Abstract
Problem
The departure of physician-scientists from education and research into clinical practice is a growing challenge for the future of academic medicine. Junior faculty face competing demands for clinical productivity, teaching, research and work-life integration which can undermine confidence in the value of an academic career. Mentorship is important to foster career development and satisfaction in junior faculty.
Intervention
The goals of this academic pediatrics department were to develop, implement, and evaluate a multi-faceted pediatric mentoring program to promote retention and satisfaction of junior faculty. Program elements included one-on-one mentor-mentee meetings, didactic workshops, grant review assistance, and facilitated peer-group mentoring. Program effectiveness was assessed using annual surveys of mentees, structured mentee exit interviews as well as retention data for assistant professors.
Context
The mentees were Instructors and Assistant Professors in the department of pediatrics
Outcome
Seventy-nine mentees participated in the program from 2007 through 2014. The response rate from seven annual surveys was 84%. Sixty-nine percent of mentees felt more prepared to advance their careers, 81% had a better understanding of the criteria for advancement, 84% were satisfied with the program, and 95% found mentors accessible. Mentees who exited the program reported they most valued the one-on-one mentoring and viewed the experience positively regardless of promotion. Retention of Assistant Professors improved after initiation of the program; 4 of 13 hired from 2002–2006 left the institution whereas 18 of 18 hired from 2007–2014 were retained.
Lessons Learned
This multi-faceted mentoring program appeared to bolster satisfaction and enhance retention of junior pediatric faculty. Mentees reported increased understanding of the criteria for promotion and viewed the program as a positive experience regardless of career path. Individual mentor-mentee meetings were needed at least twice yearly to establish the mentoring relationship. Identifying “next steps” at the end of individual meetings was helpful to hold both parties accountable for progress. Mentees most valued workshops fostering development of tangible skills (such as scientific writing) and those clarifying the criteria for promotion more transparent. Facilitated peer-group mentoring for mentees at the Instructor rank provided valuable peer support.
Keywords: FACULTY DEVELOPMENT, MENTEE, MENTOR, MENTORING PROGRAM, RETENTION, SATISFACTION
Problem
The departure of physician-scientists from education and research into clinical practice or industry is a growing challenge for the future of academic medicine. Early in their career, these physicians face competing demands for clinical productivity, teaching, research, and work-life integration. The situation is exacerbated by dwindling private and government funding for research while lucrative and flexible opportunities exist in clinical practice.1 These factors can undermine confidence in the value of an academic career and increase the risk of professional burnout.2 Mentoring is often cited as an important component of career development of medical professionals and a way to foster satisfaction and retention.3 One study found that 98% of junior faculty identified lack of mentoring as the first or second most important factor hindering career advancement.4
Despite the belief that career guidance is key, there is little consensus around the definition of mentorship or the metrics for evaluating its success.5–7 A systematic review of 18 mentoring programs for physicians in academic medicine from 2000 to 2011 found they employed 7 different models for mentorship; the dyad model was most common.5 The published metrics used to assess the success of mentoring programs have varied as well. Several mentoring programs cite only participant-reported subjective outcomes such as satisfaction with the program, psycho-social benefits, and sense of development of professional skills. Mentees in one pilot program “felt better,” reported an increased sense of camaraderie, and improved work-life balance.7 Participants in another program reported greater confidence in their abilities and their productivity with individual projects.8 Completion of a specific project was the metric of success in a different program.9 Although lack of mentoring is cited as an obstacle to retention, there remains a paucity of data demonstrating an improvement in retention in response to mentoring in academic medicine.10,11
The Pediatric Mentoring Program (PMP) was developed in response to an identified need to enhance mentorship. This stemmed in part from a 2006 survey sent to 25 junior faculty members. The 16 who responded identified a need for more support with external networking, advice on role and time balance, and formal critiquing of their scientific, clinical, and teaching performance. They rated their primary mentors as only partially successful in advising them about promotion, leaving them partially or totally unclear about the criteria for career advancement. Junior investigators overwhelmingly favored a standardized, formal annual review. The need for greater mentorship was also underscored in interviews with three junior faculty members who served on a planning committee. Additionally, senior faculty members were cognizant of the loss of several Assistant Professors prior to institution of the PMP. The other impetus for the PMP was the arrival of the new Chief of Pediatrics who had experience with a formal mentoring program at his prior institution that he found to be effective.
