Abstract
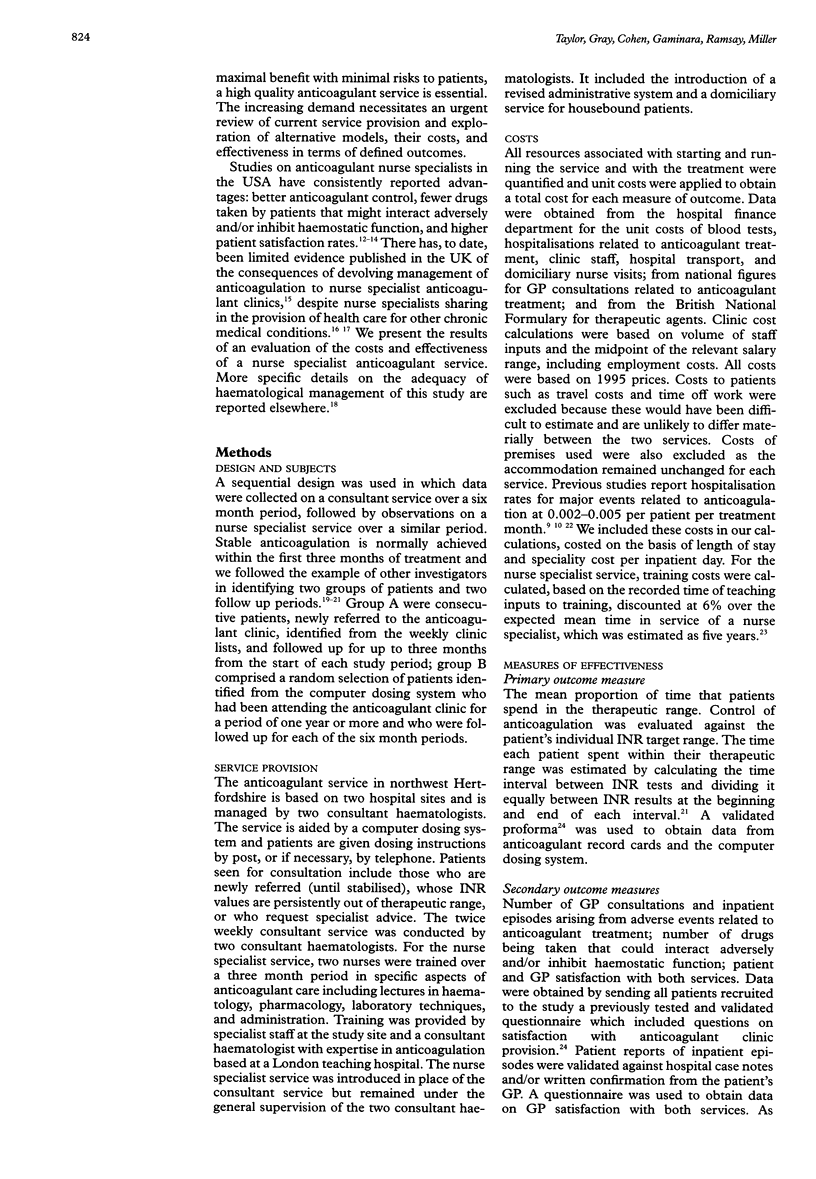
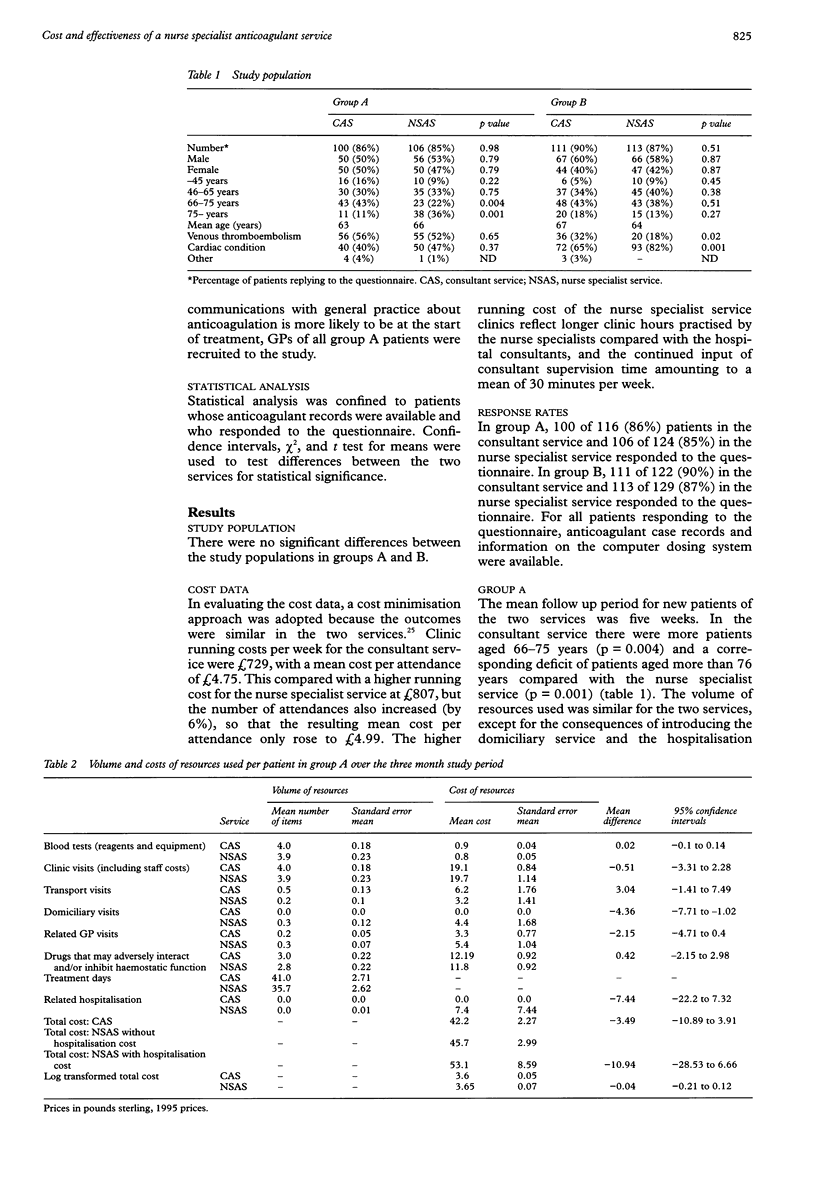
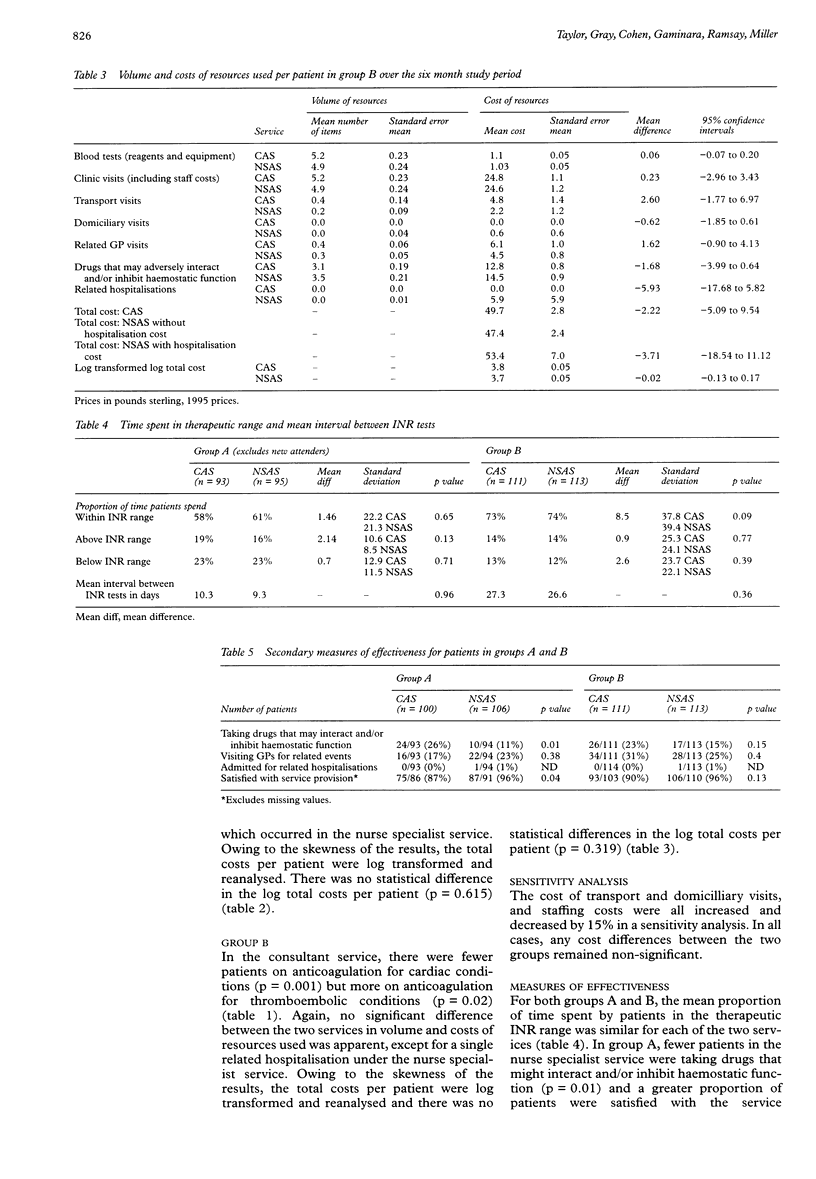
AIMS: To determine the costs and effectiveness of an anticoagulant nurse specialist service compared with a conventional consultant service based on two hospital sites in northwest Hertfordshire. METHODS: Sequential design comparing retrospectively the conduct and outcomes of a consultant service with a nurse specialist service over two six month periods. In each of the six month study periods, all new patients consecutively referred for anticoagulation over a three month period (group A) at the start of each study period and a random selection of patients who had already been attending the anticoagulant service for one year or more (group B) were included in the study. Group A patients wre followed for up to three months and group B patients for six months. The main outcome measures were costs of service provision and effectiveness. Costs included those for the use of the anticoagulant service, those related to general practitioner (GP) visits and hospitalisations, and running costs (staff time, laboratory tests, patient transport). Measures of effectiveness were the mean proportion of time patients spend in the therapeutic range, the number of drugs being taken that could interact adversely and/or inhibit haemostatic function, and patient and GP satisfaction with service provision. RESULTS: In the consultant service, for group A there were more patients aged 66-75 years (p = 0.004) and fewer patients aged more than 76 years (p = 0.001); and for group B, there were fewer patients on anticoagulation for cardiac conditions (p = 0.001), but more on anticoagulation for thromboembolic conditions (p = 0.02) than in the nurse specialist service. The clinic running costs of the nurse specialist service were 4.99 Pounds per attendance, compared with 4.75 Pounds