Abstract
Rationale: Survivors of critical illness experience significant morbidity, but the impact of surviving the intensive care unit (ICU) has not been quantified comprehensively at a population level.
Objectives: To identify factors associated with increased hospital resource use and to ascertain whether ICU admission was associated with increased mortality and resource use.
Methods: Matched cohort study and pre/post-analysis using national linked data registries with complete population coverage. The population consisted of patients admitted to all adult general ICUs during 2005 and surviving to hospital discharge, identified from the Scottish Intensive Care Society Audit Group registry, matched (1:1) with similar hospital control subjects. Five-year outcomes included mortality and hospital resource use. Confounder adjustment was based on multivariable regression and pre/post within-individual analyses.
Measurements and Main Results: Of 7,656 ICU patients, 5,259 survived to hospital discharge (5,215 [99.2%] matched to hospital control subjects). Factors present before ICU admission (comorbidities/pre-ICU hospitalizations) were stronger predictors of hospital resource use than acute illness factors. In the 5 years after the initial hospital discharge, compared with hospital control subjects, the ICU cohort had higher mortality (32.3% vs. 22.7%; hazard ratio, 1.33; 95% confidence interval, 1.22–1.46; P < 0.001), used more hospital resources (mean hospital admission rate, 4.8 vs. 3.3/person/5 yr), and had 51% higher mean 5-year hospital costs ($25,608 vs. $16,913/patient). Increased resource use persisted after confounder adjustment (P < 0.001) and using pre/post-analyses (P < 0.001). Excess resource use and mortality were greatest for younger patients without significant comorbidity.
Conclusions: This complete, national study demonstrates that ICU survivorship is associated with higher 5-year mortality and hospital resource use than hospital control subjects, representing a substantial burden on individuals, caregivers, and society.
Keywords: intensive care, mortality, hospital readmission, hospital costs, registries
At a Glance Commentary
Scientific Knowledge on the Subject
There are increasing numbers of patients surviving an episode of critical illness. Cohort studies indicate that intensive care survivors may have ongoing complex and potentially costly health care needs. However, robust population-level estimates of the excess mortality and health care costs associated with surviving intensive care are needed.
What This Study Adds to the Field
We have demonstrated an increased risk of death (33%) and hospital readmission rate (22%) in patients surviving an episode of intensive care compared with hospital control subjects in the 5 years after discharge from hospital, after adjusting for important confounders. Our population-level estimates indicate substantial costs associated with intensive care unit survivorship, which can be used to inform health policy.
Survivors of critical illness suffer significant morbidity (1), including neuromuscular complications (2), respiratory impairment (3), cognitive decline (4), psychological morbidity (5), and physical disability (3). Patients report low quality of life, especially in physical domains (6, 7).
The decline in physical, psychological, and/or cognitive function after critical illness has been termed the “post–intensive care syndrome” (8). The prevalence and severity of various morbidities have been described in cohort studies, but these provide limited information about the health care burden of the post–intensive care syndrome because of selection bias, loss to follow-up, and limited health care resource use data (9). Furthermore, the magnitude of the health care burden and duration over which it remains elevated is poorly understood (10). Linkage of national health care registries provides a more complete, national picture of longer-term outcomes for intensive care unit (ICU) survivors. Comparing ICU survivors with matched hospital or general population cohorts also provides a method by which to explore the magnitude of excess mortality and health care resources associated with ICU survivorship and to identify patients at greatest risk.
We hypothesized that indirect evidence of the clinical and financial burden of post–intensive care syndrome could be demonstrated through identifying higher longer-term mortality and hospital resource use in ICU survivors compared with control populations in the years after ICU admission. We aimed to (1) compare longer-term mortality for a national cohort of ICU survivors over a 5-year period after hospital discharge with mortality rates for a cohort of hospital control subjects (hospitalized patients not receiving intensive care) and the general population; (2) identify factors associated with increased postdischarge hospital resource use; (3) compare longer-term hospital resource use for the ICU cohort with that for hospital control subjects; and (4) compare hospital resource use in the years after an ICU admission with baseline hospital resource use within individuals. Some provisional results of these studies have been previously reported in the form of abstracts (11–13).
Methods
Study Population, Setting, and Databases
We used cohort study designs (matched and pre/post within-individual analyses). Primary data sources were routinely collected, administrative, linked registries derived from the Scottish Intensive Care Society Audit Group (SICSAG), Scottish Morbidity Record of acute hospital admissions (SMR01), and Scottish death records. The SICSAG registry captures all adult general intensive care activity within Scotland. In 2005 all 24 adult general ICUs, serving a population of 5.1 million (4.2 million aged ≥16 yr), submitted data (14). The ICU cohort comprised residents, at least 16 years of age, admitted to general ICUs in Scotland between January 1, 2005 and December 31, 2005, who survived to hospital discharge (index admission). All ICU patients were eligible regardless of length of ICU stay. For multiple admissions, only first ICU admissions with a valid linkage number were included. The matched hospital cohort was extracted from the SMR01 registry, using identical inclusion and exclusion criteria, but excluded hospital admissions with ICU episodes. Matching was undertaken 1:1, using age (in 10-yr age bands), sex, admission type (emergency surgical, elective surgical, emergency medical), and date of hospital discharge (quarter of year). Approvals were obtained from the relevant data-governing bodies (Privacy Advisory Committee, NHS Scotland Information Services Division; ref 55/09). All data were anonymized before release to the researchers. The South East Scotland Research Ethics Committee granted a waiver (ref NR/1001AB14). The online supplement provides further details regarding the registries.
Outcomes and Follow-up Period
The primary outcomes were mortality and hospital resource use. Mortality for ICU and hospital cohorts was derived from linkage to Scottish death records. General population mortality rates were obtained by indirect standardization using the general Scottish population as a reference population (15). Age- and sex-specific mortality rates were derived from national Scottish mortality data and applied to the ICU cohort population structure to produce expected mortality. Hospital resources comprised elective (scheduled) day-case, elective (scheduled) inpatient, or emergency (unscheduled) inpatient acute hospital admissions and were quantified in four ways: total number of hospital admissions; total number of days spent in hospital; total costs of hospital care; and cumulative incidence of first admission (in sensitivity analyses). Costs of hospital care included only day-case and inpatient admissions. Per diem costs for hospital care were derived from the NHS Scottish Costs Book (16) and converted to 2014 costs, using purchasing power parities. Measures of hospital resource use were calculated per person over the 5-year follow-up period (see the online supplement). Follow-up commenced from the day of index hospital discharge and ended at 5 years (with censoring on December 31, 2010 at study end). As censoring was negligible and emigration in older age groups from Scotland to the remainder of the United Kingdom or overseas is known to be low (17), follow-up was assumed to be complete for analyses (missing person-time < 0.2% for all cohorts).