Intervention and Context
Development and Participation
In 2007, the Chief of Pediatrics formed a planning committee including three junior and one senior faculty member in pediatrics, the Senior Associate Dean for Diversity and Leadership for the School of Medicine, the director of faculty affairs of pediatrics, and an administrative leader. The committee designed the program and selected the eight faculty members from a pool of 30 nominees to serve as the initial mentors. Once the PMP began, the senior faculty member (who was one of the 30 nominees) remained as a mentor and the planning committee was dissolved. Thereafter, the PMP steering committee consisted of all eight PMP mentors, the administrative leader and the director of faculty affairs. One mentor was chosen by the group to serve as lead mentor.
The eight mentors were chosen by the members of the planning committee based upon their perceived ability to model and counsel mentees in clinical care, teaching, research, and work-life integration. The criteria used to select mentors included seniority at the Associate or full Professor level, a track record of successful mentoring of junior faculty and trainees, and possession of supportive coaching and communication skills. The committee also sought to create a balanced group of PMP mentors with varied foci on clinical or bench research; five were women, one was at the Associate Professor rank and seven were Professors. All mentors were compensated for their role through a small salary offset. In addition, the program was supported by part-time effort from a program coordinator and an administrative director. During the initial two years of the program, PMP engaged a consultant with a doctorate degree in organizational development who was paid for her services from departmental funds. Her research foci included mentoring and gender and generational differences in the workforce. She had developed and led workshops on these topics for corporate, healthcare, and academic institutions.
The goals of the PMP program were to increase satisfaction and retention of faculty interested in a career as a physician scientist or clinician investigator. The activities of the PMP were intended to complement guidance provided by division chiefs and primary research mentors who are assigned to junior faculty as required by university policy. The PMP mentor was to serve as a “life coach” providing broad career support and direction rather than project-specific functional mentoring. Didactic workshops, grant-writing assistance and networking opportunities were offered as additional support. These activities were led by individuals from within the institution with the exception of workshops on gender and generational differences that were conducted by the outside consultant hired to help launch the mentoring program.
Participation in the PMP was required for all pediatric Instructors and for all Assistant Professors on the University (tenure track, UTL) or Medical Center (MCL) lines until they were promoted to the rank of Associate Professor. The Instructor position is offered to candidates showing promise for careers in academic medicine. The appointment is viewed as a transition period between completion of fellowship and Assistant Professor. Instructors can retain this rank for only three years in most cases and there is no guarantee that an Assistant Professor position will be available or offered at the end of their term as Instructors. Assistant Professors on the UTL or MCL are recruited only when there is an institutional need, a billet is open and candidates have the appropriate track record of clinical and/or basic science research productivity.
Design
The PMP adopted the dyad (mentor-mentee) structure as its mainstay. The program included additional activities that encompassed instrumental, knowledge-based, and psycho-social dimensions. Elements included:
Individualized mentee meetings with an assigned PMP mentor outside of their academic division. Participation in these sessions was the only mandatory aspect of the program which all mentees have fulfilled
Quarterly didactic workshops on interpersonal competencies, career development, and domain-specific knowledge
Facilitated peer-mentoring group meetings for Instructors
Individualized assistance with grant writing and review
The consultant with organizational expertise provided the initial training for PMP mentors and division chiefs. Subsequently, mentors have met every other month as the PMP steering committee where they discuss issues that arise with their mentees. Such meetings have provided confidential peer support and an opportunity to further develop mentoring skills.
