A new analytic approaches, the time-varying effect model (TVEM; [13-14]) has been used to examine outcomes as functions of continuous age of onset of a behavior, enabling researchers to empirically determine during which ages initiation of a behavior is a particular risk. For example, one study found that initiating smoking before age 20 was associated with increased odds of dependence in young adulthood, and that the risk of later dependence was highest for individuals who began smoking at age 10 [16]. However, no study has applied this sort of flexible approach to examine outcomes of age of initiation of sexual behavior. In this study, we apply TVEM to data from a large, nationally representative study to empirically determine which ages of onset of sexual intercourse are associated with higher risk of STIs and depression in young adulthood (defined here as ages 24-34), and how these trends may differ by gender.
Method
Participants and Procedures
Data are from the contractual sample of the National Longitudinal Study of Adolescent to Adult Health (Add Health), a longitudinal study of individuals recruited from schools when they were in 7-12th grade in 1994-1995 (Wave I) [17]. Follow-up in-home interviews occurred during 1995-1996 (Wave II), 2001-2002 (Wave III), and 2007-2008 (Wave IV). Data collection was approved by the Public Institutional Review Board at the University of North Carolina, and we received approval from the Penn State Institutional Review Board for secondary analysis. Because our focus is the effect of timing of first intercourse, we included individuals who had first engaged in sexual intercourse by Wave IV (94% of participants) and had data about timing of first intercourse and the Wave IV outcomes. In addition, we included only individuals from the core sample, which was designed to be a representative sample of the school-age population at that time and is essentially self-weighting [17]. Our resulting sample contained 8,938 individuals (55% female, 45% male; 65% white, 8% Black, 11% Latino, 3% Asian, 3% other race, M age at Wave IV = 28.9 years, SD = 1.8).
Measures
Timing of first intercourse was assessed using items from Waves I-IV. We included participants’ report of first intercourse from the earliest wave sex was reported, as the recall of events, including first intercourse, has been found to be more accurate when less time has passed between the event and the assessment [18]. At Waves I and II, participants reported if they had ever engaged in sexual intercourse, followed by questions about the month and year it occurred; age at first sex in was calculated from this information and interview date. At Waves III and IV, participants were asked if they ever engaged in vaginal intercourse, followed by a question about the age (in years) when it occurred. To be consistent across waves, we used age in years as the time metric. At all waves, intercourse was defined as when “a man inserts his penis into a woman's vagina.” The mean age of first intercourse was 16.51 (SD = 2.9); 23% of individual had sex prior to age 15, 66% between 15 and 20, and 10% after age 20.
We examined lifetime and past-year STI infection at Wave IV, when individuals were 24-34 years of age). Participants reported whether they had been diagnosed with six different STIs (chlamydia, gonorrhea, trichomoniasis, syphilis, genital herpes, and genital warts), in their lifetime, and whether this diagnosis occurred in the past year. Composite variables indicating diagnosis with any of these STIs were created (0=not diagnosed, 1=diagnosed). Similarly, we examined lifetime and past-week indicators of depression from Wave IV. For the lifetime measure, participants reported whether they had ever received a diagnosis of depression (0=no diagnosis, 1=received diagnosis). For the past-week measure, participants completed an 8-items scale of past-week depressive symptoms drawn from the Center for Epidemiological Studies Depression Scale [19]. Items were rated on a scale from 0-3 (“never or rarely” to “most or all of the time,” during the past seven days.
We controlled for age at Wave IV, race/ethnicity measured with 4 dichotomous indicators (Black, Latino, Asian, and other; White as reference group) and whether or not an individual had been sexually abused prior to first intercourse (since prior literature suggests this predicts early initiation [20]). The sexual abuse variable was calculated from 3 Wave IV items about whether an individual had been touched in a sexual way or forced to have sex by a parent or caregiver, or forced into any type of sexual activity by anyone other than a parent, followed by questions about the age at which this occurred. Individuals were coded 1 if they reported any of these types of sexual abuse prior to or at the same age as the age they initiated sex, and 0 if they report none of these or if it occurred after first intercourse.
