Abstract
Objective
Among patients with Alzheimer’s disease (AD), sleep disturbances are common and serious noncognitive symptoms. Previous studies of AD patients have identified deformations in the brain stem, which may play an important role in the regulation of sleep. The aim of this study was to further investigate the relationship between sleep disturbances and alterations in brain stem morphology in AD.
Materials and methods
In 44 patients with AD and 40 healthy elderly controls, sleep disturbances were measured using the Neuropsychiatry Inventory sleep subscale. We employed magnetic resonance imaging-based automated segmentation tools to examine the relationship between sleep disturbances and changes in brain stem morphology.
Results
Analyses of the data from AD subjects revealed significant correlations between the Neuropsychiatry Inventory sleep-subscale scores and structural alterations in the left posterior lateral region of the brain stem, as well as normalized brain stem volumes. In addition, significant group differences in posterior brain stem morphology were observed between the AD group and the control group.
Conclusion
This study is the first to analyze an association between sleep disturbances and brain stem morphology in AD. In line with previous findings, this study lends support to the possibility that brain stem structural abnormalities might be important neurobiological mechanisms underlying sleep disturbances associated with AD. Further longitudinal research is needed to confirm these findings.
Keywords: Alzheimer’s disease, sleep, brain stem, MRI, shape analysis
Introduction
Alzheimer’s disease (AD) is the most prevalent neurodegenerative condition that leads to dementia. Along with memory loss and cognitive impairment, patients with AD also suffer from dysfunctions of homeostatic and autonomic mechanisms, including mood regulation, pain perception, and sleep–wake cycles.1 Such noncognitive abnormalities are clinically referred to as behavioral and psychological symptoms of dementia (BPSD).
Sleep-related BPSD affects up to 40% of AD patients prior to their clinical diagnosis of overt dementia.2 Sleep is essential for brain function, such as memory consolidation, and it has been suggested that disturbed sleep exacerbates cognitive decline or AD progression.2,3 Although the connection between the etiology of sleep disorders and AD is poorly understood, previous findings have suggested a robust connection and a possible bidirectional link between sleep distortion and AD pathogenesis.4,5 They showed that chronic sleep deprivation increased chronic accumulation of β-amyloid (Aβ) in the brain.5 Moreover, cerebral Aβ retention may lead to wakefulness and altered sleep patterns.5 These results stress the importance of examining brain structures pertinent to regulation of sleep, which could help to pinpoint important loci in the progression of AD.
Findings in postmortem studies have located detectable AD-related biochemical changes in the brain stem, which contains neuronal networks that play key roles in the regulation of sleep.6 In addition, our previous in vivo structural imaging study using magnetic resonance imaging (MRI) showed significant morphological deformations in the upper posterior regions of the brain stem in AD patients.7 In this regard, brain stem structural abnormalities might be important neurobiological mechanisms underlying sleep disturbances associated with AD.
The aim of this study was to explore the relationships between brain stem morphological changes and sleep disturbances in patients with AD using MRI-based automated subcortical segmentation methods. We hypothesized that sleep disturbances would be correlated with deformations in posterior brain stem morphology in AD patients.
Materials and methods
Study participants
A total of 84 subjects (44 with AD and 40 healthy elderly controls) participated in this study. They were recruited from the Geriatric Psychiatry Brain Imaging Database, which holds brain scans of outpatients and inpatients at the Department of Geriatric Psychiatry, Saint Vincent Hospital, The Catholic University of Korea. All subjects were right handed. AD subjects met the National Institute of Neurological and Communicative Disorders and Stroke/Alzheimer Disease and Related Disorders Association criteria for probable AD,8 and scored 1 or greater on the Clinical Dementia Rating scale.9 Participants who suffered from other neurological or psychiatric conditions, including other forms of dementia, or who were taking any psychotropic medications were excluded. We measured cognitive functions using the Korean version of the Consortium to Establish a Registry for Alzheimer’s disease.10 Severity of sleep disturbance was measured using the sleep-disturbance domain of the Neuropsychiatric Inventory (NPI) scale. Patients who had a score of 1 or more on the scale were characterized as having sleep disturbance. To minimize the influence of other psychiatric conditions on sleep disturbances, we included only participants who scored zero in the other eleven domains of the NPI scale (delusions, hallucinations, agitation or aggression, depression, anxiety, euphoria, apathy, disinhibition, irritability, motor disturbance, and eating behavior).