Mentee-Mentor Dyads
Matching
Two principles guided the process of matching participants with PMP mentors. First, mentors were selected from outside each mentee’s division in order to reduce potential conflicts of interest and support the need for confidentiality. Second, dyads were matched by research interests (clinical versus basic science) and by academic faculty line. During the first seven years of the PMP, the proportion of male mentees ranged from 30% to 55% and females ranged from 45% to 70%; five of eight mentors were female. We did not match mentors and mentees by gender but assessed the importance of gender in the mentoring relationship. In a survey prior to the initiation of the PMP, 100% of males and 87% of females either disagreed or were neutral with the statement that same-sex mentor/mentee dyads were easier. Responses from mentees surveyed in the first few years of the PMP were similar; mentees consistently responded that gender had “no influence” on interactions in the dyads. Mentees have had the option to change their PMP mentor at any time if the relationship was suboptimal. Only one mentee has done so, a female mentee choosing a new female mentor over her assigned female mentor.
Individual mentoring meetings
Meetings between mentee and mentor were mandatory. The PMP initially required only one individual mentee-mentor meeting per year. After year one of the program, a minimum of two meetings annually was mandated because both mentors and mentees valued these counseling sessions and requested the greater frequency. Mentees received letters outlining these expectations at entry into the PMP and were reminded via email from mentors and administrators when to meet. We reviewed the data at each bimonthly PMP mentor meeting to ensure that requisite meetings and documentation had been completed.
The first mentoring session was scheduled in the fall of the academic year to help mentees prepare the departmentally required “Goals and Achievements Form”. This document was used by division chiefs and the Chief of Pediatrics to summarize clinical, research, educational, and administrative progress for the previous year. At the time of the annual meetings, mentors reminded mentees that they were welcome to schedule additional meetings with their mentor if they had interval questions or concerns. An estimated 20% of mentees initiated these additional meetings but exact data are lacking since documentation was required only for the two annual meetings. Mentees were free to seek advice from other PMP mentors as well. At times, PMP mentors referred a mentee to another mentor with special expertise, such as knowledge about promotions or university resources.
During each individual meeting, mentors typically reviewed all aspects of the mentee’s profile: clinical responsibilities, teaching, research, promotion, and work-life integration. At the first meeting, the role of the PMP as career or life coach was specified. As such, mentees understood that the mentor would explore these myriad aspects of the mentee’s professional life. Meetings typically lasted for an hour.
The content of individual mentoring meetings was tracked using a “1:1 meeting documentation form” (Figure 1), a structure that prompted mentors to inquire about all areas of professional life and to set specific goals. The form included a final section for “next steps” to hold mentee and mentor accountable. As an example, mentees might commit to have submitted manuscripts or grants; mentors might agree to contact other faculty to provide research advice.
Figure 1.
Mentee-Mentor Meeting Documentation Form (completed by mentor)
The lead mentor for the PMP reviewed all forms yearly to identify common themes and needs. Mentees were not aware that the 1:1 forms would be reviewed in this manner but all data were de-identified to maintain confidentiality and the content was summarized in general terms.
Didactic Workshops
Quarterly PMP workshops covered three main areas: (1) interpersonal competencies (gender and generational issues, negotiation skills, conflict resolution, individual preferences using the Myers-Briggs Type Indicator©, and effective coaching), (2) career development (appointment and promotion criteria), and (3) domain-specific knowledge (grant writing, funding opportunities, interviewing) (See Table 1). In the first two years of the program, the workshops were designed and facilitated by the consultant with expertise in leadership and organizational development. Subsequently, Stanford faculty including deans and others with relevant expertise in the topic facilitated the workshops. Attendance at workshops has averaged 33 attendees from a minimum of 12 (at a writing workshop limited in size) to 90 (for a session addressing strategies for grant funding open to all faculty ranks). Since most workshops were open to all faculty and fellows in the pediatrics department, the percentage of PMP mentees who attended could not be determined.
Table 1.