Statistical Analyses
TVEM is a flexible, semi-parametric model that examines how an outcome variable and its associations with different predictors vary as a function of continuous time or age [13-14]. This enables examination of how rates/levels of STIs and depressive symptoms differ over time, with the curve allowed to vary in a non-parametric way that allows for identification of more precise periods of change or risk [15, 21]. Thus this analysis is not examining the effect of age of first intercourse as a linear or other parametric function, but flexibly estimating rates by age. Using the TVEM SAS macro [22], we ran a series of intercept-only models separated by gender, in which the proportion of (or for depressive symptoms, the level of) each health outcome was estimated as a function of age of first sexual behavior. Our control variables were entered as time-invariant effects, in which the effect was fixed to be a constant effect regardless of age of onset. Because coefficients are estimated in continuous time, our primary results are presented as figures. Results are plotted with the mean level of the outcome variable for individuals in the reference group to better compare how individuals with initiation at different ages differed from the average adult.
Results
Table 1 shows the effects of control variables on each outcome. Lifetime STI was higher for Black, Latino, or other race compared to White participants, and was higher for women who had been sexually abused prior to first intercourse compared to those who had not. Past-year STI was higher for individuals who were black compared to white or had been sexually abused as well as women who were other race compared to white. Lifetime diagnosis of depression was lower for black and Latino participants compared to white participants, as well as lower for Asian compared to white women and higher for participants who had been sexually abused. Finally, levels of depressive symptoms were higher for male and female participants who were black and who had been sexually abused, as well as for Latino compared to white women and other race compared to white men.
Table 1.
Time-invariant effects of control variables of adult health outcomes, by gender
| Lifetime STI (OR) | Past Year STI (OR) | Lifetime Depression Diagnosis (OR) | Past-Week Depressive Symptoms (β) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M/% Male | M/% Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| Age | 28.98 | 28.76 | 1.06 | 0.99 | 0.96 | 0.97 | 0.95 | 1.01 | −0.00 | 0.00 |
| Black | 15.89% | 19.05% | 3.96*** | 3.50*** | 2.94*** | 3.82*** | 0.51*** | 0.44*** | 0.12*** | 0.10*** |
| Latino | 11.40% | 10.57% | 1.80*** | 1.45** | 1.37 | 1.23 | 0.58** | 0.64*** | 0.01 | 0.08** |
| Asian | 2.87% | 2.99% | 0.61 | 1.16 | 0.30 | 1.05 | 0.65 | 0.28*** | 0.08 | 0.03 |
| Other Race | 2.37% | 2.53% | 1.99* | 1.62* | 2.31* | 1.21 | 0.73 | 1.26 | 0.10* | 0.04 |
| Sexual Abuse | 3.97% | 16.50% | 1.28 | 1.37*** | 1.90* | 1.48*** | 2.77** | 2.31*** | 0.27*** | 0.15*** |
Note. STI = sexually transmitted infection. OR = Odds Ratio. Estimates represent the time-invariant effect of predictors from intercept only TVEM models. Age was centered at sample mean. Sexual abuse refers to any reported sexual abuse prior to age of first intercourse. Reference group for this analysis is white participants of average age who were not sexually abused.
p < .05
p < .01
p < .001
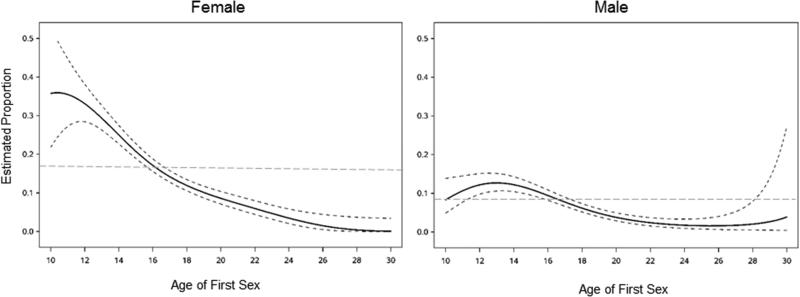
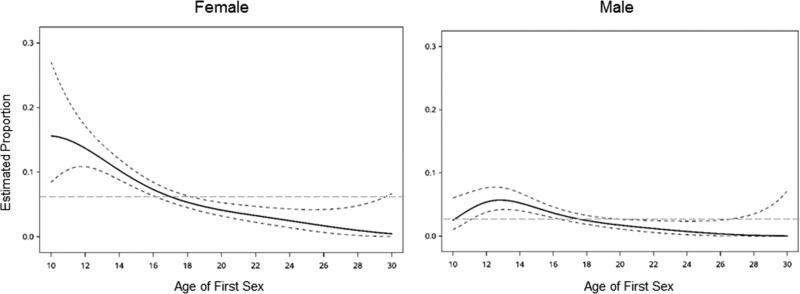
Our primary results showing health outcomes by timing of first sexual intercourse, controlling for age, race/ethnicity and sexual abuse prior to first intercourse, are presented in Figures 1-4. For lifetime STI (Figure 1), the earliest age of onset assessed (age 10) was associated with the highest estimated proportion of STI. Nearly 40% of women who initiated at age 10 had contracted an STI by young adulthood, compared to a sample average of 17%. About 10% of women who initiated at age 20 and close to 0% of women who initiated at age 30 were estimated to have an STI. For men, the highest risk for STI in adulthood was among individuals who initiated first intercourse at age 13, 13% of whom contracted an STI by adulthood, compared to an 8% average. Lifetime STI risk decreased from onset at age 13 and plateaued at about age 22, with almost no men who initiated after that age estimated to have contracted an STI. For both men and women, initiation before age 16 was associated with greater than average prevalence of a lifetime STI, whereas initiation after age 18 was associated with less than average prevalence. Figure 2 shows estimated proportion with an STI diagnosed in the past year by age of onset and shows relatively similar patterns, although rates are lower than for lifetime STI.
