Abstract
Objectives
To investigate how displacements of maxillo-mandibular structures are associated with each other at splint removal and one year post-surgery following 1-jaw and 2-jaw surgeries for correction of Class III malocclusion.
Setting and Sample Population
Fifty patients who underwent surgical correction with maxillary advancement only (n=25) or combined with mandibular set back (n=25) were prospectively enrolled in this study.
Methods
CBCTs were taken pre-surgery, at splint removal and at one year post-surgery. Three-dimensional cranial base superimpositions and shape correspondence were used to measure the outcomes from pre-surgery to splint removal (surgical changes) and splint removal to one year post-surgery (post-surgical adaptations). Pearson correlation coefficients were used to evaluate the association between the regional displacements.
Results
Both surgery groups presented mandibular clockwise rotation with surgery and post-surgical adaptive counterclockwise rotation. In patients treated with maxillary advancement only, the surgical changes of the maxilla were significantly correlated with chin changes. The amount/and direction of chin autorotation was significantly correlated with right and left ramus autorotation. Right and left condylar displacements were significantly correlated. One year post-surgery, adaptive displacements/bone remodeling of both rami were correlated to the chin and condylar changes. For the 2-jaw group, the few correlations between the positional and/or remodeling changes in the anatomic regions of interest observed due to the surgery were different than those observed after post-surgical adaptations, suggesting that these changes occurred independently.
Conclusion
Our results indicate that surgical displacements and post-surgical adaptations are often correlated in one-jaw surgery and are in general, independent in two-jaw surgery.
Keywords: Imaging, Three-Dimensional, Cone-Beam Computed Tomography, Class III, Orthognathic Surgery, Treatment Outcome
Introduction
The hierarchy of stability following orthognathic surgery for correction of Class III skeletal malocclusion indicates that maxillary advancement is highly stable, 2-jaw surgery with rigid internal fixation (RIF) only is stable, and mandible set back alone is less stable. The stability of jaw surgery outcomes may vary depending on the vertical movement of the maxilla and the posterior displacement of the mandibular gonial angle.(1,2)
Two-dimensional (2D) images have been used to diagnose and treatment plan orthognathic surgery patients in the past decades with low radiation doses.(3) With the advent of three-dimensional (3D) images, such as cone beam computed tomography (CBCT) with new superimposition methods (4,5) clinicians are now provided better understanding of bilateral structures,(6) and greater accuracy when compared to other 2D techniques.(7)
Recent 3D imaging studies reporting hard tissue outcomes of orthognathic surgery have utilized a variety of commercial and open-source software for quantification of 3D changes. Previous studies have reported 3D cephalometric conventional angular and linear measurements (x and y axis separately),(8–10) skeletal segment displacements(11) and/or remodeling,(12) or general mandibular changes.(13)
De Paula et al.(14) applied a novel method to quantify surface displacements using cranial base superimposition and, compared changes due to surgery (6 weeks follow-up) and post-surgical adaptation (1 year follow-up) for Class III patients undergoing 2-jaw surgery or maxillary advancement only. Those results revealed greater individual variability than previous 2D findings (15,16) and led to the questions addressed in the present study about possible associations between the skeletal maxillary and mandibular post-surgical adaptations that may affect the stability of the surgical correction. This present study investigated whether displacements with surgery are associated with postoperative changes in surgical correction of Class III malocclusions. Specifically, the purpose of this study was to evaluate the association between 3D changes in the position of the condyles, rami, and chin at splint removal and 1 year after surgery for correction of skeletal Class III malocclusion.
Materials and Methods
Subjects
This study performed secondary data analysis of existing data (14) prospectively collected from 50 patients (23 male, 27 female, mean age 24.7 years old) who had undergone orthognathic surgery, after approval of the Institutional Review Board of the University of North Carolina. All the patients had skeletal Class III discrepancies with edge-to-edge occlusion or negative overjet. Combined orthodontic-orthognathic surgery was the treatment option of choice to fully correct the malocclusion and skeletal imbalances for this study sample. The cohort was divided into two groups, 1-jaw (maxillary advancement only) and 2-jaw surgery (maxillary advancement and mandibular set back). The maxillary surgical procedure consisted of Le Fort 1 surgeries and the mandibular procedures were bilateral split sagittal osteotomies. Rigid internal fixation was used post-surgically for all patients. Patients with syndromes, cleft lip and/or palate or disharmonies due to trauma were excluded.
