Abstract
Purpose
According to a 1944 publication by Swyer benign prostatic hyperplasia develops in some men after age 45 with further prostatic growth whereas in other men prostate size remains stable or decreases with advancing age. Although there is an abundance of literature describing prostatic enlargement in association with benign prostatic hyperplasia, less is known about the phenomenon of prostate atrophy.
Materials and Methods
In the Baltimore Longitudinal Study of Aging serial pelvic magnetic resonance imaging was performed in men without prostate cancer beginning in 1993. From this population we retrospectively identified 278 men with 2 or more magnetic resonance imaging determined prostate volume measurements to examine differential growth rates in a cohort of community men over time.
Results
Median age was 58 years and median prostate size was 28 cc at study entry. At a median followup of 4.3 years prostate size increased in 61.9% and remained stable or decreased in 38.1% of men. The median rate of volume change was 0.6 cc per year (range −9.9 to 62.1), corresponding to a median growth rate of 2.5% per year (range −29.2 to 176.4%). During followup 64.6% of men with an initial prostate size less than 40 cc had prostate growth compared to only 50.9% of men with an initial prostate size of 40 cc or greater.
Conclusions
These results suggest that changes in prostate size are highly variable among aging men. Although benign prostatic hyperplasia is common, a considerable proportion of aging men have a stable or decreasing prostate size. Further research is needed to identify the underlying mechanism for such differences in prostate growth.
Keywords: prostatic hyperplasia, prostate, organ size, atrophy, longitudinal studies
Based on autopsy studies histological evidence of benign prostatic hyperplasia is found in 8% of men 31 to 40 years old and increases to more than 70% of men by the seventh decade of life.1 Specifically Berry et al reported that average prostate weight increases from approximately 20 gm at age 40 to 38.8 gm in men older than 80 years.
Due to its high prevalence with increasing age BPH is a significant burden on the United States health care system. According to the Urological Diseases in America Project BPH alone was responsible for approximately 4.5 million office visits and $1.1 billion in direct health care costs in the year 2000.2
Because much of the existing literature on BPH is derived from autopsy series, less is known about changes in prostate size in an individual over time. In an early randomized trial of finasteride for BPH Tempany et al used MRI to estimate changes in prostate size over time.3 In 8 men from the placebo group the median change in total prostate volume was 1.1 ± 3.1 cc which corresponded to a 4.2% change during 1 year of followup. Other clinical trials have similarly included data on prostate volume changes as a secondary end point in men with clinical symptoms of BPH.4 However, there are fewer data on intraindividual prostate volume changes over time in unselected community based populations. This information is medically relevant since prostatic enlargement is associated with the risk of clinical events including acute urinary retention and BPH surgery.5
St. Sauver et al performed serial transrectal ultrasound in a randomly selected cohort from Olmsted County, Minnesota.6 Using MRI instead our research group previously reported on age related prostate volume changes in 64 community men from the Baltimore Longitudinal Study of Aging.7 In these men the overall prostate growth rate was 2.36 cc per year. In this study we expand on these findings and further examine longitudinal changes in prostate volume in a larger population of community men from the BLSA.
METHODS
The BLSA was initiated in 1958 by the National Institute on Aging (Bethesda, Maryland) as a prospective cohort study on the effects of aging. Since then approximately 1,806 males have enrolled, primarily residents of Maryland or Washington, D. C. As part of the study protocol participants undergo a comprehensive medical, physical and neuropsychological evaluation every 2 years as previously described.7,8 All BLSA subjects provided informed consent, and the study protocol was approved by the institutional review boards of MedStar and the Johns Hopkins Medical Institutions (Baltimore, Maryland).