Statistical Analysis
All analyses were undertaken with Stata/IC version 13 (StataCorp LP, College Station, TX). For more information, see the online supplement.
Mortality (ICU cohort vs. hospital control vs. general population)
We used Kaplan-Meier survival plots to compare the ICU cohort, hospital cohort, and expected age/sex indirectly standardized survival curves derived from the general Scottish population mortality rates. Cox regression stratified by matched pairs was used to estimate the hazard ratio (HR) for mortality in ICU versus hospital control subjects adjusted for potential confounders. In addition to matched variables, we adjusted for the following: age, quintile of an area-based measure of socioeconomic status (Social Index of Multiple Deprivation) (18), remoteness (19), rurality (19), health region, preindex hospitalization health care resource use (number of hospital admissions in the prior 5 yr), and number of comorbidities from the Charlson Index (reconstructed from diagnostic codes on admission records in prior 1 yr) (20). Measures of illness severity were not included as these were not available for the hospital control subjects. For more information see the online supplement.
Predictors of resource use (ICU cohort only)
Independent predictors of number of hospital admissions over 5 years were identified for the whole ICU cohort, using a negative binomial multivariable regression model (see the online supplement). This analysis was limited to individuals in the ICU cohort. Coefficients produced from this regression model—once exponentiated—can be interpreted as an admission rate ratio. This is because it represents the ratio of admission rates in one group compared with the reference group. Variables were grouped into demographic factors, prior illness/resource use factors, and index admission factors. We specifically assessed the association of several acute illness factors with resource use in additional analyses due to collinearity: Simplified Acute Physiology Score II (SAPS II) on ICU admission, organ support (provision of mechanical ventilation, renal replacement therapy, or cardiovascular support), total number of organs supported, ICU length of stay (LOS), post-ICU hospital LOS, and total hospital LOS (see the online supplement).
Resource use (ICU cohort vs. hospital control subjects)
The first approach to explore potential excess resource use on a relative scale associated with ICU admission was a comparison of matched ICU and hospital control subjects. We estimated admission rate ratios using negative binomial regression to model the number of hospital admissions during the 5-year follow-up period, allowing for the matched nature of the data by using standard errors that accommodated clustering (correlation between matched pairs) (21). Potential confounders were included in the multivariable model as for mortality analyses. We explored effect modification by reporting stratum-specific admission rate ratios and including interaction terms in regression models for the following variables: age (dichotomized <70, ≥70 yr) and presence of any Charlson comorbidity (dichotomized 0, ≥1).
Resource use (pre/post within-individual; ICU cohort only)
The second approach to explore potential excess resource use associated with ICU admission was a pre/post comparison within individuals on an absolute scale. This analysis was limited to individuals in the ICU cohort. We calculated excess postdischarge hospital costs by subtracting baseline hospital costs (those that would have accrued had the patient not been admitted to ICU) from postdischarge hospital costs during the time spent alive and under follow-up. Baseline hospital costs were derived from hospital admissions during the period before index hospital admission, varying this period from 1 to 5 years preindex admission for each patient (see the online supplement). No adjustment for confounders was undertaken as confounding was controlled by comparisons within individuals. However, we modeled the uncertainty of the effect of increasing age during follow-up on hospital costs and the uncertainty of baseline costs by varying these two factors under six scenarios in additional analyses (see the online supplement).
Sensitivity Analyses
Resource use
For analyses to identify predictors of resource use and comparing resource use in the ICU cohort and hospital control subjects, we performed a sensitivity analysis using Fine–Gray competing risks (22). This allows for the competing risk of death by modeling an estimate of cumulative incidence of first hospital admission with early deaths remaining in the denominator. Exponentiated regression coefficients can be interpreted as subdistribution HRs (23). This sensitivity analysis was important because in both negative binomial external-controlled and pre/post within-individual analytical approaches described previously, people who die do not subsequently accrue costs. Patient groups with high, early mortality, therefore, would be less likely to accrue substantial health care resource use over the 5-year follow-up period. However, this sensitivity analysis using competing risks regression differs from the other two approaches as the outcome being modeled is cumulative incidence of first hospital admission whereas the other approaches model the total number of admissions or total hospital costs during the follow-up period.
Results
Baseline Characteristics
In 2005, 5,259 of 7,656 patients survived to hospital discharge after an index ICU admission (see Figure E1 in the online supplement); 5,215 (99.2%) were successfully matched to hospital control subjects (Table E1). ICU patient cohort characteristics are shown in Table E1. The median age was 60 years (interquartile range [IQR], 44–72), 61% were mechanically ventilated, 73% had one or more hospital admission during the prior 5 years, and 27% had one or more preexisting Charlson comorbidities. Median ICU LOS was 2 days (IQR, 1–5; mean, 5) and median hospital LOS was 17 (IQR, 9–39; mean, 34). Compared with matched hospital control subjects, the ICU cohort subjects were more likely to live in areas of socioeconomic deprivation (P = 0.001), had more comorbidities (P < 0.001), and had greater numbers of previous hospital admissions (P < 0.001) (Table 1).
Table 1.
Baseline Characteristics of Intensive Care Unit Cohort Compared with Hospital Control Cohort
| ICU Cohort (n = 5,215) | Hospital Control Cohort (n = 5,215) | P Value | |
|---|---|---|---|
| Age, yr, median (IQR) | 60 (44–72) | 60 (44–72) | — |
| Female, n (%) | 2,327 (44.6) | 2,327 (44.6) | — |
| Scottish Index of Multiple Deprivation quintile, n (%) | 0.001 | ||
| 1 (least deprived) | 653 (12.5) | 781 (15.0) | |
| 2 | 848 (16.3) | 906 (17.4) | |
| 3 | 1,065 (20.4) | 1,012 (19.4) | |
| 4 | 1,233 (23.6) | 1,179 (22.6) | |
| 5 (most deprived) | 1,416 (27.2) | 1,337 (25.6) | |
| Resident in remote area, n (%) | 471 (9.0) | 542 (10.4) | 0.02 |
| Resident in rural area, n (%) | 916 (17.6) | 905 (17.4) | 0.77 |
| Count of Charlson comorbidities, n (%) | <0.001 | ||
| 0 | 3,799 (72.9) | 4,748 (91.1) | |
| 1 | 1,012 (19.4) | 357 (6.9) | |
| 2 or more | 404 (7.8) | 110 (2.1) | |
| Hospital admissions in previous 5 yr, n (%) | <0.001 | ||
| 0 | 1,403 (26.9) | 2,021 (38.8) | |
| 1 | 962 (18.5) | 1,092 (20.9) | |
| 2 | 709 (13.6) | 692 (40.3) | |
| 3 | 510 (9.8) | 399 (7.7) | |
| 4 | 347 (6.7) | 292 (5.6) | |
| 5 or more | 1,284 (24.7) | 719 (13.8) | |
| Admission type, n (%) | — | ||
| Elective operation | 1,146 (22.0) | 1,146 (22.0) | |
| Emergency operation | 1,447 (27.8) | 1,447 (27.8) | |
| Medical | 2,622 (50.3) | 2,622 (50.3) | |
| Index hospitalization length of stay, d | <0.001 | ||
| Mean (SD) | 32.5 (43.8) | 11.4 (32.8) | |
| Median (IQR) | 17 (9–38) | 3 (1–8) |
Definition of abbreviations: ICU = intensive care unit; IQR = interquartile range.