Pediatric Mentoring Program Workshops, Stanford University School of Medicine, 2007–2014*
| Topic Area | Individual Workshop Topic (times repeated) |
|---|---|
| Appointment and Promotion |
|
| Career Development |
|
| Grant and Manuscript Writing |
|
| Research Related |
|
| Mentor and Mentee Training |
|
Thirty-one workshops were offered from 2007–2014: seven led by an external consultant (+), six annual sessions on promotion criteria led by university deans, and the remaining led by internal university speakers.
Facilitated Peer-Group Mentoring for Instructors
In the fifth year of the program, participants at the Instructor level requested opportunities to discuss distinct challenges they faced related to funding, academic billets, and productivity within the institution. In response to this request, the program began to host quarterly facilitated peer-group mentoring lunches or wine and cheese gatherings for Instructors. We alternated between holding these sessions with or without two or three mentors in attendance at the request of the Instructors. Sessions without mentors were designed to provide a relaxed atmosphere for networking and sharing experiences on a peer-to-peer basis. Attendance at Instructor-only sessions ranged between six and twelve, representing 33 – 86% of PMP mentees at this rank. Themes for the first sessions were “Work life balance: strategies to make it happen” and “Where am I in my career?” In subsequent meetings, mentees who had successfully navigated from Instructor to Assistant Professorships were invited to share their experiences, thus serving as near-peer role models.
Grant Review Assistance
Also in the fifth year of the program, mentees requested individualized assistance with grant writing. Eighteen pediatric faculty members with funding from the National Institutes of Health (NIH) and other sources were recruited to serve as grant readers. Thirteen of these agreed to share their successful NIH grants with PMP participants in a secure PMP resource library. To date, six mentees have had their grants reviewed using this resource.
Outcome
The PMP was evaluated in terms of its goals for mentees: satisfaction with the quality of their experience as clinician-scientists and retention at Stanford and in academic medicine. Both formative and summative approaches were used. From the outset of the PMP, mentees were asked to complete an annual survey of the program which the program coordinator e mailed to each mentee. Responses were recorded using a Qualtrics ™ (on line) system. The same instrument was employed annually to allow for longitudinal analysis over the life of the program. The average response rate was 84%, likely reflecting the use of repeated reminders from the program coordinator and encouragement from mentors.
To perform a formative evaluation of the PMP, in 2011 we also began to conduct structured exit interviews of mentees. All but one of the 30 former PMP mentees agreed to be interviewed. The administrative director invited the mentees and conducted the interviews confidentially to encourage open feedback. A standardized set of questions was employed:
What was your overall experience as a PMP mentee in the Department of Pediatrics?
What impact did the program and the mentors have on your career development?
Do you have any suggestions for improving this program?
What could we do differently to better support our junior faculty?
Are there formal mentoring initiatives in your current institution (if leaving Stanford)?
Satisfaction
The annual questionnaire assessed satisfaction as measured by agreement with statements about quality of life, feelings about the program and relationships with colleagues and self-efficacy (Table 2). Mentees were asked about accessibility of mentors, the value of the mentoring experience, their sense of belonging to the institution and to the scientific community, feeling respected as a scientist or physician, and feeling comfortable in discussing one’s career with peers and with more senior colleagues. Mentees were most satisfied with their relationship with mentors, with 95% of the respondents ‘agreeing’ or ‘strongly agreeing’ that the PMP mentors were accessible. The PMP was valued as an educational experience and recommended to by 82–85% of survey respondents. In contrast, fewer respondents agreed with statements that reflected collegiality within their units: feeling welcomed as members of a scientific/clinical community (69%), feeling that one’s opinion is respected by the senior faculty in the unit (69%), and comfort speaking about one’s career with senior faculty in the unit (70%).
Table 2.