Beginning in September 1991 PSA measurements and digital rectal examinations were performed at each evaluation. Transrectal ultrasound guided prostate biopsy was recommended for a PSA greater than 4.0 ng/ml or suspicious digital rectal examination. For men without evidence of prostate cancer pelvic magnetic resonance imaging was performed every 2 years as part of the urological examination beginning in 1993. The T2 axial images were used to calculate prostate volume using a semiautomated image analysis system as previously described.7
In this study we identified 540 men without prostate cancer who underwent pelvic MRI. We excluded from analysis 24 men with a history of finasteride use and 24 who underwent transurethral resection of the prostate at an unknown time. Of the remaining men 278 had at least 2 prostate volume measurements on MRI and formed the final study population. Of the 278 men 136 (49%) had 2 serial MRIs, 76 (27%) had 3, 49 (18%) had 4 and 17 (6%) had 5 available. To account for the various numbers of MRIs available in the study population we calculated volume changes by a 2-point method using the first and last measurement for all participants. To validate this approach we compared the results of the 2-point method to a linear regression using all values for men with more than 2 MRIs and found a Pearson correlation coefficient of 0.999. Prostate growth was defined as an increase in prostate size between MRIs whereas prostate shrinkage was defined as a decrease in prostate size between measurements. Finally prostate size was considered stable if the volume remained the same.
Baseline measurements of testosterone and sex hormone-binding globulin were available in 181 men. These measurements were performed between 7:00 a.m. and 9:30 a.m. after an overnight fast as previously described.9 The free testosterone index was calculated as the molar ratio of testosterone-to-sex hormone-binding globulin. Participants with sex hormone data were significantly younger at the initial visit than those who did not have hormonal measurements (mean age 54.6 vs 58.2 years, p = 0.013). However, baseline prostate volume (p = 0.936) and PSA (p = 0.198) were similar between the groups.
We used descriptive statistics to examine the demographics and prostate volume distribution in the overall study population. The rate of change in prostate size was calculated in cc per year and percent change per year. We created box plots of changes in prostate size (cc per year) by age at first MRI (younger than 55, 55 to 65, and 65 years or older) based on distribution in the BLSA.7 Pearson correlation coefficients were used to examine the correlation between prostate volume changes and age. In the overall study population linear regression models were performed with the rate of change in volume as the dependent variable, including the covariates (continuous) of age, prostate volume and PSA measured at baseline. In the subset of 181 men with baseline sex hormone measurements a separate linear regression model was performed to evaluate the association between baseline free testosterone index and the rate of change in prostate volume, also controlling for the initial age, prostate volume and PSA. The t test was used to compare clinical characteristics between men who did and those who did not have sex hormone data. SAS® version 9.1 was used for all statistical analysis.
RESULTS
In the study population the median age was 58 years (range 30 to 74) at the first MRI and the majority of the men were white. Median PSA was 1.0 ng/ml (range 0.05 to 10.9) at the first MRI. Most men had 2 serial MRIs (range 2 to 5) during a median followup of 4.3 years (range 1.8 to 9.8).
Median prostate volume was 28.1 cc (range 4.4 to 135.0) on the first MRI and 31.1 cc (range 8.7 to 237.3) at the end of the study period. In the overall study population prostate volume increased at a median rate of 0.6 cc per year (range −9.9 to 62.1), which corresponded to a median 2.5% annual change. Overall 172 (61.9%) men had prostate growth, 4 (1.4%) had a stable prostate size and 102 (36.7%) had a decrease in prostate size during the study period.