Ethical and safety approval for the study was obtained from the local institutional review board of The Catholic University of Korea. Written informed consent was obtained from all participants and their guardians.
MRI acquisition
MRI scans of all participants were obtained using a 3 T whole-body scanner equipped with an 8-channel phased-array head coil (Verio; Siemens AG, Munich, Germany). The scanning parameters of the T1-weighted three-dimensional magnetization-prepared rapid gradient-echo sequences were as follows: echo time 2.5 ms, repetition time 1,900 ms, inversion time 900 ms, flip angle 91°, field of view 250×250 mm, matrix 256×256 mm, and voxel size 1.0×1.0×1.0 mm3.
Image processing
The three-dimensional MRI images were registered and processed within the Bayesian Appearance Model framework as designed in an earlier study by the Oxford Centre for Functional MRI of the Brain (FMRIB).11 During registration, MRI images were transformed to the MNI152 standard space by affine transformations on the basis of df=12. Different subcortical structures, such as the brain stem, were located based on shape models and voxel intensities through the application of a subcortical mask and the FMRIB Integrated Registration and Segmentation Tool (FIRST). Boundary correction was applied for improved accuracy. Absolute volumes of the subcortical structures were calculated with consideration of the transformations performed during the initial registration steps. Brain stem volumes (BVs) were normalized to the total intracranial volume (TICV), measured using the Sienax software.12 Normalized BV (NBV) was defined as NBV = mean TICV × BV/TICV.
Volume and shape analysis
FIRST analyzes the volume and shape of each subcortical structure using a deformable surface-mesh model. Although the segmentation process of FIRST is largely automated, two important aspects of the mesh model must be inspected in its application: vertex correspondence and surface alignment. First, the number of vertices for each structure must have a fixed value, so that corresponding vertices can be compared across individuals and between groups. Such vertex correspondence is crucial for the FIRST methodology, because group differences in the spatial location of each vertex are directly used for the examination of localized shape differences. Second, even when the vertices retain correspondence, the surfaces of the mesh reside in the native image space, and thus are arbitrarily oriented or positioned. Therefore, surface alignment must be standardized before investigating any group differences. The mean surface from FIRST models was used as the target to which surfaces from individual participants were aligned. Pose was removed by minimizing the sum-of-squares difference between the corresponding vertices of a participant’s surface and the mean surface. Correlation analyses of the vertices were performed using F-statistics with the statistical significance threshold set at a P-value of less than 0.05 (false-discovery rate [FDR]) to resolve the issue of multiple comparisons. The effects of age, education, TICV, and sex were regressed out. The Duvernoy brain stem atlas was incorporated as a reference in determining the approximate anatomical location of our statistical maps.13