Mentee Ratings of Statements about the Pediatric Mentoring Program (PMP) 2007–2014*
| % who “agree” or “strongly agree” (no.) | Mean score (median) | |
|---|---|---|
| Statement rated | ||
| The PMP mentors were accessible to me. | 95 (183/193) | 4.41 (5) |
| I would recommend the PMP to my colleagues. | 85 (165/193) | 4.25 (4) |
| Overall, I am satisfied with the PMP. | 84 (163/193) | 4.21 (4) |
| The PMP was a valuable educational experience. | 82 (159/193) | 4.15 (4) |
| My colleagues seek out my opinion as a physician and/or scientist. | 83 (166/199) | 4.04 (4) |
| I feel comfortable speaking with my peers about my career. | 77 (153/199) | 3.90 (4) |
| I am comfortable speaking about my career with senior faculty in my division/dept. | 70 (139/199) | 3.78 (4) |
| I feel like a welcomed member of the scientific/clinical community at Stanford. | 69 (137/199) | 3.81 (4) |
| I feel my opinion is respected by the senior faculty in my division/department. | 69 (137/199) | 3.80 (4) |
| Based on my participation in the PMP (self-efficacy): | ||
| I have a better understanding of the criteria for advancement. | 81 (156/193) | 3.99 (4) |
| I have experienced progress towards my research goals. | 70 (136/193) | 3.78 (4) |
| I am better prepared to advance my career. | 69 (134/193) | 3.82 (4) |
| I have implemented in my job the knowledge and skills I have gained. | 66 (127/193) | 3.79 (4) |
| I feel more comfortable in my clinical/teaching role. | 48 (92/193) | 3.49 (4) |
| My relationship with my primary academic mentor(s) has improved. | 41 (79/193) | 3.34 (3) |
| I have developed collaborative relationships with other PMP participants. | 28 (54/193) | 3.02 (3) |
| My work/life balance has improved. | 22 (43/193) | 2.94 (3) |
Data from seven years of responses combined: n = 32 (2007–08); n = 30 (2008–09); n = 29 (2009–10); n = 40 (2010–11); n = 27 (2011–12); n = 25 (2012–13); n = 28 (2013–14); overall response rate was 84% (211/254). Participants (52% instructor, 48% assistant professor) were asked to rate each statement on the following scale: Strongly Disagree (1), Disagree (2), Neutral (3), Agree (4), Strongly Agree (5); the mean and median scores were calculated from this scale.
The annual questionnaire also explored the mentees’ sense of self-efficacy with their career trajectory and progress towards becoming a physician-scientist. Specific items asked if participation in the PMP helped with preparation for career advancement, implementation of knowledge gained, work-life balance, the relationship with the primary mentor (the individual formally assigned outside of the program), development of peer collaborations, progress towards research goals, and understanding of the criteria for advancement. The number of respondents who “agreed” or “strongly agreed” with self-efficacy statements was significantly less than the number of those expressing satisfaction. Better understanding of the criteria for advancement ranked highest at 81% of respondents, followed by better prepared for advancement (69% of respondents), implementation of knowledge and skills gained and making progress towards research goals (66–70% of respondents). Significantly fewer respondents expressed a feeling of self-efficacy in work/life balance (22%), developed collaborations with peers (28%), or saw improvement in the relationship with the primary (assigned) mentor in their units (41%).
The exit interviews corroborated the findings from the survey analysis. All 30 exiting mentees interviewed described PMP as a valuable experience regardless of promotion or relocation. Individual meetings with PMP mentors were viewed as the most important “reality checks” on progress towards promotion. Mentees appreciated having a mentor outside their division without potential conflicts of interest. In the words of one mentee, “PMP was a carrot to counter balance the hierarchy. The relationship of PMP was more nurturing [than division chief].” Exiting mentees recommended increasing individual meetings to at least twice yearly, concluding meetings with action items for mentors and mentees, providing individualized grant review assistance, and focusing on the Instructor rank. These suggestions were incorporated as described earlier.
Responses in the interviews varied by academic rank. Assistant Professors promoted to the Associate Professor rank were uniformly positive about the program and hoped to continue the formal mentoring relationship even after completing the program. In fact, former PMP mentees have continued to seek out mentors for informal advice. Instructors identified PMP as one of the most valuable offerings to junior faculty and valued their facilitated peer group mentoring meetings. However, not all feedback was positive. Instructors viewed the academic environment as less nurturing for early-career faculty, a sentiment that paralleled the survey results about the sense of collegiality especially regarding senior colleagues. Despite this, Instructors found meetings with PMP mentors and workshops on promotion criteria to be a highly valuable compensation.