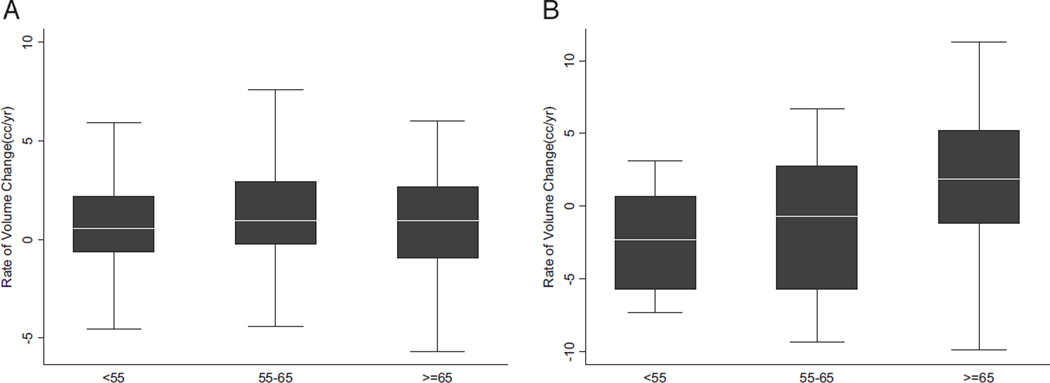
The figure shows the distribution of prostate volume changes by age at first MRI. Among 223 men with an initial prostate size less than 40 cc, an increase in size occurred in 144 (64.6%) and the remaining 79 (35.4%) had a stable or decreasing size. In these men the median prostate growth rate was 0.7 cc per year (range −8.6 to 62.1), which corresponded to a median 2.9% annual change. In 55 men with an initial prostate size of 40 cc or greater 28 (50.9%) had a further increase in size and 27 (49.1%) had no change or shrinkage. Among these men the median prostate growth rate was 0.1 cc per year (range −9.9 to 48.7), which corresponded to a median 0.3% annual change.
Box plots showing changes in prostate volume (cc per year) by age at first MRI in men with initial volume less than 40 cc (A) and 40 cc or greater (B). Boxes represent IQR (25th to 75th percentiles) with horizontal line indicating median. Vertical line indicates 1.5 times IQR and outliers are not shown.
Table 1 shows the Pearson correlation coefficients between measures of prostate volume change and age. Overall there was no statistically significant correlation between age and the rate of change in prostate volume. Linear regression was then performed to predict the rate of change in prostate volume for the overall study population. As shown in table 2 baseline PSA was significantly associated with the rate of volume change (p = 0.0006) while age and prostate volume were not.
Table 1.
Pearson correlation coefficients between age at the first MRI and rate of prostate volume changes
| Overall | Initial Prostate Vol Less Than 40 cc |
Initial Prostate Vol 40 cc or Greater |
|
|---|---|---|---|
| Correlation between age + rate of vol change (cc/yr): |
|||
| Correlation coefficient (r) | 0.064 | 0.037 | 0.230 |
| p Value | 0.285 | 0.584 | 0.092 |
| Correlation between age + rate of vol change (% change/yr): |
|||
| Correlation coefficient (r) | −0.012 | 0.006 | 0.211 |
| p Value | 0.846 | 0.931 | 0.123 |
Table 2.
Regression model to predict the rate of change in prostate volume for the overall study population
| Coefficient | p Value | |
|---|---|---|
| Age | −0.006 | 0.868 |
| Prostate vol | −0.017 | 0.553 |
| PSA | 0.997 | 0.0006 |
In the subset of 181 men who had baseline sex hormone measurements available a linear regression model was performed to examine the relationship between free testosterone index and the rate of change in prostate volume adjusting for baseline age, PSA and prostate volume. In this subset baseline age (p = 0.003), PSA (p = 0.005) and free testosterone index (p = 0.040) had significant positive associations with the rate of change in prostate volume, whereas baseline prostate volume had a statistically significant inverse relationship (p <0.0001).
DISCUSSION
In 1944 Swyer described the typical patterns of prostate growth in human men with different patterns emerging after age 45.10 Specifically he suggested that some men with BPH experience further increases in prostate size, while in others the size remains unchanged or the prostate atrophies with advancing age. More recently Tsukamoto et al examined the longitudinal changes in prostate volume in 67 Japanese men with lower urinary tract symptoms and at least 2 serial transrectal ultrasound measurements.11 Prostate volume increased in 46 men (70%), remained stable in 10 (15%) and decreased in 11 (15%).