Hypothesis tests were not undertaken on variables used in matching. Note that data are presented for matched cohort n = 5,215; these values differ from full ICU cohort (n = 5,259) as 44 individuals were not matched. See Table E1 in the online supplement for more detailed characteristics of the full, matched, and unmatched ICU cohort.
Mortality
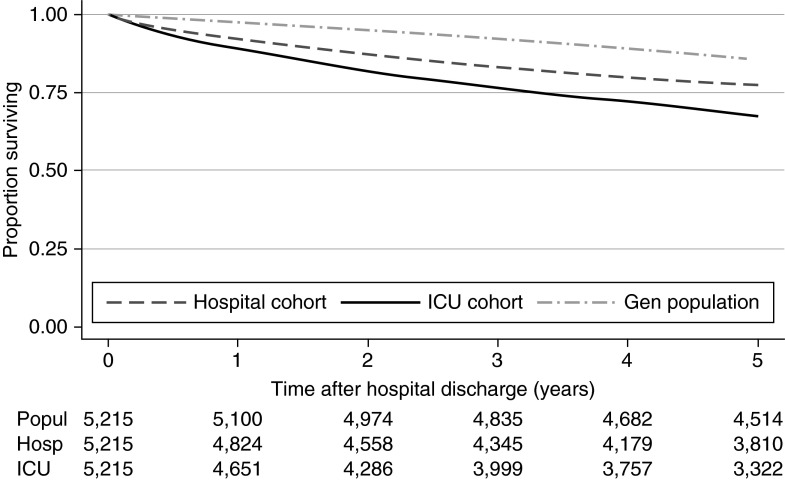
Mortality for the ICU cohort at 1 year was 10.9% (95% confidence interval [CI], 10.0–11.7) and at 5 years was 32.3% (95% CI, 31.0–33.6) (Figure 1). Mortality in the ICU cohort was higher than for matched hospital control subjects (1 yr, 7.5%; 5 yr, 22.7%) and for an age- and sex-standardized general population (1 yr, 2.2%; 5 yr, 13.4%). After adjustment, the relative risk of death for the ICU cohort was 33% higher, during the 5-year follow-up period, than for hospital control subjects (unadjusted HR, 1.56; 95% CI, 1.41–1.67; adjusted HR, 1.33; 95% CI, 1.22–1.46; P < 0.001). On stratification by age, relative mortality was substantially higher in those less than 70 years of age (HR, 1.68; 95% CI, 1.47–1.92; P < 0.001) but was similar for survivors at least 70 years old compared with hospital control subjects (HR, 1.05; 95% CI, 0.92–1.19; P = 0.45; interaction term, P < 0.001). Comorbidity was not found to be a statistically significant effect modifier (interaction term, P = 0.09).
Figure 1.
Kaplan-Meier plot of 5-year survival after hospital discharge for the intensive care unit (ICU) survivor cohort, hospital cohort, and general population of Scotland. General population mortality rates were derived using age–sex indirect standardization. Gen = general; Popul = general population at risk of event; Hosp = hospital control cohort at risk of event; ICU = ICU cohort at risk of event.
Resource Use
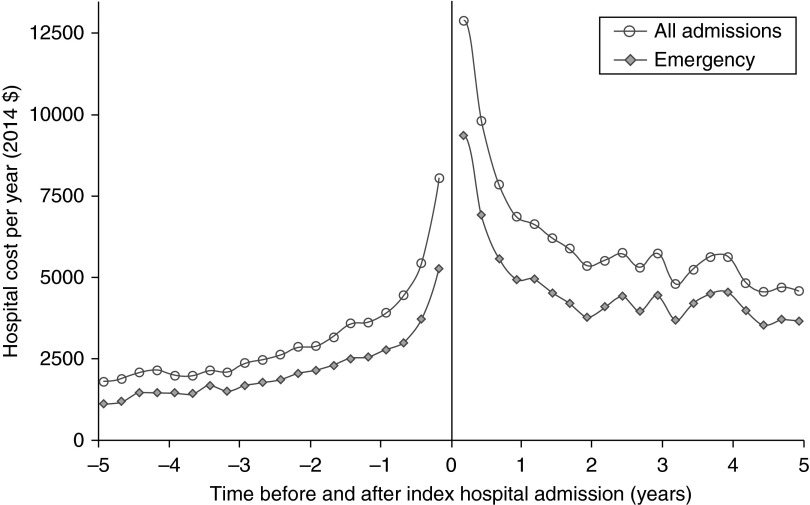
Over the 5-year follow-up period, 81.7% of the ICU cohort had one or more hospital admissions, with a mean 4.8 hospital admissions per patient (accounting for 173,113 d in hospital; mean, 32.9 hospital days per patient; accounting for 2.2% of days alive) (Table E2). Total costs were $136.1 million, equivalent to $25,881 per person in the ICU cohort over the 5-year follow-up period. Emergency admissions to hospital comprised 54% of all hospital admissions, accounting for 77% of hospital days and 75% of hospital admission costs (Figure 2).
Figure 2.
Hospital costs for all admission types and emergency admissions before and after index hospital admission for the intensive care unit survivor cohort (n = 5,259). Each point represents the mean cost in 2014 US$ for each quarter (reported as cost per year) for each patient alive at the start of each quarter.