Participation and retention
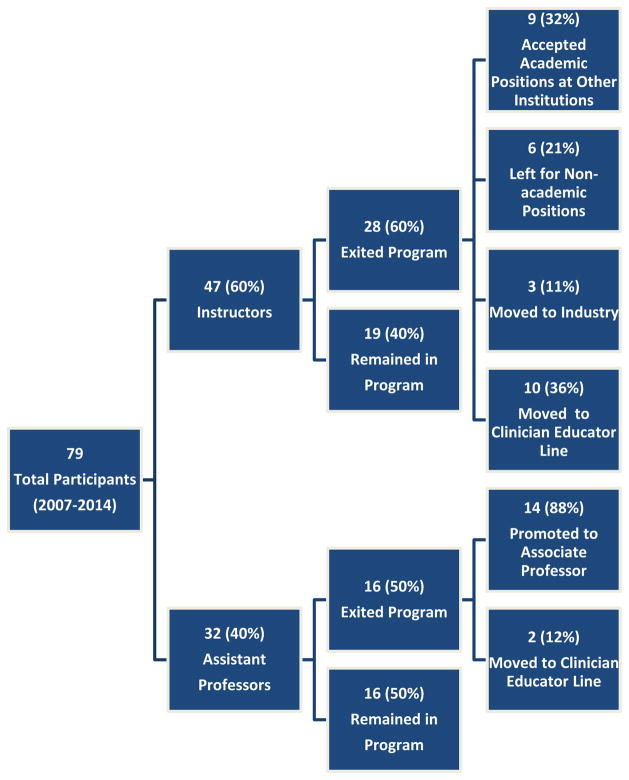
A total of 47 Instructors and 32 Assistant Professor participated as mentees during the first seven years of the program. At the time this report was prepared, 35 mentees were active in the program. Between 2007 and 2014, 44 mentees exited the PMP for a variety of reasons (Figure 2). Sixteen assistant professors “graduated” from the program because they were promoted to the rank of Associate Professor; two of these elected to move to the Clinician Educator line at Stanford which has a separate mentoring program.
Figure 2.
Flow chart of mentor program participants
There was a pattern of increased retention of Assistant Professors hired after introduction of the PMP (2007–2014) as compared with those hired at that rank between 2002–2006 using university institutional data. Unfortunately, there was no systematic tracking of retention of pediatric faculty prior to 2002. Of 13 Assistant Professors hired between 2002 and 2006, 4 left the institution for non-academic (N=3) or academic (N=1) positions at other institutions. By contrast, none of the 18 Assistant Professors hired after the PMP began in 2007 left the institution.
The remaining 28 mentees who exited the PMP were all Instructors including 9 who accepted academic positions at other institutions, 6 who left for non-academic positions and 3 who moved to industry; 10 opted to remain at Stanford on the Clinician Educator line which has a separate but similar mentoring program to the PMP. Interpreting data on retention of Instructors within the institution was more complex than that for Assistant Professors. As mentioned above, the Instructor rank is typically limited to a three year term intended to prepare junior academic physicians for a faculty role as clinician scientist or researcher. There is no commitment or expectation that a faculty position will be available or offered within the institution at the end of the Instructor term. For this reason, many Instructors leave the institution to assume academic, clinical, or industry positions after three years. Six have successfully competed for Assistant Professor billets on the MCL or UL lines at Stanford while 10 others have opted to transition to the Clinician Educator line within the department of pediatrics.