CBCT acquisition
CBCT images were acquired at three different time points: before surgery, at splint removal 6 weeks after surgery, and at 1 year follow up. The scanning protocol involved a 36-second full head exposure, using the NewTom 3G scanner (Aperio Services, Sarasota, FL) with a 12 inch field of view. Ten patients had at least one CBCT taken with a NewTom 9000 (Aperio Services, Sarasota, FL) with a 9 inch field of view, therefore, either the chin or the condyles were missing in these patients. The voxel dimension was an isotropic 0.3 × 0.3 × 0.3mm that was reformatted to 0.5 × 0.5 × 0.5 mm using CMFreg (formerly Imagine, http://www.slicer.org/slicerWiki/index.php/Documentation/Nightly/Extensions/CMFreg) to facilitate image processing. During the scan all the subjects were biting a thin wax to maintain centric relation.
Image processing
After the CBCT acquisitions, segmentations of the volumes were performed using open-source software, ITK-Snap (www.itksnap.org).(17) After this step, to superimpose different time points, all the post-surgical models were registered using the cranial base of the pre-surgery volume as reference. This procedure consists of a fully automated voxel-wise rigid registration that compares and matches the intensities of the voxel gray scales at the cranial base between different time points and relocates the image with 6 degrees of freedom.(4)
Six anatomic regions of interest were selected (Figure 1) and the largest displacement for each region was calculated from pre surgery to splint removal (surgical changes) and splint removal to 1 year post-surgery (post-surgical adaptations). Shape analyses and measurements of surgical outcomes were computed by subtracting pre and post-surgeries point-based correspondent models. Corresponding surface distances were displayed via color-coded distance magnitude and vector maps (Figure 2). The shape correspondence method, SPHARM-PDM software, was introduced by Styner et al (18) and later applied to orthognathic surgery patients by other authors.(14,19–21) The distance maps provided the magnitude of the position changes between two point-based correspondent models, while the vector maps provided the directionality of these positional displacements. Semi-transparencies showed the qualitative comparison between the two time points.
Figure 1.
Anatomic regions of interest: 1 – maxilla, 2 – right condyle, 3 – left condyles, 4 – right ramus, 4 – left ramus, 5 – chin.
Figure 2.
The magnitude and directionality of displacement is shown by the color-coded map and vectors.
Statistical analysis
All statistical analyses were performed with Statistical Package for the Social Sciences 17.0 (Chicago, IL, USA). Intra class correlation (ICC) was calculated to assess intra-observer error, 10 patients were randomly selected and measured twice in a 10 day interval.
Pearson correlation coefficients were calculated to assess the associations between surgical displacements and post-surgical adaptations of the anatomic regions for both types of surgery. Statistical significance was set at 0.05.
Results
Intra class correlation reveled greater than 0.90 agreement between repeated measurements for all anatomic regions of interest.
The analysis of the average surgical and postoperative displacements for each anatomic region and the descriptive statistics for this sample have been described in detail by De Paula et al.(14).
Maxilla only
The evaluation of the semi-transparencies showed that the condyles were pushed backward and upward in the glenoid fossa, and that clockwise rotation of the ramus/chin occurred. At 1 year post-surgery, the condyles had returned closer to their initial pre-surgical position, while the ramus and chin had counterclockwise rotation. Partial post-surgical posterior displacement of the maxilla was observed, with also post-surgical superior displacement in a few cases where downward movement occurred during surgery.
The Pearson correlation coefficients for surgical changes are shown in Table 1. The maxillary displacement was positively correlated with the chin clockwise rotation (r = .579, p = .002). The chin displacement was negatively correlated with the right (r = −.499, p = .018) and left ramus (r = −.630, p = .001). The displacement of the right condyle was correlated with the right ramus (r = .478, p = .009) and the left condyle (r = .348, p = .048).