Within the ICU cohort, factors associated with the number of hospital admissions over the 5-year follow-up period are presented in Table E3a. Comparing factors grouped into three categories (demographics, prior illness/resource use, and index admission factors), the strongest predictors (based on Wald χ2 statistic) were prior illness/resource use factors (χ2 = 420.6, 4 degrees of freedom [df]; P < 0.001), followed by index admission factors (χ2 = 140.1, 34 df; P < 0.001), and demographic factors (χ2 = 41.1, 10 df; P < 0.001). ICU admission diagnoses in the ICU cohort associated with hospital admission are shown in Table E3b; esophageal variceal bleeding was associated with the highest admission rate ratio (ARR). Competing risk of death analysis yielded similar results for most covariates (Table E3a and E3b). Where differences existed (e.g., age), these largely reflected differences in mortality (oldest vs. youngest, 52% vs. 12%) and therefore a shorter follow-up time to experience readmissions. This led to a lower ARR produced by the negative binomial analysis, which did not substantially affect competing risks analyses. Most markers of ICU acute severity of illness and index hospitalization were either weakly or not associated with 5-year hospital admission rate or cumulative incidence of first admission (Table E4). The strongest association was with hospital LOS.
Resource Use: ICU Cohort versus Hospital Control Subjects
During the 5-year follow-up period, the mean time under follow-up while alive was 4.02 years/person in the ICU cohort compared with 4.30 years/person in hospital control subjects. Compared with control subjects, the ICU cohort subjects were more likely to have one or more hospital admissions (81.6% vs. 73.3%), used more hospital resources (admission rate, 4.8 vs. 3.3 per person/5 years; ARR, 1.47; 95% CI, 1.38–1.57; P < 0.001), had a higher number of mean days in hospital (32.6 vs. 21.5; 2.2% vs. 1.4% of days alive), and had 51% higher mean costs of hospital admissions ($25,608 vs. $16,912 per patient; $133.5 million vs. $88.2 million for the whole cohort) (Table 2). The majority of costs for both cohorts was attributable to emergency hospital admissions (ICU cohort: mean, $19,078; 74.5% of total costs; hospital control subjects: $12,239; 72.4% of total costs).
Table 2.
Mean Resource Use per Year for Intensive Care Unit Cohort and Hospital Control Cohort
| No. Alive at Start of Interval | Mean Hospital Resource Use during Interval |
Mean Hospital Cost Accrued during Interval ($) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Emergency | Elective | Day Case | Total (95% CI) | Emergency | Elective | Day Case | Total (95% CI) | ||
| ICU cohort | |||||||||
| 0–1 yr | 5,215 | 6,317 | 1,880 | 666 | 8,863 (8,332–9,393) | ||||
| No. of admissions | 0.83 | 0.31 | 0.52 | 1.66 (1.57–1.75) | |||||
| Length of stay, d | 8.3 | 2.5 | 0.5 | 11.2 (10.6–11.9) | |||||
| 1–2 yr | 4,651 | 4,116 | 1,175 | 412 | 5,704 (5,269–6,138) | ||||
| No. of admissions | 0.60 | 0.20 | 0.32 | 1.11 (1.04–1.18) | |||||
| Length of stay, d | 5.4 | 1.5 | 0.3 | 7.2 (6.7–7.8) | |||||
| 2–3 yr | 4,286 | 4,104 | 973 | 342 | 5,421 (4,949–5,892) | ||||
| No. of admissions | 0.57 | 0.16 | 0.27 | 1.00 (0.93–1.07) | |||||
| Length of stay, d | 5.4 | 1.3 | 0.3 | 6.9 (6.3–7.5) | |||||
| 3–4 yr | 3,999 | 4,078 | 726 | 340 | 5,146 (4,639–5,652) | ||||
| No. of admissions | 0.53 | 0.14 | 0.26 | 0.93 (0.86–1.00) | |||||
| Length of stay, d | 5.3 | 1.0 | 0.3 | 6.6 (5.9–7.2) | |||||
| 4–5 yr | 3,757 | 3,593 | 628 | 300 | 4,521 (4,061–4,982) | ||||
| No. of admissions | 0.48 | 0.12 | 0.23 | 0.84 (0.78–0.90) | |||||
| Length of stay, d | 4.7 | 0.8 | 0.2 | 5.8 (5.2–6.4) | |||||
| 0–5 yr | 5,215 | 19,077 | 4,738 | 1,793 | 25,608 (24,360–26,856) | ||||
| No. of admissions | 2.58 | 0.82 | 1.39 | 4.79 (4.57–5.02) | |||||
| Length of stay, d | 25.0 | 6.2 | 1.4 | 32.6 (30.9–34.2) | |||||
| Hospital control cohort | |||||||||
| 0–1 yr | 5,215 | 3,662 | 1,351 | 381 | 5,392 (4,969–5,815) | ||||
| No. of admissions | 0.50 | 0.26 | 0.30 | 1.05 (0.99–1.11) | |||||
| Length of stay, d | 4.8 | 1.8 | 0.3 | 6.9 (6.3–7.4) | |||||
| 1–2 yr | 4,824 | 2,936 | 698 | 272 | 3,906 (3,534–4,279) | ||||
| No. of admissions | 0.37 | 0.15 | 0.21 | 0.73 (0.68–0.78) | |||||
| Length of stay, d | 3.8 | 0.9 | 0.2 | 5.0 (4.5–5.5) | |||||
| 2–3 yr | 4,558 | 2,608 | 629 | 235 | 3,473 (3,098–3,848) | ||||
| No. of admissions | 0.33 | 0.13 | 0.18 | 0.65 (0.60–0.69) | |||||
| Length of stay, d | 3.4 | 0.8 | 0.2 | 4.4 (3.9–4.9) | |||||
| 3–4 yr | 4,345 | 2,268 | 583 | 255 | 3,105 (2,759–3,450) | ||||
| No. of admissions | 0.31 | 0.11 | 0.20 | 0.62 (0.57–0.67) | |||||
| Length of stay, d | 3.0 | 0.8 | 0.2 | 3.9 (3.5–4.4) | |||||
| 4–5 yr | 4,179 | 2,111 | 516 | 221 | 2,850 (2,517–3,183) | ||||
| No. of admissions | 0.30 | 0.10 | 0.17 | 0.57 (0.53–0.61) | |||||
| Length of stay, d | 2.8 | 0.7 | 0.2 | 3.6 (3.2–4.0) | |||||
| 0–5 yr | 5,215 | 12,240 | 3,445 | 1,227 | 16,912 (15,955–17,869) | ||||
| No. of admissions | 1.63 | 0.68 | 0.95 | 3.26 (3.12–3.41) | |||||
| Length of stay, d | 16.0 | 4.5 | 1.0 | 21.5 (20.2–22.7) | |||||
Definition of abbreviations: CI = confidence interval; ICU = intensive care unit.