in the consultant service. Including all other costs related to treatment, there was no statistically significant difference in cost per patient. There was no significant difference in the proportion of time patients spent in the therapeutic range between the consultant service and the nurse specialist service. In the nurse specialist service, fewer patients in group A were taking drugs that could interact adversely and/or inhibit haemostatic function (p = 0.01) and more patients were satisfied with service provision (p = 0.04) compared with the consultant service. There was no significant variation in GP satisfaction between the two services. CONCLUSION: In the provision of outpatient anticoagulation, the nurse specialist service was no more expensive than the consultant service and, using our primary outcome, at least as effective. The nurse specialist service has some clear advantages compared to the consultant service: provision of domicilliary care for housebound patients, fewer new patients taking drugs that could interact adversely and/or inhibit haemostatic function patients, it is preferred by newly referred patients to the consultant service, and it is as acceptable to their GPs.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ansell J. E. Oral anticoagulant therapy--50 years later. Arch Intern Med. 1993 Mar 8;153(5):586–596. [PubMed] [Google Scholar]
- Baradell J. G. Cost-effectiveness and quality of care provided by clinical nurse specialists. J Psychosoc Nurs Ment Health Serv. 1994 Mar;32(3):21–24. doi: 10.3928/0279-3695-19940301-07. [DOI] [PubMed] [Google Scholar]
- Duxbury B. M. Therapeutic control of anticoagulant treatment. Br Med J (Clin Res Ed) 1982 Mar 6;284(6317):702–704. doi: 10.1136/bmj.284.6317.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fihn S. D., McDonell M., Martin D., Henikoff J., Vermes D., Kent D., White R. H. Risk factors for complications of chronic anticoagulation. A multicenter study. Warfarin Optimized Outpatient Follow-up Study Group. Ann Intern Med. 1993 Apr 1;118(7):511–520. doi: 10.7326/0003-4819-118-7-199304010-00005. [DOI] [PubMed] [Google Scholar]