Table 1.
Correlation between surfaces displacement for maxilla only group.
| T1–T2
|
T2–T3
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maxilla | RC | RR | Chin | LC | LR | Maxilla | RC | RR | Chin | LC | LR | |
| T1–T2 | ||||||||||||
| Maxilla | - | −.121 | −.231 | .579* | −.088 | −.211 | −.311 | .154 | .024 | −.335 | .079 | .559* |
| RC | .287 | - | .478* | −.262 | .348* | .271 | −.395* | −.345* | −.143 | .137 | −.236 | −.172 |
| RR | .139 | .009 | - | −.449* | .389* | .237 | −.122 | .172 | .189 | .166 | −.096 | −.073 |
| Chin | .002 | .119 | .018 | - | .110 | −.630* | .039 | .103 | .334 | −.639* | .302 | .603* |
| LC | .342 | .048 | .030 | .312 | - | −.169 | .131 | .030 | .202 | −.212 | −.056 | .115 |
| LR | .161 | .100 | .132 | .001 | .215 | - | .097 | .018 | −.284 | .153 | −.479** | −.581* |
| T2–T3 | ||||||||||||
| Maxilla | .074 | .236 | .455 | .064 | .356 | .002 | - | −.011 | −.179 | −.026 | −.137 | −.337 |
| RC | .031 | .050 | .252 | .271 | .133 | .211 | .480 | - | .461* | −.129 | .375* | .102 |
| RR | .290 | .211 | .189 | .230 | .327 | .368 | .206 | .012 | - | −.589* | .397* | .206 |
| Chin | .431 | .324 | .064 | .001 | .086 | .001 | .454 | .283 | .002 | - | −.248 | −.432* |
| LC | .275 | .445 | .171 | .171 | .398 | .296 | .266 | .036 | .027 | .133 | - | .499* |
| LR | .330 | .467 | .090 | .249 | .009 | .001 | .058 | .318 | .167 | .022 | .007 | - |
Lower left “triangle” shows P values and upper right “triangle” shows r value.
RC (right condyle), RR (right ramus), LC (left condyle), LR (left ramus).
Statistically significant, P ≤ 0.05
Between splint removal and 1 year after surgery, post-surgical adaptations of maxilla were not correlated to displacements of any other anatomic region of interest (Table 1). The chin displacement was correlated to the right (r = −.589, p = .002) and left ramus (r = −.432, p = .022). The displacement of the right condyle was correlated to the right ramus (r = .461, p = 0.12) and the left condyle (r = .375, p = .036). The displacement of the left condyle was also correlated with the left (r = .499, p = .007) and right ramus (r = .397, p = .027).
Two-jaw
Patients who underwent 2-jaw surgery also presented clockwise rotation of the mandible and posterosuperior condyles translation with surgery. In addition, there was lateral rotation of the rami/condyles resulting from the mandibular surgery and fixation. Between splint removal and 1 year post-surgery, post-surgical adaptations included counterclockwise rotation of the mandible, and lateral rotation of the rami/condyles. Partial post-surgical posterior displacement of the maxilla was observed, with also post-surgical superior displacement in a few cases where downward movement occurred during surgery.
The Pearson correlation coefficients of the associations between displacements with surgery in this group are shown in Table 2. The right ramus displacement was correlated to the chin (r = −.467, p = .025) and the right condyle (r = .415, p = .024). The displacement of the right condyle was correlated to the left condyle (r = −.367, p = .042).
Table 2.
Correlation between surfaces displacement for two jaw group.