Mean number of admissions, mean hospital length of stay, and mean cost are calculated per patient alive and under follow-up at the start of each interval. The 95% CIs are shown only for total columns for clarity of presentation. Resource use is presented for matched cohorts (n = 5,215 per cohort); for resource use quantities for full ICU cohort (n = 5,259) see Table E2 in the online supplement.
After adjusting for potential confounders, the relative rate of hospital admission in the 5-year period remained significantly higher for the ICU cohort (ARR, 1.22; 95% CI, 1.15–1.30; P < 0.001). Allowing for competing risk of death by modeling cumulative incidence of first hospital admission, the ICU cohort had a 19% increased risk of hospital admission compared with hospital control subjects (subdistribution HR, 1.19; 95% CI, 1.13–1.24; P < 0.001).
To account in part for differences in mortality rates between ICU and hospital cohorts, a comparison of annual hospital resources used per patient alive at the start of each year was undertaken. This demonstrated a reduction in hospital resource use for each year of follow-up in both cohorts, but this remained higher in the ICU cohort throughout (Table 2). After adjusting for confounding, the ICU cohort had higher hospital admission rates for each year of follow-up, which persisted in the fifth year of follow-up (Year 1: ARR, 1.30; 95% CI, 1.20–1.41; P < 0.001; Year 5: ARR, 1.19; 95% CI, 1.07–1.32; P = 0.002).
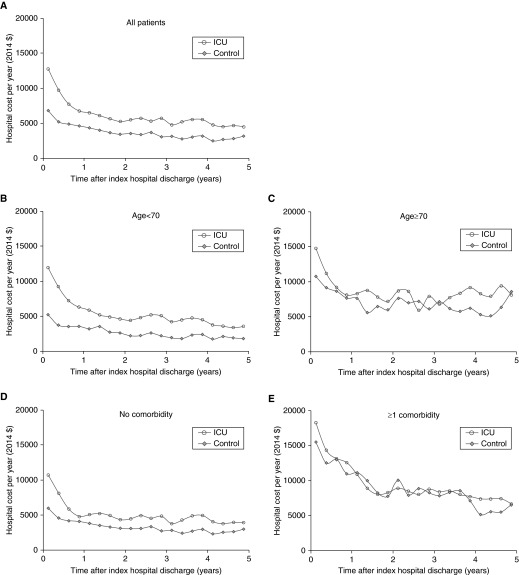
Effect modification
The adjusted excess rate of 5-year hospital admissions (on a relative scale) in the ICU cohort, compared with hospital control subjects, varied by age and comorbidity (Figure 3). On stratification by age, relative hospital admission rates for the ICU cohort compared with hospital control subjects were higher for people less than 70 years of age (ARR, 1.28; 95% CI, 1.18–1.38; P < 0.001) than for those aged 70 years of age or older (ARR, 1.09; 95% CI, 1.00–1.19; P = 0.05; interaction term, P < 0.001) (Figure 3). In competing risks analyses, age was an effect modifier (interaction term, P < 0.001), but comorbidity was not (P = 0.26) (Figure E2).
Figure 3.
Mean hospital costs in the 5-year period after discharge from index hospitalization in intensive care unit (ICU) survivors compared with hospital control subjects (A) for all patients, (B and C) for patients stratified by age (B, age < 70 yr; C, age ≥ 70 yr), and (D and E) in the presence of Charlson comorbidity (D, no comorbidity; E, one or more comorbidities). Each point represents the mean cost for each quarter (reported as cost per year) for each patient alive at the start of each quarter. Modeling number of admissions rather than costs, age was an effect modifier for the admission rate ratio (ARR) of ICU survivors compared with hospital controls (age < 70 yr: ARR, 1.28; 95% confidence interval [CI], 1.18–1.38; P < 0.001; age ≥ 70 yr: ARR, 1.09; 95% CI, 1.00–1.19; P = 0.05; interaction term, P < 0.001). Similarly, comorbidity is an effect modifier (no comorbidity: ARR, 1.25; 95% CI, 1.17–1.34; P < 0.001; one or more comorbidities: ARR, 1.02; 95% CI, 0.91–1.14; P = 0.72; interaction term, P = 0.02).
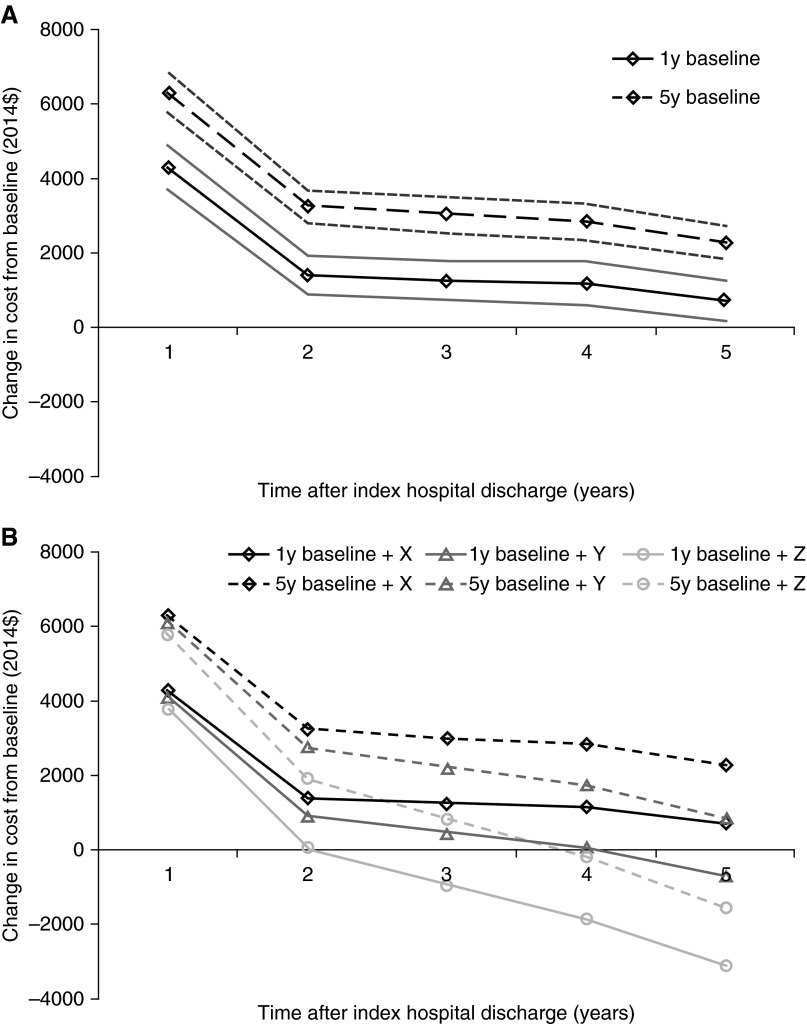
Resource Use: Pre/Post Within-Individual Analysis
For individuals in the ICU cohort, mean 5-year postdischarge hospital costs were greater than baseline cost of hospital care, derived from hospital costs in the year before ICU admission (mean difference from baseline, $7,919 per person; 95% CI, $6,324–$9,516; P < 0.001). Mean annual hospital costs were greater than baseline costs for each year of follow-up (Figure 4). These were highest for the first year ($9,349; difference from baseline, $4,239; 95% CI, $3,670–$4,809; P < 0.001) and lowest for the fifth year ($4,670; difference, $724; 95% CI, $200–$1,248; P = 0.007). Under all six scenarios of varying baseline costs and including effects of aging, subsequent hospital costs were higher than baseline for the first year after hospital discharge; for the third year, the five scenarios still indicated higher hospital costs than baseline; for the fifth year, this was reduced to three scenarios (Figure 4).