- Gray A. M., Phillips V. L. Turnover, age and length of service: a comparison of nurses and other staff in the National Health Service. J Adv Nurs. 1994 Apr;19(4):819–827. doi: 10.1111/j.1365-2648.1994.tb01155.x. [DOI] [PubMed] [Google Scholar]
- Gustafsson C., Asplund K., Britton M., Norrving B., Olsson B., Marké L. A. Cost effectiveness of primary stroke prevention in atrial fibrillation: Swedish national perspective. BMJ. 1992 Dec 12;305(6867):1457–1460. doi: 10.1136/bmj.305.6867.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornblit P., Senderoff J., Davis-Ericksen M., Zenk J. Anticoagulation therapy: patient management and evaluation of an outpatient clinic. Nurse Pract. 1990 Aug;15(8):21-6, 29, 32. [PubMed] [Google Scholar]
- Loken S., Shioshita G. Factors that influence therapeutic anticoagulation control. Nurse Pract Forum. 1992 Jun;3(2):95–104. [PubMed] [Google Scholar]
- Pamir G., Cağlar N., Oral D., Akyol T., Kaymakçalan S. Evaluation of coronary arterial disease by oral dipyridamole stress testing using 12-lead electrocardiography. Int J Cardiol. 1990 Dec;29(3):311–316. doi: 10.1016/0167-5273(90)90119-p. [DOI] [PubMed] [Google Scholar]
- Pell J. P., McIver B., Stuart P., Malone D. N., Alcock J. Comparison of anticoagulant control among patients attending general practice and a hospital anticoagulant clinic. Br J Gen Pract. 1993 Apr;43(369):152–154. [PMC free article] [PubMed] [Google Scholar]
- Poller L., Wright D., Rowlands M. Prospective comparative study of computer programs used for management of warfarin. J Clin Pathol. 1993 Apr;46(4):299–303. doi: 10.1136/jcp.46.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seabrook G. R., Karp D., Schmitt D. D., Bandyk D. F., Towne J. B. An outpatient anticoagulation protocol managed by a vascular nurse-clinician. Am J Surg. 1990 Nov;160(5):501–505. doi: 10.1016/s0002-9610(05)81015-3. [DOI] [PubMed] [Google Scholar]