Figure 1.
Estimated proportion of lifetime STI infection by age of onset of first sexual intercourse for male and female young adults. Solid black lines = estimated proportion, dashed black lines = 95% Confidence Interval, grey dashed line = whole sample STI prevalence. Models were estimated as intercept-only TVEM models adjusted for age, race/ethnicity and sexual abuse prior to first intercourse as time-invariant effects.
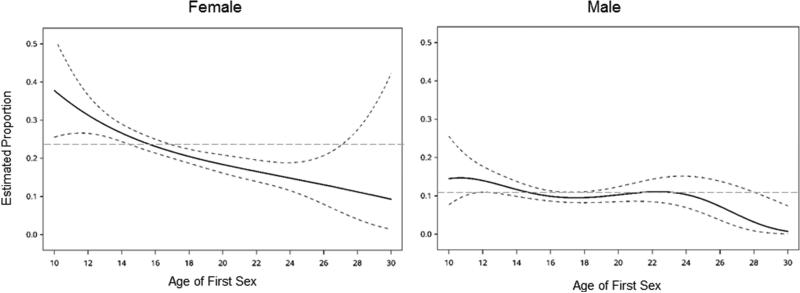
Figure 4.
Estimated level of depressive symptoms by age of onset of first sexual intercourse for male and female young adults. Solid black lines = estimated proportion, dashed black lines = 95% Confidence Interval, grey dashed line = whole sample STI prevalence. Models were estimated as intercept-only TVEM models adjusted for age, race/ethnicity and sexual abuse prior to first intercourse as time-invariant effects.
Figure 2.
Estimated proportion of past-year STI infection by age of onset of first sexual intercourse for male and female young adults. Solid black lines = estimated proportion, dashed black lines = 95% Confidence Interval, grey dashed line = whole sample STI prevalence. Models were estimated as intercept-only TVEM models adjusted for age, race/ethnicity and sexual abuse prior to first intercourse as time-invariant effects.
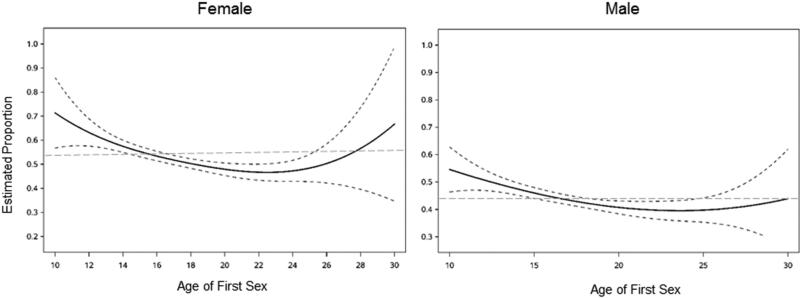
Figure 3 shows estimated proportion with a lifetime depression diagnosis by age of onset of sexual intercourse. Women who initiated before age 16 had greater than average prevalence of a lifetime diagnosis of depression by young adulthood. The estimated proportion of women with a depression diagnosis was highest at an age of onset around age 10 (38%) and decreased relatively steadily, with about 10% of those initiating at age 30 reporting lifetime depression. For men, there was relatively little difference in depression diagnoses by age of onset.