Results
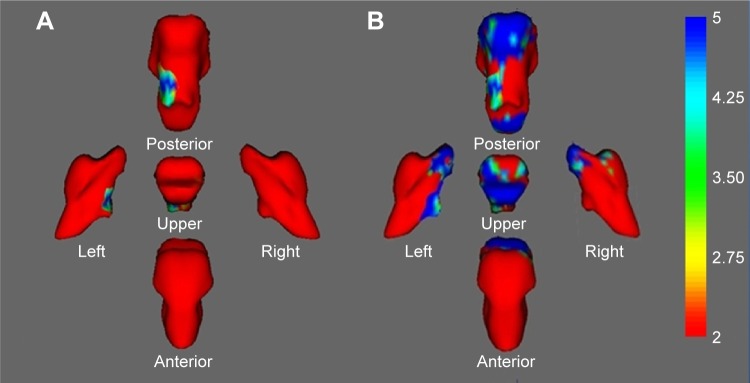
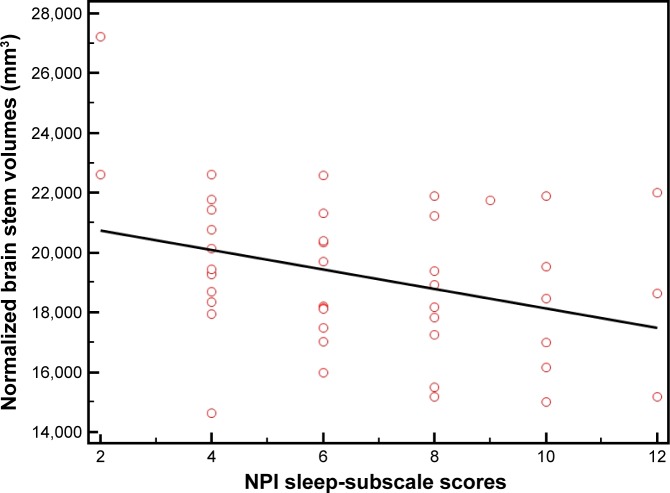
Table 1 shows the baseline demographic data of our participants. Of the 44 AD subjects with sleep disturbances, 26 (59%) had circadian rhythm disturbances, 14 (32%) had insomnia, and four (9%) had hypersomnia. There were no sleep disturbances in the control subjects. The data from surface-based vertex analyses revealed significant structural alterations in the left posterior lateral region of the AD patients’ brain stems that correlated with their NPI sleep-subscale scores (FDR-corrected P<0.05, Figure 1A). In addition, significant group differences between the AD group and the control group were observed in posterior brain stem morphology (FDR-corrected P<0.05, Figure 1B). Furthermore, the normalized BVs of the AD patients correlated with their NPI sleep-subscale scores (r=−0.33, P=0.024, Figure 2).
Table 1.
Demographic and clinical characteristics of study participants
| Control group (n=40) |
AD group (n=44) |
P-value | |
|---|---|---|---|
| Age (years) | 75.2±4.7 | 76.2±5.7 | NS |
| Education (years) | 9.2±2.1 | 9.2±2.4 | NS |
| Sex (male:female) | 14:26 | 13:31 | NS |
| CDR score | 0 | 1.5±0.5 | |
| CERAD-K battery | |||
| VF | 14.3±2.7 | 6.3±3.2 | <0.0001 |
| BNT | 11.1±3.1 | 7.2±2.3 | <0.0001 |
| MMSE | 28.7±1.2 | 21.2±3.1 | <0.0001 |
| WLM | 17.5±3.2 | 7.1±3.4 | <0.0001 |
| CP | 8.9±2.5 | 6.8±1.9 | <0.0001 |
| WLR | 7.5±1.5 | 3.3±1.8 | <0.0001 |
| WLRc | 10.1±1.4 | 3.5±1.7 | <0.0001 |
| CR | 6.5±2.8 | 3.2±2.9 | <0.0001 |
| NPI sleep-disturbance subscale | 0 | 6.7±2.6 | <0.0001 |
| Normalized brain stem volume (mm3) | 21,927±1,623.6 | 18,216.3±2,120.7 | <0.0001 |
Note: Data shown as number or mean ± SD.
Abbreviations: AD, Alzheimer’s disease; SD, standard deviation; NS, not significant; CDR, Clinical Dementia Rating; CERAD-K, Consortium to Establish a Registry for Alzheimer’s Disease, Korean version; VF, verbal fluency; BNT, Boston Naming Test; MMSE, Mini-Mental Status Examination; WLM, word-list memory; CP, constructional praxis; WLR, word-list recall; WLRc, word-list recognition; CR, constructional recall; NPI, Neuropsychiatric Inventory.
Figure 1.
(A) Statistical maps corrected for age, education, and sex showing brain stem shape deformation associated with NPI sleep-disturbance subscale scores in patients with AD. (B) Group-comparison results of brain stem shape deformation between the AD group and the normal controls. Color coding of the surface reflects the FDR-corrected F-statistic values.
Abbreviations: NPI, Neuropsychiatric Inventory; AD, Alzheimer’s disease; FDR, false-discovery rate.
Figure 2.
Negative association between normalized brain stem volumes and NPI sleep-subscale scores in the AD patients (r=−0.33, P=0.024).
Abbreviations: NPI, Neuropsychiatric Inventory; AD, Alzheimer’s disease.