- Shafi M., Mayberry J., Calcraft B. An audit of a medical anticoagulant clinic in a District General Hospital. Postgrad Med J. 1983 Aug;59(694):492–494. doi: 10.1136/pgmj.59.694.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor F. C., Ramsay M. E., Renton A., Cohen H. Methods for managing the increased workload in anticoagulant clinics. BMJ. 1996 Feb 3;312(7026):286–286. doi: 10.1136/bmj.312.7026.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vadher B., Patterson D. L., Leaning M. Evaluation of a decision support system for initiation and control of oral anticoagulation in a randomised trial. BMJ. 1997 Apr 26;314(7089):1252–1256. doi: 10.1136/bmj.314.7089.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Pette J., Mackie C. Managing the increased workload in anticoagulant clinics. Clinics led by nurse practitioners can work well. BMJ. 1996 May 11;312(7040):1226–1227. doi: 10.1136/bmj.312.7040.1226b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyness M. A. Evaluation of an educational programme for patients taking warfarin. J Adv Nurs. 1990 Sep;15(9):1052–1063. doi: 10.1111/j.1365-2648.1990.tb01986.x. [DOI] [PubMed] [Google Scholar]
- van den Besselaar A. M. Recommended method for reporting therapeutic control of oral anticoagulant therapy. Control of Anticoagulation Subcommittee of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Thromb Haemost. 1990 Apr 12;63(2):316–317. [PubMed] [Google Scholar]
- van den Besselaar A. M., van der Meer F. J., Gerrits-Drabbe C. W. Therapeutic control of oral anticoagulant treatment in The Netherlands. Am J Clin Pathol. 1988 Dec;90(6):685–690. doi: 10.1093/ajcp/90.6.685. [DOI] [PubMed] [Google Scholar]


