To the Editor:
Bronchoscopic lung volume reduction with endobronchial valves (BLVR) can improve lung function and exercise capacity in appropriately selected patients with emphysema (1–5). Although early data have been encouraging (6), it is not clear whether response to BLVR will translate into sustained survival benefit, as observed after lung volume reduction surgery (LVRS) (7).
Methods
We reviewed the long-term outcome of BLVR in 19 patients with heterogeneous emphysema (Table 1) treated with Emphasys valves, placed to achieve occlusion of a single target lobe, between July 2002 and February 2004 (3, 4, 6). Survival data to November 2015 were compared, using Kaplan-Meier analysis, between those with (n = 5) and those without (n = 14) evidence of atelectasis on thoracic computed tomography scan performed 1 month postprocedure.
Table 1.
Baseline Characteristics
| All (N = 19) | Nonatelectasis (n = 14) | Atelectasis (n = 5) | t Test | |
|---|---|---|---|---|
| Age, yr | 58.7 (8.7) | 59.6 (9.0) | 56.0 (7.6) | 0.4 |
| Female, % | 16 | 14 | 20 | 0.7 |
| BMI, kg ⋅ m−2 | 23.3 (4.1) | 21.6 (2.9) | 28.2 (2.9) | 0.004 |
| FFMI | 16.1 (1.6) | 15.8 (1.5) | 17.5 (1.4) | 0.05 |
| SGRQ symptoms | 63.7 (19.2) | 63.3 (18.2) | 64.9 (24.3) | 0.9 |
| SGRQ activity | 78.5 (16.5) | 76.9 (18.1) | 83.2 (11.0) | 0.5 |
| SGRQ impacts | 45.1 (13.5) | 42.8 (13.9) | 51.9 (11.0) | 0.2 |
| SGRQ total | 58.4 (12.8) | 56.5 (14.2) | 63.5 (2.3) | 0.3 |
| FEV1% pred | 28.4 (11.9) | 28.6 (11.8) | 27.7 (13.3) | 0.9 |
| FVC, % pred | 80.3 (22.4) | 80.1 (18.2) | 81.0 (34.3) | 0.9 |
| TLC, % pred | 139.3 (15.6) | 141.1 (16.0) | 134.3 (14.7) | 0.4 |
| RV, % pred | 260.5 (68.4) | 264.4 (66.6) | 249.4 (80.0) | 0.7 |
| RV/TLC | 63.2 (12.0) | 64.0 (10.8) | 60.9 (16.1) | 0.6 |
| FRC, % pred | 208.9 (38.9) | 213.3 (37.9) | 200.1 (44.1) | 0.5 |
| DlCO, % pred | 35.9 (10.9) | 35.6 (11.2) | 36.9 (11.1) | 0.8 |
| PaCO2 | 4.8 (0.6) | 4.8 (0.5) | 4.8 (0.8) | 0.9 |
| PaO2 | 9.8 (1.5) | 10.0 (1.4) | 9.2 (1.7) | 0.3 |
| Exacerbation rate/yr | 2.2 (1.9) | 1.9 (1.5) | 2.8 (2.7) | 0.4 |
| Peak workload, W | 48.9 (18.0) | 50.4 (20.0) | 40 (11.8) | 0.6 |
| o2, L/min | 0.84 (0.22) | 0.85 (0.23) | 0.85 (0.26) | 0.99 |
| Vco2, L/min | 0.78 (0.21) | 0.79 (0.27) | 0.79 (0.23) | 0.98 |
| e, L/min | 29.7 (8.1) | 29.5 (9.9) | 29.5 (4.1) | 0.99 |
Definition of abbreviations: BMI = body mass index; DlCO = diffusing capacity of the lung for carbon monoxide; FFMI = fat-free mass index; FRC = functional residual capacity; pred = predicted; SGRQ = St. George’s Respiratory Questionnaire; RV = residual volume; TLC = total lung capacity.
Values are mean (SD). Exercise parameters are values obtained during symptom-limited incremental cycle ergometry.
Results
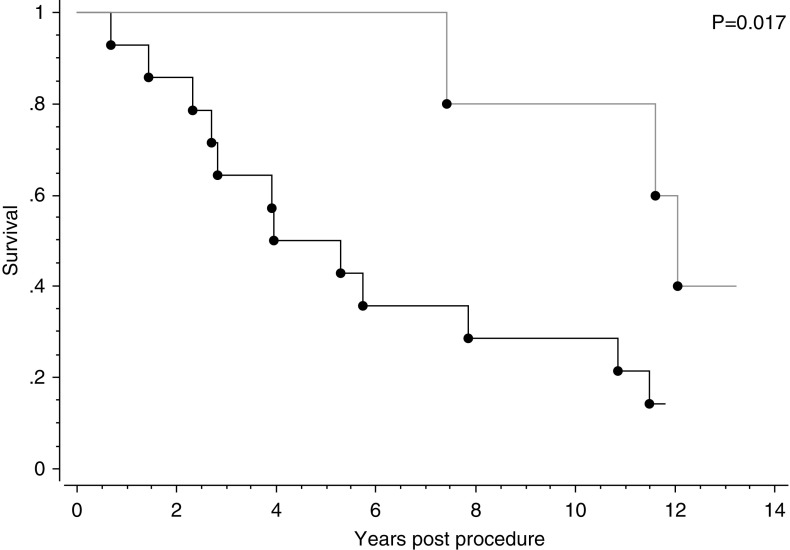
In the atelectasis group, two of five patients (40%) were still alive compared with 2 of 14 (14%) of the nonatelectasis group (P = 0.017) (Figure 1).
Figure 1.