Lessons Learned
We have learned valuable lessons during the first seven years of the PMP. Firstly, we confirmed the value of individual mentoring by faculty who were not part of the mentee’s division. The PMP mentoring role was that of career and life coach, addressing professional activities as well as work-life balance without the potential conflicts of interest biasing a division chief or department chair. This allowed the mentor to serve as advocate when appropriate (and with permission from the mentee) to negotiate for more protected research time, expanded teaching opportunities, or promotion on behalf of the mentee. It was important to mandate the mentoring meetings both to eliminate the perception that mentees needed remedial support and to engage the mentees who were skeptical initially that they needed this guidance. As evidence of the success of the individual dyad meetings, the mentees ranked this as the most valuable aspect of PMP, took the initiative at times to meet between required meetings as problems arose, and asked to increase the minimum number of annual meetings from one to two. Secondly, based upon the attendance and evaluation data, mentees found the most worthwhile workshops to be those that fostered tangible skills (such as scientific writing) or clarified the criteria for promotion. Thirdly, we learned that Instructors at the beginning of their academic careers wanted additional support from peers to address their professional uncertainties. They requested that we establish opportunities for them to meet with and without mentors and to hear from near-peers about their paths to promotion. Fourthly, we believe that financial support from the department of pediatrics was important to sustain the PMP for more than seven years. This funding ensured protected time for mentoring and paid for the administrative services needed to organize workshops, perform annual assessments of the program, track mentor-mentee meetings, and facilitate the grant review process. Limited or unprotected time for both mentor and mentee and lack of funding have been identified as key barriers to success in several mentoring programs.4, 6
We acknowledge several limitations of the descriptive, qualitative nature of this report. The findings represent data from a single institution with limited “pre-PMP” data and no control group for comparison. The program focused only on Instructors and Assistant Professors interested in a career as a physician scientist or clinician investigator. We did not collect data on acquisition of grants, the number or impact factor of publications or other objective measures of productivity after initiation of the PMP because these metrics would be influenced by myriad factors beyond the control of the mentoring program. In addition, the PMP mentor role was not viewed as a functional one with a specific project as an end point; it was anticipated that research mentors and division chiefs would fulfill that role. 9 We assessed the success of the program through reported satisfaction and retention data, both of which had limitations. Annual surveys were anonymous, precluding analysis of changes in satisfaction for individual mentees. Exit interviews with mentees leaving the program were conducted only after year 3. The PMP program appeared to boost satisfaction more than self-efficacy according to data from annual questionnaires perhaps because we could provide information in some areas such as the criteria for advancement (a highly rated satisfaction item). By contrast, helping mentees attain work-life balance (a poorly rated self-efficacy item) involves factors beyond the control of the PMP. We could not exclude the contribution of factors other than mentoring that could have contributed to increased faculty retention after initiation of the PMP. During this period, the Chief of Pediatrics increased faculty salaries to match national guidelines and university regulations were modified to allow faculty on the Clinician Educator line to act as Principal Investigators on clinical research projects. The latter change made the option of remaining at this institution on the Clinician Educator line more attractive. At the same time, negative pressure on retention came from stricter enforcement of the three year limit for Instructors unless individuals had continuing grant support. Finally, we recognize that the PMP alone was insufficient to ensure successful retention of all mentees in part because faculty opportunities were not available.
The next steps for the PMP will include ongoing monitoring of retention and satisfaction. Specifically, we plan discussions with division chiefs, mentors and mentees to address the concerns raised by questionnaires and interviews. The goal will be to envision additional ways to better support and guide junior faculty. Overall, we view the PMP as successful in building satisfaction and conveying the commitment of the pediatrics department to fostering career development. As a clear-cut testament to the value of the program, once faculty on the Clinician Educator (CE) line learned of the PMP offerings, they requested that similar mentoring support be provided to them. We have fashioned a mentoring program for faculty on CE line using the model of the PMP, with emphasis on individual mentoring sessions and relevant workshops. Shared observations from programs such as PMP are needed to refine the optimal mentoring models to retain and advance the careers of physicians in academic settings.