Figure 3.
Estimated proportion of lifetime diagnosis of depression by age of onset of first sexual intercourse for male and female young adults. Solid black lines = estimated proportion, dashed black lines = 95% Confidence Interval, grey dashed line = whole sample STI prevalence. Models were estimated as intercept-only TVEM models adjusted for age, race/ethnicity and sexual abuse prior to first intercourse as time-invariant effects.
Finally, figure 4 shows level of past-week depressive symptoms in adulthood by age of onset of sexual intercourse. Initiation before age 16 was associated with a higher than average level of depressive symptoms. For both men and women, the level of symptoms decreased with later age of onset until about age 24, after which the level of depressive symptoms started to rise with later age of onset.
Discussion
This study examined how rates of STIs and depression in adulthood varied as a function of age of onset of sexual intercourse. Consistent with prior research, women were more likely to report STIs and had higher depressive symptoms compared to men [23-24]. STI findings may be driven by physiological factors [25], whereas differences in depression may reflect differences in experiencing and reacting to stress [24], as well as men's lower usage of health care [26]. However, rates of these outcomes differ based upon age of first sexual intercourse. Findings support prior research suggesting that early initiation of sexual intercourse is associated with STIs and depression [1, 3, 4, 7], and that higher than average rates of negative outcomes are present in those initiating prior to age 16. This result was consistent for both lifetime and past-year STIs, suggesting that the increased risk was not solely a result of additional time to engage in sexual behavior with a greater number of partners, but may also reflect different patterns of adult sexual behaviors that result in STI acquisition. For example, individuals who engaged in early sexual behavior may be less likely to use condoms or have more partners during young adulthood. Similar findings for early timing of first intercourse were observed for both lifetime depressive diagnoses and past-year depressive symptoms. There was less variation by age of onset for men's lifetime depression diagnoses, which may be due to greater cultural acceptability of sexual behavior at younger ages for men compared to women, as well as women's greater tendency to engage in sex to please a partner [10, 12]. Overall, findings suggest sexual intercourse prior to age 16 may be associated with both depression and STIs into adulthood.
Results showed a relatively steady pattern of decreased risk with later age of onset of sex, with one notable exception: past-year depressive symptoms. For both men and women, the lowest levels of past-year depressive symptoms were observed for individuals who initiated sex around age 24, with past-year depressive symptoms starting to increase with later age of onset after that age. Because the individuals who initiated sex in adulthood engaged in sex for the first time more recently than someone who initiated at earlier ages, they may still be adjusting to their relatively new status of being sexually active, which may lead to more negative affect and slightly elevated levels of depressive symptoms. This differs from the results for lifetime depression diagnosis, for which odds continued to decrease after onset at age 24. Individuals who are abstinent into adulthood differ from those who initiated sex earlier in a number of ways, including being more religious [27], which may help to buffer them from more serious mental health issues such as a diagnosis of major depression or other disorders [28].
There are several implications of this study for future research and sexuality education programs. First, this study suggests that higher than average risk of STIs and depression are present for individuals who initiate before age 16. This provides some evidence for using age 16 as a cutoff for studying early sexual behavior, as, on average, individuals who engage in intercourse before, but not after, this age are at greater than average risk of negative outcomes. Second, findings provide some evidence for the benefits of delaying first intercourse, at least into the late teens and possibly into early adulthood. This is consistent with the emphasis on delaying sexual intercourse that researchers have found to be present in many sexuality education programs [29]. However, although individuals’ health outcomes may, on average, be improved by delay of first intercourse, it is important to note that abstinence-focused programs are largely ineffective in reducing STI risk behaviors [30], and that delay of intercourse into the twenties for all individuals is likely unrealistic. Thus, the high rates of STIs found for individual who engage in first intercourse at an early age demonstrate the necessity of comprehensive sexuality education programs that encourage protective measures for those who are sexually active.