| T1–T2
|
T2–T3
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maxilla | RC | RR | Chin | LC | LR | Maxilla | RC | RR | Chin | LC | LR | |
| T1–T2 | ||||||||||||
| Maxilla | - | .142 | .212 | .027 | −.098 | −.028 | .057 | .021 | −.411* | .264 | −.163 | −.011 |
| RC | .260 | - | .415* | −.140 | −.367* | −.101 | −.243 | .188 | −.012 | −.152 | −.094 | −.171 |
| RR | .160 | .024 | - | −.467* | −.335 | .272 | −.022 | .060 | −.199 | .358 | −.059 | −.204 |
| Chin | .457 | .296 | .025 | - | −.242 | −.297 | −.216 | −.174 | .127 | −.262 | .112 | .475* |
| LC | .325 | .042 | .055 | .167 | - | .100 | .199 | .148 | .271 | .001 | −.119 | −.148 |
| LR | .448 | .324 | .100 | .116 | .321 | - | .166 | −.096 | −.281 | .155 | .042 | −.236 |
| T2–T3 | ||||||||||||
| Maxilla | .403 | .462 | .023 | .145 | .223 | .479 | - | −.192 | −.072 | .218 | −.642* | −.438* |
| RC | .151 | .195 | .479 | .280 | .335 | .217 | .208 | - | −.287 | .372 | .340 | −.048 |
| RR | .462 | .393 | .176 | .072 | .392 | .170 | .378 | .092 | - | −.252 | −.103 | .258 |
| Chin | .210 | .253 | .308 | .155 | .329 | .023 | .209 | .071 | .157 | - | −.159 | −.165 |
| LC | .194 | .251 | .100 | .499 | .289 | .246 | .001 | .056 | .316 | .265 | - | .508* |
| LR | .236 | .331 | .091 | .269 | .424 | .133 | .024 | .414 | .112 | .256 | .006 | - |
Lower left “triangle” shows P values and upper right “triangle” shows r value.
Statistically significant, P ≤ 0.05
The Pearson correlation coefficients of the associations between post-surgical adaptations at different anatomic regions of interest are shown in Table 2. The maxillary changes were correlated to the left condyle (r = −.642, p = .001) and left ramus (r = −.438, p = 0.24). The changes in the left ramus were correlated to the left condyle (r = .508, p = .006).
Discussion
The preliminary assessments of post-surgical adaptations reported by De Paula et al.(14), for each anatomical region in 1 and 2-jaw surgery, revealed that all the mandibular regions of interest had greater changes from splint removal to 1 year follow-up in the 2-jaw surgery group, Maxillary changes were not influenced by the type of surgery. The present study shed light into the associations between postoperative adaptations at different anatomic regions after surgeries for Class III correction.
The results of the present study indicate that in the 1-jaw surgery group, the maxillary and condylar displacements led to clockwise rotation of the mandible. The correlation between the chin and posterior border of the ramus shows that as the mandible rotates clockwise or counterclockwise, the gonial angle is pushed back or forward, respectively. Given the fact that there was no surgical displacement of the mandible in the surgery patients, we would expect all the regional changes would be correlated. Our findings can possibly be explained by 1) the condyles could have been displaced asymmetrically in the glenoid fossa, therefore the changes in one side could have been different than the other side, affecting the statistical report or 2) the mandible rotated but the condyles were not translated in the glenoid fossa. For the 1-jaw group, post-surgical adaptations were correlated to maxillary downward movement leading to counterclockwise rotation of the mandible. According to Proffit et al (15), if the maxilla moved downwards after surgery, there is a likelihood of greater post-surgical adaptative changes, mostly due to the vertical relapse and occlusal forces.(15) Such maxillary post-surgical adaptive changes may explain the combination of forward and downward condylar displacement, with counterclockwise rotation of the mandible between splint removal and 1 year after surgery.