Acknowledgments
We acknowledge the Department of Pediatrics, Stanford School of Medicine; Lucile Packard Foundation for Children’s Health; Stanford Child Health Research Institute; and the National Institutes of Health Clinical and Translational Science Award UL1 TR001085 for supporting this work. Sponsors were not involved in study design, analysis, or interpretation of data. We thank Dr. Hugh O’Brodovich, Chief of the Department of Pediatrics, for his support; Dr. Hannah Valentine for her leadership; Jessica Olson, Margaret Venables, Guadalupe Makasyuk, and Michael Canizares for technical assistance; Linda McLaughlin for invaluable contributions in early program design, implementation and evaluation; the mentees and the other program mentors, Drs. Paul Grimm, Elizabeth Mellins, Richard Moss, Stephen Roth, Eric Sibley, and Krisa Van Meurs for their dedication.
Contributor Information
Mary M. Chen, Department of Pediatrics, Stanford University School of Medicine, Stanford Palo Alto, California, USA
Christy I. Sandborg, Department of Pediatrics, Stanford University School of Medicine, Stanford Palo Alto, California, USA
Louanne Hudgins, Department of Pediatrics, Stanford University School of Medicine, Stanford Palo Alto, California, USA.
Rania Sanford, Faculty Development and Diversity, Stanford University, Stanford, California, USA.
Laura K. Bachrach, Department of Pediatrics, Stanford University School of Medicine, Stanford Palo Alto, California, USA
References
- 1.Moses H, III, Matheson DHM, Cairns-Smith S, George BP, Palisch C, Dorsey R. The Anatomy of Medical Research: US and International Comparisons. Journal of the American Medical Association. 2015;313:174–89. doi: 10.1001/jama.2014.15939. [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents and early career physicians relative to the general U.S. Population. Academic Medicine. 2014;89:443–51. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 3.Ries A, Wingard D, Morgan C, Farrell E, Letter S, Reznik V. Retention of junior faculty in academic medicine at the University of California, San Diego. Academic Medicine. 2009;84:37–41. doi: 10.1097/ACM.0b013e3181901174. [DOI] [PubMed] [Google Scholar]
- 4.Jackson VA, Palepu A, Szalacha L, Caswell C, Carr PL, Inui T. “Having the right chemistry”: A qualitative study of mentoring in academic medicine. Academic Medicine. 2003;78:328–34. doi: 10.1097/00001888-200303000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Academic Medicine. 2013;88:1029–37. doi: 10.1097/ACM.0b013e318294f368. [DOI] [PubMed] [Google Scholar]
- 6.Berk RA, Berg J, Mortimer R, Walton-Moss B, Yeo TP. Measuring the effectiveness of faculty mentoring relationships. Academic Medicine. 2005;80:66–71. doi: 10.1097/00001888-200501000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Tracy EE, Jagsi R, Starr R, Tarbell MJ. Outcomes of a pilot faculty mentoring program. American Journal of Obstetrics and Gynecology. 2004;191:1846–50. doi: 10.1016/j.ajog.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Thorndyke LE, Gusic ME, George JH, Quillen DA, Milner RJ. Empowering junior faculty: Penn State’s faculty development and mentoring program. Academic Medicine. 2006;81:668–73. doi: 10.1097/01.ACM.0000232424.88922.df. [DOI] [PubMed] [Google Scholar]
- 9.Gusic ME, Milner RJ, Tisdell EJ, Taylor EW, Quillen DA, Thorndyke LE. The essential value of projects in faculty development. Academic Medicine. 2010;85:1484–91. doi: 10.1097/ACM.0b013e3181eb4d17. [DOI] [PubMed] [Google Scholar]
- 10.Kubiak NT, Guidot DM, Trimm RF, Kamen DL, Roman J. Recruitment and Retention in Academic Medicine—What Junior Faculty and Trainees Want Department Chairs to Know. The American Journal of the Medical Sciences. 2012;344:24–7. doi: 10.1097/MAJ.0b013e318258f205. [DOI] [PubMed] [Google Scholar]
- 11.Mann S. Medical schools improve retention, job satisfaction. AAMC Reporter. 2011;20(7):10. [Google Scholar]