It is important to note that these associations are correlational, and do not necessarily reflect causality; there may be confounding variables that predict both adolescent risk behavior and health outcomes, or may reflect mediating factors like dissolution of relationships with sexual partners. For example, early substance use is associated with early onset of sexual activity [31] and with future depression [32]. Research that has used stronger causal inference approaches found a causal effect of sexual behavior before age 14 on depressive symptoms in the next year and on STIs in young adulthood for girls, but found no effect on young adult depression [3, 7]. Future research could use causal inference approaches to better understand the effects of timing of sex at a wider variety of ages, though causal inference approaches in TVEM are an open area of inquiry and require more intensive data [21]. Regardless of causality, results show that timing of sexual behavior is a marker for later health outcomes, and suggests individuals who could benefit from targeted interventions
Although results do suggest potential benefits of delaying sexual intercourse, it is important to note that such associations may not be universal, but may result from cultural messages related to sexual behavior. One study of the United States and 4 European countries found that sex prior to age 15 was associated with girls’ depressive symptoms in the U.S. and Poland, but not Finland, France or Scotland [33]. In addition, rates of STIs among adolescents are much higher among adolescents in the United States compared to those in Australia, France, and the Netherlands [34]. Explanations for these differences include more negative cultural messages about sexual behavior and less comprehensive sexuality education programs in the U.S. compared to other Western nations [33-34]. Rather than being seen as evidence for continuing abstinence-focused sexuality education programs, our results may be documenting some of the negative outcomes of these programs. Future research should examine outcomes of timing of sexual initiation in different countries in order to better identify factors that are associated with more positive or negative health outcomes.
There are a number of limitations. First, as discussed above, we cannot definitely prove directionality or causality of associations with the current data and approach. Because we did not have pre-intercourse values on depressive symptoms for individuals who initiated sex prior to Wave I, we were not able to examine changes in depressive symptoms or directionality of associations. Second, relatively few people in the study initiated sex after age 25 or before age 12, meaning our estimates of health outcomes for these group are less precise, and should be interpreted with caution. We did not have information about the relationship context of first sexual intercourse, which may be an important moderator in associations between sexual behavior and depressive symptoms [7, 35-36]. All of our measures were self-report and could be biased by retrospective reporting. In addition, individuals may have undiagnosed STIs or depression. Prior research has suggested that associations between early age at first intercourse and STIs are stronger at earlier ages and dissipate with time [2], and future research should further investigate at what ages it continues to exert an effect. In addition, research should examine potential mediators of these associations, such as differences in condom use or number of partners for individuals with different ages of first intercourse. We only examined initiation of one sexual behavior, and future research could look at effects of timing of oral or anal sexual behavior, and include sexual initiation with same-sex partners. Although we controlled for sexual abuse, the extent to which intercourse was coerced or wanted likely has a considerable impact on outcomes of first intercourse at early ages, and future research with more information about the contexts of both first intercourse and abuse could better understand these associations. Finally, future research with a larger sample of ethnic minority participants could examine racial/ethnic differences in outcomes of first sexual intercourse, as different average ages of initiation by race ethnicity have been documented [37] and could point to differing norms about sexual behavior [38], which could in turn be associated with different mental health outcomes.
Despite these limitations, this paper contributes to our understanding of the effects of timing of sexual intercourse initiation in several ways. It uses a large, nationally representative longitudinal sample and a new method that allows us to estimate outcomes of sexual initiation at different ages as a function of continuous time. In short, results suggest that initiation before age 16 is associated with greater than average risks of both depression and STIs in young adulthood, whereas the impact of sexual initiation at later ages is more nuanced.
Acknowledgments
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. This research and the authors were supported by grant P50- DA039838 from the National Institute on Drug Abuse (NIDA). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA, NICHD, or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Implications and Contribution
Early sexual behavior is associated with negative health outcomes, but it is less clear what ages of initiation are problematic. Results suggest intercourse before age 16 is associated with STIs and depression, with mixed findings for later ages. Programmatic efforts to delay first intercourse and promote safe-sex are warranted.