Figure 4.
Difference in mean annual hospital costs from baseline cost in pre/post within-individual analyses in the 5-year period after discharge from index hospitalization: sensitivity analysis in varying baseline hospital cost and effect of aging on hospital costs. (A) Baseline hospital cost was varied from the mean annual hospital cost in the 1 year before index hospital admission (solid lines) and the mean annual hospital cost in the 5 years before index hospital admission (dashed lines). Lighter lines represent 95% confidence intervals. (B) In addition to varying baseline costs, the effect of aging on hospital costs was modeled, using the gradient of increasing costs during the preindex hospitalization period. The gradient was assumed to vary under three scenarios: no effect of aging on costs (X); the assumption that the cost gradient during Years –5, –4, and –3 pre–index hospitalization continued during Years 0 to 5 years posthospitalization (Y); and finally, the assumption that the cost gradient from –5 years to 0 years pre–index hospitalization continued during Years 0 to 5 years posthospitalization (Z).
Discussion
This national, complete cohort of ICU patients experienced significantly higher mortality and used more hospital resources in the 5 years after hospital discharge compared with hospital survivors who did not require ICU admission. The excess resource use persisted throughout the 5-year follow-up. Factors present before ICU admission were much stronger predictors of hospital resource use than those associated with the acute illness. The excess mortality and use of hospital resource were most pronounced in patients less than 70 years of age and those with no preexisting illness.
The persisting excess mortality and hospital costs associated with ICU survivorship likely result from a complex interplay between preillness factors, acute illness factors, and health care organizational structures. We were surprised that the acute illness factors such as ICU admission illness severity and requirement for organ support had little or no influence on subsequent resource use. It is widely assumed that acute illness factors are important mediators in the causal pathway to post–critical illness morbidity, for example, through residual organ dysfunction or disability (24–26). Our data indicate that preillness factors, such as previous hospital resource use and comorbidity, most strongly influence subsequent hospital resource use. These findings have implications for clinicians and health service planners, and in future trial design where survivorship and health care costs beyond the acute hospital admission episode are of interest. The complex health and social care problems of ICU survivors, which in many cases may be part of a chronic trajectory of deteriorating health, justify the more holistic approach to post-ICU recovery that has been recommended by stakeholder groups (8) and the United Kingdom’s National Institute for Health and Care Excellence (27). Clinicians are increasingly aware of the burden that ICU survivorship places on patients and families. Our results will help to inform discussions with family members of the consequences of surviving an admission to ICU. In the context of recent ICU survivorship trials yielding disappointing results (28–30), further investigation of preillness trajectories may identify those at highest risk of readmission and enable targeted interventions (31).
Compared with hospital control subjects, we found that excess hospital resource use was concentrated in younger patients and those with no previous comorbidities. These patients are most likely to be previously fit and well patients experiencing a critical illness “hit” leaving them with new health problems (32). This novel finding has implications for these patients, which may contrast with patients whose ICU admission punctuates an already deteriorating health trajectory. The economic consequences may be substantially greater than the costs relating to acute hospital admission, for example, through substantial loss of earnings and long-term social costs. This is an important consideration for health and social policy makers, and requires confirmation in other settings.
Our population-level estimates of the cost associated with ICU survivorship can be used to inform health policy. The high emergency hospital readmission rate in ICU survivors represents unplanned access to the health service. We did not have sufficient information to classify these as potentially avoidable or unavoidable admissions in this study. Readmissions may be modifiable through proactive primary care, social care, or improvement in transitions of care. Further work is required to investigate this issue.
Other studies describe excess mortality in ICU survivors compared with hospital populations, ranging from 7% (33) to 21% (34). Our data are consistent with these estimates. Comparison with other studies reporting health care resource use or costs is difficult because of organizational differences at ICU and wider health service level and international differences in costing health care (35). However, compared with resource data for the first year after discharge summarized in a systematic review and a more recent publication (35, 36), our cohort experienced comparable hospital readmission rates (1.1 compared with 0.6–2.8/patient) and days in hospital (11.1 compared with 4.2–19.0/patient), although lower average 1-year hospitalization ($8,863 compared with $9,769–$66,812 [converted to 2014 U.S. dollars]).
Some studies with control populations report results in conflict with our findings. A Canadian study reported that ICU survivors had a lower readmission rate compared with hospital control subjects during 3 years of follow-up (ARR, 0.80; 95% CI, 0.77–0.82) (37). Differences in study population (substantially younger ICU and hospital cohorts; median age, 54 and 47 yr, respectively), analysis methods (stratified analysis on vital status at the end of follow-up), and confounder selection (models included index admission hospital length of stay, strongly correlated with ICU cohort membership) may explain the discordant results. A study limited to U.S. Medicare beneficiaries more than 65 years of age found higher unadjusted 1- and 3-year readmission rates in ICU survivors compared with hospital and population control subjects (33). A third study of survivors of severe sepsis found that, relative to other hospital survivors, patients spent a greater proportion of days alive admitted to inpatient facilities and fewer days at home in the year after hospital discharge (38).