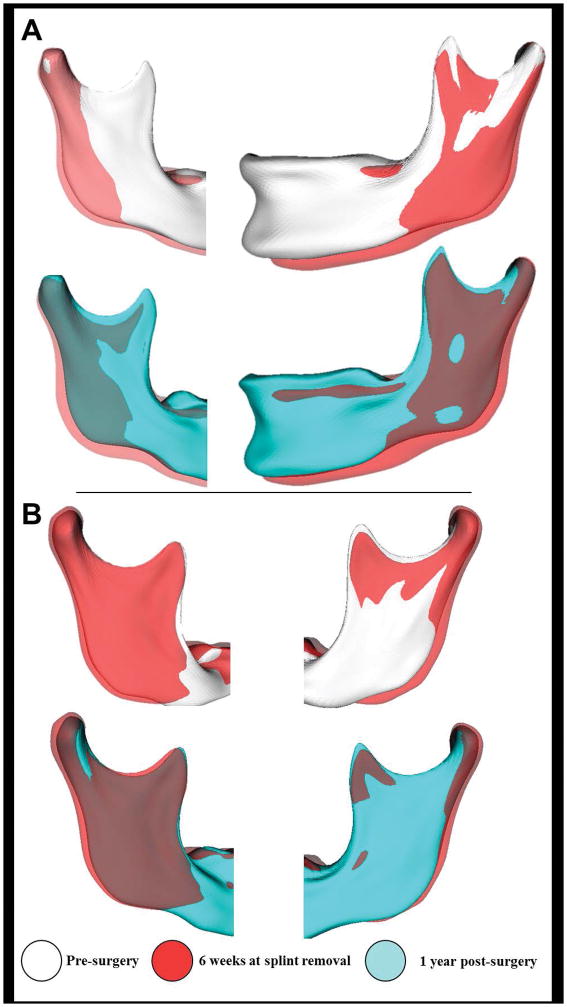
Based on the 3D superimpositions the same pattern of mandibular changes (clockwise rotation after surgery and counterclockwise rotation after post-surgical adaptation, Figure 3) and condyles translation occurred in both 1 and 2-jaw surgery groups. Our findings suggest that in 2-jaw surgery patients, even if the maxilla is not displaced downward, care should be taken during the mandibular set back not to push the gonial angle posteriorly or over seat the condyles at the glenoid fossa. Ayoub et al(22) suggested that condylar repositioning is an important maneuver to avoid postoperative relapse and the rotation is expected during the fixation with screws in bilateral sagittal split osteotomy. Our results corroborate the findings of Kim et al(9) who showed postero superior condylar displacement 6 months after surgery, that returned to its initial position after 17 months. On the contrary, Kim et al(11) reported insignificant condylar displacement 3 months after surgery. Such variability in postoperative adaptations requires additional investigation using the 3D superimposition methods described in this study.
Figure 3.
Semi-transparencies of a 2-jaw surgery patient showing a clockwise rotation. Notice that in the left image, there was clockwise rotation with the anterior nasal spine region was displaced forward and downward. The middle image shows the post-surgical readaptation with counterclockwise rotation and maxilla moving up. In the right image comparing pre-surgery and one year follow-up, seems that the maxillary advancement was linear.
In the present study, the position of the mandibular ramus was not correlated to the chin displacements with surgery or post-surgery in the 2-jaw surgery group. Politi et al(23) found the surgical set back at Pog was correlated to displacement of Go, displacement at Pog was correlated to clockwise rotation of ramus, and post-surgical counterclockwise rotation of the ramus was correlated to relapse at Pog. Such findings corroborate the results reported by Proffit et al (16) and Franco et al (24) and differ from the present study. The lack of associations between mandibular anatomic regions in the 2-jaw surgery group in this study can possibly be explained by lateral rather than anteroposterior ramus displacement (Figure 4). Figure 5 clearly shows that when the gonial angle is pushed back during the surgery it will likely move forward during post-surgical adaptation as described in the literature.(2,22,25) To avoid such ramus displacements, a semi-rigid fixation has been proposed (26,27) that would allow the movement of the proximal segment without having direct effect in the distal segment. Post-surgical adaptive changes in the mandible may be also be controlled by careful condylar seating during surgery. Politi et al (23) found that the surgical displacement of the chin was correlated to its post-surgical adaptation for 2-jaw surgery group. The present study found a correlation between surgical displacement of the chin and its post-surgical adaptation only in the 1-jaw surgery group.
Figure 4.
Semi-transparencies of a 2-jaw surgery patient showing the lateral displacement of the ramus after surgery and during post-surgical adaptation.
Figure 5.
Semi-transparencies of a 2-jaw surgery patients. A – Ramus was pushed back during surgery and returned to forward after 1 year. Notice that the condyles were maintained in the same position for the 3 time points. B – Another example of the muscle forces acting on the ramus, however, in this case the condyles were pushed backward and upward during surgery. The post-surgical adaptation showed a combination of condyles and ramus being displaced anteriorly.
