Abstract
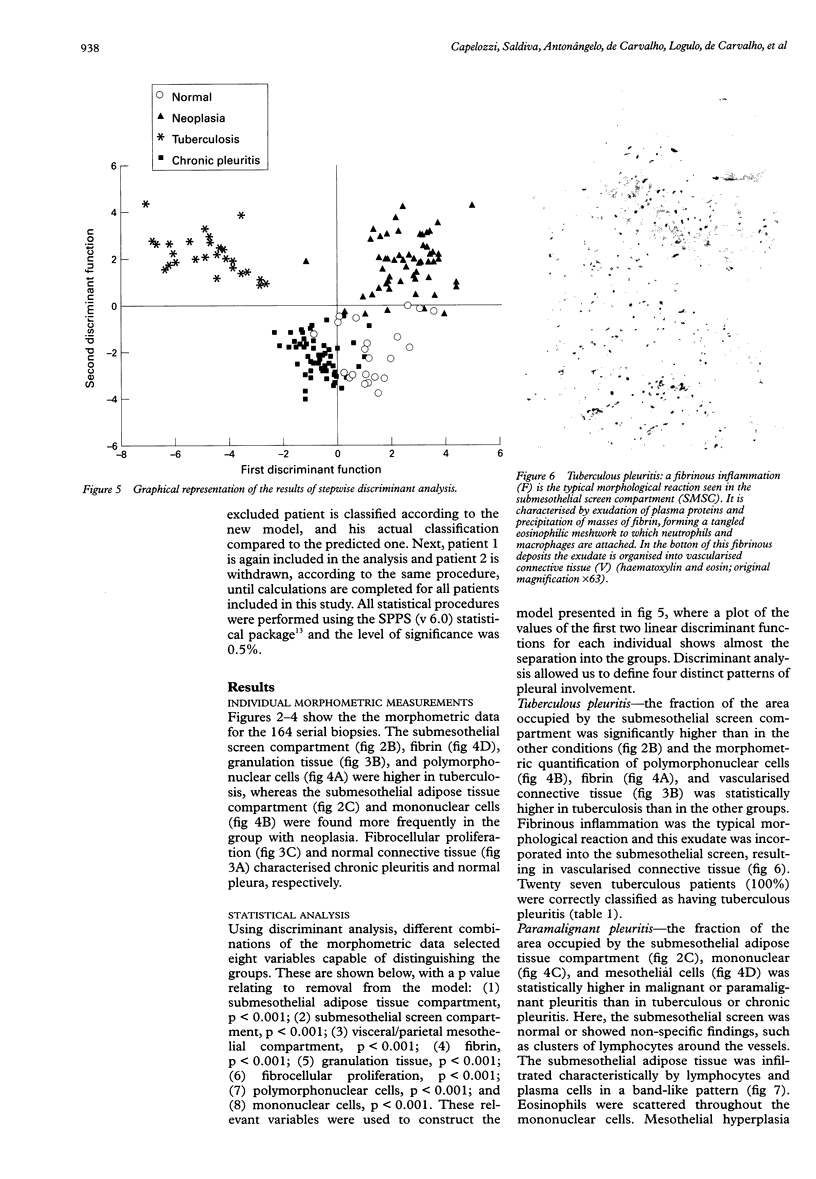
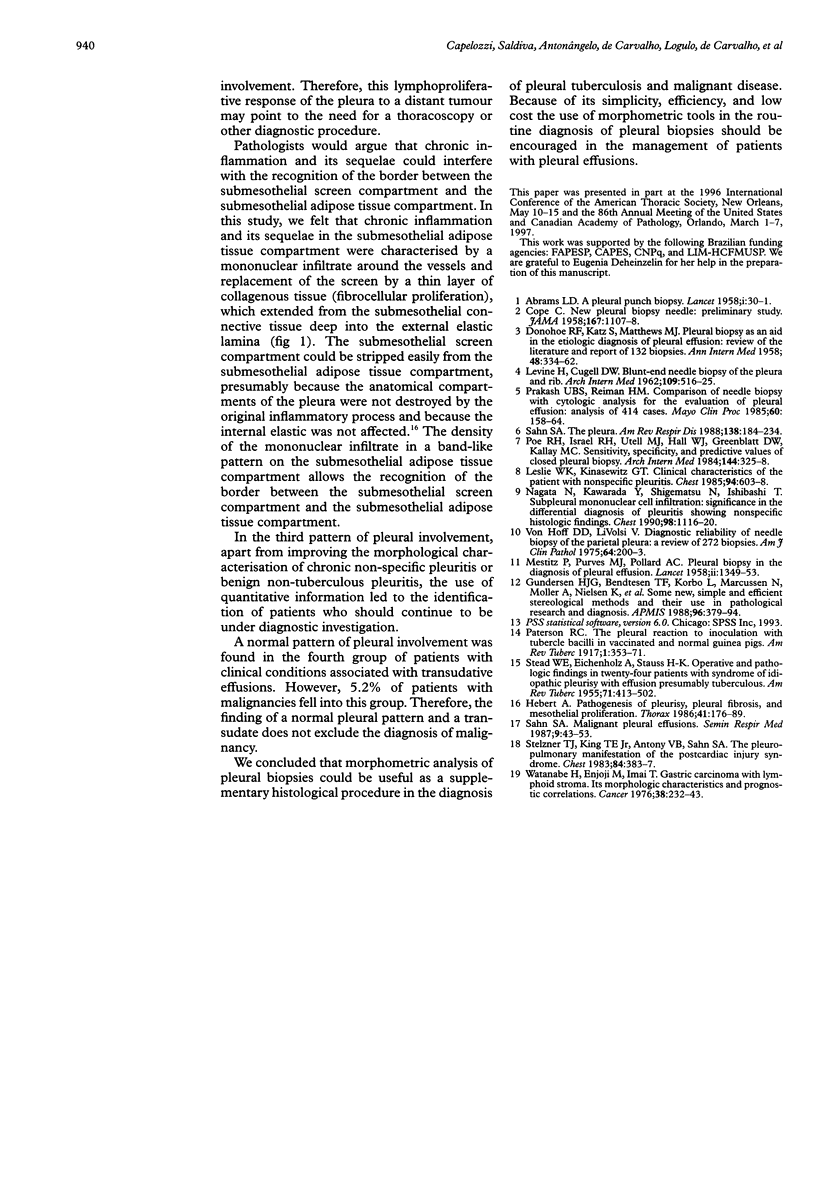
AIM: To determine by morphometry if pleural biopsies with the histopathological diagnosis of "non-specific pleuritis", malignant, and tuberculous disease could be distinguished morphologically from those with truly non-specific disease. METHODS: Each pleural biopsy was reviewed taking into account three compartments of reference: the visceral/parietal mesothelial compartment, the submesothelial screen compartment, and the submesothelial adipose tissue compartment. Normal connective tissue, granulation tissue, fibrocellular proliferation, fibrin, polymorphonuclear cells, mononuclear cells, and mesothelial cells were measured using conventional point counting procedures in terms of the fractional area occupied by each parameter within each compartment of reference. Ranking was carried out on 164 patients, based on their diagnosis: chronic non-specific disease (n = 57), tuberculosis (n = 27), malignant disease (n = 58), and conditions associated with transudative effusions (n = 22). RESULTS: Stepwise discriminant analysis of the resulting data showed that biopsies from patients with tuberculosis, malignant disease, and chronic non-specific disease could be distinguished between themselves and normal cases. Statistical differences among the four groups were observed for eight morphometric parameters related to components of inflammation and extension throughout the three pleural anatomical compartments. A robust discriminant function permitted an adequate classification of the three groups of disease in 88.41% of the cases. Pleural biopsies with fibrin incorporated within granulation tissue on the submesothelial screen compartment showed 100% specificity for patients with tuberculosis, while mononuclear cells in a band-like infiltrate on the submesothelial adipose tissue compartment showed 