Strengths of our study include the use of a complete national cohort of patients, inclusion of all ICU admissions, and near complete follow-up. These factors minimize the risk of bias frequently encountered in prospective observational studies (9). To investigate and fully describe the excess burden associated with ICU survivorship, we used a variety of outcomes (mortality, hospital admissions, costs), control subjects (hospital control subjects and pre/post within-individual), and multivariable models (negative binomial, competing risk regression), which allowed more accurate modeling of heavily skewed resource data. As mortality rates were higher in the ICU population, our primary analysis may have demonstrated lower resource use in the ICU population because of the shorter duration of time spent alive during follow-up, although health care costs may also increase toward the end of life and therefore reduce this difference (39). Our primary analysis is the correct approach from a health accounting perspective: modeling future funding of health care for ICU survivor populations by health care providers requires data relating to costs, which will be lower with high, early mortality rates. However, to better understand the attributable cost of ICU survivorship, we also presented resource use by cohorts, using an actuarial, life table approach, presenting mean costs per person for time intervals conditional on survival at the start of each time interval, as well as conducting additional statistical modeling to allow for the competing risk of death when comparing estimates of resource use between cohorts.
A potential weaknesses was loss of patients through emigration during follow-up; however, emigration in Scotland is known to be only 0.6% annually for residents at least 45 years of age (17). We were also unable to identify hospital control subjects who “crossed over” to become ICU survivors, thereby potentially biasing estimates away from the null. A further weakness was the method used to cost hospital resources. We used a per diem cost for each day of hospital stay, which may overestimate hospital costs, particularly for hospital admissions with prolonged lengths of stay. Exposures, confounders, and outcomes were also limited to those collected in registries. For example, comorbidity was likely to be imperfectly measured, and there was no measure of premorbid functional status or frailty, which are factors that influence decision-making around ICU admission and outcomes (40). Furthermore, data relating to limiting or withdrawing life-sustaining therapy within the ICU were not available, which may have reduced the frequency of frailer individuals in the ICU cohort but not the hospital control cohort. These factors may have led to residual confounding in comparisons between ICU and hospital populations, in which the direction of bias may be away from the null if the ICU population had greater unmeasured comorbidity. Despite matching cohorts on four variables and adjusting for available variables including preindex admission hospital resource use, we cannot assume that hospital control subjects were similar to the ICU cohort in all aspects other than being admitted to the ICU (41). Because of the importance of this issue, we explored this further in the pre/post within-individual analyses of hospital readmissions. Triangulation of our observational findings, using these two different approaches, each of which had its own sources of bias and confounding, demonstrated consistency in the direction of excess costs associated with ICU survivorship. Consistency in the magnitude of excess costs was more difficult to demonstrate as cost comparisons between cohorts were not controlled for imbalances between cohort characteristics other than those on which cohorts were matched.
Measurement of additional outcomes, such as functional status and quality of life, would have allowed a more complete understanding of the consequences of critical illness, but these are not available at the population level. Although hospital resource use dominates postdischarge costs (35, 36), extending resource measurement beyond this to social care and societal costs, such as loss of earnings or the financial burden on caregivers, would have allowed a more comprehensive assessment of resource use (42).
Conclusions
ICU survivors have increased mortality and hospital costs in the 5 years after ICU admission, which represents a substantial burden on individuals, caregivers, and society. Pre-ICU admission factors indicative of poor health are strong predictors of higher long-term resource use, but excess resource use compared with that of other hospitalized patients is greatest for younger patients without significant preexisting comorbidity. A better understanding of causal mechanisms, effective interventions, and subgroups at higher risk is required to guide policy makers and clinicians.
Supplementary Material
Acknowledgments
Acknowledgment
The authors are grateful to the Scottish Intensive Care Society Audit Group and Information Services Division (ISD Scotland) for providing data and undertaking linkage.
Footnotes
Supported by a fellowship from the Chief Scientist Office for Scotland. The funder had no role in any of the following: design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author Contributions: N.I.L. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. N.I.L., T.S.W., S.H.W., K.M.R., and G.D.M. contributed to the conception and design of the work. N.I.L., M.A.G., C.H., and R.D. contributed to data acquisition and analysis. All authors contributed to interpretation of data for the work. N.I.L. and T.S.W. drafted the work. All authors revised it critically for important intellectual content. All authors gave final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201511-2234OC on January 27, 2016
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39:371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 2.Stevens RD, Dowdy DW, Michaels RK, Mendez-Tellez PA, Pronovost PJ, Needham DM. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33:1876–1891. doi: 10.1007/s00134-007-0772-2. [DOI] [PubMed] [Google Scholar]
- 3.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, et al. Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 4.Jackson JC, Hopkins RO, Miller RR, Gordon SM, Wheeler AP, Ely EW. Acute respiratory distress syndrome, sepsis, and cognitive decline: a review and case study. South Med J. 2009;102:1150–1157. doi: 10.1097/SMJ.0b013e3181b6a592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009;35:796–809. doi: 10.1007/s00134-009-1396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, Needham DM. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005;31:611–620. doi: 10.1007/s00134-005-2592-6. [DOI] [PubMed] [Google Scholar]
- 7.Cuthbertson BH, Roughton S, Jenkinson D, Maclennan G, Vale L. Quality of life in the five years after intensive care: a cohort study. Crit Care. 2010;14:R6. doi: 10.1186/cc8848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40:502–509. doi: 10.1097/CCM.0b013e318232da75. [DOI] [PubMed] [Google Scholar]