While this study utilized novel image analysis methods, shape correspondence computation is very time consuming, and requires extensive training to perform the evaluations. This method has potential research applications, but its translation to clinical use still requires further software development. The image analysis software engineering continues to be developed thanks to the open-source nature of the programming code. Additionally, the image analysis findings in this study refer to displacements and changes relative to the cranial base registration. Assessments of local bone resorption and apposition would require regional registration to specifically measure bone resorption. The present study sample included patients with different severity of Class III, which could be affect the postsurgical adaptive association among local changes. The condyle remodeling due to the different types of surgery and long term maxillo-mandibular changes using 3D images and cranial base superimposition is a relatively new subject that requires further investigation.
Conclusions
Superimposition of 3D virtual surface models clearly showed the associations of postoperative adaptations of different anatomic regions after 1-jaw surgery for correction of Class III skeletal discrepancies. The postoperative adaptations of different anatomic regions occurred independently of each other in the 2-jaw surgery group. Both groups had surgical mandibular clockwise rotation, and counterclockwise rotation occurred during post-surgical adaptation.
Clinical relevance.
Previous 2D cephalometry studies tracings indicated instability in 20% of the Class III patients treated with either 1 or 2-jaw surgeries. Cranial base superimpositions using CBCT imaging have helped the understanding of surgical changes and post-surgical adaptations that occur in the maxilla and mandible after correction of Class III malocclusions. Surgical displacements and post-surgical adaptations are often correlated in 1-jaw surgery and are in general, independent in 2-jaw surgery.
Acknowledgments
Supported by NICDR DE-017727 and NIDCIR/NIBIB DE-024450.
References
- 1.Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthod Orthognath Surg. 1996;11:191–204. [PubMed] [Google Scholar]
- 2.Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007;3:21. doi: 10.1186/1746-160X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grunheid T, Kolbeck Schieck JR, Pliska BT, Ahmad M, Larson BE. Dosimetry of a cone-beam computed tomography machine compared with a digital x-ray machine in orthodontic imaging. Am J Orthod Dentofacial Orthop. 2012;141:436–43. doi: 10.1016/j.ajodo.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 4.Cevidanes LH, Bailey LJ, Tucker GR, Jr, Styner MA, Mol A, Phillips CL, et al. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2005;34:369–75. doi: 10.1259/dmfr/17102411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kapila S, Conley RS, Harrell WE., Jr The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011;40:24–34. doi: 10.1259/dmfr/12615645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stratemann SA, Huang JC, Maki K, Hatcher DC, Miller AJ. Evaluating the mandible with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137:S58–70. doi: 10.1016/j.ajodo.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 7.Hilgers ML, Scarfe WC, Scheetz JP, Farman AG. Accuracy of linear temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiography. Am J Orthod Dentofacial Orthop. 2005;128:803–11. doi: 10.1016/j.ajodo.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 8.Kim YI, Cho BH, Jung YH, Son WS, Park SB. Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:681–7. doi: 10.1016/j.tripleo.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Cevidanes LH, Tucker S, Styner M, Kim H, Chapuis J, Reyes M, et al. Three-dimensional surgical simulation. Am J Orthod Dentofacial Orthop. 2010;138:361–71. doi: 10.1016/j.ajodo.2009.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Draenert FG, Erbe C, Zenglein V, Kammerer PW, Wriedt S, Al Nawas B. 3D analysis of condylar position after sagittal split osteotomy of the mandible in mono- and bimaxillary orthognathic surgery - a methodology study in 18 patients. J Orofac Orthop. 2010;71:421–9. doi: 10.1007/s00056-010-1021-9. [DOI] [PubMed] [Google Scholar]