Discussion
To the best of our knowledge, this is the first in vivo study on brain stem morphological changes associated with sleep disturbances in AD. Recently, a growing body of evidence has suggested a potential causal relationship between sleep disturbances and AD.14 Daytime drowsiness was shown to be an accurate predictor of AD within a time span of 2–4 years.14,15 Also, improved sleep was linked with delayed onset of AD, while reduction in sleep was correlated with lower cellular tolerance of oxidation stress in the brain.16 A shared genetic risk background, such as variations in the APOE and MAOA genes, has also been implicated in disrupted sleep and AD.17,18 In addition, research with mouse models has proposed that disturbed sleep and AD pathology could affect each other by affecting the accumulation of Aβ, which is widely accepted as a major contributor to altered sleep patterns and AD pathogenesis.5
Additional lines of evidence indicate that decline in brain stem function holds important implications in the potential connection between sleep and AD. The brain stem contains networks of aminergic and cholinergic nuclei that are critical for sleep regulation. Brain stem aminergic and cholinergic neurons, such as the dorsal raphe (serotonin), locus coeruleus (noradrenaline), ventral tegmental area (dopamine), and laterodorsal tegmentum (acetylcholine) in particular, have been strongly implicated in sleep quality.1 Specific disruption or transection of these neurons is directly related to fragmented sleep with rapid eye-movement sleep deficits and even a near-constant wakefulness state.19 Slow-wave sleep, during which memory consolidation occurs, is also governed by the brain stem structures, is commonly fragmented in AD patients, and disruption of this process could potentially be a contributing factor to the cognitive decline in AD.20
The results of our study identified significant structural changes in the brain stem that correlated with the severity of sleep disturbances in AD patients. These results are consistent with those from previous studies that identified neuropathological changes and morphological alterations in the brain stems of AD patients.6,7 Although preliminary, our findings lend support to the involvement of the brain stem in both sleep and AD.
Limitations
Our study has several limitations. First, the sample size was small, and control subjects with sleep disturbances were not included in the study. Therefore, our study design was insufficient to arrive at robust conclusions about the relationship between AD and sleep. Additional in vivo neuroimaging studies would be needed to expand on the topic. Second, our analyses relied on the underlying assumption that morphological changes in the brain are measures of neuronal loss caused by intracellular neurofibrillary tangles of hyperphosphorylated tau and extracellular Aβ plaques, which are hallmark biochemical symptoms of AD.6 Therefore, a direct link between such biochemical alterations and sleep disturbances may require additional in vivo analyses utilizing amyloid or tau positron-emission tomography.21,22 Finally, the different kinds of sleep-related BPSD were not distinguished in the NPI-sleep subscale. In future studies, objective and specific measurements of sleep disturbances, such as polysomnography, might be helpful to differentiate specific types of sleep disturbances and their associations with brain stem morphology in AD.
Conclusion
In summary, this study identified morphological alterations in the brain stems of AD patients that significantly correlated with disturbances in their sleep. Sleep complications commonly occur in AD patients, starting in preclinical stages, and the connection between AD and sleep disorders has become a praised topic in the field.4 Although further research and data are needed, our results suggest that brain stem alterations might be at the core of underlying neurobiological mechanisms of sleep disturbances associated with AD.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT and Future Planning (NRF-2015R1C1A1A02036578).