Prolonged transplant-free survival in which atelectasis occurs after bronchoscopic lung volume reduction with endobronchial valves. The upper line shows significantly improved survival in patients (n = 5) in whom radiological atelectasis occurred after endobronchial valve placement occurred compared with the lower line (n = 14), for which atelectasis did not occur (P = 0.017).
Discussion
These data suggest that successful BLVR may be associated with a substantial, persisting survival benefit similar to that observed after LVRS. The most likely explanation for the occurrence of atelectasis in some, but not other, patients is the absence or presence of collateral ventilation between the target lobe and adjacent lung because of disruption of the interlobar fissures by emphysema. Patients in whom collateral ventilation is thought to be present (either measured directly or assessed using analysis of interlobar fissures on computed tomography scans) are not now recommended for BLVR. A second issue is a technical one around valve placement and airway anatomy. Sometimes it is difficult to achieve a satisfactory seal, and valves may need to have their placement adjusted. Overall, the response rate was similar to that observed in other trials in which patients were not selected on the basis of collateral ventilation (5).
Although it is possible that the difference in survival could be explained by some disparity in the baseline characteristics of the two groups other than collateral ventilation, this seems unlikely. The groups were well matched (Table 1), including for gas transfer, the lung function parameter most strongly associated with survival in chronic obstructive pulmonary disease (8), as well as for cardiopulmonary exercise parameters and exacerbation history.
The absence of a control group is, of course, a limitation for the interpretation of these data, but they do nevertheless support the idea that BLVR, similar to LVRS, can improve the natural history of chronic obstructive pulmonary disease and support equipoise between the procedures. The indications for endobronchial valves and LVRS overlap considerably: heterogeneous emphysema with an appropriate target area and hyperinflation and gas trapping in patients who are not too frail to be able to cope safely with the intervention or are outside the lung function safety criteria (9). Direct comparison studies of adequate duration are now needed to compare outcomes between these two treatment modalities so that clinicians and patients can make informed choices about whether to proceed with a bronchoscopic or surgical approach.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank Emphasys Medical Inc. (Redwood, CA) for providing the valves used in the original procedures.
Footnotes
Supported by the National Institute for Health Research Respiratory Biomedical Research Unit at Royal Brompton and Harefield National Health Service Foundation Trust and Imperial College, London, United Kingdom, who part fund M.I.P.’s salary. D.M.H. is a National Institute for Health Research Senior Investigator. N.S.H. was supported by The Wellcome Trust (G062414).
The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research, or the Department of Health.
Author Contributions: Patients were recruited and studied by T.P.T., M.I.P., and N.S.H.; D.M.H. performed radiologic analysis; S.V.K. and P.L.S. interpreted the data; and N.S.H. and J.G. produced a first draft to which all authors contributed and that was approved by all authors in this final version.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Davey C, Zoumot Z, Jordan S, McNulty WH, Carr DH, Hind MD, Hansell DM, Rubens MB, Banya W, Polkey MI, et al. Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomised controlled trial. Lancet. 2015;386:1066–1073. doi: 10.1016/S0140-6736(15)60001-0. [DOI] [PubMed] [Google Scholar]
- 2.Klooster K, ten Hacken NHT, Hartman JE, Kerstjens HAM, van Rikxoort EM, Slebos D-J. Endobronchial valves for emphysema without interlobar collateral ventilation. N Engl J Med. 2015;373:2325–2335. doi: 10.1056/NEJMoa1507807. [DOI] [PubMed] [Google Scholar]
- 3.Hopkinson NS, Toma TP, Hansell DM, Goldstraw P, Moxham J, Geddes DM, Polkey MI. Effect of bronchoscopic lung volume reduction on dynamic hyperinflation and exercise in emphysema. Am J Respir Crit Care Med. 2005;171:453–460. doi: 10.1164/rccm.200407-961OC. [DOI] [PubMed] [Google Scholar]
- 4.Toma TP, Hopkinson NS, Hillier J, Hansell DM, Morgan C, Goldstraw PG, Polkey MI, Geddes DM. Bronchoscopic volume reduction with valve implants in patients with severe emphysema. Lancet. 2003;361:931–933. doi: 10.1016/S0140-6736(03)12762-6. [DOI] [PubMed] [Google Scholar]
- 5.Sciurba FC, Ernst A, Herth FJF, Strange C, Criner GJ, Marquette CH, Kovitz KL, Chiacchierini RP, Goldin J, McLennan G VENT Study Research Group. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med. 2010;363:1233–1244. doi: 10.1056/NEJMoa0900928. [DOI] [PubMed] [Google Scholar]
- 6.Hopkinson NS, Kemp SV, Toma TP, Hansell DM, Geddes DM, Shah PL, Polkey MI. Atelectasis and survival after bronchoscopic lung volume reduction for COPD. Eur Respir J. 2011;37:1346–1351. doi: 10.1183/09031936.00100110. [DOI] [PubMed] [Google Scholar]
- 7.Criner GJ, Cordova F, Sternberg AL, Martinez FJ. The National Emphysema Treatment Trial (NETT) part II: lessons learned about lung volume reduction surgery. Am J Respir Crit Care Med. 2011;184:881–893. doi: 10.1164/rccm.201103-0455CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boutou AK, Shrikrishna D, Tanner RJ, Smith C, Kelly JL, Ward SP, Polkey MI, Hopkinson NS. Lung function indices for predicting mortality in COPD. Eur Respir J. 2013;42:616–625. doi: 10.1183/09031936.00146012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zoumot Z, Jordan S, Hopkinson NS. Emphysema: time to say farewell to therapeutic nihilism. Thorax. 2014;69:973–975. doi: 10.1136/thoraxjnl-2014-205667. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.