- 11.Kim YJ, Oh KM, Hong JS, Lee JH, Kim HM, Reyes M, et al. Do patients treated with bimaxillary surgery have more stable condylar positions than those who have undergone single-jaw surgery? J Oral Maxillofac Surg. 2012;70:2143–52. doi: 10.1016/j.joms.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 12.Park SB, Yang YM, Kim YI, Cho BH, Jung YH, Hwang DS. Effect of bimaxillary surgery on adaptive condylar head remodeling: metric analysis and image interpretation using cone-beam computed tomography volume superimposition. J Oral Maxillofac Surg. 2012;70:1951–9. doi: 10.1016/j.joms.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 13.de Carvalho FA, Cevidanes LH, da Motta AT, Almeida MA, Phillips C. Three-dimensional assessment of mandibular advancement 1 year after surgery. Am J Orthod Dentofacial Orthop. 2010;137:S53e1–12. doi: 10.1016/j.ajodo.2010.01.017. discussion S53–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Paula LK, Ruellas AC, Paniagua B, Styner M, Turvey T, Zhu H, et al. One-year assessment of surgical outcomes in Class III patients using cone beam computed tomography. Int J Oral Maxillofac Surg. 2013;42:780–9. doi: 10.1016/j.ijom.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Proffit WR, Phillips C, Prewitt JW, Turvey TA. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. 2. Maxillary advancement. Int J Adult Orthod Orthognath Surg. 1991;6:71–80. [PubMed] [Google Scholar]
- 16.Proffit WR, Phillips C, Turvey TA. Stability after surgical-orthodontic corrective of skeletal Class III malocclusion. 3. Combined maxillary and mandibular procedures. Int J Adult Orthod Orthognath Surg. 1991;6:211–25. [PubMed] [Google Scholar]
- 17.Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31:1116–28. doi: 10.1016/j.neuroimage.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Styner M, Oguz I, Xu S, Brechbuhler C, Pantazis D, Levitt JJ, et al. Framework for the Statistical Shape Analysis of Brain Structures using SPHARM-PDM. Insight J. 2006:242–50. [PMC free article] [PubMed] [Google Scholar]
- 19.Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:110–7. doi: 10.1016/j.tripleo.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen T, Cevidanes L, Paniagua B, Zhu H, Koerich L, De Clerck H. Use of shape correspondence analysis to quantify skeletal changes associated with bone-anchored Class III correction. Angle Orthod. 2014;84:329–36. doi: 10.2319/041513-288.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paniagua B, Cevidanes L, Walker D, Zhu H, Guo R, Styner M. Clinical application of SPHARM-PDM to quantify temporomandibular joint osteoarthritis. Comput Med Imaging Graph. 2011;35:345–52. doi: 10.1016/j.compmedimag.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayoub AF, Millett DT, Hasan S. Evaluation of skeletal stability following surgical correction of mandibular prognathism. Br J Oral Maxillofac Surg. 2000;38:305–11. doi: 10.1054/bjom.2000.0303. [DOI] [PubMed] [Google Scholar]
- 23.Politi M, Costa F, Cian R, Polini F, Robiony M. Stability of skeletal class III malocclusion after combined maxillary and mandibular procedures: rigid internal fixation versus wire osteosynthesis of the mandible. J Oral Maxillofac Surg. 2004;62:169–81. doi: 10.1016/j.joms.2003.04.010. [DOI] [PubMed] [Google Scholar]
- 24.Franco JE, Van Sickels JE, Thrash WJ. Factors contributing to relapse in rigidly fixed mandibular setbacks. J Oral Maxillofac Surg. 1989;47:451–6. doi: 10.1016/0278-2391(89)90276-0. [DOI] [PubMed] [Google Scholar]
- 25.Wolford LM. The sagittal split ramus osteotomy as the preferred treatment for mandibular prognathism. J Oral Maxillofac Surg. 2000;58:310–2. doi: 10.1016/s0278-2391(00)90062-4. [DOI] [PubMed] [Google Scholar]
- 26.Ghang MH, Kim HM, You JY, Kim BH, Choi JP, Kim SH, et al. Three-dimensional mandibular change after sagittal split ramus osteotomy with a semirigid sliding plate system for fixation of a mandibular setback surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 doi: 10.1016/j.oooo.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 27.Mavili ME, Canter HI, Saglam-Aydinatay B. Semirigid fixation of mandible and maxilla in orthognathic surgery: stability and advantages. Ann Plast Surg. 2009;63:396–403. doi: 10.1097/SAP.0b013e318190322f. [DOI] [PubMed] [Google Scholar]