References
- 1.Coker AL, Richter DL, Valois RF, McKeown RE, Garrison CZ, Vincent ML. Correlates and consequences of early initiation of sexual intercourse. J School Health. 1994;64:372–377. doi: 10.1111/j.1746-1561.1994.tb06208.x. [DOI] [PubMed] [Google Scholar]
- 2.Kaestle CE, Halpern CT, Miller WC, Ford CA. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. Am J Epidemiol. 2005;161(8):774–780. doi: 10.1093/aje/kwi095. doi:10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- 3.Kugler KC, Vasilenko SA, Butera N, Coffman D. Long-term consequences of early sexual initiation on young adult health: A causal inference approach. J of Early Adolescence. doi: 10.1177/0272431615620666. Manuscript Accepted for Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandfort TGM, Orr M, Hirsch JS, Santelli JS. Long-term health correlates of timing of sexual debut: results from a national US study. Am J Public Health. 2008;98(1):155–161. doi: 10.2105/AJPH.2006.097444. doi:10.2105/AJPH.2006.097444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kahn JA, Rosenthal SL, Succop PA, Ho GYF, Burk RD. Mediators of the Association Between Age of First Sexual Intercourse and Subsequent Human Papillomavirus Infection. Pediatrics. 2002;109(1):e5–e5. doi: 10.1542/peds.109.1.e5. doi:10.1542/peds.109.1.e5. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg J, Magder L, Aral S. Age at first coitus: A marker for risky sexual behavior in women. Sex Transm Dis. 1992;19:331–334. [PubMed] [Google Scholar]
- 7.Meier AM. Adolescent first sex and subsequent mental health. Am J Sociol. 2007;112(6):1811–1847. doi:10.1086/512708. [Google Scholar]
- 8.Spriggs AL, Halpern CT. Sexual Debut Timing and Depressive Symptoms in Emerging Adulthood. J Youth Adolesc. 2008;37(9):1085–1096. doi: 10.1007/s10964-008-9303-x. doi:10.1007/s10964-008-9303-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elder GH. The life course as developmental theory. Child Dev. 1998;69(1):1–12. doi:10.1111/j.1467-8624.1998.tb06128.x. [PubMed] [Google Scholar]
- 10.Crawford M, Popp D. Sexual double standards : A review and methodological critique of two decades of research. J Sex Res. 2003;40(1):13–26. doi: 10.1080/00224490309552163. doi:10.1080/00224490309552163. [DOI] [PubMed] [Google Scholar]
- 11.Impett EA, Peplau LA. Compliance: Gender, motivational and relationship perspectives. J Sex Res. 2012;40(1):87–100. doi: 10.1080/00224490309552169. doi:10.1080/00224490309552169. [DOI] [PubMed] [Google Scholar]
- 12.Joyner K, Udry JR. You don't bring me anything but down: adolescent romance and depression. J Health Soc Behav. 2000;41(4):369–391. [PubMed] [Google Scholar]
- 13.Marsiglio W. Adolescent male sexuality and heterosexual masculinity: a conceptual model and review. Journal of Adolescent Research. 1998;3:285–303. doi: 10.1177/074355488833005. [DOI] [PubMed] [Google Scholar]
- 14.Tan X, Shiyko MP, Li R, Li Y, Dierker LC. A time-varying effect model for intensive longitudinal data. Psychol Methods. 2012;17(1):61–77. doi: 10.1037/a0025814. doi:10.1037/a0025814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanza ST, Vasilenko S a, Liu X, Li R, Piper ME. Advancing the Understanding of Craving During Smoking Cessation Attempts: A Demonstration of the Time-Varying Effect Model. Nicotine Tob Res. 2013 Aug;:1–8. doi: 10.1093/ntr/ntt128. doi:10.1093/ntr/ntt128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lanza ST, Vasilenko SA. New methods shed light on age of onset as a risk factor for nicotine dependence. Addict Behav. 2015;50:161–164. doi: 10.1016/j.addbeh.2015.06.024. doi:10.1016/j.addbeh.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris KM. Design features of Add Health. University of North Carolina at Chapel Hill; Chapel Hill, NC: 2011. [Google Scholar]