Using prostate volume measurements from MRI instead, we found that a larger proportion of community men (38%) had a stable or decreasing prostate size with age compared to prostate growth. However, differences in study design (clinical cohort vs unselected community sample) limit comparisons with the study by Tsukamoto et al.11
Of note, several other population based studies have instead used TRUS to evaluate prostate volume changes over time. Bosch et al reported on men from the population based Krimpen study who had transrectal ultrasound examinations at baseline, and 2.1 and 4.2 years of followup.12 They calculated an average increase in prostate volume of 2.2% yearly. In another population based study Rhodes et al reported an average annual prostate volume increase of 1.6%, and demonstrated a relationship between larger baseline prostate size and growth rate.13
Our group previously reported a relationship between baseline PSA and the long-term risk of prostatic enlargement.14 In the current study we similarly demonstrated a significant relationship between baseline PSA and the rate of change in volume, adjusting for age and initial prostate volume.
Despite the large body of literature on BPH, less is known about the opposing phenomenon of prostate shrinkage in the absence of androgen deprivation.1 Indeed the reasons for prostate shrinkage in some healthy community men are unknown and could relate to various genetic, hormonal or environmental factors. Clearly further investigation is warranted at a basic level to elucidate the underlying pathophysiology of such disparate growth patterns in aging men. We did find a significant association between the baseline free testosterone index and the rate of change in volume in the subset with baseline sex hormone data. However, serial testosterone measurements were not available for the majority of study participants, precluding an evaluation of the role of changes over time.
Another interesting finding in our overall study population was the lack of a statistically significant correlation between age and the rate of change in prostate volume. These results are in agreement with those of St. Sauver et al, who previously demonstrated a relatively stable annual percent change in sonographic prostate volume in men 40 to 79 years old.6
A limitation of our study is that prostate volume estimates were based on MRI, whereas TRUS is primarily used for prostate volume measurement in clinical practice. Although prostate volume calculations correlate well between TRUS and MRI (r >0.8), it is possible that small volume changes using either modality may be artifactual.15 Nevertheless, Rahmouni et al compared prostate size estimates using MRI or TRUS to specimen weight at radical prostatectomy and showed that MRI is more accurate.16
Another limitation is that the median followup of 4.3 years is relatively short. Based on Swyer’s data larger changes in prostate volume may have become apparent in both studies with additional followup.10 In addition, the BLSA study population was primarily white so the present observations on prostate volume changes may not be generalizable to other ethnic groups. However, the median prostate volume in our study (28 cc) was consistent with the reported range of 16.7 to 29.2 cc for men in the sixth decade of life from several autopsy studies.1 Finally MRI based prostate volume measurements were initiated in 1993 and, therefore, were not available for a considerable proportion of male BLSA participants.
CONCLUSIONS
Changes in prostate size are highly variable in the aging male population. Although BPH ultimately affects the majority of aging men, a considerable proportion instead have stable or slight decreases in prostate size with age. Future research is warranted into the genetic, hormonal and environmental factors that determine the differential prostatic growth patterns in aging men.
Acknowledgments
Supported by the Intramural Research Program of the National Institutes of Health, National Institute on Aging.
Study received institutional review board approval.
Abbreviations and Acronyms
- BLSA
Baltimore Longitudinal Study of Aging
- BPH
benign prostatic hyperplasia
- MRI
magnetic resonance imaging
- PSA
prostate specific antigen
- TRUS
transrectal ultrasound
Footnotes
Nothing to disclose.