93.1% specificity for patients with malignant disease. The truly non-specific pleuritis was characterised by deposits of fibrin in the subpleural compartment and discrete signs of chronic inflammation and reparatory fibrosis on the submesothelial screen. CONCLUSIONS: Morphometric analysis of pleural biopsies may be a useful supplementary histological procedure to support the diagnosis of pleural tuberculosis and malignant disease.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ABRAMS L. D. A pleural-biopsy punch. Lancet. 1958 Jan 4;1(7010):30–31. doi: 10.1016/s0140-6736(58)92521-2. [DOI] [PubMed] [Google Scholar]
- COPE C. New pleural biopsy needle; preliminary study. J Am Med Assoc. 1958 Jun 28;167(9):1107–1108. doi: 10.1001/jama.1958.72990260005011a. [DOI] [PubMed] [Google Scholar]
- Gundersen H. J., Bendtsen T. F., Korbo L., Marcussen N., Møller A., Nielsen K., Nyengaard J. R., Pakkenberg B., Sørensen F. B., Vesterby A. Some new, simple and efficient stereological methods and their use in pathological research and diagnosis. APMIS. 1988 May;96(5):379–394. doi: 10.1111/j.1699-0463.1988.tb05320.x. [DOI] [PubMed] [Google Scholar]
- Herbert A. Pathogenesis of pleurisy, pleural fibrosis, and mesothelial proliferation. Thorax. 1986 Mar;41(3):176–189. doi: 10.1136/thx.41.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LEVINE H., CUGELL D. W. Blunt-end needle biopsy of pleura and rib. Arch Intern Med. 1962 May;109:516–525. doi: 10.1001/archinte.1962.03620170014003. [DOI] [PubMed] [Google Scholar]
- Leslie W. K., Kinasewitz G. T. Clinical characteristics of the patient with nonspecific pleuritis. Chest. 1988 Sep;94(3):603–608. doi: 10.1378/chest.94.3.603. [DOI] [PubMed] [Google Scholar]
- MESTITZ P., PURVES M. J., POLLARD A. C. Pleural biopsy in the diagnosis of pleural effusion; a report of 200 cases. Lancet. 1958 Dec 27;2(7061):1349–1353. doi: 10.1016/s0140-6736(58)91439-9. [DOI] [PubMed] [Google Scholar]