- 18.Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: Methodological challenges in survey research. Sex Transm Infections. 2001;77:84–92. doi: 10.1136/sti.77.2.84. doi:10.1136/sti.77.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radloff LS. The use of the Center for Epidemiological Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20:149e66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 20.Senn TE, Carey MP, Vanable PA. Childhood and adolescent sexual abuse and subsequent sexual risk behavior: Evidence from controlled studies, methodological critique, and suggestions for research. Clin Psych Rev. 2008;28(5):711–35. doi: 10.1016/j.cpr.2007.10.002. 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vasilenko SA, Lanza ST. Predictors of Multiple Sexual Partners From Adolescence Through Young Adulthood. J Adolesc Heal. 2014 Feb;:1–7. doi: 10.1016/j.jadohealth.2013.12.025. doi:10.1016/j.jadohealth.2013.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li R, Dziak JD, Tan X, Huang L, Wagner AT, Yang J. TVEM (time-varying effect modeling) SAS macro users’ guide (Version 3.1.0) University Park: The Methodology Center; Penn State: 2015. 2015. Retrieved from http://methodology.psu.edu. [Google Scholar]
- 23.Coombs RW, Reichelderfer PS, Landay AL. Recent observations on HIV type-1 infection in the genital tract of men and women. AIDS. 2003;17(4):455–80. doi: 10.1097/00002030-200303070-00001. 7. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) Sexually Transmitted Disease Surveillance 2014. U.S. Department of Health and Human Services; Atlanta: 2015. [Google Scholar]
- 25.Nolen-Hoeksema S. Gender differences in depression. Cur Dir in Psych Sci. 2001;10(5):173–6. 1. [Google Scholar]
- 26.Mustard CA, Kaufert P, Kozyrsky A, Mayer T. Sex differences in the use of health care services. N Engl J Med. 1998;338:1678–83. doi: 10.1056/NEJM199806043382307. [DOI] [PubMed] [Google Scholar]
- 27.Eisenberg ML, Shindel AW, Smith JF, Lue TF, Walsh TJ. Who is the 40-year-old virgin and where did he/she come from? Data from the National Survey of Family Growth. J Sex Med. 2009;6(8):2154–2161. doi: 10.1111/j.1743-6109.2009.01327.x. doi:10.1111/j.1743-6109.2009.01327.x. [DOI] [PubMed] [Google Scholar]
- 28.Smith TB, McCullough ME, Poll J. Religiousness and depression: Evidence for a main effect and the moderating influence of stressful life events. Psychol Bull. 2003;129(4):614–636. doi: 10.1037/0033-2909.129.4.614. doi:10.1037/0033-2909.129.4.614. [DOI] [PubMed] [Google Scholar]
- 29.Kirby DB. Emerging Answers 2007: Research Findings on Programs to Reduce Teen Pregnancy and Sexually Transmitted Diseases. Washington D.C.: 2007. [Google Scholar]
- 30.Ott MA, Santelli JS. Abstinence and abstinence-only education. Curr Op Obst Gyn. Oct 1. 2007;19(5):446–52. doi: 10.1097/GCO.0b013e3282efdc0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tubman JG, Windle M, Windle RC. Cumulative sexual intercourse patterns among middle adolescents: Problem behavior precursors and concurrent health risk behaviors. J Adolesc Heal. 1996;18:182–191. doi: 10.1016/1054-139X(95)00128-F. doi:10.1016/1054-139X(95)00128-F. [DOI] [PubMed] [Google Scholar]
- 32.McGue M, Iacono WG. The association of early adolescent problem behavior and adult psychopathology. Am J Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. doi:10.1007/s10519-006-9061-z. [DOI] [PubMed] [Google Scholar]
- 33.Madkour AS, Farhat T, Halpern CT, Godeau E, Nic Gabhainn S. Early adolescent sexual initiation and physical/psychological symptoms: a comparative analysis of five nations. J Youth Adolesc. 2010;39(10):1211–1225. doi: 10.1007/s10964-010-9521-x. doi:10.1007/s10964-010-9521-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weaver H, Smith G, Kippax S. School-based sex education policies and indicators of sexual health among young people : A comparison of the Netherlands, France, Australia and the United States. 2005;5(2):171–188. doi:10.1080/14681810500038889. [Google Scholar]
- 35.Grello CM, Welsh DP, Harper MS, Dickson JW. Dating and relationship trajectories and adolescent functioning. Adolesc Fam Heal. 2003;3:103–112. [Google Scholar]
- 36.Mendle J, Ferrero J, Moore SR, Harden KP. Depression and Adolescent Sexual Activity in Romantic and Nonromantic Relational Contexts: A Genetically-Informative Sibling Comparison. J Abnorm Psychol. 2012;122(1):51–63. doi: 10.1037/a0029816. doi:10.1037/a0029816. [DOI] [PubMed] [Google Scholar]
- 37.Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, et al. Age of sexual debut among US adolescents. Contraception. 2009;80(2):158–162. doi: 10.1016/j.contraception.2009.02.014. doi:10.1016/j.contraception.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feldman SS, Turner RA, Araujo K. Interpersonal context as an influence on sexual timetables of youths: Gender and ethnic effects. J Res Adolesc. 1999;9:25–52. doi:10.1207/s15327795jra0901_2. [Google Scholar]