The abstract of this paper was presented at 30th CINP World Congress of Neuropsychopharmacology, CINP – The International College of Neuropsychopharmacology, July 3–5, 2016, COEX, Seoul, South Korea.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Grinberg LT, Rueb U, Heinsen H. Brainstem: neglected locus in neurodegenerative diseases. Front Neurol. 2011;2:42. doi: 10.3389/fneur.2011.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moran M, Lynch CA, Walsh C, Coen R, Coakley D, Lawlor BA. Sleep disturbance in mild to moderate Alzheimer’s disease. Sleep Med. 2005;6(4):347–352. doi: 10.1016/j.sleep.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306(6):613–619. doi: 10.1001/jama.2011.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark CN, Warren JD. A hypnic hypothesis of Alzheimer’s disease. Neurodegener Dis. 2013;12(4):165–176. doi: 10.1159/000350060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ju YE, Lucey BP, Holtzman DM. Sleep and Alzheimer disease pathology: a bidirectional relationship. Nat Rev Neurol. 2014;10(2):115–119. doi: 10.1038/nrneurol.2013.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grinberg LT, Rüb U, Ferretti RE, et al. The dorsal raphe nucleus shows phospho-tau neurofibrillary changes before the transentorhinal region in Alzheimer’s disease: a precocious onset? Neuropathol Appl Neurobiol. 2009;35(4):406–416. doi: 10.1111/j.1365-2990.2009.00997.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Ryan J, Andreescu C, Aizenstein H, Lim HK. Brainstem morphological changes in Alzheimer’s disease. Neuroreport. 2015;26(7):411–415. doi: 10.1097/WNR.0000000000000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 9.Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 10.Lee JH, Lee KU, Lee DY, et al. Development of the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD–K): clinical and neuropsychological assessment batteries. J Gerontol B Psychol Sci Soc Sci. 2002;57(1):P47–P53. doi: 10.1093/geronb/57.1.p47. [DOI] [PubMed] [Google Scholar]
- 11.Patenaude B, Smith SM, Kennedy DN, Jenkinson M. A Bayesian model of shape and appearance for subcortical brain segmentation. Neuroimage. 2011;56(3):907–922. doi: 10.1016/j.neuroimage.2011.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith SM, Zhang Y, Jenkinson M, et al. Accurate, robust, and automated longitudinal and cross-sectional brain change analysis. Neuroimage. 2002;17(1):479–489. doi: 10.1006/nimg.2002.1040. [DOI] [PubMed] [Google Scholar]
- 13.Naidich TP, Duvernoy HM. Duvernoy’s Atlas of the Human Brain Stem and Cerebellum. Vienna: Springer; 2009. [Google Scholar]
- 14.Costandi M. Neurodegeneration: amyloid awakenings. Nature. 2013;497(7450):S19–S20. doi: 10.1038/497S19a. [DOI] [PubMed] [Google Scholar]
- 15.Lim AS, Kowgier M, Yu L, Buchman AS, Bennett DA. Sleep fragmentation and the risk of incident Alzheimer’s disease and cognitive decline in older persons. Sleep. 2013;36(7):1027–1032. doi: 10.5665/sleep.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Musiek ES, Xiong DD, Holtzman DM. Sleep, circadian rhythms, and the pathogenesis of Alzheimer disease. Exp Mol Med. 2015;47:e148. doi: 10.1038/emm.2014.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yesavage JA, Friedman L, Kraemer H, et al. Sleep/wake disruption in Alzheimer’s disease: APOE status and longitudinal course. J Geriatr Psychiatry Neurol. 2004;17(1):20–24. doi: 10.1177/0891988703261994. [DOI] [PubMed] [Google Scholar]
- 18.Craig D, Hart DJ, Passmore AP. Genetically increased risk of sleep disruption in Alzheimer’s disease. Sleep. 2006;29(8):1003–1007. doi: 10.1093/sleep/29.8.1003. [DOI] [PubMed] [Google Scholar]
- 19.Batini C, Moruzzi G, Palestini M, Rossi GF, Zanchetti A. Persistent patterns of wakefulness in the pretrigeminal midpontine preparation. Science. 1958;128(3314):30–32. doi: 10.1126/science.128.3314.30-a. [DOI] [PubMed] [Google Scholar]
- 20.Westerberg CE, Mander BA, Florczak SM, et al. Concurrent impairments in sleep and memory in amnestic mild cognitive impairment. J Int Neuropsychol Soc. 2012;18(3):490–500. doi: 10.1017/S135561771200001X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James OG, Doraiswamy PM, Borges-Neto S. PET imaging of tau pathology in Alzheimer’s disease and tauopathies. Front Neurol. 2015;6:38. doi: 10.3389/fneur.2015.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doraiswamy PM, Sperling RA, Johnson K, et al. Florbetapir F 18 amyloid PET and 36-month cognitive decline: a prospective multicenter study. Mol Psychiatry. 2014;19(9):1044–1051. doi: 10.1038/mp.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]