- Nagata N., Kawarada Y., Shigematsu N., Ishibashi T. Subpleural mononuclear cell infiltration. Significance in the differential diagnosis of pleuritis showing nonspecific histologic findings. Chest. 1990 Nov;98(5):1116–1120. doi: 10.1378/chest.98.5.1116. [DOI] [PubMed] [Google Scholar]
- Poe R. H., Israel R. H., Utell M. J., Hall W. J., Greenblatt D. W., Kallay M. C. Sensitivity, specificity, and predictive values of closed pleural biopsy. Arch Intern Med. 1984 Feb;144(2):325–328. [PubMed] [Google Scholar]
- Prakash U. B., Reiman H. M. Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusion: analysis of 414 cases. Mayo Clin Proc. 1985 Mar;60(3):158–164. doi: 10.1016/s0025-6196(12)60212-2. [DOI] [PubMed] [Google Scholar]
- STEAD W. W., EICHENHOLZ A., STAUSS H. K. Operative and pathologic findings in twenty-four patients with syndrome of idiopathic pleurisy with effusion, presumably tuberculous. Am Rev Tuberc. 1955 Apr;71(4):473–502. doi: 10.1164/artpd.1955.71.4.473. [DOI] [PubMed] [Google Scholar]
- Sahn S. A. State of the art. The pleura. Am Rev Respir Dis. 1988 Jul;138(1):184–234. doi: 10.1164/ajrccm/138.1.184. [DOI] [PubMed] [Google Scholar]
- Stelzner T. J., King T. E., Jr, Antony V. B., Sahn S. A. The pleuropulmonary manifestations of the postcardiac injury syndrome. Chest. 1983 Oct;84(4):383–387. doi: 10.1378/chest.84.4.383. [DOI] [PubMed] [Google Scholar]
- Von Hoff D. D., LiVolsi V. Diagnostic reliability of needle biopsy of the parietal pleura. A review of 272 biopsies. Am J Clin Pathol. 1975 Aug;64(2):200–203. doi: 10.1093/ajcp/64.2.200. [DOI] [PubMed] [Google Scholar]
- Watanabe H., Enjoji M., Imai T. Gastric carcinoma with lymphoid stroma. Its morphologic characteristics and prognostic correlations. Cancer. 1976 Jul;38(1):232–243. doi: 10.1002/1097-0142(197607)38:1<232::aid-cncr2820380135>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]