REFERENCES
- 1.Berry SJ, Coffey DS, Walsh PC, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132:474. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 2.Wei JT, Calhoun E, Jacobsen SJ. Urologic Diseases in America Project: benign prostatic hyperplasia. J Urol. 2008;179:S75. doi: 10.1016/j.juro.2008.03.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tempany CM, Partin AW, Zerhouni EA, et al. The influence of finasteride on the volume of the peripheral and periurethral zones of the prostate in men with benign prostatic hyperplasia. Prostate. 1993;22:39. doi: 10.1002/pros.2990220106. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan SA, McConnell JD, Roehrborn CG, et al. Combination therapy with doxazosin and finasteride for benign prostatic hyperplasia in patients with lower urinary tract symptoms and a baseline total prostate volume of 25 ml or greater. J Urol. 2006;175:217. doi: 10.1016/S0022-5347(05)00041-8. [DOI] [PubMed] [Google Scholar]
- 5.Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate-specific antigen concentration is a powerful predictor of acute urinary retention and need for surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology. 1999;53:473. doi: 10.1016/s0090-4295(98)00654-2. [DOI] [PubMed] [Google Scholar]
- 6.St. Sauver JL, Jacobson DJ, Girman CJ, et al. Tracking of longitudinal changes in measures of benign prostatic hyperplasia in a population based cohort. J Urol. 2006;175:1018. doi: 10.1016/S0022-5347(05)00408-8. [DOI] [PubMed] [Google Scholar]
- 7.Williams AM, Simon I, Landis PK, et al. Prostatic growth rate determined from MRI data: age-related longitudinal changes. J Androl. 1999;20:474. [PubMed] [Google Scholar]
- 8.Carter HB, Pearson JD, Metter EJ, et al. Longitudinal evaluation of prostate-specific antigen levels in men with and without prostate disease. JAMA. 1992;267:2215. [PMC free article] [PubMed] [Google Scholar]
- 9.Parsons JK, Carter HB, Platz EA, et al. Serum testosterone and the risk of prostate cancer: potential implications for testosterone therapy. Cancer Epidemiol Biomarkers Prev. 2005;14:2257. doi: 10.1158/1055-9965.EPI-04-0715. [DOI] [PubMed] [Google Scholar]
- 10.Swyer GI. Post-natal growth changes in the human prostate. J Anat. 1944;78:130. [PMC free article] [PubMed] [Google Scholar]
- 11.Tsukamoto T, Masumori N, Rahman M, et al. Change in International Prostate Symptom Score, prostrate-specific antigen and prostate volume in patients with benign prostatic hyperplasia followed longitudinally. Int J Urol. 2007;14:321. doi: 10.1111/j.1442-2042.2007.01596.x. [DOI] [PubMed] [Google Scholar]
- 12.Bosch JL, Tilling K, Bohnen AM, et al. Establishing normal reference ranges for prostate volume change with age in the population-based Krimpen-study: prediction of future prostate volume in individual men. Prostate. 2007;67:1816. doi: 10.1002/pros.20663. [DOI] [PubMed] [Google Scholar]
- 13.Rhodes T, Girman CJ, Jacobsen SJ, et al. Longitudinal prostate growth rates during 5 years in randomly selected community men 40 to 79 years old. J Urol. 1999;161:1174. [PubMed] [Google Scholar]
- 14.Wright EJ, Fang J, Metter EJ, et al. Prostate specific antigen predicts the long-term risk of prostate enlargement: results from the Baltimore Longitudinal Study of Aging. J Urol. 2002;167:2484. doi: 10.1016/s0022-5347(05)65010-0. [DOI] [PubMed] [Google Scholar]
- 15.al-Rimawi M, Griffiths DJ, Boake RC, et al. Transrectal ultrasound versus magnetic resonance imaging in the estimation of prostatic volume. Br J Urol. 1994;74:596. doi: 10.1111/j.1464-410x.1994.tb09190.x. [DOI] [PubMed] [Google Scholar]
- 16.Rahmouni A, Yang A, Tempany CM, et al. Accuracy of in-vivo assessment of prostatic volume by MRI and transrectal ultrasonography. J Comput Assist Tomogr. 1992;16:935. doi: 10.1097/00004728-199211000-00020. [DOI] [PubMed] [Google Scholar]