- 9.Williams TA, Leslie GD. Challenges and possible solutions for long-term follow-up of patients surviving critical illness. Aust Crit Care. 2011;24:175–185. doi: 10.1016/j.aucc.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Iwashyna TJ, Netzer G. The burdens of survivorship: an approach to thinking about long-term outcomes after critical illness. Semin Respir Crit Care Med. 2012;33:327–338. doi: 10.1055/s-0032-1321982. [DOI] [PubMed] [Google Scholar]
- 11.Lone NI, Haddow C, Dobbie R, Gillies MA, Rowan KM, Walsh TS, Wild SH, Murray GD. Major healthcare resource use in ICU survivors: a national data linkage cohort study [abstract] J Intensive Care Soc. 2013;14(1) Suppl:S6–S7. [Google Scholar]
- 12.Lone NI. Long-term mortality and major healthcare resource use following admission to Scottish intensive care units [abstract] J Intensive Care Soc. 2013;14:68–69. [Google Scholar]
- 13.Lone NI, Walsh TS. Healthcare cost trajectories before and after critical illness: a national data linkage cohort study [abstract] J Intensive Care Soc. 2015;16(1) Suppl:18. [Google Scholar]
- 14.Scottish Intensive Care Society Audit GroupScottish Intensive Care Society Audit Group annual report: audit of intensive care units in Scotland 2014: reporting on 2013. 2014[accessed 2016 Feb 1]. Available from: http://www.sicsag.scot.nhs.uk/docs/SICSAG-report-2014-web.pdf
- 15.National Records of ScotlandVital events reference tables. 2015[accessed 2016 Feb 1]. Available from: http://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/vital-events-reference-tables
- 16.Information Services Division ScotlandScottish Health Service costs. 2014[accessed 2016 Feb 1]. Available from: http://www.isdscotland.org/Health-Topics/Finance/Costs/
- 17.National Records of ScotlandMigration between Scotland and overseas. 2014[accessed 2016 Feb 1]. Available from: http://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/migration/migration-statistics/migration-between-scotland-and-overseas
- 18.National StatisticsScottish Index of Multiple Deprivation: 2009 general report. 2009[accessed 2016 Feb 1]. Available from: http://www.scotland.gov.uk/Resource/Doc/933/0115249.pdf
- 19.Scottish GovernmentUrban rural classification 2007–2008. 2010[accessed 2016 Feb 1]. Available from: http://www.scotland.gov.uk/Resource/Doc/233802/0063988.pdf
- 20.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Hilbe JM. Cambridge: Cambridge University Press; 2011. Negative binomial regression. [Google Scholar]
- 22.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 23.Andersen PK, Geskus RB, de Witte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol. 2012;41:861–870. doi: 10.1093/ije/dyr213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lone NI, Walsh TS. Impact of intensive care unit organ failures on mortality during five years following critical illness. Am J Respir Crit Care Med. 2012;186:640–647. doi: 10.1164/rccm.201201-0059OC. [DOI] [PubMed] [Google Scholar]
- 25.Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175:523–529. doi: 10.1001/jamainternmed.2014.7889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ranzani OT, Zampieri FG, Besen BA, Azevedo LC, Park M. One-year survival and resource use after critical illness: impact of organ failure and residual organ dysfunction in a cohort study in Brazil. Crit Care. 2015;19:269. doi: 10.1186/s13054-015-0986-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan T, Brett SJ, Stokes T Guideline Development Group. Rehabilitation after critical illness: summary of NICE guidance. BMJ. 2009;338:b822. doi: 10.1136/bmj.b822. [DOI] [PubMed] [Google Scholar]
- 28.Walsh TS, Salisbury LG, Merriweather JL, Boyd JA, Griffith DM, Huby G, Kean S, Mackenzie SJ, Krishan A, Lewis SC, et al. RECOVER Investigators. Increased hospital-based physical rehabilitation and information provision after intensive care unit discharge: the RECOVER randomized clinical trial. JAMA Intern Med. 2015;175:901–910. doi: 10.1001/jamainternmed.2015.0822. [DOI] [PubMed] [Google Scholar]
- 29.Cuthbertson BH, Rattray J, Campbell MK, Gager M, Roughton S, Smith A, Hull A, Breeman S, Norrie J, Jenkinson D, et al. PRaCTICaL study group. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. BMJ. 2009;339:b3723. doi: 10.1136/bmj.b3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elliott D, McKinley S, Alison J, Aitken LM, King M, Leslie GD, Kenny P, Taylor P, Foley R, Burmeister E. Health-related quality of life and physical recovery after a critical illness: a multi-centre randomised controlled trial of a home-based physical rehabilitation program. Crit Care. 2011;15:R142. doi: 10.1186/cc10265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iwashyna TJ, Netzer G, Langa KM, Cigolle C. Spurious inferences about long-term outcomes: the case of severe sepsis and geriatric conditions. Am J Respir Crit Care Med. 2012;185:835–841. doi: 10.1164/rccm.201109-1660OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Iwashyna TJ. Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Respir Crit Care Med. 2012;186:302–304. doi: 10.1164/rccm.201206-1138ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA. 2010;303:849–856. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- 34.Keenan SP, Dodek P, Chan K, Hogg RS, Craib KJP, Anis AH, Spinelli JJ. Intensive care unit admission has minimal impact on long-term mortality. Crit Care Med. 2002;30:501–507. doi: 10.1097/00003246-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Lone NI, Seretny M, Wild SH, Rowan KM, Murray GD, Walsh TS. Surviving intensive care: a systematic review of healthcare resource use after hospital discharge. Crit Care Med. 2013;41:1832–1843. doi: 10.1097/CCM.0b013e31828a409c. [DOI] [PubMed] [Google Scholar]
- 36.Ruhl AP, Lord RK, Panek JA, Colantuoni E, Sepulveda KA, Chong A, Dinglas VD, Shanholtz CB, Pronovost PJ, Steinwachs DM, et al. Health care resource use and costs of two-year survivors of acute lung injury: an observational cohort study. Ann Am Thorac Soc. 2015;12:392–401. doi: 10.1513/AnnalsATS.201409-422OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Keenan SP, Dodek P, Chan K, Simon M, Hogg RS, Anis AH, Spinelli JJ, Tilley J, Norena M, Wong H. Intensive care unit survivors have fewer hospital readmissions and readmission days than other hospitalized patients in British Columbia. Crit Care Med. 2004;32:391–398. doi: 10.1097/01.CCM.0000108882.65743.91. [DOI] [PubMed] [Google Scholar]
- 38.Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190:62–69. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geue C, Briggs A, Lewsey J, Lorgelly P. Population ageing and healthcare expenditure projections: new evidence from a time to death approach. Eur J Health Econ. 2014;15:885–896. doi: 10.1007/s10198-013-0543-7. [DOI] [PubMed] [Google Scholar]
- 40.Bagshaw SM, Stelfox HT, Johnson JA, McDermid RC, Rolfson DB, Tsuyuki RT, Ibrahim Q, Majumdar SR. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med. 2015;43:973–982. doi: 10.1097/CCM.0000000000000860. [DOI] [PubMed] [Google Scholar]
- 41.Maldonado G, Greenland S. Estimating causal effects. Int J Epidemiol. 2002;31:422–429. [PubMed] [Google Scholar]
- 42.Griffiths J, Hatch RA, Bishop J, Morgan K, Jenkinson C, Cuthbertson BH, Brett SJ. An exploration of social and economic outcome and associated health-related quality of life after critical illness in general intensive care unit survivors: a 12-month follow-up study. Crit Care. 2013;17:R100. doi: 10.1186/cc12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.